Abstract
Percutaneous vertebral augmentation (PVA), which includes percutaneous kyphoplasty (PKP) and percutaneous vertebroplasty (PVP). Robot-assisted (RA) and fluoroscopy-assisted (FA) are important methods for treating osteoporotic vertebral compression fractures (OVCFs), though it is still unclear which is superior. This analysis aimed to compare the efficacy and safety of RA and FA. PubMed, Web of Science, Cochrane Library, and China National Knowledge Infrastructure were systematically searched, the outcomes included surgical parameters (leakage rate, operation time, number of fluoroscopic, injection volume, inclination angle), and clinical indexes (hospital stays, Visual Analog Scale (VAS), Oswestry Disability Index (ODI), Cobb angle, the midline height of vertebral). Thirteen articles involving 1094 patients were included. RA group produced better results than the FA group in the leakage rate (OR = 0.27; 95% CI 0.17–0.42; P < 0.00001), number of fluoroscopic (WMD = – 13.88; 95% CI – 18.47 to – 9.30; P < 0.00001), inclination angle (WMD = 5.02; 95% CI 4.42–5.61; P < 0.00001), hospital stays (WMD = – 0.32; 95% CI – 0.58 to – 0.05; P = 0.02), VAS within 3 days (WMD = – 0.19; 95% CI – 0.26 to – 0.12; P < 0.00001), Cobb angle within 3 days (WMD = – 1.35; 95% CI – 2.56 to – 0.14; P = 0.003) and Cobb angle after 1 month (WMD = – 1.02; 95% CI – 1.84 to – 0.20; P = 0.01). But no significant differences in operation time, injection volume, ODI, the midline height of vertebral, and VAS score after 1 month. Our analysis found that the RA group had lower cement leakage rates, number of fluoroscopic and hospital stays, a larger inclination angle, better short-term pain improvement, and Cobb angle improvement. It is worth acknowledging that robotic-assisted surgery holds promise for the development of spine surgery. The study was registered in the PROSPERO (CRD42023393497).
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporotic vertebral compression fractures (OVCFs) commonly occur in elderly individuals with osteoporosis. Vertebral compression fractures can occur due to minor forces, as a result of reduced bone density and weakened bone mass. These fractures can cause back pain, reduced height, abnormal body posture, and other issues that significantly impact the quality of life of elderly individuals. OVCFs are increasingly posing a health threat to elderly individuals. Therefore, early diagnosis and treatment of OVCFs are crucial for maintaining their health and quality of life [1, 2]. Percutaneous vertebral augmentation (PVA) is an interventional procedure for the treatment of OVCFs that includes percutaneous kyphoplasty (PKP) and percutaneous vertebroplasty (PVP). In both procedures, the surgeon injects special bone cement into the vertebral body to enhance stability and reduce pain. Percutaneous vertebral augmentation is considered one of the current methods of choice for the treatment of OVCFs because it is a minimally invasive procedure that reduces patient pain and recovery time [3]. Percutaneous vertebroplasty is an effective treatment for vertebral compression fractures. However, it cannot completely restore the original height of the vertebral body, as fractures typically cause a reduction in height [4]. Percutaneous kyphoplasty is different from percutaneous vertebroplasty because it involves inserting and expanding a balloon into the fracture space before cement injection, which restores vertebral height [5].
Surgical robotics is increasingly used in spine surgery to enhance the precision of PKP or PVP and reduce the risk of complications. Furthermore, it can reduce operating time and patient exposure to radiation, promoting better clinical outcomes [6]. Several studies [7,8,9] have reported the results of robot-assisted (RA) PKP or PVP surgery for OVCFs. It is important to note that clinical outcomes and complications of robot-assisted treatment of OVCFs may vary among studies due to limited sample size. Therefore, this meta-analysis evaluates clinical outcomes and imaging improvements of robot-assisted PKP or PVP for OVCFs and analyzes complications of robot-assisted PVA and fluoroscopy-assisted PVA for OVCFs, providing a scientific basis for spine surgeons to use robot-assisted treatment of OVCFs.
Materials and methods
Protocol and registration
This systematic review was reported according to updated PRISMA guidelines [10]. The study was registered in the PROSPERO (CRD42023393497).
Search strategy
To make a comprehensive search of all relevant studies, PubMed, Web of Science, Cochrane Library, and core journals of China National Knowledge Infrastructure were systematically searched by two independent reviewers (XW and YHZ). The free-word search of “(Robotic Surgical Procedures OR robotics) AND (percutaneous kyphoplasty OR PKP OR percutaneous vertebroplasty OR PVP) AND (osteoporotic vertebral compression fractures OR OVCFs)” was used. Meanwhile, a MeSH search of (“Robotic Surgical Procedures” [Mesh] AND (“Vertebroplasty” [Mesh]) OR “Kyphoplasty” [Mesh]) AND (“Spinal Fractures” [Mesh] AND “Osteoporotic Fractures” [Mesh])) was also used to provide additional results. The search results were last updated on April 30, 2023. The reference lists of included studies were also manually searched for additional eligible studies.
Selection strategy
The PICOS (Patient/Problem, Intervention, Comparison, Outcome, Study design) strategy was utilized to guide the study selection process. Two reviewers (XW and YHZ) independently screened articles based on predetermined inclusion and exclusion criteria. Any discrepancies were resolved through discussion until a consensus was reached. The inclusion criteria were as follows: (1) patients with symptomatic osteoporotic vertebral compression fractures; (2) percutaneous kyphoplasty (PKP) or percutaneous vertebroplasty (PVP) as interventional treatment; (3) comparative studies between robot-assisted and fluoroscopy-assisted treatments; (4) outcomes including at least one of the following data: leakage rate, number of fluoroscopic, Visual Analog Scale (VAS) [11], Oswestry disability index (ODI) [12], Cobb angle, and midline vertebral height; (5) observational studies and randomized controlled trials were eligible. Exclusion criteria were as follows: (1) case reports, reviews, or letters; (2) duplicate publications.
Data extraction
The data from eligible studies were extracted by two independent reviewers (XW and YHZ). Disagreements were resolved through discussion or with the involvement of a third reviewer until a consensus was reached. The indispensable data extracted from eligible studies included first author, publication time, study type, sample size, age, gender distribution, body mass index, bone mineral density (T score), type of robot, type of surgery, fracture site, surgical segment, follow-up time, and outcomes. The outcomes in this analysis included surgical parameters (leakage rate, operation time, number of fluoroscopic, injection volume, inclination angle), and clinical indexes (hospital stays, Visual Analog Scale (VAS), Oswestry Disability Index (ODI), Cobb angle, the midline height of vertebral). The number of fluoroscopic means the X-ray frequency of fluoroscopies, which refers to the number of fluoroscopy shots in one operation, not the total time that the device was actively radiating. The operation time means the overall time during a surgical procedure, mainly includes robot positioning time and surgery handling time.
Risk of bias
The risk of bias was independently analyzed by two reviewers (XW and YHZ). Disagreements were resolved by recruiting a third author to attain a consensus. We assessed the risk of bias of RCTs using the revised Cochrane risk of bias tool for randomized trials (RoB2.0) [13]. The risk of bias of non-randomized comparative studies was assessed using the risk of bias in non-randomized studies of interventions (ROBINS-I) tool [14]. Sensitivity analysis was performed by excluding a single study of each study in turn and reanalyzing the data. Publication bias was analyzed qualitatively by funnel plot.
Level of evidence
We assessed the overall quality of evidence using the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) criteria. The studies included were evaluated by two independent reviewers (XW and YHZ) for risk of bias, inconsistency, indirectness, imprecision, and publication bias. Based on these evaluations, the quality of evidence was classified as high, moderate, low, or very low.
Statistical analysis
For continuous data, we calculated the weighted mean difference (WMD) or standardized mean difference (SMD) and their 95% confidence interval (CI), and for dichotomous data, we calculated the odds ratio (OR) and its 95% CI. We assessed statistical heterogeneity using the chi-square test and I-square test [15]. Heterogeneity was considered significant if the p value of the chi-square test was less than 0.10 or if the I2 value exceeded 50%. We used a random-effects model when I2 was greater than 50% and a fixed-effects model when I2 was less than 50%. We performed this meta-analysis using RevMan 5.3 software (Cochrane Collaboration, Copenhagen, Denmark), and the level of statistical significance was set at P < 0.05.
Results
Selection and characteristics of included studies
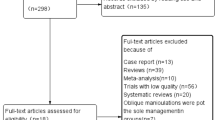
The screening process of articles is presented in Fig. 1. Initially, a total of 102 articles were identified, out of which 20 were considered for full-text evaluation after the screening. Finally, thirteen articles involving 1094 patients were included in this meta-analysis. Table 1 summarized the characteristics of the included studies, all of which were published between 2018 and 2023. Six articles [16,17,18,19,20,21] investigated the clinical efficacy of robot-assisted PKP for OVCFs, and seven articles [22,23,24,25,26,27,28] reported on the treatment of OVCFs with robot-assisted PVP.
Risk of bias and quality of evidence
The risk of bias assessment for randomized clinical trials was summarized in Table 2, while Table 3 summarized the risk of bias assessment for nonrandomized studies. The risk of bias was considered low in nine studies [16,17,18,19, 21, 23, 25, 26, 28] and moderate in four studies [20, 22, 24, 27]. The overall quality of the evidence of the included studies was shown in the supplementary information (supplementary Table S1).
Outcome analysis of surgical parameters
Leakage rate
A total of twelve studies [16,17,18,19,20,21,22,23,24,25,26, 28] involving 1064 patients compared the cement leakage rate between the RA group and the FA group. The meta-analysis was conducted using a fixed-effect model with I2 = 0. In subgroup analysis, the RA-PKP group (OR = 0.23; 95% CI 0.12–0.43; P < 0.00001) and RA-PVP group (OR = 0.32; 95% CI 0.17–0.58; P = 0.0002) had equally good results in reducing bone cement leakage rate, and there was no heterogeneity between the PKP group and the PVP group in the subgroup. The overall outcomes indicated that the cement leakage rate was significantly lower in the RA group than in the FA group (OR = 0.27; 95% CI 0.17–0.42; P < 0.00001). (Fig. 2).
Operation time
A total of twelve studies [16,17,18, 20,21,22,23,24,25,26,27,28] involving 939 patients reported the effect of robotic-assisted treatment on operation time, the figure was shown in the supplementary information (supplementary Fig. S1). In the subgroup analysis, compared with the FA group, there was no significant difference in the reduction of operation time in both the RA-PKP group (WMD = 0.96; 95% CI – 9.28 to 11.20; P = 0.85) and RA-PVP group (WMD = – 9.98; 95% CI – 21.56 to 1.60; P = 0.09). And there was high heterogeneity between the PKP group and the PVP group in the subgroup (I2 = 48%). The overall outcomes indicated that compared with the FA group, the difference in operative time in the RA group was not statistically significant (WMD = – 5.38; 95% CI – 13.25 to 2.50; P = 0.18), and there was high heterogeneity (I2 = 99%).
Number of fluoroscopic
Eight studies [16,17,18, 20, 23, 24, 26, 28] involving 477 patients compared the number of fluoroscopic between the RA group and the FA group. In subgroup analysis, the RA-PKP group (WMD = – 14.79; 95% CI – 22.24 to – 7.33; P = 0.0001) and RA-PVP group (MD = – 13.32; 95% CI – 20.64 to – 6.01; P = 0.0004) had equally good results in reducing the number of fluoroscopic, and there was no heterogeneity between the PKP group and the PVP group in the subgroup. The overall outcomes indicated that the number of fluoroscopic was significantly fewer in the RA group than in the FA group (WMD = – 13.88; 95% CI – 18.47 to – 9.30; P < 0.00001), and there was high heterogeneity (I2 = 97%). (Fig. 3).
Injection volume
A total of eight studies [18,19,20,21,22,23, 25, 26] involving 805 patients compared the injection volume between the RA group and the FA group, the figure was shown in supplementary information (supplementary Fig. S2). In the subgroup analysis, compared with the FA group, there was no significant difference in the injection volume in both the RA-PKP group (WMD = 0.03; 95% CI – 0.81 to 0.87; P = 0.94) and RA-PVP group (WMD = – 0.85; 95% CI – 1.71 to 0.01; P = 0.05). And there was high heterogeneity between the PKP group and the PVP group in the subgroup (I2 = 51.6%). The overall outcomes indicated that compared with the FA group, the difference in the injection volume in the RA group was not statistically significant (WMD = – 0.43; 95% CI – 1.05 to 0.19; P = 0.18), and there was high heterogeneity (I2 = 91%).
Inclination angle
As was shown in the supplementary information (supplementary Fig. S3), only two studies [18, 25] involving 204 patients compared the inclination angle between the RA group and the FA group, the two studies are both RCTs and there was no heterogeneity. The overall outcomes indicated that the inclination angle was significantly larger in the RA group than in the FA group (WMD = 5.02; 95% CI 4.42–5.61; P < 0.00001).
Outcome analysis of clinical indexes
Hospital stays
A total of six studies [17, 20, 21, 23, 25, 28] involving 612 patients compared the hospital stays between the RA group and the FA group. In the subgroup analysis, compared with the FA group, there was no significant difference in the hospital stays in both the RA-PKP group (WMD = – 0.21; 95% CI – 0.54 to 0.12; P = 0.21) and RA-PVP group (WMD = – 0.49; 95% CI – 1.03 to 0.05; P = 0.08), and there was no heterogeneity between the PKP group and the PVP group in the subgroup. The overall outcomes indicated that the hospital stays were significantly shorter in the RA group than in the FA group (WMD = – 0.32; 95% CI – 0.58 to – 0.05; P = 0.02), and there was high heterogeneity (I2 = 50%) (Fig. 4).
Visual analog scale (VAS)
A total of ten studies [16, 19,20,21,22, 24,25,26,27,28] involving 930 patients compared the VAS score within 3 days between the RA group and the FA group. In subgroup analysis, the RA-PKP group (WMD = – 0.19; 95% CI – 0.34 to – 0.04; P = 0.01) and RA-PVP group (WMD = – 0.19; 95% CI – 0.27 to – 0.11; P < 0.00001) had equally good results in reducing the VAS score within 3 days, and there was no heterogeneity between the PKP group and the PVP group in the subgroup. The overall outcomes indicated that the VAS score within 3 days was significantly lower in the RA group than in the FA group (WMD = – 0.19; 95% CI – 0.26 to – 0.12; P < 0.00001), and there was low heterogeneity (I2 = 4%). (Fig. 5A).
A total of eleven studies [16, 18,19,20,21,22,23, 25,26,27,28] involving 944 patients compared the VAS score after 1 month between the RA group and the FA group. In the subgroup analysis, compared with the FA group, there was no significant difference in the VAS score after 1 month in both the RA-PKP group (WMD = – 0.04; 95% CI – 0.24 to 0.16; P = 0.70) and RA-PVP group (WMD = – 0.12; 95% CI – 0.43 to 0.19; P = 0.44), and there was no heterogeneity between the two groups in the subgroup. The overall outcomes indicated that compared with the FA group, the difference in the VAS score after 1 month in the RA group was not statistically significant (WMD = – 0.08; 95% CI – 0.25 to 0.09; P = 0.35), and there was high heterogeneity(I2 = 75%). (Fig. 5B).
Oswestry disability index (ODI)
As was shown in the supplementary information (supplementary Fig. S4A), a total of six studies [21, 22, 24, 25, 27, 28] involving 602 patients compared the ODI score within 3 days between the RA group and the FA group. In the subgroup analysis, compared with the FA group, there was no significant difference in the ODI score within 3 days in both the RA-PKP group (SMD = – 0.22; 95% CI – 0.06 to 0.50; P = 0.12) and RA-PVP group (SMD = – 0.30; 95% CI – 0.65 to 0.05; P = 0.10), and there was high heterogeneity between the two groups in the subgroup (I2 = 80.7%). The overall outcomes indicated that compared with the FA group, the difference in the ODI score within 3 days in the RA group was not statistically significant (SMD = – 0.17; 95% CI – 0.56 to 0.21; P = 0.38), and there was high heterogeneity (I2 = 78%).
And five studies [21, 22, 26,27,28] involving 512 patients compared the ODI score after 1 month between the RA group and the FA group. Compared with the FA group, there was no significant difference in the ODI score after 1 month in both the RA-PKP group (SMD = – 0.10; 95% CI – 0.38 to 0.18; P = 0.48) and RA-PVP group (SMD = – 0.09; 95% CI – 0.32 to 0.14; P = 0.45), and there was no heterogeneity between the two groups in the subgroup. The overall outcomes indicated that compared with the FA group, the difference in the ODI score after 1 month in the RA group was not statistically significant (SMD = – 0.09; 95% CI – 0.27 to 0.08; P = 0.30), and there was no heterogeneity (supplementary Fig. S4B).
Cobb angle
As was shown in the supplementary information (supplementary Fig. S5A), a total of three studies [16, 20, 25] involving 269 patients compared the Cobb angle within 3 days between the RA group and the FA group. In subgroup analysis, the RA-PKP group (WMD = – 1.98; 95% CI – 3.94 to – 0.03; P = 0.05) and RA-PVP group (WMD = – 0.90; 95% CI – 1.24 to – 0.56; P < 0.00001) had equally good results in reducing the Cobb angle within 3 days, and there was low heterogeneity between the two groups in the subgroup (I2 = 13.3%). The overall outcomes indicated that the Cobb angle within 3 days was significantly lower in the RA group than in the FA group (WMD = – 1.35; 95% CI – 2.56 to – 0.14; P = 0.003), and there was high heterogeneity (I2 = 50%).
And five studies [16, 18, 19, 23, 25] involving 498 patients compared the Cobb angle after 1 month between the RA group and the FA group. As was shown in the supplementary information (supplementary Fig. S5B), in subgroup analysis, the RA-PKP group (WMD = – 1.64; 95% CI – 2.91 to – 0.37; P = 0.01) showed a significantly lower Cobb angle compared with the FA group. However, there was no significant difference in the Cobb angle after 1 month in both the RA-PVP group (WMD = – 0.45; 95% CI – 1.66 to 0.76; P = 0.47), and there was high heterogeneity between the two groups in the subgroup (I2 = 43.3%). The overall outcomes indicated that the Cobb angle after 1 month was significantly lower in the RA group than in the FA group (WMD = – 1.02; 95% CI – 1.84 to – 0.20; P = 0.01), and there was high heterogeneity (I2 = 59%).
The midline height of vertebral
As was shown in the supplementary information (supplementary Fig. S6A), only three studies [16, 20, 28] involving 139 patients compared the midline height of vertebral within 3 days between the RA group and the FA group. In the subgroup analysis, compared with the FA group, there was no significant difference in the midline height of vertebral within 3 days in both the RA-PKP group (WMD = – 1.53; 95% CI – 10.64 to 7.58; P = 0.74) and RA-PVP group (WMD = 0.58; 95% CI – 1.77 to 2.93; P = 0.63), and there was no heterogeneity between the two groups in the subgroup. The overall outcomes indicated that compared with the FA group, the difference in the midline height of vertebral within 3 days in the RA group was not statistically significant (WMD = – 0.73; 95% CI – 5.65 to 4.19; P = 0.77), and there was high heterogeneity (I2 = 95%).
As was shown in the supplementary information (supplementary Fig. S6B), four studies [16, 18, 19, 28] involving 288 patients compared the midline height of vertebral after 1 month between the RA group and the FA group. In the subgroup analysis, compared with the FA group, there was no significant difference in the midline height of the vertebral after 1 month in both the RA-PKP group (WMD = 1.43; 95% CI – 0.45 to 3.31; P = 0.14) and RA-PVP group (WMD = 0.22; 95% CI – 1.92 to 2.36; P = 0.84), and there was no heterogeneity between the two groups. The overall outcomes indicated that compared with the FA group, the difference in the midline height of vertebral after 1 month in the RA group was not statistically significant (WMD = 1.17; 95% CI –0.52 to 2.87; P = 0.18), and there was high heterogeneity (I2 = 93%).
Sensitivity analysis and publication bias
Significant interstudy heterogeneity was observed in the meta-analysis of various factors, including operation time, number of fluoroscopies, injection volume, hospital stays, VAS score after 1 month, ODI score within 3 days, Cobb angle, and midline height of vertebral (I2 > 50%). We conducted a sequential single-elimination analysis to identify potential sources of heterogeneity. The results showed that heterogeneity was significantly reduced in hospital stays, VAS score after 1 month, ODI score within 3 days, and midline height of vertebral, but not in operation time, number of fluoroscopies, injection volume, and Cobb angle. Possible reasons for the high degree of heterogeneity may include differences in the fracture location, surgical technique, and robot type. Publication bias was not evident based on the funnel plot as shown in the supplementary information (supplementary Fig. S7).
Discussion
The purpose of this meta-analysis was to examine the clinical efficacy and safety of robot-assisted PKP or PVP for the treatment of OVCFs. The results showed that RA-PKP or RA-PVP produced better results than FA-PKP or FA-PVP regarding the leakage rate, number of fluoroscopic, inclination angle, hospital stays, Visual Analog Scale, and Cobb angle.
Cement leakage is a common complication of PKP or PVP surgery, which can result in adverse outcomes. It often occurs when the vertebral body's hollow bony structures are filled with cement, causing it to leak into the surrounding soft tissues or vascular system. Previous studies have shown that several factors may contribute to cement leakage, including the degree of vertebral body osteoporosis, cement filling pressure and rate, and surgical skill and experience level [29, 30]. Cement leakage risk may increase due to low BMD value (T score < – 3.0 SD), cortical bone defects, and inappropriate timing of cement injection (early stage of wire drawing) [31]. The meta-analysis revealed that the use of robotic-assisted techniques effectively reduced the incidence of bone cement leakage during PKP or PVP treatment for OVCFs. The incidence of bone cement leakage was significantly lower in the RA group compared to the FA group. This is attributed to the precise puncture provided by the robotic-assisted technique, which reduces the risk of cement leakage by minimizing damage to the pedicle wall and vertebral body. Therefore, the use of robotic-assisted techniques can effectively enhance the safety of PKP or PVP for OVCFs.
The evaluation of robot-assisted surgery merits requires considering important parameters such as operation time, the number of fluoroscopic, injection volume, and inclination angle. Operation time mainly includes positioning time and surgery handling time. The installation of the robot and the use of robotic software, which are unique technical features of RA, also lead to an increased operative time in the RA group. Our analysis did not reveal any significant differences between the RA and FA groups regarding operation time and bone cement injection volume. In different studies, the operation time varies among the RA groups [32, 33], and some learning curve studies [9, 34] have also suggested that total surgery time and robot-assisted surgery time may decrease as the number of cases increases. The operation time in the RA group can vary depending on the type of robotic equipment, surgical experience, and patient condition, and different types of robots also require different preoperative preparation times. The Mazor robotic system preplans the puncture path for surgery by utilizing computed tomography (CT) scans to generate three-dimensional (3D) images. On the other hand, the TiRobot robotic system relies on automatic registration with intraoperative 3D C-arm scans for determining the puncture path. Nonetheless, robotic-assisted technology can generally enhance the efficiency and precision of surgeries, resulting in shorter operation time in the RA group, as observed in many investigations. Notably, the operation time is just one aspect of evaluating the efficacy of robot-assisted technology.
The risk of exposure to high doses of radiation during PKP or PVP surgery is a significant concern in the treatment of OVCFs since it can elevate the risk of future malignancies. Despite the advances in minimally invasive spine surgery and the use of protective clothing and lead plates during surgery, spine surgeons still have vulnerable body parts that are not adequately shielded from radiation [35]. The number of fluoroscopies means fluoroscopy frequency, it includes puncture fluoroscopy number and bone cement perfusion fluoroscopy number. Our meta-analysis revealed a significant reduction in the number of fluoroscopies used in both the RA-PKP and RA-PVP groups, despite high heterogeneity in the number of fluoroscopies reported between studies. Our findings suggested that robot-assisted technology can significantly reduce the risk of fluoroscopy for both surgeons and patients during PKP or PVP procedures. The heterogeneity in reports of fluoroscopies was found to be influenced by surgeon proficiency in robot operation and the type of robotic system used. For instance, the Mazor robotic system plans the puncture path before surgery using computed tomography (CT) scans to create 3D images, while the TiRobot robotic system requires automatic registration with intraoperative 3D C-arm scans. Surgeon proficiency in robot operation and experience levels may also impact surgical outcomes. Additionally, operational difficulty, visualization, and safety vary among different types of robotic systems, all of which can affect the outcome and safety of the procedure.
Robot-assisted technology has been widely used in the medical field, especially in spine surgery [36, 37]. This technology can improve the accuracy and safety of surgery and reduce the risk and complications of surgery [38, 39]. The meta-analysis showed that the RA group had a significantly greater inclination angle during the PKP or PVP procedure than the FA group. During surgery, the increased inclination angle allows the guide needle to be placed closer to the vertebral midline, resulting in more uniform cement distribution, but it also increases the risk of breaking through the bone cortex during free puncture. In contrast, robotic-assisted technology allows for a safe increase in inclination angle during route planning, which ensures a safe puncture by bringing the needle closer to the vertebral midline. This reduces the risk of cortical breakage, nerve damage, and dural sac rupture from accidental entry into the spinal canal. Furthermore, this technique allows for more precise placement of the balloon in the center of the vertebral body or at the site of the most severe fracture collapse. This reduces the risk of cortical breach during free puncture, ensuring safe and even cement distribution, ultimately improving the accuracy and safety of the procedure.
Our analysis suggested that robot-assisted PKP or PVP for OVCFs is effective in reducing patients' length of stay and pain levels in the short term, especially within 3 days postoperatively. This result can be attributed to the high precision and efficiency of the robot-assisted technique. Compared with traditional FA techniques, which often require multiple adjustments of the puncture point based on fluoroscopic results, long working channel establishment time, and high pain irritation to the patient, robot-assisted techniques can accurately place the guide needle at one time and then accurately place the working channel along the guide needle, which is more accurate and faster in guide needle placement and working channel establishment, and can significantly reduce pain irritation and operation time to the patient, thus improving safety and efficiency. Despite the significant short-term effects, our meta-analysis also found that robot-assisted PKP or PVP for OVCFs was similar to fluoroscopy-assisted in terms of long-term pain improvement and functional improvement, with no statistical difference in VAS scores and ODI scores between the RA group and the FA group at 1 month. This suggests that although robotic-assisted techniques can provide short-term advantages in surgery, they do not significantly improve the long-term prognosis of patients. Therefore, when choosing a surgical option, we need to consider several factors such as surgical safety, efficiency, and long-term results. Future long-term follow-up RCT studies are necessary to determine the clinical outcomes between the RA and FA groups.
The advantages and disadvantages of robot-assisted PKP or PVP versus conventional fluoroscopic assistance in correcting kyphosis remain controversial. Robot-assisted PKP or PVP can provide more accurate placement of intravertebral guide pins, which can better correct vertebral deformities, the improvement rate of vertebral body kyphosis Cobb angle and vertebral body height after RA-PKP was significantly better than that of the conventional FA group [40]. However, some studies [22, 28] have also concluded that there is no significant difference between the two in improving kyphoscoliosis. Based on the results of our meta-analysis, we found that the Cobb angle in the RA group was significantly lower than that in the FA group at both 3 days and 1 month after surgery, which indicated that the RA group had a better surgical outcome than the FA group. However, in terms of vertebral midline height, there was no statistically significant difference between the RA group and the FA group within 3 days and after 1 month. There was a significant positive correlation between the amount of bone cement injected and the recovery of postoperative vertebral height. Specifically, we found that the higher the amount of bone cement injection, the better the recovery of postoperative vertebral body height [41]. Based on the results of our study, we did not observe a significant difference in the amount of bone cement injection between the two groups. This indicated that although there was a significant correlation between the amount of bone cement injection and postoperative vertebral height recovery, the level of postoperative correction of kyphosis and vertebral height recovery in both groups may be influenced by other factors. Further studies are needed to explore these factors in depth and to determine how they affect the outcome of spinal surgery.
In addition, further research is needed to explore the cost-effectiveness of robot-assisted PVA procedures. Some studies have shown significant cost-effectiveness in improving the accuracy of pedicle screws using RA technology [42, 43]. However, it is essential to strike a balance between the advantages and the expenses associated with integrating this technology into PKP or PVP procedures.
Limitations and prospects
This research has several limitations. Firstly, studies of robot-assisted treatment of OVCFs are mostly focused on non-randomized controlled trials, and more high-quality randomized controlled trials are needed in the future. Secondly, our meta-analysis only included studies from Asian countries. However, different countries and regions can also have an impact on the extent of disease and patient outcomes. Thirdly, there is a high degree of heterogeneity between studies, and different robot types and learning curves may cause risk of biases and potentially influence the results. Nevertheless, our study does elucidate promising results that provide a basis for future randomized controlled trials and prospective studies.
Conclusions
Our meta-analysis and systematic review found that the RA group had lower cement leakage rates, number of fluoroscopic and hospital stays, larger inclination angle, better short-term pain improvement, and Cobb angle improvement. But no significant differences in operation time, injection volume, Oswestry Disability Index, and the midline height of vertebral, and the RA and FA groups were similar in terms of postoperative pain relief at long-term follow-up. It is worth acknowledging that robot-assisted surgery holds promise for the development of spine surgery, but further validation of the safety and efficacy of the robot is still needed. More high-quality prospective studies and RCTs are needed in the future to update and refine the results of this analysis.
Data availability
The data sets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- OVCFs:
-
Osteoporotic vertebral compression fractures
- PVA:
-
Percutaneous vertebral augmentation
- PKP:
-
Percutaneous kyphoplasty
- PVP:
-
Percutaneous vertebroplasty
- RA:
-
Robot-assisted
- FA:
-
Fluoroscopy-assisted
- BMI:
-
Body mass index
- BMD:
-
Bone mineral density
- VAS:
-
Visual analog scale
- ODI:
-
Oswestry disability index
- RCT:
-
Randomized controlled trial
- WMD:
-
Weighted mean difference
- SMD:
-
Standardized mean difference
- CI:
-
Confidence interval
- OR:
-
Odds ratio
- CT:
-
Computed tomography
- M–H:
-
Mantel–Haenszel
- IV:
-
Inverse variance
- df:
-
Degrees of freedom
References
Patel D, Liu J, Ebraheim NA (2022) Managements of osteoporotic vertebral compression fractures: a narrative review. World J Orthop 13:564–573. https://doi.org/10.5312/wjo.v13.i6.564
Qin J, Zhong W, Quan Z (2022) The surgical management trends of osteoporotic vertebral compression fractures: 5-year experience in one institution. Sci Rep 12:18040. https://doi.org/10.1038/s41598-022-23106-y
Long Y, Yi W, Yang D (2020) Advances in vertebral augmentation systems for osteoporotic vertebral compression fractures. Pain Res Manag 2020:3947368. https://doi.org/10.1155/2020/3947368
Ren H, Feng T, Cao J et al (2022) A retrospective study to evaluate the effect of dynamic fracture mobility on cement leakage in percutaneous vertebroplasty and percutaneous kyphoplasty in 286 patients with osteoporotic vertebral compression fractures. Med Sci Monit 28:e935080. https://doi.org/10.12659/MSM.935080
Patel S, Chiu RG, Chaker AN et al (2022) Current trends and socioeconomic disparities in the utilization of spine augmentation for patients with osteoporotic vertebral compression fracture: a nationwide inpatient sample analysis from 2012 to 2016. Int J Spine Surg 16:490–497. https://doi.org/10.14444/8262
Lopez IB, Benzakour A, Mavrogenis A et al (2023) Robotics in spine surgery: systematic review of literature. Int Orthop 47:447–456. https://doi.org/10.1007/s00264-022-05508-9
Qian J, Fang C, Ge P et al (2022) Efficacy and safety of establishing an optimal path through unilateral pedicle under the assistance of surgical robot in percutaneous kyphoplasty. Pain Physician 25:E133–E140
Huang J, Xing T, Cheng Z et al (2022) AOSRV: development and preliminary performance assessment of a new robotic system for autonomous percutaneous vertebroplasty. Int J Med Robot 18:e2456. https://doi.org/10.1002/rcs.2456
Yuan W, Cao W, Meng X et al (2020) Learning curve of robot-assisted percutaneous kyphoplasty for osteoporotic vertebral compression fractures. World Neurosurg 138:e323–e329. https://doi.org/10.1016/j.wneu.2020.02.110
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med 18:e1003583. https://doi.org/10.1371/journal.pmed.1003583
Faiz KW (2014) VAS–visual analog scale. Tidsskr Nor Laegeforen 134:323. https://doi.org/10.4045/tidsskr.13.1145
Fairbank JC, Pynsent PB (2000) The Oswestry disability index. Spine Phila Pa (1976) 25:2940–2952. https://doi.org/10.1097/00007632-200011150-00017
Sterne JAC, Savovic J, Page MJ et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Sterne JA, Hernan MA, Reeves BC et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355:i4919. https://doi.org/10.1136/bmj.i4919
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21:1539–1558. https://doi.org/10.1002/sim.1186
Yuan W, Meng X, Cao W et al (2022) Robot-assisted versus fluoroscopy-assisted kyphoplasty in the treatment of osteoporotic vertebral compression fracture: a retrospective study. Global Spine J 12:1151–1157. https://doi.org/10.1177/2192568220978228
Wang B, Cao J, Chang J et al (2021) Effectiveness of Tirobot-assisted vertebroplasty in treating thoracolumbar osteoporotic compression fracture. J Orthop Surg Res 16:65. https://doi.org/10.1186/s13018-021-02211-0
Sun T, Zhang YZ, Hu XF et al (2022) Feasibility analysis of bi-planar fluoroscopic imaging robot assisted PKP in the treatment of osteoporotic vertebral compression fractures. Orthop Biomech Mater Clin Study 19:27–31. https://doi.org/10.3969/j.issn.1672-5972.2022.03.005
Lin S, Tan K, Hu J et al (2022) Effectiveness of modified orthopedic robot-assisted percutaneous kyphoplasty in treatment of osteoporotic vertebral compression fracture. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 36:1119–1125. https://doi.org/10.7507/1002-1892.202204013
Li Q, Wu C, Huang Z et al (2022) A comparison of robot-assisted and fluoroscopy-assisted kyphoplasty in the treatment of multi-segmental osteoporotic vertebral compression fractures. J Biomed Res 36:208–214. https://doi.org/10.7555/JBR.36.20220023
Jin M, Ge M, Lei L et al (2022) Clinical and radiologic outcomes of robot-assisted kyphoplasty versus fluoroscopy-assisted kyphoplasty in the treatment of osteoporotic vertebral compression fractures: a retrospective comparative study. World Neurosurg 158:e1–e9. https://doi.org/10.1016/j.wneu.2021.10.066
Zheng BL, Hao DJ, Lin B et al (2021) Puncture assisted by a “TINAVI” orthopaedic robot versus freehand puncture in vertebroplaty for osteoporotic vertebral compression fracture of the upper thoracic vertebra. Chin J Orthop Trauma 23:20–26
Zhang ZT, Zhang XH, Wei ZH et al (2018) Comparison of outcomes of robot assisted and conventional percutaneous vertebroplasty on osteoporotic vertebral compression fracture. J Clin Orthop Res 3:205–208
Yang N, Wang SB, Liu SF et al (2022) Effectiveness of robot-assisted percutaneous vertebroplasty for osteoporotic vertebral compression fracture in the elderly. West China Med J 37:1471–1475. https://doi.org/10.7507/1002-0179.202108283
Xie HQ, Li XK, Sun J et al (2021) Percutaneous vertebroplasty with robotic orthopedic assistance versus conventional fluoroscopy assistance for treatment of osteoporotic vertebral compression fractures: a clinical comparative study. Guangdong Med J 42:1102–1106
Tan L, Wen B, Guo Z et al (2023) Robot-assisted percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a retrospective matched-cohort study. Int Orthop 47:595–604. https://doi.org/10.1007/s00264-022-05654-0
Shi B, Hu L, Du H et al (2021) Robot-assisted percutaneous vertebroplasty under local anaesthesia for osteoporotic vertebral compression fractures: a retrospective, clinical, non-randomized, controlled study. Int J Med Robot 17:e2216. https://doi.org/10.1002/rcs.2216
Guo S, Fu Q, Hang DH et al (2021) Effectiveness of Mazor spine robot -assisted percutaneous vertebroplasty with modified approach in treating lumbar osteoporotic vertebral compression fractures. Chin J Spine Spinal Cord 31:818–824. https://doi.org/10.3969/j.issn.1004-406X.2021.09.06
Zhang K, She J, Zhu Y et al (2021) Risk factors of postoperative bone cement leakage on osteoporotic vertebral compression fracture: a retrospective study. J Orthop Surg Res 16:183. https://doi.org/10.1186/s13018-021-02337-1
Tang B, Cui L, Chen X et al (2021) Risk factors for cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: an analysis of 1456 vertebrae augmented by low-viscosity bone cement. Spine (Phila Pa 1976) 46:216–222. https://doi.org/10.1097/BRS.0000000000003773
Li M, Zhang T, Zhang R et al (2023) Systematic retrospective analysis of risk factors and preventive measures of bone cement leakage in percutaneous kyphoplasty. World Neurosurg 171:e828–e836. https://doi.org/10.1016/j.wneu.2022.12.117
Wang L, Li C, Wang Z et al (2023) Comparison of robot-assisted versus fluoroscopy-assisted minimally invasive transforaminal lumbar interbody fusion for degenerative lumbar spinal diseases: 2-year follow-up. J Robot Surg 17:473–485. https://doi.org/10.1007/s11701-022-01442-5
Lin S, Wang F, Hu J et al (2022) Comparison of the accuracy and safety of TiRobot-assisted and fluoroscopy-assisted percutaneous pedicle screw placement for the treatment of thoracolumbar fractures. Orthop Surg 14:2955–2963. https://doi.org/10.1111/os.13504
Probst T, Akalin ER, Giannouchos A et al (2022) Learning curves of robotic technology in an orthopedic teaching hospital. Orthopadie (Heidelb) 51:739–747. https://doi.org/10.1007/s00132-022-04287-w
Hijikata Y, Kotani Y, Suzuki A et al (2023) Protective attitudes toward occupational radiation exposure among spine surgeons in japan: an epidemiological description from the survey by the society for minimally invasive spinal treatment. Medicina (Kaunas). https://doi.org/10.3390/medicina59030545
Li J, Fang Y, Jin Z et al (2020) The impact of robot-assisted spine surgeries on clinical outcomes: a systemic review and meta-analysis. Int J Med Robot 16:1–14. https://doi.org/10.1002/rcs.2143
D’Souza M, Gendreau J, Feng A et al (2019) Robotic-assisted spine surgery: history, efficacy, cost, and future trends. Robot Surg 6:9–23. https://doi.org/10.2147/RSRR.S190720
Zhang RJ, Zhou LP, Zhang L et al (2022) Safety and risk factors of TINAVI robot-assisted percutaneous pedicle screw placement in spinal surgery. J Orthop Surg Res 17:379. https://doi.org/10.1186/s13018-022-03271-6
Matur AV, Palmisciano P, Duah HO et al (2023) Robotic and navigated pedicle screws are safer and more accurate than fluoroscopic freehand screws: a systematic review and meta-analysis. Spine J 23:197–208. https://doi.org/10.1016/j.spinee.2022.10.006
Alsalmi S, Capel C, Chenin L et al (2018) Robot-assisted intravertebral augmentation corrects local kyphosis more effectively than a conventional fluoroscopy-guided technique. J Neurosurg Spine 30:289–295. https://doi.org/10.3171/2018.8.SPINE18197
Song Q, Zhao Y, Li D et al (2023) Effect of different bone cement distributions in percutaneous kyphoplasty on clinical outcomes for osteoporotic vertebral compression fractures: a retrospective study. Medicine (Baltimore) 102:e33309. https://doi.org/10.1097/MD.0000000000033309
Garcia D, Akinduro OO, De Biase G et al (2022) Robotic-assisted vs nonrobotic-assisted minimally invasive transforaminal lumbar interbody fusion: a cost-utility analysis. Neurosurgery 90:192–198. https://doi.org/10.1227/NEU.0000000000001779
Soliman MAR, Pollina J, Poelstra K et al (2022) Can a spine robot be more efficient and less expensive while maintaining accuracy? Int J Spine Surg 16:S50–S54. https://doi.org/10.14444/8277
Acknowledgements
The authors acknowledged the Department of Statistics, Public Health College of Jilin University for their suggestions concerning the statistical analysis in this manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Q-sZ designed the study protocol. XW and Y-hZ managed the literature search and data acquisition. XW and Y-hZ performed the statistical analysis and drafted the manuscript. Q-sZ provided critical revision to the manuscript. Q-sZ resolved ambiguities during the study and gave final approval of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. All the authors have no conflict of interest to declare.
Informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, X., Zhu, Yh. & Zhu, Qs. Efficacy and safety of robot-assisted versus fluoroscopy-assisted PKP or PVP for osteoporotic vertebral compression fractures: a systematic review and meta-analysis. J Robotic Surg 17, 2597–2610 (2023). https://doi.org/10.1007/s11701-023-01700-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-023-01700-0