Abstract
Background
Roux-en-Y gastric bypass (RYGB) has been associated with negative effects on bone. Whether this association is affected by pre-surgical type 2 diabetes (T2D) and surgically induced diabetes remission is unknown.
Methods
In this cross-sectional, matched cohort study 6 years after RYGB, we investigated bone health in 96 individuals with body mass index (BMI) > 35 kg/m2 and T2D (stratified on current diabetes status) treated by RYGB 6 years earlier compared with 49 non-operated individuals with T2D matched with respect to sex, age, and current BMI. Main outcome measures were areal and volumetric bone mineral density (aBMD and vBMD), bone turnover, and odds ratio of osteoporosis/osteopenia.
Results
The RYGB group had lower hip (0.916 vs 1.010 g/cm2, p < 0.001), forearm (0.497 g/cm2 vs 0.554 g/cm2, p < 0.001) aBMD, (269.63 mg/cm3 vs 306.07 mg/cm3, p < 0.001) tibial, and radial (238.57 mg/cm3 vs 278.14 mg/cm3, p < 0.0001) vBMD than the control group. Relative to the control group, c-terminal cross-linked telopeptide, procollagen type I amino-terminal propeptide, and osteocalcin were 75%, 41%, and 72% higher in the RYGB group, respectively (all p < 0.001). Odds ratio for osteopenia/osteoporosis in operated individuals was 2.21 (95% CI 1.06; 4.79, p = 0.05). Overall, stratified analysis on current diabetes status did not alter these outcomes.
Conclusions
Individuals with T2D treated by RYGB, compared to individuals with T2D of similar age and body composition not treated by RYGB, have lower BMD, lower bone strength, and increased levels of several bone turnover markers. Bone health was not associated with current diabetes status in the RYGB group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Roux-en-Y gastric bypass (RYGB) is one of the most commonly performed bariatric procedures worldwide [1] and highly effective in the treatment of severe obesity, as well as resolution of obesity-related comorbidities such as type 2 diabetes mellitus (T2D), hypertension, and sleep apnea [2, 3]. However, evidence of negative effects of RYGB on bone health is emerging [4] and must be taken into consideration by patients and healthcare providers when considering RYGB.
Following RYGB, food bypasses a great part of the stomach and duodenum, as well as the proximal jejunum [5]. Therefore, the mixture of food with pancreatic enzymes and bile acids is delayed until distally in the small intestine, leading to decreased absorption of minerals (e.g., calcium) and fat-soluble vitamins (e.g., vitamin D) [6, 7]. In order to prevent inadequate absorption and negative effects on bone health, RYGB-operated individuals are advised life-long supplementation of vitamin D, calcium, iron, multivitamins, and vitamin B12 [8,9,10].
Human studies addressing bone health following RYGB have reported a decline in areal bone mineral density (aBMD) [4, 11,12,13,14], some [11] but not all [13] have reported secondary hyperparathyroidism, while several studies [4, 15] have reported increased bone turnover indicating bone loss following RYGB [4]. Only a few studies have evaluated bone health beyond 2 years following RYGB [11, 12], and with a few exceptions [13,14,15], previous studies have not evaluated individuals with pre-surgical T2D. This could be important since individuals with T2D display lower bone turnover and higher aBMD than individuals without T2D [16, 17]. Moreover, individuals with T2D have a higher fracture risk than individuals without T2D with identical aBMD [17, 18], indicating that aBMD may underestimate fracture risk in individuals with T2D. Because dual-energy X-ray absorptiometry (DXA) has a limited accuracy in individuals with obesity due to artifacts from unevenly distributed soft tissue [4, 19], an alternative way of evaluating bone structure is applying high-resolution peripheral quantitative computed tomography (HR-pQCT) [20], a method only applied in a few studies investigating bone health following RYGB [4, 21] and not previously in cohorts restricted to individuals with T2D.
Hence, the aim of this study was to investigate bone health applying DXA, HR-pQCT, and bone turnover markers in individuals with obesity and T2D treated by RYGB, and a non-operated matched control group. We hypothesized that RYGB individuals had lower aBMD and vBMD, impaired bone microarchitecture, lower estimated bone strength, and higher bone turnover than the matched control group, and that remission of T2D in the RYGB group to some extent could prevent the deterioration of bone health.
Materials and Methods
Participants
In this cross-sectional, matched cohort study, conducted February–November 2016, we examined 96 individuals with obesity and T2D treated by RYGB in the period 2006–2011, and a control group of 49 non-operated individuals with T2D and obesity matched with respect to sex, age, and BMI at the date of examination. The Danish National Board of Health provides the Danish population with tax-supported health care, including full payment of, e.g., bariatric surgery fulfilling specific criteria (BMI > 35 kg/m2 in the presence of T2D). We approached individuals registered with both a RYGB procedure and a T2D code via the Danish National Patients Registry [22] by letter. Detailed recruitment is shown in Fig. 1. We recruited the matched controls from the endocrine outpatient clinic at Aarhus University Hospital.
Flow chart of recruitment of the RYGB-operated individuals. Overall response rate was 67%. Individuals suffering from primary and tertiary hyperparathyroidism were excluded (n = 3), resulting in a cohort of 96 RYGB individuals. Abbreviations: RYGB, Roux-en-Y gastric bypass; T1D, type 1 diabetes mellitus; T2D, type 2 diabetes mellitus; Primary HP, primary hyperparathyroidism; Tertiary HP, tertiary hyperparathyroidism.
Clinical Examination and Blood Testing
After an overnight fast blood samples were obtained before 9 a.m. We measured height and weight without shoes and calculated BMI as weight divided by height squared. By questionnaire, we enquired data concerning maximum weight, weight loss, use of medication including vitamin supplements, diagnosis of diabetes, and smoking. Remission of T2D was defined as hemoglobinA1c (HbA1c) < 6.5% and no use of antidiabetic medication or HbA1c < 6.0% and use of metformin only [23, 24]. Calcium-ion, magnesium, HbA1c, and PTH were analyzed immediately according to accredited international standards. Additional blood was stored for batch analyses of phosphate, 25-hydroxy vitamin D (25OHD), sclerostin, osteocalcin, procollagen type I amino-terminal propeptide (PINP), bone-specific alkaline phosphatase (BAP), and c-terminal cross-linked telopeptide (CTX). All analyses were performed at Aarhus University Hospital, Denmark, except sclerostin analyses which were performed at Rigshospitalet, Denmark, using a Human Sclerostin EIA kit (TECOmedical, San Diego, CA). 25OHD was analyzed using isotope dilution liquid chromatography-tandem mass spectrometry (LS-MS/MS). Intact and N-terminal midfragment osteocalcin, CTX, and PINP were measured using an immunoassay on Cobas e601 (Roche Diagnostics, Penzberg, Germany). BAP was measured using an immunoassay on iSYS (IDS Ltd., Boldon, UK). The coefficients of variation (CV) were as follows: osteocalcin 3%, CTX 5%, PINP 3.7%, BAP 10%, and sclerostin < 10%.
Dual-Energy X-Ray Absorptiometry
aBMD and corresponding T-scores were measured by dual-energy X-ray absorptiometry (DXA) (Discovery A scanner; Hologic, USA) at the lumbar spine (L1–L4), total hip, and forearm (preferably left side) with NHANES data as reference [25]. CV of repositioning were 1.5% for lumbar spine aBMD and 2.1% for total hip aBMD [26, 27]. In addition, Vertebral Fracture Assessment (VFA) and whole-body DXA were performed. Osteopenia and osteoporosis were defined as lumbar spine and/or total hip T-scores < − 1.0 and ≤ − 2.5, respectively.
High-Resolution Peripheral Quantitative Computed Tomography
vBMD and microarchitecture of the distal radius and tibia (preferably left side) were assessed using high-resolution peripheral quantitative computed tomography (HR-pQCT) (XtremeCT; Scanco Medical, Switzerland) [28, 29]. CV of repositioning for radius and tibia density measures were 1 and 3–4% for the structural parameters [20]. Built-in standard evaluation software and finite element analysis software were used to assess bone density parameters (average, trabecular, and cortical vBMD), bone microarchitecture parameters (trabecular number, trabecular thickness, trabecular space, and cortical thickness), and to estimate bone stiffness (resistance to deformation) and failure load (the load needed to apply for the bone to break) [20].
Statistics
We compared the RYGB group with the non-operated control group using Student’s t test reporting means (standard deviation [SD]). Wilcoxon rank-sum (Mann–Whitney) test reporting medians (interquartile ranges [IQR]) or chi-squared test for categorical variables. By applying logistic regression, we calculated unadjusted and adjusted odds ratio (adjusting for menopause) for impaired bone health (osteopenia/osteoporosis). Difference in bone turnover markers was adjusted by applying a linear regression model, adjusting for pre-specified clinical relevant variables: HbA1c, 25OHD and PTH levels, use of calcium/vitamin D supplements, tobacco use, and menopausal status. Sample size was determined by participant response rate, but with 96 RYGB-operated individuals and 49 control patients, we would be able to detect a 10% difference in forearm average vBMD (SD 20%) with a power of 81%. When comparing RYGB-operated stratified in accordance with T2D and the non-operated group, one-way ANOVA with Bonferroni or Kruskal–Wallis ANOVA with Dunn’s test were applied. We considered two-tailed p value less than 0.05 significant. All calculations were made using Stata IC 13 (College Station, TX: StataCorp LP).
Results
Participant Characteristics
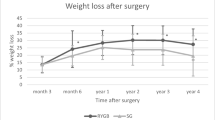
Characteristics of the RYGB group and the age-, sex-, and BMI-matched control group are shown in Table 1. Median time since RYGB was 6.1 years (IQR 5.4; 7.0). As expected, HbA1c was lower in the RYGB group than in the control group, owing to RYGB-induced improvement of hyperglycemia. Daily use of multivitamins (82 vs. 31%, p < 0.001) and vitamin D and calcium supplements (86 vs. 33%, p < 0.001) was higher in the RYGB group (Table 1).
Bone Density Measured by DXA
Figure 2 shows aBMD in the RYGB and control groups. Whole-body aBMD (1.061 g/cm2 [0.134] vs 1.116 g/cm2 [0.124], p = 0.019), aBMD at the total hip (0.916 g/cm2 [0.146] vs 1.010 g/cm2 [0.162], p < 0.001), total forearm (0.497 g/cm2 [0.084] vs 0.554 g/cm2 [0.064], p < 0.001), and distal third of forearm (0.623 g/cm2 [0.107] vs 0.698 g/cm2 [0.074], p < 0.001) were significantly lower in the RYGB group than in the non-operated group, whereas we found no difference at the lumbar spine (p = 0.141) and the ultra-distal forearm (p = 0.297) (Fig. 2). When stratifying the RYGB cohort on daily intake of recommended supplementation, we found no difference in aBMD between the compliant and non-compliant individuals. From DXA, we found that 33/95 in the RYGB group had osteopenia and 8/95 had osteoporosis. In contrast, 11/49 in the control group had osteopenia and 3/49 had osteoporosis (Supplementary Table 1). Thus, relative to the non-operated group, odds ratio of having osteopenia or osteoporosis in the RYGB group was 1.90 (95% CI 0.90; 3.98, p = 0.09), and 2.21 (95% CI 1.06; 4.79, p = 0.05) when adjusted for menopausal status (additional data shown in Supplementary Table 1). VFA did not identify any spinal fractures.
aBMD at lumbar spine, femoral, and forearm in the RYGB group (n = 95) and the non-operated control group (n = 49). Mean areal aBMD in the RYGB group (black diamonds) and the non-operated control group (gray-filled circles) with 95% confidence intervals for whole body, lumbar spine, total hip, total forearm, distal 1/3 of forearm (mainly cortical bone), and ultra-distal forearm (mainly trabecular bone). One of the RYGB-operated individuals did not complete the DXA.*p < 0.05. Abbreviations: RYGB, Roux-en-Y gastric bypass; aBMD, areal bone mineral density.
Bone Variables Measured by HR-pQCT
Total vBMD at the radius (238.57 mg/cm3 [63.0] vs 278.14 mg/cm3 [57.4], p < 0.0001) and at the tibia (269.63 mg/cm3 [51.5] vs 306.07 mg/cm3 [43.7], p < 0001) were lower in the RYGB group than in the control group (Table 2). In the radius, this difference was primarily due to a lower trabecular vBMD in the RYGB-operated group (Table 2). Especially in the radius, we found lower trabecular number (1.85 mm−1 [0.431] vs 2.10 mm−1 [0.321], p < .001) and trabecular thickness (0.059 mm [0.01] vs 0.067 mm [0.01], p < .001) with a reciprocal higher trabecular space (0.519 mm [0.175] vs 0.422 mm [0.087], p < 0.001) accompanied by lower, although not statistically significant, cortical thickness (0.59 mm [0.010] vs 0.67 mm [0.009], p = 0.223) in the RYGB group than in the control group (Table 2). The estimated failure load was 12% lower in tibia and 16% lower in radius in the RYGB group (all p < 0.001, Table 2).
Bone Turnover Markers
In general, bone turnover markers were higher in the RYGB group than in the control group (Table 3). Even though 86% of the RYGB individuals supplemented their diet with daily calcium and vitamin D, resulting in higher 25OHD levels (p < 0.001), PTH (upper reference level 6.9 pmol/l) was higher (7.24 pmol/l [IQR 6.59; 7.95] vs 5.36 pmol/l [IQR 4.83; 5.96], p < 0.001) in the RYGB group than in the control group. Forty-nine out of 96 in the RYGB group vs 12/49 in the control group displayed a PTH > 6.9 pmol/l (p = 0.003), while 40/96 in the RYGB group vs. 6/49 in the control group displayed 25OHD > 50 nmol/l with PTH > 6.9 pmol/l (i.e., elevated PTH with 25OHD within normal range) (p < 0.001).
Impact of Type 2 Diabetes Remission after RYGB
Basic characteristics of the RYGB group with and without diabetes remission are shown in Supplementary Table 2. When stratifying by current T2D status, we found no difference between RYGB individuals with and without diabetes regarding neither aBMD, vBMD, characteristics of cortical, and trabecular bone nor estimated strength or failure load (Supplementary Table 3). We did find higher levels of CTX (0.51 ng/ml [IQR 0.38; 0.67] vs 0.42 ng/ml [IQR 0.28; 0.55], p = 0.043) and PINP (63.1 ng/ml [IQR 44.2; 82.6] vs 46.9 ng/ml [IQR 32.9; 62.9], p = 0.010) in the RYGB group with diabetes remission compared with the group without remission, while there were no differences in osteocalcin, BAP, or sclerostin (Supplementary Table 4).
Discussion
This cross-sectional study demonstrates that 6 years after RYGB surgery, individuals with pre-surgical T2D have poorer bone quality than a non-operated control group. RYGB-operated individuals demonstrate higher bone turnover (predominantly CTX and osteocalcin), lower aBMD, and impaired HR-pQCT derived measurements of bone mass (vBMD), structure (trabecular thickness, number, and space), and strength (stiffness and failure load), despite a high adherence to daily calcium and vitamin D supplements. Furthermore, relative to the control group, we found that the RYGB group had an adjusted 6-year post-surgical odds ratio of 2.21 of having osteopenia or osteoporosis. Overall, diabetes status after RYGB did not influence the observed impairment of bone health.
To our knowledge, only three previous studies have evaluated RYGB cohorts restricted to patients with T2D, but not using HR-pQCT. The STAMPEDE randomized trial reported DXA findings after 2 years follow-up in 19 participants randomized to RYGB and found 9.5% lower total hip aBMD compared to the non-operated control group, but no difference at the lumbar spine [14]. Yu et al. evaluated 11 RYGB-operated individuals with T2D compared with gastric sleeve–operated individuals 1 year after surgery and found higher CTX (221%) and PINP (93%) in the RYGB group [15]. Finally, Billetter et al. reported declining aBMD at the hip and at the lumbar spine in addition to increased osteocalcin and urine collagen DPD crosslink (resorption marker) in a 2-year prospective study of 20 individuals with T2D treated by RYGB [13]. We confirm these results in a larger cohort and add valuable HR-pQCT-derived information distinguishing between the effects on cortical and trabecular bone. Furthermore, we hypothesized that diabetes remission following RYGB would be beneficial to bone health. In general, we found no differences in bone mass or quality according to diabetes status, although bone turnover was somehow affected with higher CTX and PINP in the RYGB group with remission than in those without remission. The latter most likely reflecting the known modification of diabetes on markers of bone turnover [16].
Previous studies have evaluated bone health following RYGB in cohorts without T2D. After 2 years of follow-up, Yu et al. found a 6–10% lower hip aBMD and 5–7% lower lumbar spine aBMD compared to non-operated controls, lower vBMDs (especially due to lower trabecular vBMD), and higher bone turnover markers [30]. Two prospective studies of 3 and 5 years of follow-up reported progressively declining aBMD, more renounced at the total hip than at the lumbar spine [11, 12]. In general, we replicate these findings in a restricted cohort of individuals with T2D 6 years after RYGB.
The mechanisms behind impaired bone quality following RYGB are not fully elucidated, but mechanical unloading due to substantial weight loss is a common theory. We measured sclerostin as a marker of unloading, expecting sclerostin to be higher in RYGB operated due to substantial weight loss. Quite opposite, we found significantly lower sclerostin levels in the RYGB group suggesting that weight loss and mechanical unloading do not play an important role for the level of sclerostin 6 years after surgery. Interestingly, the RYGB group displayed even poorer bone quality in non-weight bearing (radius) bone than in weight-bearing bone (tibia), suggesting that the ongoing mechanical loading partly counteracts the influence of RYGB in weight-bearing areas.
Elevated PTH levels due to decreased absorption of calcium and/or vitamin D is another suggested mechanism for poorer bone health after RYGB. In our study, 51% of the RYGB group displayed normocalcemic hyperparathyroidism. High levels of PTH seem to promote cortical bone loss as shown by Stein et al., reporting both lower aBMD at total hip and distal forearm and cortical bone loss measured by HR-pQCT in women with primary hyperparathyroidism [31]. This concurs with our findings of lower aBMD at distal third (mainly cortical bone) and total forearm, as well as at total hip. Our results also suggest that the recommended supplementation of multivitamins and calcium with vitamin D (1200–1300 mg elementary calcium and 2000–2400 IU vitamin D3 in total) following RYGB is not sufficient to prevent RYGB-induced bone loss in all operated patients.
Even though RYGB individuals display poorer bone health than the control patients, average CTX, PINP, and osteocalcin, as well as aBMD at the lumbar spine and femoral neck remained within the normal range. Only aBMD at the forearm was below the normal range. Taking into account that the female participants on average are only a few years after menopause and therefore have to live with this condition for many years to come and the fact that individuals with T2D have been demonstrated to suffer fractures at higher aBMDs than patients without diabetes [17, 18], the observed differences may still be clinically relevant. Whether bariatric surgery, in general, leads to an increased risk of fragility fractures is still being debated [32,33,34,35]. Studies focusing on the RYGB procedure have, however, reported increased risk of peripheral fractures [34, 35].
The main strength of this study is the large cohort of nearly 150 individuals either treated by RYGB or non-operated controls of both sexes all suffering from T2D, where we evaluated bone health in details applying both DXA, HR-pQCT, and bone turnover markers 6 years after RYGB. By matching the two cohorts with respect to current BMI, in addition to age and sex, we sought to omit the influence of weight on BMD. Moreover, the RYGB-operated individuals were very compliant regarding vitamin and mineral supplementation, providing insight to bone metabolism when sticking to guidelines. Furthermore, we were able to describe bone parameters after RYGB in individuals with pre-surgical T2D, according to the diabetes status 6 years after RYGB. Albeit the power calculations were not made for this endpoint.
This study has several limitations. Firstly, with a participation rate of 49%, we cannot rule out selection bias. Secondly, we evaluated our participants over a period of 9 months, which could lead to seasonal variation in 25OHD and PTH assessment [36]. However, we evaluated participants in random order, and when adjusting for examination date, the differences in 25OHD and PTH levels between groups did not change (data not shown). The cross-sectional study design does not allow interpretation of causality. Moreover, the duration of diabetes and HbA1c levels, factors that might be associated with aBMD, were not comparable between the two cohorts. However, adjusting for diabetes duration and HbA1c in a regression model did not change the aBMD estimates (data not shown). We do present several risk factors associated with osteoporosis (Supplementary Table 5), however, the list is not exhaustive and lack information on, e.g., parental history of hip fracture. Retrospectively, assessment of renal calcium excretion, gastrointestinal hormones, food intake, and use of pedometer might have provided a greater understanding of the underlying mechanisms for poorer bone quality after RYGB. With an average BMI > 30 kg/m2 in both groups, the risk of artifacts in DXA scans cannot be ruled out; however, we assume that the risk of artifacts is evenly distributed between groups. Finally, the Danish population is mainly Caucasian, why our findings may not apply in other populations.
Conclusion
We found that 6 years after surgery, RYGB-operated individuals with pre-surgical T2D have poorer bone health than a non-operated control group and an adjusted 6-year odds ratio of 2.21 of osteopenia or osteoporosis despite high adherence to daily calcium and vitamin D supplementation. However, in individuals with T2D preoperatively, diabetes status after RYGB (remission versus non-remission) had no influence on the observed impairment of bone health. While waiting for longitudinal data from RYGB operated and unbiased control cohorts, we suggest that clinicians acknowledge the potential risk of adverse effects of RYGB on bone health and in case of clinical suspicion of osteoporosis include DXA and biochemical markers in the post-RYGB management.
References
Angrisani L, Santonicola A, Iovino P, Vitiello A, Zundel N, Buchwald H, Scopinaro N. Bariatric surgery and endoluminal procedures: IFSO worldwide survey 2014. Obes Surg. 2017;27(9):2279–89
Chang SH, Stoll CR, Song J, et al. The effectiveness and risks of bariatric surgery: an updated systematic review and meta-analysis, 2003-2012. JAMA Surg. 2014;149(3):275–87.
Schauer PR, Bhatt DL, Kirwan JP, et al. Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med. 2017;376(7):641–51.
Yu EW. Bone metabolism after bariatric surgery. J Bone Miner Res. 2014;29(7):1507–18.
Pories WJ. Bariatric surgery: risks and rewards. J Clin Endocrinol Metab. 2008;93(11 Suppl 1):589–96.
Schafer AL, Weaver CM, Black DM, et al. Intestinal calcium absorption decreases dramatically after gastric bypass surgery despite optimization of vitamin D status. J Bone Miner Res. 2015;30(8):1377–85.
Toh SY, Zarshenas N, Jorgensen J. Prevalence of nutrient deficiencies in bariatric patients. Nutrition. 2009;25(11–12):1150–6.
Hage MP, El-Hajj Fuleihan G. Bone and mineral metabolism in patients undergoing Roux-en-Y gastric bypass. Osteoporos Int. 2014;25(2):423–39.
Via MA, Mechanick JI. Nutritional and micronutrient care of bariatric surgery patients: current evidence update. Curr Obes Rep. 2017;6(3):286–96.
Madsen LR, Espersen R, Rejnmark L, Richelsen B. Effect of calcium citrate vs calcium carbonate on elevated parathyroid hormone after Roux-en-Y gastric bypass. A double-blinded, randomized trial. Clin Endocrinol (Oxf). 2018;89(6):734–41
Raoof M, Naslund I, Rask E, et al. Effect of gastric bypass on bone mineral density, parathyroid hormone and vitamin D: 5 years follow-up. Obes Surg. 2016;26(5):1141–5.
Vilarrasa N, San Jose P, Garcia I, et al. Evaluation of bone mineral density loss in morbidly obese women after gastric bypass: 3-year follow-up. Obes Surg. 2011;21(4):465–72.
Billeter AT, Probst P, Fischer L, et al. Risk of malnutrition, trace metal, and vitamin deficiency post roux-en-y gastric bypass--a prospective study of 20 patients with BMI < 35 kg/m(2). Obes Surg. 2015;25(11):2125–34.
Maghrabi AH, Wolski K, Abood B, et al. Two-year outcomes on bone density and fracture incidence in patients with T2DM randomized to bariatric surgery versus intensive medical therapy. Obesity (Silver Spring). 2015;23(12):2344–8.
Yu EW, Wewalka M, Ding SA, et al. Effects of gastric bypass and gastric banding on bone remodeling in obese patients with type 2 diabetes. J Clin Endocrinol Metab. 2016;101(2):714–22.
Hygum K, Starup-Linde J, Harslof T, et al. MECHANISMS IN ENDOCRINOLOGY: diabetes mellitus, a state of low bone turnover - a systematic review and meta-analysis. Eur J Endocrinol. 2017;176(3):R137–57.
Vestergaard P. Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes--a meta-analysis. Osteoporos Int. 2007;18(4):427–44.
Leslie WD, Rubin MR, Schwartz AV, et al. Type 2 diabetes and bone. J Bone Miner Res. 2012;27(11):2231–7.
Stein EM, Silverberg SJ. Bone loss after bariatric surgery: causes, consequences, and management. Lancet Diabetes Endocrinol. 2014;2(2):165–74.
Fuller H, Fuller R, Pereira RMR. High resolution peripheral quantitative computed tomography for the assessment of morphological and mechanical bone parameters. Rev Bras Reumatol. 2015;55:352–62.
Stein EM, Carrelli A, Young P, et al. Bariatric surgery results in cortical bone loss. J Clin Endocrinol Metab. 2013;98(2):541–9.
Lynge E, Sandegaard JL, Rebolj M. The Danish National Patient Register. Scand J Public Health. 2011;39(7 Suppl):30–3.
Buse JB, Caprio S, Cefalu WT, Ceriello A, Del Prato S, Inzucchi SE, McLaughlin S, Phillips GL 2nd, Robertson RP, Rubino F, Kahn R, Kirkman MS. How do we define cure of diabetes?. Diabetes Care. 2009;32(11):2133-5.
Dicker D, Yahalom R, Comaneshter DS, et al. Long-term outcomes of three types of bariatric surgery on obesity and type 2 diabetes control and remission. Obes Surg. 2016;26(8):1814-20.
Looker AC, Melton 3rd LJ, Harris T, et al. Age, gender, and race/ethnic differences in total body and subregional bone density. Osteoporos Int. 2009;20(7):1141–9.
Abrahamsen B, Gram J, Hansen TB, et al. Cross calibration of QDR-2000 and QDR-1000 dual-energy X-ray densitometers for bone mineral and soft-tissue measurements. Bone. 1995;16(3):385–90.
Mosekilde L, Beck-Nielsen H, Sorensen OH, et al. Hormonal replacement therapy reduces forearm fracture incidence in recent postmenopausal women - results of the Danish osteoporosis prevention study. Maturitas. 2000;36(3):181–93.
Ornstrup MJ, Harslof T, Kjaer TN, et al. Resveratrol increases bone mineral density and bone alkaline phosphatase in obese men: a randomized placebo-controlled trial. J Clin Endocrinol Metab. 2014;99(12):4720–9.
Pauchard Y, Liphardt AM, Macdonald HM, et al. Quality control for bone quality parameters affected by subject motion in high-resolution peripheral quantitative computed tomography. Bone. 2012;50(6):1304–10.
Yu EW, Bouxsein ML, Putman MS, et al. Two-year changes in bone density after Roux-en-Y gastric bypass surgery. J Clin Endocrinol Metab. 2015;100(4):1452–9.
Stein EM, Silva BC, Boutroy S, et al. Primary hyperparathyroidism is associated with abnormal cortical and trabecular microstructure and reduced bone stiffness in postmenopausal women. J Bone Miner Res. 2013;28(5):1029–40.
Lalmohamed A, de Vries F, Bazelier MT, et al. Risk of fracture after bariatric surgery in the United Kingdom: population based, retrospective cohort study. BMJ. 2012;345:e5085.
Rousseau C, Jean S, Gamache P, et al. Change in fracture risk and fracture pattern after bariatric surgery: nested case-control study. BMJ. 2016;354:i3794.
Yu EW, Lee MP, Landon JE, Lindeman KG, Kim SC. Fracture risk after bariatric surgery: Roux-en-Y gastric bypass versus adjustable gastric banding. J Bone Miner Res. 2.
Axelsson KF, Werling M, Eliasson B, et al. Fracture risk after gastric bypass surgery: a retrospective cohort study. J Bone Miner Res. 2018;33(12):2122–31.
Webb AR, Kline L, Holick MF. Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. J Clin Endocrinol Metab. 1988;67(2):373–8.
Acknowledgments
The authors would like to thank the staff at our outpatient clinic for help in recruiting participants.
Funding
LRM is affiliated to the Danish Diabetes Academy funded by the Novo Nordisk Foundation (NNF 12SA1016522). The study was funded by the Health Research Fund of Central Denmark Region (A294), the Novo Nordisk Foundation (NNF16OC0020870), the A.P. Møller Foundation (15–253), and the Danish Osteoporosis Society (grant number n/a).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
LRM has received grant support from the Danish Diabetes Academy funded by the Novo Nordisk Foundation, the A.P. Møller Foundation, and the Health Research Fund of Central Denmark Region. RE has received grant support from the Danish Osteoporosis Society. MJO and NRJ have nothing to disclose. BL has received grant support from Amgen and Novo Nordisk and has received lecture fees from the advisory board of Amgen, UCB, Eli Lilly, and TEVA. BR has received grant support from the Novo Nordisk Foundation.
Ethical Approval
The study was approved by the ethical committee of Central Denmark Region (VEK 1-10-72-167-15) and registered at clinicaltrials.org (NCT02625649). The study was conducted according to the 1964 Declaration of Helsinki and its later amendments.
Informed Consent
Participation in this study was preceded by full explanation of the purpose and nature of all procedures used and written consent.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 30 kb)
Rights and permissions
About this article
Cite this article
Madsen, L.R., Espersen, R., Ornstrup, M.J. et al. Bone Health in Patients with Type 2 Diabetes Treated by Roux-En-Y Gastric Bypass and the Role of Diabetes Remission. OBES SURG 29, 1823–1831 (2019). https://doi.org/10.1007/s11695-019-03753-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-019-03753-3