Abstract
Sclerosing mesenteritis (SM) is a rare disorder that involves the mesenteric adipose tissue with chronic fibrosing inflammation. Few reports mention the natural history of severe SM cases. Here, we report a severe and relapsing SM case in which a long-term natural history could be followed. The patient had undergone surgery for small bowel stenosis of unknown cause 10 years earlier. He had stopped visiting the hospital at his discretion. He was admitted to the hospital 10 years later due to recurrent symptoms, and a close examination revealed multiple small intestinal strictures; thus, surgery was performed again. The pathological results revealed that the patient had SM, corticosteroid administration dramatically improved his symptoms, and he has maintained remission for a long time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sclerosing mesenteritis (SM) is a rare benign disorder that is characterized by fibroinflammatory changes in the mesenteric adipose tissue [1]. Only approximately 200 cases have been reported since Sulla first described retractile mesenteritis in 1924 [2,3,4,5]. SM, sometimes referred to by other names, such as mesenteric panniculitis or mesenteric lipodystrophy, is now generally accepted as an umbrella term [6, 7]. A recent systematic review on SM described that symptoms of SM are non-specific, such as abdominal pain, fever, weight loss, diarrhea, bloating, nausea, vomiting, and constipation, with varying degrees, and that the most prevalent complication is small bowel obstruction [3]. However, the natural course of SM remains unclear due to its rarity.
A definitive SM diagnosis can be made only by histopathology [8]. The frequent histopathological features include fibrosis with scant inflammation and fat necrosis in the adipose tissue of bowel mesentery [1, 3]. Conversely, asymptomatic or mild cases of SM may not justify histopathological examination. In such cases, SM is diagnosed by radiology. The most predominant computed tomography (CT) feature of SM is increased mesenteric fatty tissue density [8, 9].
SM treatment depends on its severity. Symptomatic cases may require surgery or medical treatment, while asymptomatic cases can be conservatively managed [1, 3]. Most SM cases have good courses; however, some cases have significant morbidity and a chronic debilitating course [10]. Here, we report a severe and relapsing case of SM with multiple ileal strictures in which we followed a long-term natural course.
Case presentation
An 84-year-old male patient was admitted to the Department of Gastroenterology and Hepatology, Nagahama City Hospital with chief complaints of abdominal pain and persistent diarrhea. He had a past history of appendicectomy and cholecystectomy. He had also undergone small bowel resection for multiple small intestinal strictures 10 years earlier at Shiga University of Medical Science. However, the small intestinal strictures had unknown causes at that time. He subsequently stopped visiting the hospital on his own initiative.
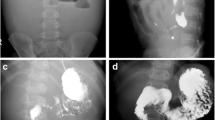
Laboratory tests on admission revealed elevated serum C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) (3.56 mg/dL and 64 mm/h, respectively), hypoalbuminemia (2.7 g/dL), and anemia (hemoglobin 10.7 g/dL). Interferon-gamma release assay (IGRA) for diagnosing latent tuberculosis infection was negative. A contrast-enhanced -CT revealed extensive wall thickening and multiple segmental strictures in the ileum near the anastomosis with increased mesenteric fat density and multiple swollen lymph nodes (Figs. 1a, b). Therefore, we performed a double-balloon enteroscopy (EI-580BT, Fujifilm Holdings Corporation, Tokyo, Japan) to observe the ileal mucosa and revealed shallow ulcers (Fig. 2a) and stricture with pre-stenotic dilation (Figs. 2b, c) in the ileum. No lesions were found in the colorectum. Initially, we highly suspected elderly-onset Crohn’s disease because of multiple ileal strictures, but the histopathology of the biopsy specimens from the ileum mucosa revealed no evidence of Crohn’s disease such as noncaseating granulomas. The strictures around the anastomosis were too long and considered to require small intestinal resection although the cause of the ileum lesions remained unknown at that point (Fig. 2c, red arrows).
Ileocecal resection was then performed at the Shiga University of Medical Science Hospital. The postoperative course was uneventful, and the patient was discharged 13 days postoperatively. The pathological results of the surgical specimen revealed severe mesenteric adipose tissue fibrosis with poor inflammatory cell infiltration (Figs. 3a, b), resulting in SM diagnosis. Severe fibrosis was observed just below the small intestinal ulcer site (Figs. 3c, d), indicating that the ileal ulcers may be due to mesenteric fatty tissue fibrosis. The mucosa demonstrated no disease-specific or characteristic inflammatory findings, such as inflammatory bowel disease. Arteritis and phlebitis were also absent. Because some cases of SM show histologically characteristic findings of IgG4-related disease [11], we also checked serum IgG4 level and found it to be normal.
The pathological findings (hematoxylin and eosin stain) of the surgical specimen. Irregular mesenteric adipose tissue fibrosis with poor inflammatory cell infiltration was observed (a, original magnification ×40; b, original magnification ×100). Severe fibrosis was also seen just below the ileal ulcer site (c, original magnification ×40; d, original magnification ×100)
Surgery did not completely ameliorate diarrhea and abdominal pain and lymph nodes remained swollen in CT examination (Fig. 4a). Therefore, we initiated oral prednisolone at 40 mg daily. Promptly thereafter, the symptoms improved and serum CRP and ESR decreased. Furthermore, the increased mesenteric fatty tissue density and swollen lymph nodes almost disappeared (Fig. 4b). Prednisolone has been reduced gradually and is currently maintained at 5 mg/day. At present, the patient has not had a recurrence for more than 2 years.
Discussion and conclusions
This report presents a case of SM with multiple ileal strictures that required surgery. Postoperatively, a histopathological examination revealed SM. His surgical history for small intestinal strictures 10 years earlier was considered a series of SM symptoms.
SM is a rare fibroinflammatory disorder that primarily affects the adipose tissue of mesentery with varying degrees [12]. The etiology, natural history, prognosis, and optimal treatment remained unknown because only approximately 200 cases have been reported. SM appears to be a disease of middle-aged or elderly people, with onset in the 50 s to 70 s and affects males more frequently than females, consistent with our case [13]. Elevated CRP and ESR are frequently seen in patients with SM. Low protein levels and anemia were the other predominant abnormalities [3]. We could not confirm the definitive diagnosis of SM despite presenting these abnormalities because they are not specific tests for SM.
The differential diagnosis for ileal strictures is diverse, including neoplasms, Crohn’s disease, nonsteroidal anti-inflammatory drug (NSAID)-induced ulcerations, intestinal tuberculosis, post-surgical strictures, and chronic enteropathy associated with SLCO2A1 (CEAS) [14,15,16]. Our case was not taking NSAIDs and was negative for IGRA, indicating no possibility of NSAID-induced ulcers and intestinal tuberculosis. Although we did not perform a genetic examination of the SLCO2A1 gene, it is unlikely that our case is CEAS, since CEAS is usually not accompanied by mesenteric fatty tissue fibrosis. We initially suspected old-onset Crohn’s disease because SM is not well known to present with severe small bowel strictures, but pathology results confirmed an SM diagnosis. To the best of our knowledge, a few previous studies reported SM with such severe multiple ileum stenosis [1, 17].
The pathogenesis of SM is poorly understood, although several causes have been indicated, including previous surgery, vasculitis, trauma, paraneoplasia, autoimmunity, medications, and infection [2, 3]. Recently, there have been reports of IgG4-related SM [11], but in this case, serum IgG4 level was normal and pathological findings showed poor inflammatory cell infiltration, including plasma cells, suggesting that this case is not IgG4-related SM.
Previous surgery can cause SM, and our case had a history of small bowel resection 10 years earlier. However, the small intestinal strictures before the second surgery were similar to the ones before the first surgery, indicating that these were a series of SM symptoms. Coincidentally, our case had discontinued visiting the hospital on his initiative after the first surgery, which enabled us to follow the poor natural course of SM over 10 years. This poor course indicates the importance of medical treatment in severe cases.
Medical therapy for SM remains unestablished but is recommended in symptomatic cases [1]. Corticosteroids were most predominantly used, although other drugs, such as colchicine, tamoxifen, 6-mercaptopurine, azathioprine, methotrexate, and infliximab, have been administered [3]. No optimal schedule for corticosteroid reduction has been established, and criteria for corticosteroid discontinuation remained unavailable. We have continued to administer corticosteroids at low doses in our case, considering the severe and poor course, and no signs of recurrence have been observed thus far. Accumulating refractory or relapsed cases is necessary to establish treatment methods. Hence, this case is considered valuable.
In conclusion, we encountered a case of relapsing SM with ileal multiple strictures. SM should be suspected when the patient presents with unexplained ileal strictures accompanied by swollen lymph nodes.
Abbreviations
- SM:
-
Sclerosing mesenteritis
- CT:
-
Computed tomography
- CRP:
-
C-reactive protein
- ESR:
-
Erythrocyte sedimentation rate
- IGRA:
-
Interferon-gamma release assay
- NSAID:
-
Nonsteroidal anti-inflammatory drug
- CEAS:
-
Chronic enteropathy associated with SLCO2A1
References
Akram S, Pardi DS, Schaffner JA, et al. Sclerosing mesenteritis: clinical features, treatment, and outcome in ninety-two patients. Clin Gastroenterol Hepatol. 2007;5:589–96.
McLaughlin PD, Filippone A, Maher MM. The “misty mesentery”: mesenteric panniculitis and its mimics. AJR Am J Roentgenol. 2013;200:W116–23.
Sharma P, Yadav S, Needham CM, et al. Sclerosing mesenteritis: a systematic review of 192 cases. Clin J Gastroenterol. 2017;10:103–11.
Corado SC, Almeida H, Baltazar JR. A severe case of sclerosing mesenteritis. BMJ Case Rep. 2019. https://doi.org/10.1136/bcr-2018-229035.
Sulla JV. Mesenterite rectratile e sclerosante. Policlinico. 1924; 575–81
Emory TS, Monihan JM, Carr NJ, et al. Sclerosing mesenteritis, mesenteric panniculitis and mesenteric lipodystrophy: a single entity? Am J Surg Pathol. 1997;21:392–8.
Nyberg L, Bjork J, Bjorkdahl P, et al. Sclerosing mesenteritis and mesenteric panniculitis—clinical experience and radiological features. BMC Gastroenterol. 2017;17:75.
van Breda Vriesman AC, Schuttevaer HM, Coerkamp EG, et al. Mesenteric panniculitis: US and CT features. Eur Radiol. 2004;14:2242–8.
Wat SY, Harish S, Winterbottom A, et al. The CT appearances of sclerosing mesenteritis and associated diseases. Clin Radiol. 2006;61:652–8.
Mc Cormack O, Meaney JF, Reynolds JV. Resolving sclerosing mesenteritis. Surgery. 2013;153:879–80.
Fukuda M, Miyake T, Matsubara A, et al. Sclerosing mesenteritis mimicking IgG4-related disease. Intern Med. 2020;59:513–8.
Issa I, Baydoun H. Mesenteric panniculitis: various presentations and treatment regimens. World J Gastroenterol. 2009;15:3827–30.
Vlachos K, Archontovasilis F, Falidas E, et al. Sclerosing mesenteritis: diverse clinical presentations and dissimilar treatment options. A case series and review of the literature: Int Arch Med.; 2011. https://doi.org/10.1186/1755-7682-4-17.
Tsuboi A, Oka S, Tanaka S, et al. Experience with balloon dilatation in crohn’s and non-crohn’s benign small-bowel strictures: is there a difference? Gastroenterol Res Pract. 2019;2019:1262595.
Matsumoto T, Nakamura S, Esaki M, et al. Endoscopic features of chronic nonspecific multiple ulcers of the small intestine: comparison with nonsteroidal anti-inflammatory drug-induced enteropathy. Dig Dis Sci. 2006;51:1357–63.
Hosoe N, Ohmiya N, Hirai F, et al. Chronic enteropathy associated with SLCO2A1 gene [CEAS]-characterisation of an enteric disorder to be considered in the differential diagnosis of Crohn’s disease. J Crohns Colitis. 2017;11:1277–81.
Mazure R, Fernandez Marty P, Niveloni S, et al. Successful treatment of retractile mesenteritis with oral progesterone. Gastroenterology. 1998;114:1313–7.
Funding
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this article. This work was supported by JSPS KAKENHI Grant Number JP21K15947.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors state no conflict of interest (COI).
Consent for publication
The patient has provided informed consent for the publication of this case report and accompanying images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ohno, M., Nishida, A., Imai, T. et al. Relapsing sclerosing mesenteritis with multiple strictures of the small intestine. Clin J Gastroenterol (2024). https://doi.org/10.1007/s12328-024-01989-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12328-024-01989-w