Abstract
Background and Aims
Bowel obstruction due to internal hernia (IH) is a well-known late complication of a laparoscopic roux-en-y gastric bypass (LRYGBP). The objective of this study is to evaluate if closure of the mesenteric defect and Petersen’s space will decrease the rate of internal hernias compared to only closure of the mesenteric defect.
Methods
A single-center retrospective descriptive study was performed. All patients with LRYGBP from 2011 till April 2017 were included. An antecolic technique was used with closure of the mesenteric defect with a non-absorbable running suture between 2011 and October 2013 (group A), and from November 2013, we added closure of the Petersen defect (group B).
Results
From a total of 3124 patients, 116 patients (3.71%) had an exploratory laparoscopy due to suspicion of bowel obstruction, but in only 67 (2.14%) patients, an IH was found. Preoperative CT predicted the diagnosis in only 73%. In group A, including 1586 patients, 53 (3.34%) were diagnosed with an internal hernia: 39 at Petersen’s space and 14 at the mesenteric defect. The mean time interval was 24.2 months and the mean BMI 25.7 kg/m2. After routine closure of the Petersen defect in 1538 patients in group B, an internal hernia during laparoscopy was found in 14 (0.91%) patients after a mean period of 13.5 months: 11 at Petersen’s space and 3 at the mesenteric defect. In two subgroups (C and D) with an equal follow-up time (24–42 m), the incidence of 1.15% (8/699) was halved in the closure group of both defects compared to the incidence of 2.58% (23/893) in the group with only closure of the mesenteric defect.
Conclusions
After descriptive analysis, these results can provide strong recommendation of closure of the mesenteric defect and Petersen’s space, as we notice a tendency to lower incidence of internal hernias.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A well-known complication of LRYGBP is bowel obstruction due to internal herniation (IH). The incidence of IH after LRYGBP has been reported to be between 0.5 and 11% [1]. Clinical symptoms related to an IH can vary from vague nonspecific symptoms, like intermittent or postprandial pain to persistent abdominal pain and an acute abdomen [2]. Because of the nonspecific clinical presentation and the absence of reliable diagnostic imaging, it can cause a high morbidity and even mortality.
The symptoms can develop at any time after the operation, but the incidence of small bowel obstruction seems to be the highest at 1–2 years after surgery [3]. This corresponds to the time of the greatest weight loss with rapid loss of mesenteric fat [4]. There are no guidelines concerning closure of the mesenteric defects, but it has been suggested that the mesenteric defects should be closed during LRYGBP to reduce the risk of IH. In the antecolic approach we used, two defects can be defined, which are potential locations at risk for an internal hernia. The mesenteric defect (Fig. 1 (1)) at the jejuno-jejunostomy when creating the roux limb or the potential space posterior to the roux limb immediately distal to the mesocolon referred as Petersen defect (Fig. 1 (2)).
To our knowledge, no studies have been published concerning the benefit of additional closure of the Petersen and mesenteric defect compared to closure of only the mesenteric defect. Therefore, the aim of this study is to determine the impact of closure of the Petersen and mesenteric defect on the incidence of internal herniation. We also report the accuracy of CT in diagnosing IH after gastric bypass.
Methods
Study Design
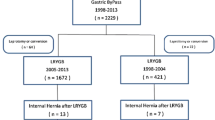
We performed a large single center retrospective study and included 3124 patients from 2011 until April 2017. All patients underwent a laparoscopic gastric bypass in the IFSO certified Obesity Centre ZNA Stuivenberg in Antwerp, Belgium. The patients were divided in two groups, group A with closure of the mesenteric defect (n = 1586) and group B in which the mesenteric and Petersen defect was closed (n = 1538).
Surgical Procedure
During the laparoscopic antecolic gastric bypass, a very small gastric pouch of 20 ml is created. The jejenunum is mobilized, 40–60 cm distal to the ligament of Treitz, and connected to the pouch via an antecolic route to create a gastrojejenustomy. The biliopancreatic loop is anastomosed to the alimentary loop 150 cm distally to the gastrojejunostomy. We used a linear stapler for the gastrojejunostomy and the jejunojejunostomy, with hand-sewn closure of the remaining defect. To close the mesenteric defects (Fig. 2a), we used a non-absorbable running suture. The first stitch started at transition between serosa of small bowel/colon and the mesentery, continuously down to the bottom and then upwards to the first suture. For the Petersen defect (Fig. 2b), only the infracolic part was closed.
Data Selection Process
Data from patients who underwent a LRYGBP and laparoscopy for suspicion of bowel obstruction were retrospectively retrieved from case files in our hospital database and we identified 116 patients who underwent an exploratory laparoscopy for suspicion of small bowel obstruction in our center (Fig. 3). After reviewing all the patient’s files and operation reports manually, we determined that only in 67 patients, an internal hernia was proven during laparoscopy. The patients in which an open mesenteric or Petersen defect was found without a sign of small bowel obstruction at the time of operation were not included in these 67 patients, as the existence of intermittent hernia cannot be objectified. All patients were followed up till April 2017. To define the diagnostic value of CT scan, the radiology reports were analyzed whether the typical known signs of IH were described: mesenteric swirl, small bowel obstruction, mushroom sign, clustered loops, hurricane eye, small bowel behind the superior mesenteric artery, and right-sided anastomosis [5].
Statistics
Data were analyzed using STATA/SE version 13.1. Normality of continuous variables was evaluated using sk (skewness and kurtosis) test. Categorical data were compared with X2 test and continuous data with the independent sample t test. Survival analysis is used for analyzing the occurrence of IH in both groups. A two-tailed p < 0.05 was considered significant.
Results
Between January 2011 and April 2017, a total of 3124 morbidly obese patients underwent a LRYGBP. In 1586 patients of group A, only the mesenteric defect was closed, while in group B in 1538 patients, the mesenteric and Petersen defect (infracolic portion) was closed.
From both groups, a total of 116 patients underwent an explorative laparoscopy for suspicion of bowel obstruction, but only in 67 patients, an IH, with proven bowel in the mesenteric defects, was found. Other causes found were adhesions in 28 patients and food impaction at the jejuno-jejunostomy in one patient. In the remaining 28 patients, no reason could be determined. In the last group, we did not assess the exact number of patients with open mesenteric defects. Although in all patients, the defects were closely inspected during explorative laparoscopy and closed if they were found open.
From the 67 patients with an internal herniation, 53 were in group A and 14 in group B (Table 1). There were no statistical differences between both groups according to age, BMI, and comorbidities (hypertension, diabetes mellitus, and sleep apnea). Female to male ratio was 9:1 in group A and 1:1 in group B. Previous bariatric surgery (e.g., gastric banding) was performed in six patients in group A and one in group B.
In group A, 39 patients (74%) had a herniation at Petersen’s defect and 14 (26%) at the mesenteric defect. The mean BMI at the time of laparoscopy was 25.7 kg/m2 and the mean excess BMI loss 96%. The mean time after the LRYGBP was 24.2 months (18.5–24.4). The observation period was from 42 till 76 months.
After closure of the Petersen defect in group B, an internal hernia during laparoscopy was found in 11 patients (79%) at the infracolic portion of the Petersen defect and in 3 patients (21%) at the mesenteric defect. A total of 13.5 months (5.7–16) was the mean time interval between LRYGBP and IH. The mean BMI at that moment was 25.6 kg/m2 and the mean excess BMI loss 97%. In this group, the follow-up period is from 0 till 42 months.
In our hospital database, we have a follow-up time of 75% after 1 year and 50% after 2 years of the patients after bariatric surgery. Clinical follow-up is performed every 3 months during the first year, every 6 months during the second year and annually thereafter. Follow-up at the dietician is planned after 6 and 12 months and then annually combined with a blood examination to check the vitamin status.
Due to the different follow-up time in both groups, there was a significant (p = 0.002) difference in time of IH after LRYGBP, 749 days in group A and 420 days in group B. To compare both groups, a survival analysis was performed (Fig. 4). The log rank test for equality of survivor functions was significant (p = 0.000), showing a tendency of a lower number of IH after closure of the mesenteric and Petersen defect.
A preoperative CT was performed in 61 patients and confirmed the diagnosis in 70% in group 1 and 86% in group 2 (Table 1). We did not demonstrate any false positive reports.
To compare the groups within an equal follow-up time (24–42 m), two subgroups were created (Fig. 5). In group C, 893 had a LRYGBP with closure of the mesenteric defect. While in group D, 699 underwent a LRYGBP with closure of both defects. The incidence of IH in group C was 2.58% (n = 23); however, only eight patients developed an IH in group D, an incidence of 1.15%. The incidence was halved in the closure group of both defects compared to the group with only closure of the mesenteric defect. The locations were 6 at the mesenteric and 17 at the Petersen defect in group C and 1 at the mesenteric and 7 at the Petersen defect in group D. We have no explanation for the reduction of IH in the mesenteric defects and the higher proportion of IH at the Petersen defect in both groups, as these groups are too small for report any significant differences.
Complications due to closure of the defects were not assessed.
Discussion
This study shows a tendency to lower incidence of internal herniation after closure of the mesenteric and Petersen’s defect in groups A and B. If we compare two groups with an equal follow-up period, we found a significant reduced incidence from 2.58 to 1.15%. These results are comparable with previously reported data. In literature, a mean incidence of IH after LRYGBP is 2.5% [6], varying from 0.5 till 11% [1]. A nationwide Danish study by Kristensen et al. [7] revealed a 4% cumulative 5-year incidence of IH without routinely closure of any defect. Studies comparing the effect of closure of both defects compared to no closure can already be found. Chowbey et al. [8] described a reduced incidence from 3.5% if no mesenteric defects were closed to 1.7% after closure of both defects. None show the added value of closure of the Petersen defect.
In our study, 116 patients (3.71%) underwent a diagnostic laparoscopy for suspicion of small bowel obstruction. Stenberg et al. [3] defined the number of reoperations for small bowel obstruction as main outcome and reported a significantly reduced cumulative incidence in the closure group (0.055) compared to non-closure (0.102). In 20 patients, no cause could be defined during surgery. It is possible that some of these patients had an intermittent IH [7] that was not identified during the procedure.
Although an abdominal CT scan is the recommended radiologic investigation to diagnose IH, the results are often inconclusive. Mesenteric swirl is one of the best indicators of IH after gastric bypass surgery [5, 9]. The sensitivity in our study is 70–86%, equivalent to previously reported values from 76% [10] to 85% [3]. So, a negative CT scan cannot rule out the potential for internal hernia and surgical exploration should remain the gold standard when there is a clinical suspicion for IH.
The strength of this study is the large number of patients from a single center and the equally experienced surgeons in laparoscopic bariatric surgery, using the same technique for closure of the defects. All defects were closed with a non-absorbable running suture. The use of other techniques is also a subject of debate, like stapling [11] and fibrin glue. In literature, suturing or using clips, having the highest tensile strength, was superior and equally effective at closing the mesenteric defect, but the use of fibrin glue needs to be further investigated [12]. We do not believe that closure of the supracolic portion of the Petersen defect would decrease the number of IH. We think that the mechanism of IH at the Petersen defect is originating at a medial angle of Treitz from which the small bowel can pass medially in the infracolic portion of the Petersen defect to cause an IH.
We did not demonstrate a learning curve for closure of the Petersen defects, as this standardized procedure was performed by highly skilled and well-experienced bariatric surgeons trained in closure of the mesenteric defects.
Complications reported related to closure of the mesenteric defects in other studies are IH due to incomplete closure (1.4%), kinking (0.2%), hematoma (0.9%), and adhesions (4.6%). Although the overall risk for this seems low [13], our study did not particularly focus on complications.
Our study is not without limitations. One of the drawbacks of this non-randomized retrospective study is that patients presenting with IH at other hospitals are not included. Although all patients were encouraged to come to our hospital if they experience any abdominal complaints, we can assume that some patients are missing at a comparable rate in both groups. So, this may slightly underestimate the true incidence of IH in this study. Another limitation is that the remaining data of the 3008 patients without IH were no subject of further evaluation in this particular study. The last limitation is the difference in follow up-time, so that patients operated in a later period of the study can still present with an IH in the future. Therefore, we created two subgroups, to compare groups with a same observation period from 24 to 42 months. We will continue the follow-up for analysis of longer term results. As the incidence of IH is very low, it is difficult to estimate the sample size and power of the study necessary to define statistically significant differences.
Conclusion
We report a reduced incidence of internal herniation after additional closure of the Petersen defect. We provide a strong recommendation to close the mesenteric and the Petersen defect, although this will not bring the risk down to zero. A diagnostic laparoscopy remains the gold standard in suspicion of bowel obstruction, as clinical symptoms and radiologic findings are often inconclusive.
References
Iannelli A, Buratti MS, Novellas S, et al. Internal hernia as a complication of laparoscopic roux-en-Y gastric bypass. Obes Surg. 2007;17(10):1283–6.
Marmuse JP, Parenti LR. Gastric bypass. Principles, complications, and results. J Visc Surg. 2010;147(5 Suppl):e31–7.
Stenberg E, Szabo E, Agren G, et al. Closure of mesenteric defects in laparoscopic gastric bypass: a multicentre, randomised, parallel, open-label trial. Lancet. 2016;387(10026):1397–404.
Schneider C, Cobb W, Scott J, et al. Rapid excess weight loss following laparoscopic gastric bypass leads to increased risk of internal hernia. Surg Endosc. 2011;25(5):1594–8.
Dilauro M, McInnes MD, Schieda N, et al. Internal hernia after laparoscopic roux-en-Y gastric bypass: optimal CT signs for diagnosis and clinical decision making. Radiology. 2017;282(3):752–60.
Iannelli A, Facchiano E, Gugenheim J. Internal hernia after laparoscopic roux-en-Y gastric bypass for morbid obesity. Obes Surg. 2006;16(10):1265–71.
Kristensen SD, Jess P, Floyd AK, et al. Internal herniation after laparoscopic antecolic roux-en-Y gastric bypass: a nationwide Danish study based on the Danish National Patient Register. Surg Obes Relat Dis. 2016;12(2):297–303.
Chowbey P, Baijal M, Kantharia NS, et al. Mesenteric defect closure decreases the incidence of internal hernias following laparoscopic roux-en-Y gastric bypass: a retrospective cohort study. Obes Surg. 2016;26(9):2029–34.
Lockhart ME, Tessler FN, Canon CL, et al. Internal hernia after gastric bypass: sensitivity and specificity of seven CT signs with surgical correlation and controls. AJR Am J Roentgenol. 2007;188(3):745–50.
Altieri MS, Pryor AD, Telem DA, et al. Algorithmic approach to utilization of CT scans for detection of internal hernia in the gastric bypass patient. Surg Obes Relat Dis. 2015;11(6):1207–11.
Aghajani E, Jacobsen HJ, Nergaard BJ, et al. Internal hernia after gastric bypass: a new and simplified technique for laparoscopic primary closure of the mesenteric defects. J Gastrointest Surg. 2012;16(3):641–5.
Jacobsen H, Dalenback J, Ekelund M, et al. Tensile strength after closure of mesenteric gaps in laparoscopic gastric bypass: three techniques tested in a porcine model. Obes Surg. 2013;23(3):320–4.
Kristensen SD, Floyd AK, Naver L, et al. Does the closure of mesenteric defects during laparoscopic gastric bypass surgery cause complications? Surg Obes Relat Dis. 2015;11(2):459–64.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval Statement
For this type of study, formal consent is not required.
Informed Consent Statement
Does not apply.
Rights and permissions
About this article
Cite this article
Blockhuys, M., Gypen, B., Heyman, S. et al. Internal Hernia After Laparoscopic Gastric Bypass: Effect of Closure of the Petersen Defect - Single-Center Study. OBES SURG 29, 70–75 (2019). https://doi.org/10.1007/s11695-018-3472-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-3472-9