Abstract
This study was performed to prospectively compare the clinical and radiographic outcomes between robot-assisted minimally invasive transforaminal lumbar interbody fusion (RA MIS-TLIF) and fluoroscopy-assisted minimally invasive transforaminal lumbar interbody fusion (FA MIS-TLIF) in patients with degenerative lumbar spinal diseases. One hundred and twenty-three patients with lumbar degenerative diseases (lumbar spinal stenosis with instability and spondylolisthesis [degenerative spondylolisthesis or isthmic spondylolisthesis]) who underwent MIS-TLIF in our hospital were included in this study. Sixty-one patients underwent RA MIS-TLIF (Group A) and 62 patients underwent FA MIS-TLIF (Group B). Group A was further divided into Subgroup AI (46 single-level procedures) and Subgroup AII (15 double-level procedures). Group B was further divided into Subgroup BI (45 single-level procedures) and Subgroup BII (17 double-level procedures). The clinical outcome parameters were the visual analog scale (VAS) score, Oswestry Disability Index (ODI) score, operative time, number of intraoperative fluoroscopies, blood loss, postoperative hospital stay, and postoperative complications. The radiographic change measures were the accuracy of screw placement, facet joint violation (FJV), fusion status, and change in disc height at the proximal adjacent segment at the 2-year follow-up. There were no significant differences in the VAS and ODI scores, blood loss, or postoperative hospital stay between Groups A and B (p > 0.05). The operative time was longer in Group A than B (p = 0.018). The operative time was longer in Subgroup AI than BI (p = 0.001). However, there was no significant difference between Subgroups AII and BII (p > 0.05). There was no significant difference in the number of intraoperative fluoroscopies for patients between Groups A and B (p > 0.05). Although the number of intraoperative fluoroscopies for patients was significantly higher in Subgroup AI than BI (p = 0.019), there was no significant difference between Subgroups AII and BII (p > 0.05). The number of intraoperative fluoroscopies for the surgeon was significantly lower in Group A than B (p < 0.001). For surgeons, the difference in the average number of intraoperative fluoroscopies between Subgroups AI and AII was 2.98, but that between Subgroups BI and BII was 10.73. In Group A, three guide pins exhibited drift and one patient developed a lateral wall violation by a pedicle screw. One pedicle screw perforated the anterior wall of the vertebral body and another caused an inner wall violation in Group B. The rate of a perfect screw position (grade A) was higher in Group A than B (p < 0.001). However, there was no significant difference in the proportion of clinically acceptable screws (grades A and B) between the two groups. The mean FJV grade was significantly higher in Group B than A (p < 0.001). During at 2-year postoperative follow-up, there was no significant difference in the fusion status between the two groups (p > 0.05); however, the decrease in disc height at the proximal adjacent segment was significantly less in Group A than B (p < 0.001). Robot-assisted percutaneous pedicle screw placement is a safer and more accurate alternative to conventional freehand fluoroscopy-assisted percutaneous pedicle screw insertion in MIS-TLIF.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Harms and Rolinger [1] first reported transforaminal lumbar interbody fusion (TLIF) in 1982. As a development of TLIF, Foley and Lefkowitz [2] first described minimally invasive TLIF (MIS-TLIF) to reduce the incidence and severity of intraoperative paraspinal muscle injury. Compared with conventional open TLIF, MIS-TLIF has demonstrated less intraoperative blood loss, shorter hospitalization, earlier rehabilitation, fewer complications, less initial postoperative pain, and less analgesic medication use with similar clinical outcomes and fusion rates [3,4,5].
Percutaneous pedicle screw fixation plays a vital role in the clinical results of MIS-TLIF. Misplaced percutaneous pedicle screws may cause visceral injuries, neurological deficits, and adjacent segmental degeneration [6,7,8]. Until now, the freehand fluoroscopy-guided method has remained the principal method for pedicle screw insertion [9]. In recent years, there has been explosive growth in navigation, imaging, and robot-assisted technologies in spine surgery, especially in minimally invasive spine surgery [10]. Computer-assisted image guidance systems were first described in 1995 as computed tomography (CT)-based navigation systems [11]. Thereafter, intraoperative CT and three-dimensional C-arm were also used for navigation assistance in spine surgery [12]. With the use of navigation systems, the accuracy of pedicle screw placement has improved significantly compared with freehand techniques or C-arm fluoroscopic guidance [13]. The first robotic guidance system was described in 2004 [14]. The robotic guidance unit is mounted directly onto the patient’s bony anatomy (e.g., spinous process, iliac crest) and directly indicates preoperatively planned trajectories maneuvered after an automated registration process between the patient’s location relative to the robotic guidance unit [15]. No intraoperative radiation exposure is necessary once the registration process is completed at the beginning of the surgery. The advantages of robot-guided techniques include increased accuracy, shortened surgical time, and reduction of intraoperative radiation exposure for both patients and surgeons [16, 17].
This study was performed to compare the clinical outcomes and radiographic changes during 2 years of follow-up between robot-assisted percutaneous pedicle screw insertion and freehand fluoroscopy-assisted percutaneous pedicle screw insertion for patients undergoing MIS-TLIF.
Methods
Inclusion and exclusion criteria
This study was approved by the ethics committee of Qilu Hospital of Shandong University [KYLL-2021(KS)-055] and performed in accordance with the Helsinki Declaration. The inclusion criteria were lumbar degenerative diseases, including spondylolisthesis and lumbar spinal stenosis with instability (slip distance of > 5 mm or range of motion of > 10° on flexion and extension radiographs), and the requirement for interbody fusion and pedicle fixation. The exclusion criteria were a history of lumbar surgery, pure lumbar disc herniation without bony spinal canal stenosis, and any other neurological lesions or diseases that might affect precise preoperative and postoperative clinical assessments. Written informed consent was obtained from all patients before enrollment.
Patients’ characteristics
The patients with surgical indications for lumbar degenerative disease from 2019 to 2020 in our single institution were prospectively enrolled. Indication for surgery was made on the basis of the correlating clinical symptoms and the evidence on recent plain radiography, computed tomography, and magnetic resonance imaging. Prior to surgery, it was decided to perform MIS-TLIF either in the way using a robotic navigation, or by way of the freehand technique. These 2 described techniques were alternated regularly between each consecutive week. Therefore, each consecutive week patients received only one from the described techniques. All surgical procedures were performed by a same surgical team.
Surgical procedures
Robot-assisted MIS-TLIF (RA MIS-TLIF) procedure
RA MIS-TLIF at L4/5 is described in brief as an example of this surgical procedure. Implantation of percutaneous pedicle screws was assisted by a spinous process-mounted miniature device (TiRobot; TINAVI Medical Technologies Co., Ltd., Beijing, China). The three-dimensional images were acquired by a C-arm scanner (Siemens Healthineers, Erlangen, Germany), and registration was performed via automatic recognition using the calibrator. Screw trajectories were planned on the TiRobot, which included the optimal positioning and dimensions of the implants in the axial, coronal, and sagittal views. Next, the robot steered toward the chosen trajectory and indicated the entry point and direction of the pedicle screw trajectory. The surgeons drilled the guide pin through the guiding tube into the bilateral pedicles percutaneously. A skin incision (about 2.5 cm long) was made between L4 and L5 K-wires on the left side. Serial dilators were consecutively passed to split the paraspinous muscles, and a minimally invasive retractor of appropriate size was placed to expose the L4/5 facet joint. Next, the facet joint and hypertrophied ligamentum flavum at the fusion segment were removed for complete decompression. The intervertebral discs and cartilage endplate were then removed, and interbody fusion with bone chips and a cage were performed. Finally, the cannulated pedicle screws were inserted through K-wires, and the set screws were placed and given a final tightening. Figure 1 illustrates the operative technique.
Fluoroscopy-assisted MIS-TLIF (FA MIS-TLIF) procedure
Freehand FA MIS-TLIF at L4/5 is described in brief as an example of this surgical procedure. With use of fluoroscopic C-arm guidance, Jamshidi needles were inserted into the bilateral L4 and L5 pedicles with a freehand technique, and K-wires were then inserted through the needles. The rest of the procedure was identical to RA MIS-TLIF.
Assessment of clinical outcomes
The visual analog scale (VAS) score for back pain and leg pain and the Oswestry Disability Index (ODI) score were evaluated preoperatively and 3 days and 2 years postoperatively. The mean VAS and ODI scores were compared between the two groups. The operative time, number of intraoperative fluoroscopies, blood loss, postoperative hospital stay, and postoperative complications related to the surgeries were investigated and compared.
Assessment of radiographic changes
The accuracy of screw placement was assessed on postoperative CT. The pedicle screw positions were assessed with the Gertzbein and Robbins scale [16, 18]. Each screw position was classified as grade A (screw completely within the pedicle), grade B (pedicle cortical breach of < 2 mm), grade C (pedicle cortical breach of ≥ 2 to < 4 mm), grade D (pedicle cortical breach of ≥ 4 to < 6 mm), or grade E (pedicle cortical breach of ≥ 6 mm) (Fig. 2). Grade A and B screw positions were considered clinically acceptable, while all other grades indicated misplacement.
Computed tomography scans demonstrating the Gertzbein and Robbins classification. Grade A, screw completely within the pedicle; Grade B, pedicle cortical breach of < 2 mm; Grade C, pedicle cortical breach of ≥ 2 to < 4 mm; Grade D, pedicle cortical breach of ≥ 4 to < 6 mm; and Grade E, pedicle cortical breach of ≥ 6 mm
Postoperative superior facet joint violation (FJV) was assessed according to Babu et al. [19], and the degree of violation was classified into four grades (Fig. 3).
Disc degeneration at the proximal adjacent segment was evaluated by measurement of the disc height in the lateral standing X‐ray image preoperatively and 2 years postoperatively; the 2-year postoperative results were compared with the preoperative values. Disc height was measured using the modified method described by Son et al. [20] (Fig. 4).
The fusion status (interbody fusion) was graded by two methods using X‐ray examination at 2 years postoperatively. Each level and each side were judged individually. Interbody fusion was graded by the Brantigan, Steffee, and Fraser (BSF) classification outlined in Table 1 [21, 22].
Statistical analysis
Statistical analyses were performed using SPSS version 25.0 (IBM Corp., Armonk, NY, USA). All continuous data are expressed as mean ± standard deviation. Differences between the two groups were determined by the independent-sample T test. The Chi-square test was performed to analyze categorical variables. The significance level was set to be 0.05.
Results
Patient population
In total, 123 patients were included in the current study. Group A comprised 61 patients treated with robot-assisted MIS-TLIF (RA MIS-TLIF) (16 men, 45 women; average age, 57.46 years). Group A was further divided into Subgroup AI (single-level RA MIS-TLIF, n = 46) and Subgroup AII (double-level RA MIS-TLIF, n = 15). Group B comprised 62 patients treated with fluoroscopy-assisted MIS-TLIF (FA MIS-TLIF) (21 men, 41 women; average age, 57.69 years). Group B was further divided into Subgroup BI (single-level FA MIS-TLIF, n = 45) and Subgroup BII (double-level FA MIS-TLIF, n = 17). The patients’ characteristics are summarized in Table 2. There were no significant differences in age, sex, or body mass index between the two groups. All patients were followed up for 2 years postoperatively.
Clinical outcomes
Perioperative clinical results
The operative time was significantly longer in Group A than in Group B (p = 0.018). The operative time was also significantly longer in Subgroup AI than in Subgroup BI (p = 0.001), but there was no significant difference between Subgroup AII and Subgroup BII (p > 0.05). There was no significant difference in blood loss or the postoperative hospital stay between Group A and Group B (p > 0.05).
There was no significant difference in the number of intraoperative fluoroscopies for patients between Group A and Group B (p > 0.05). Although the number of intraoperative fluoroscopies for patients was significantly higher in Subgroup AI than in Subgroup BI (p = 0.019), there was no significant difference between Subgroup AII and Subgroup BII (p > 0.05). The number of intraoperative fluoroscopies for the surgeon was significantly lower in Group A than in Group B (p < 0.001). For surgeons, the difference in the average number of intraoperative fluoroscopies between Subgroup AI and Subgroup AII was 3.08, but that between Subgroup BI and Subgroup BII was 10.47.
Two-year follow-up
There were no significant differences in the VAS score for back and leg pain or the ODI score preoperatively between Group A and Group B (p > 0.05). In both Group A and Group B, postoperative back and leg pain and the ODI score were significantly improved (p < 0.05). There were no significant differences in the VAS score for back and leg pain or the ODI score at 3 days postoperatively or at the 2-year follow-up between Group A and Group B (p > 0.05). All the clinical results are shown in Tables 2 and 3.
Radiographic changes and related complications
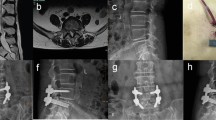
A detailed listing of the pedicle screw placement accuracy grades is provided in Table 3. The rate of perfect screw position (grade A) was higher in Group A (85.4%) than in Group B (69.5%; p < 0.001). However, there was no significant difference in the proportion of clinically acceptable screws (grades A and B) between the two groups (97.1% and 95.0%; p > 0.05). The mean grade of FJV in Group B was significantly higher than that in Group A (p < 0.001). At the 2-year postoperative lumbar CT examination, the decrease in disc height at the proximal adjacent segment was significantly less in Group A than in Group B (p < 0.001). In addition, there was no significant difference in the interbody fusion status between Group A and Group B (p > 0.05). All the radiographic changes are shown in Tables 4 and 5. A patient undergoing RA MIS-TLIF and a patient undergoing FA MIS-TLIF are shown in Figs. 5 and 6.
The patient was diagnosed with L4 spondylolisthesis, and RA MIS-TLIF was performed. The anteroposterior and lateral X-ray of the entire spine, the flexion–extension X-ray of the lumbar spine, computed tomography and magnetic resonance imaging of the lumbar spine at pre-operation (a–g). The anteroposterior and lateral X-ray and computed tomography of the lumbar spine at immediately post-operation (h–j). The anteroposterior and lateral X-ray and the flexion–extension X-ray image at 2-year follow-up (k–n)
The patient was diagnosed with L4 spondylolisthesis, and FA MIS-TLIF was performed. The anteroposterior and lateral X-ray of the entire spine, the flexion–extension X-ray of the lumbar spine, computed tomography and magnetic resonance imaging of the lumbar spine at pre-operation (a–g). The anteroposterior and lateral X-ray and computed tomography of the lumbar spine at immediately post-operation (h–j). The anteroposterior and lateral X-ray and the flexion–extension X-ray image at 2-year follow-up (k–n)
In Group A, three guide pins exhibited drift and one patient developed a lateral wall violation by a pedicle screw. All these phenomena were adjusted accordingly during the surgery. One pedicle screw perforated the anterior wall of the vertebral body in Group B, and this was adjusted during the surgery; however, the patient experienced abdominal pain for 3 days. In addition, an inner wall violation by a pedicle screw occurred in Group B, which irritated the exiting nerve root and required immediate surgical revision. Aside from the above, no other complications were reported in either group.
Discussion
Clinical outcomes
Previous studies have shown the great clinical effects of robot-assisted percutaneous pedicle screw insertion in TLIF [16, 23, 24]. In the present series, the VAS and ODI scores at the 2-year follow-up were significantly lower than the preoperative scores in both Group A and Group B. There was no significant difference between the two groups at the 2-year follow-up. In addition, there was no significant difference in blood loss or the postoperative hospital stay between the two groups.
The operative time was longer in Group A than in Group B. The increase in surgical time in Group A can be partly attributed to the learning curve of robot-assisted surgery and the intraoperative preparation phase. However, there was no significant difference between Subgroup AII and Subgroup BII, and even the average operative time was shorter in Subgroup AII than in Subgroup BII. This may indicate that a longer operation segment is associated with a higher efficiency of using robot assistance.
Spinal surgery is 10 to 12 times more radioactive than non-spinal surgery; therefore, an important goal of robotic research is to reduce radiation exposure for both patients and surgeons [25]. The difference between minimally FA RA-MIS-TLIF and purely FA MIS-TLIF was only the use of robot assistance in the process of pedicle screw placement. Recent studies have shown that the use of robot navigation in minimally invasive surgery can significantly reduce radiation exposure and residence time [16, 26]. In the present study, the radiation exposure for spinal surgeons was significantly lower in Group A than in Group B, and the medical staff left the room during the robot scanning and imaging, effectively reducing the radiation exposure. In addition, the number of intraoperative fluoroscopies for patients was significantly higher in Subgroup AI than in Subgroup BI, but there was no significant difference between Subgroup AII and Subgroup BII. Comprehensive analysis of the above results demonstrated that compared with FA MIS-TLIF, a longer operation segment was associated with less radiation exposure for patients and surgeons in RA MIS-TLIF.
Accuracy of screw placement
The success of spinal pedicle screw fixation mainly depends on the accuracy of screw placement. High screw accuracy restores the normal curvature of the spine and thus maintains stability. Recent studies have suggested that the use of robotic guidance significantly increases the accuracy of screw placement [16, 27,28,29,30]. Lieberman and Phillips [31, 32] also demonstrated that robot-assisted percutaneous pedicle screw placement had fewer cortical breaches and screw placement deviations than freehand screw placement. The present study showed that the accuracy of robot-assisted percutaneous pedicle screw insertion was significantly higher than that of freehand fluoroscopy-assisted percutaneous pedicle screw insertion, which is consistent with some previous studies. In addition, the related complications were less in Group A.
However, robot navigation does not mean 100% accuracy. In this study, three guide pins exhibited drift and one patient developed a lateral wall violation by a pedicle screw in robot-assisted group. Some studies have shown that insertion of the guide wire through the skin may result in drift on the bone surface, which may lead to an inaccurate drilling process [33]. To minimize this risk, we inserted the cannula and rotated the guide wire prior to bone contact to enter the pedicle on a preset trajectory. It is also critical to improve the accuracy of pedicle placement by controlling the tidal volume and reducing intraoperative lumbar and back movement during robot navigation. Overall, the TiRobot can improve the accuracy and safety of percutaneous pedicle screw placement.
FJV and adjacent segment disease
Since FJV is closely associated with long-term adjacent segment disease complications, its avoidance during surgery has important clinical value. Previous reports have described a grading system for this phenomenon: if any part of the screw, tulip, or connecting rod is clearly within the facet joint or within 1 mm of the joint, the facet joint is considered violated [19, 34]. Previous studies have suggested that the incidence of FJV ranges from 9.5 to 32.0% of screws [19, 35,36,37]. A recent study showed that the incidence and grade of proximal FJV in robot-assisted percutaneous pedicle screw insertion were lower than those in fluoroscopic-guided pedicle screw placement [38]. In this study, the FJV grade was significantly lower in the robot-assisted percutaneous group than in the freehand fluoroscopy-assisted percutaneous group. This difference can be explained by the mechanism of intraoperative robotic guidance. Babu et al. [19] suggested that the FJV grade was higher for freehand fluoroscopy-assisted percutaneous pedicle screw insertion because it depended on radiographic and limited tactile feedback for determination of the screw entry site and trajectory. In contrast, the robotic system mechanically guides the surgeons to the preplanned trajectory and provides three-dimensional images. The screw insertion point was relatively lateral in the robot-assisted group of our study, which reduced the occurrence of FJV. In addition, the soft tissue resistance of percutaneous guide pin insertion via the robotic arm was less than that of the freehand technique. Therefore, the FJV grade was significantly lower in the robot-assisted percutaneous group than in the freehand fluoroscopy-assisted percutaneous group. However, because of the lack of real-time dynamic monitoring in the first-generation robot system, deep implantation of some screws is an important cause of FJV. Related studies have shown that tulip violation also damages biomechanical structures of the facet joint, and such a situation should be carefully avoided during surgery [39]. Therefore, the screws should not be inserted too deeply during percutaneous screw placement. A proper distance between the tulip and superior facet joint is the key to preventing the tulip from impinging on the articular process.
There is increasing focus on the impact of the top of the construct screws on the development of post-fusion adjacent segment disease [40, 41]. Previous studies have suggested that violation of adjacent facet joints by pedicle screw insertion may be a large contributor to ASD [39, 42]. The destruction of the proximal facet will affect the stability of the spine, thus accelerating the degeneration and development of lesions of adjacent segments of the disc [43]. Kim et al. [23] found that the decrease in disc height at the proximal adjacent segment was significantly less in the robot-assisted group than in the freehand fluoroscopy-assisted group (p = 0.039). In this study, because the FJV grade in the robot-assisted group was significantly lower than that in the freehand fluoroscopy-assisted group, the decrease in disc height at the proximal adjacent segment was significantly less in Group A than in Group B during the 2-year follow-up.
Interbody fusion
Accurate radiographic assessment of fusion success is important to identify patients who might benefit from further surgery. Fusion assessment with plain X-ray films and helical CT scans showed equal accuracy after posterior lumbar interbody fusion confirmed by surgical exploration [22]. In the present study, both groups showed similar radiological fusion rates on X-ray at the 2-year follow-up after surgery, which is similar to the findings of previous studies. Chang et al. [24] found no significant difference in the fusion rate between the robot-assisted percutaneous fully endoscopic group and freehand fluoroscopy-assisted group. Kim et al. [23] also found no significant difference in the fusion rate at 1 year after surgery between the robot‐assisted and freehand posterior lumbar interbody fusion groups.
Limitations
This study has three main limitations. First, this study was conducted at a single center and included a relatively small number of patients. The sample size will be increased in the follow-up study to improve the accuracy of the results. Second, only patients who underwent single-level and double-level lumbar surgery were included in this study; longer surgical segments are needed to confirm the findings.
Conclusion
Robot-assisted percutaneous pedicle screw placement is a safer and more accurate alternative to conventional freehand fluoroscopy-assisted percutaneous pedicle screw insertion in MIS-TLIF. Compared with freehand fluoroscopy-assisted percutaneous pedicle screw insertion, a longer operation segment is associated with better clinical outcomes in robot-assisted percutaneous pedicle screw placement.
Data availability
All data available for this study were reported in the manuscript.
Code availability
Not applicable.
References
Harms J, Rolinger H (1982) A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author’s transl). Z Orthop Ihre Grenzgeb 120:343–347. https://doi.org/10.1055/s-2008-1051624
Foley KT, Lefkowitz MA (2002) Advances in minimally invasive spine surgery. Clin Neurosurg 49:499–517
Goldstein CL, Macwan K, Sundararajan K, Rampersaud YR (2014) Comparative outcomes of minimally invasive surgery for posterior lumbar fusion: a systematic review. Clin Orthop Relat Res 472:1727–1737. https://doi.org/10.1007/s11999-014-3465-5
Jin-Tao Q, Yu T, Mei W, Xu-Dong T, Tian-Jian Z, Guo-Hua S, Lei C, Yue H, Zi-Tian W, Yue Z (2015) Comparison of MIS vs. open PLIF/TLIF with regard to clinical improvement, fusion rate, and incidence of major complication: a meta-analysis. Eur Spine J 24:1058–1065. https://doi.org/10.1007/s00586-015-3890-5
Khan NR, Clark AJ, Lee SL, Venable GT, Rossi NB, Foley KT (2015) surgical outcomes for minimally invasive vs open transforaminal lumbar interbody fusion: an updated systematic review and meta-analysis. Neurosurgery 77:847–874; discussion 874. https://doi.org/10.1227/NEU.0000000000000913
Jutte PC, Castelein RM (2002) Complications of pedicle screws in lumbar and lumbosacral fusions in 105 consecutive primary operations. Eur Spine J 11:594–598. https://doi.org/10.1007/s00586-002-0469-8
Katonis P, Christoforakis J, Kontakis G, Aligizakis AC, Papadopoulos C, Sapkas G, Hadjipavlou A (2003) Complications and problems related to pedicle screw fixation of the spine. Clin Orthop Relat Res. https://doi.org/10.1097/01.blo.0000068761.86536.1d
Fan Y, Du JP, Zhang JN, Liu SC, Xue XK, Huang YF, Zhang J, Hao D (2017) Comparison of accuracy of pedicle screw insertion among 4 guided technologies in spine surgery. Med Sci Monit 23:5960–5968. https://doi.org/10.12659/Msm.905713
Fan Y, Du JP, Liu JJ, Zhang JN, Qiao HH, Liu SC, Hao DJ (2018) Accuracy of pedicle screw placement comparing robot-assisted technology and the free-hand with fluoroscopy-guided method in spine surgery: an updated meta-analysis. Medicine (Baltimore) 97:e10970. https://doi.org/10.1097/MD.0000000000010970
D’Souza M, Gendreau J, Feng A, Kim LH, Ho AL, Veeravagu A (2019) Robotic-assisted spine surgery: history, efficacy, cost, and future trends. Robot Surg 6:9–23. https://doi.org/10.2147/RSRR.S190720
Nolte LP, Zamorano L, Visarius H, Berlemann U, Langlotz F, Arm E, Schwarzenbach O (1995) Clinical evaluation of a system for precision enhancement in spine surgery. Clin Biomech (Bristol, Avon) 10:293–303. https://doi.org/10.1016/0268-0033(95)00004-5
Park P, Foley KT, Cowan JA, Marca FL (2010) Minimally invasive pedicle screw fixation utilizing O-arm fluoroscopy with computer-assisted navigation: feasibility, technique, and preliminary results. Surg Neurol Int 1:44. https://doi.org/10.4103/2152-7806.68705
Tian NF, Huang QS, Zhou P, Zhou Y, Wu RK, Lou Y, Xu HZ (2011) Pedicle screw insertion accuracy with different assisted methods: a systematic review and meta-analysis of comparative studies. Eur Spine J 20:846–859. https://doi.org/10.1007/s00586-010-1577-5
Wolf A, Shoham M, Michael S, Moshe R (2004) Feasibility study of a mini, bone-attached, robotic system for spinal operations: analysis and experiments. Spine (Phila Pa 1976) 29:220–228. https://doi.org/10.1097/01.BRS.0000107222.84732.DD
Fujishiro T, Nakaya Y, Fukumoto S, Adachi S, Nakano A, Fujiwara K, Baba I, Neo M (2015) Accuracy of pedicle screw placement with robotic guidance system: a cadaveric study. Spine (Phila Pa 1976) 40:1882–1889. https://doi.org/10.1097/BRS.0000000000001099
Han X, Tian W, Liu Y, Liu B, He D, Sun Y, Han X, Fan M, Zhao J, Xu Y, Zhang Q (2019) Safety and accuracy of robot-assisted versus fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery: a prospective randomized controlled trial. J Neurosurg Spine. https://doi.org/10.3171/2018.10.SPINE18487
Kim HJ, Lee SH, Chang BS, Lee CK, Lim TO, Hoo LP, Yi JM, Yeom JS (2015) Monitoring the quality of robot-assisted pedicle screw fixation in the lumbar spine by using a cumulative summation test. Spine (Phila Pa 1976) 40:87–94. https://doi.org/10.1097/BRS.0000000000000680
Gertzbein SD, Robbins SE (1990) Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976) 15:11–14. https://doi.org/10.1097/00007632-199001000-00004
Babu R, Park JG, Mehta AI, Shan T, Grossi PM, Brown CR, Richardson WJ, Isaacs RE, Bagley CA, Kuchibhatla M, Gottfried ON (2012) Comparison of superior-level facet joint violations during open and percutaneous pedicle screw placement. Neurosurgery 71:962–970. https://doi.org/10.1227/NEU.0b013e31826a88c8
Son S, Lee SG, Kim WK, Ahn Y, Jung JM (2021) Disc height discrepancy between supine and standing positions as a screening metric for discogenic back pain in patients with disc degeneration. Spine J 21:71–79. https://doi.org/10.1016/j.spinee.2020.07.006
Selby MD, Clark SR, Hall DJ, Freeman BJ (2012) Radiologic assessment of spinal fusion. J Am Acad Orthop Surg 20:694–703. https://doi.org/10.5435/JAAOS-20-11-694
Fogel GR, Toohey JS, Neidre A, Brantigan JW (2008) Fusion assessment of posterior lumbar interbody fusion using radiolucent cages: X-ray films and helical computed tomography scans compared with surgical exploration of fusion. Spine J 8:570–577. https://doi.org/10.1016/j.spinee.2007.03.013
Kim HJ, Kang KT, Chun HJ, Hwang JS, Chang BS, Lee CK, Yeom JS (2018) Comparative study of 1-year clinical and radiological outcomes using robot-assisted pedicle screw fixation and freehand technique in posterior lumbar interbody fusion: a prospective, randomized controlled trial. Int J Med Robot 14:e1917. https://doi.org/10.1002/rcs.1917
Chang M, Wang L, Yuan S, Tian Y, Zhao Y, Liu X (2022) Percutaneous endoscopic robot-assisted transforaminal lumbar interbody fusion (PE RA-TLIF) for lumbar spondylolisthesis: a technical note and two years clinical results. Pain Phys 25:E73–E86
Ravi B, Zahrai A, Rampersaud R (2011) Clinical accuracy of computer-assisted two-dimensional fluoroscopy for the percutaneous placement of lumbosacral pedicle screws. Spine 36:84–91. https://doi.org/10.1097/BRS.0b013e3181cbfd09
Hyun SJ, Kim KJ, Jahng TA, Kim HJ (2017) Minimally invasive robotic versus open fluoroscopic-guided spinal instrumented fusions: a randomized controlled trial. Spine 42:353–358. https://doi.org/10.1097/brs.0000000000001778
Roser F, Tatagiba M, Maier G (2013) Spinal robotics: current applications and future perspectives. Neurosurgery 72:A12–A18. https://doi.org/10.1227/NEU.0b013e318270d02c
Hyun SJ, Kim KJ, Jahng TA, Kim HJ (2017) Minimally invasive robotic versus open fluoroscopic-guided spinal instrumented fusions a randomized controlled trial. Spine 42:353–358. https://doi.org/10.1097/Brs.0000000000001778
Kantelhardt S, Martinez R, Baerwinkel S, Burger R, Giese A, Rohde V (2011) Perioperative course and accuracy of screw positioning in conventional, open robotic-guided and percutaneous robotic-guided, pedicle screw placement. Eur Spine J 20:860–868. https://doi.org/10.1007/s00586-011-1729-2
Molliqaj G, Schatlo B, Alaid A, Solomiichuk V, Rohde V, Schaller K, Tessitore E (2017) Accuracy of robot-guided versus freehand fluoroscopy-assisted pedicle screw insertion in thoracolumbar spinal surgery. Neurosurg Focus 42:E14. https://doi.org/10.3171/2017.3.Focus179
Lieberman IH, Hardenbrook MA, Wang JC, Guyer RD (2012) Assessment of pedicle screw placement accuracy, procedure time, and radiation exposure using a miniature robotic guidance system. J Spinal Disord Tech 25:241–248. https://doi.org/10.1097/BSD.0b013e318218a5ef
Phillips FM (2009) Percutaneous placement of pedicle screws in the lumbar spine using a bone mounted miniature robotic system first experiences and accuracy of screw placement point of view. Spine 34:399–399. https://doi.org/10.1097/BRS.0b013e3181973450
Hu X, Ohnmeiss DD, Lieberman IH (2013) Robotic-assisted pedicle screw placement: lessons learned from the first 102 patients. Eur Spine J 22:661–666. https://doi.org/10.1007/s00586-012-2499-1
Moshirfar A, Jenis LG, Spector LR, Burke PJ, Losina E, Katz JN, Rand FF, Tromanhauser SG, Banco RJ (2006) Computed tomography evaluation of superior-segment facet-joint violation after pedicle instrumentation of the lumbar spine with a midline surgical approach. Spine (Phila Pa 1976) 31:2624–2629. https://doi.org/10.1097/01.brs.0000240691.35707.e8
Tian W, Xu YF, Liu B, Liu YJ, He D, Yuan Q, Lang Z, Lyu YW, Han XG, Jin PH (2014) Lumbar spine superior-level facet joint violations: percutaneous versus open pedicle screw insertion using intraoperative 3-dimensional computer-assisted navigation. Chin Med J 127:3852–3856. https://doi.org/10.3760/cma.j.issn.0366-6999.20141860
Park Y, Ha JW, Lee YT, Sung NY (2011) Cranial facet joint violations by percutaneously placed pedicle screws adjacent to a minimally invasive lumbar spinal fusion. Spine J 11:295–302. https://doi.org/10.1016/j.spinee.2011.02.007
Moshirfar A, Jenis LG, Spector LR, Burke PJ, Losina E, Katz JN, Rand FF, Tromanhauser SG, Banco RJ (2006) Computed tomography evaluation of superior-segment facet-joint violation after pedicle instrumentation of the lumbar spine with a midline surgical approach. Spine 31:2624–2629. https://doi.org/10.1097/01.brs.0000240691.35707.e8
Zhang Q, Xu YF, Tian W, Le XF, Liu B, Liu YJ, He D, Sun YQ, Yuan Q, Lang Z, Han XG (2019) Comparison of superior-level facet joint violations between robot-assisted percutaneous pedicle screw placement and conventional open fluoroscopic-guided pedicle screw placement. Orthop Surg 11:850–856. https://doi.org/10.1111/os.12534
Zhao Y, Yuan S, Tian Y, Liu X (2020) Risk factors related to superior facet joint violation during lumbar percutaneous pedicle screw placement in minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF). World Neurosurg 139:e716–e723. https://doi.org/10.1016/j.wneu.2020.04.118
Knox JB, Dai JM 3rd, Orchowski JR (2011) Superior segment facet joint violation and cortical violation after minimally invasive pedicle screw placement. Spine J 11:213–217. https://doi.org/10.1016/j.spinee.2011.01.024
Cheh G, Bridwell KH, Lenke LG, Buchowski JM, Daubs MD, Kim Y, Baldus C (2007) Adjacent segment disease following lumbar/thoracolumbar fusion with pedicle screw instrumentation: a minimum 5-year follow-up. Spine 32:2253–2257. https://doi.org/10.1097/BRS.0b013e31814b2d8e
Park P, Garton HJ, Gala VC, Hoff JT, McGillicuddy JE (2004) Adjacent segment disease after lumbar or lumbosacral fusion: review of the literature. Spine (Phila Pa 1976) 29:1938–1944. https://doi.org/10.1097/01.brs.0000137069.88904.03
Kim HJ, Kang KT, Park SC, Kwon OH, Son J, Chang BS, Lee CK, Yeom JS, Lenke LG (2017) Biomechanical advantages of robot-assisted pedicle screw fixation in posterior lumbar interbody fusion compared with freehand technique in a prospective randomized controlled trial-perspective for patient-specific finite element analysis. Spine J 17:671–680. https://doi.org/10.1016/j.spinee.2016.11.010
Acknowledgements
We thank Angela Morben, DVM, ELS, from Liwen Bianji (Edanz) (www.liwenbianji.cn), for editing the English text of a draft of this manuscript.
Funding
This work was supported in part by the National Natural Science Foundation of China (81874022 and 82172483 to Xinyu Liu; 82102522 to Lianlei Wang) and Natural Science Foundation of Shandong province (ZR202102210113 to Lianlei Wang).
Author information
Authors and Affiliations
Contributions
LW, CL, and ZW carried out the entire procedure including the study design, data extraction, statistical analysis, manuscript writing and editing. XL conceived of the study, coordinated and participated in the entire process of drafting and editing the manuscript. DL and YT contributed to the data extraction, literature reviewing and statistical analysis. SY contributed to the study design and data analysis. All the authors have contributed significantly. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Ethical approval
This study was approved by the ethics committee of Qilu Hospital of Shandong University [KYLL-2021(KS)-055] and performed according to the tenets of the Declaration of Helsinki.
Informed consent
Written informed consent was obtained from all the enrolled patients.
Consent for publication
The authors agree to publication. This manuscript has not been published in any journals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, L., Li, C., Wang, Z. et al. Comparison of robot-assisted versus fluoroscopy-assisted minimally invasive transforaminal lumbar interbody fusion for degenerative lumbar spinal diseases: 2-year follow-up. J Robotic Surg 17, 473–485 (2023). https://doi.org/10.1007/s11701-022-01442-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11701-022-01442-5