Abstract
Background
Bariatric surgeries have been widely used in obesity associated type II diabetes. However, the mechanisms of surgical treatments for type II diabetes in non-obese patients remain controversial. Our study aims to compare the effectiveness of various bariatric surgeries in a non-obese diabetic rat model.
Methods
Goto-Kakisaki (GK) rats were used to compare the outcome of total gastrectomy (TG), Roux-en-Y reconstruction after total gastrectomy (RYTG), and Roux-En-Y gastric bypass (RYGB). Body weight, food and water intake, and glucose level were monitored prior to and after surgery. Oral glucose tolerance tests (OGTT) were performed, and key metabolic hormones were measured at selected time points.
Results
Despite a significant reduction in body weight in TG and RYTG groups, their glucose metabolic rate was not improved. RYGB rats, with only moderate reduction in food intake and body weight, had significantly improved glucose metabolism. Insulin and ghrelin were significantly reduced in TG and RYTG groups, but remained unchanged in RYGB group.
Conclusions
Our study demonstrated the effectiveness of RYGB surgery in treating type II diabetes in non-obese diabetic rats. These results suggest an important role of gastric system in regulating glucose homeostasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type II diabetes is a chronic disease characterized by hyperglycemia and insulin resistance. Globally, the rate of type II diabetes has been rapidly increasing over the years. In clinical treatments for type II diabetes, major approaches are pharmaceutical interventions for food restriction and stimulation for insulin secretion. In addition, bariatric surgeries have been widely used in obesity-associated type II diabetes. The most common bariatric surgeries include gastric banding, gastric bypass, laparoscopic sleeve gastrectomy (LSG), and biliopancreatic diversion (BPD). The purpose of these surgeries is to limit food intake and nutrient absorption, which in turn reduce body weight and fat tissue mass, thereby promoting glucose metabolism and insulin sensitivity. A meta-analysis study indicated improved glycemic control in 83.8 % of morbidly obese patients after gastric bypass and 47.8 % after gastric banding [1].
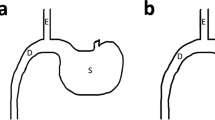
Total gastrectomy (TG), or total gastrectomy with a Roux-en-Y reconstruction (RYTG), involves complete removal of the entire stomach, which is usually performed in patients with stomach cancer [2]. However, despite reduced food intake and body weight, previous studies indicate that patients with TG often had even higher risk of developing diabetes, which could be triggered by postprandial hyperglycemia [3]. In contrast, patients undergoing Billroth’s operation II and Roux-en-Y anastomosis had significantly improved glycemic control [4]. Based on these evidences, it is proposed that hormones secreted by the gastrointestinal tract may play an important role in maintaining glucose balance. Roux-en-Y gastric bypass (RYGB) is the most popular bariatric surgery [5]. Compared to TG and RYTG, RYGB surgery does not completely remove the stomach, but reduces it to a smaller pouch. The smaller stomach is connected directly to jejunum, bypassing the rest of the stomach and duodenum. By partially reducing stomach size and rerouting nutrients to distal intestine, RYGB often leads to significantly improved glucose metabolism and insulin sensitivity in the patients [6]. However, with remarkable success of bariatric surgeries in obesity-related diabetes, their effectiveness on treating type II diabetes in non-obese patients remains controversial.
In our study, we used a non-obese diabetic rat model, Goto-Kakisaki (GK) rats, which spontaneously develop mild hyperglycemia at an early age due to impaired pancreatic β-cell development [7]. Three surgical procedures were compared for their effectiveness in regulating glucose metabolism, including TG, RYTG, and RYGB. Food and water intake, glucose level, and key metabolic hormones, such as insulin, glucagon-like peptide 1 (GLP-1), and ghrelin were measured prior to and after surgery. Oral glucose tolerance tests (OGTT) were performed to characterize glucose clearance rate.
Materials and Methods
Animals
Sixty male GK rats were purchased from Shanghai SLAC Laboratory Animal Inc. The rats were all 11-week old and weighed around 400 g. The rats were housed in specific-pathogen-free (SPF) grade animal laboratory in the Center of Experimental Animals, Second Military Medical University. The animal room has air filter and gradient pressure isolation system, with temperature controlled between 22 and 24 °C, and relative humidity between 50 and 60 %. The room has automatic 12-h light/12-h dark cycle. No more than five rats were housed in each cage. Unless preoperative fasting, the rats had free access to food and water. Water was contained in jars with scaled drops. Experimental diet for diabetic rats (M04-F) was purchased from Shanghai SLAC Laboratory Animal Inc., with standard GB14924.2-GB14924.6. The diet contained protein 18.8 %, raw fat 16.2 %, and carbohydrate 65 %, with total energy 379 Kcal per cup. The diet was sterilized using 60Co radiation.
Surgical Procedures
The rats were divided into five groups (n = 8 per group): total gastrectomy (TG), Roux-en-Y total gastrectomy (RYTG), Roux-en-Y gastric bypass (RYGB), sham operation (SO), and non-operated control (NC). The rats were fasted for 12 h prior to surgery. The procedures were performed under anesthesia (1 % sodium pentobarbital). TG, with or without Roux-en-Y reconstruction (RYTG), was performed as previously described [8]. The whole stomach was removed, with esophagus being directly connected to duodenum. Roux-en-Y gastric bypass (RYGB) was performed using protocol described previously [9]. Sham operation (SO) was performed by midline laparotomy, with abdominal incision length and stitching procedures similar to other surgical groups. Body weight and food and water intake were monitored weekly before and after surgery. All procedures were performed in accordance with the guidelines of Tongji University of Shanghai, China.
Metabolic Parameter Measurements and Oral Glucose Tolerance Test (OGTT)
Glucose, glucagon-like peptide 1 (GLP-1), insulin, and ghrelin level were measured before and after surgery at selected time points. Glucose was measured using One Touch Ultra® glucose meter and test trips (Johnson & Johnson), with around 20 μL blood collected from the tail vein. Ghrelin, GLP-1, and insulin were measured using Ghrelin (Rat, Mouse) radioimmunoassay (RIA) kit, GLP-1 (Rat, Mouse) RIA kit (Phoenix Pharmaceuticals, Inc. USA), and Insulin (Rat, Mouse) enzyme-linked immunosorbent assay (ELISA) kit (Phoenix Pharmaceuticals, Beijing, Co., Ltd.), respectively. For measuring hormone levels, 1–3 mL of blood samples was collected from each rat through angular vein under anesthesia after 12 h of fasting. For OGTT, after 12 h of fasting, 25 % glucose solution was gavage fed to each rat, at 1 g glucose per kilogram body weight. Glucose level was then determined at indicated intervals.
Statistics
Data are expressed as mean ± S.E. The significance of difference in mean values was evaluated by two-way ANOVA followed by a Bonferroni post-test. Comparison of area under the curve (AUC) among the groups was analyzed by one-way ANOVA followed by a Bonferroni post-test. p < 0.05 was considered statistically significant. All statistical analyses were carried out using GraphPad Prism 5.0.
Results
Measurements of Physiological Parameters
GK rat is a genetic model of spontaneous diabetes, exhibiting impaired glucose metabolism, hyperglycemia, and hyperinsulinemia from early age. Prior to surgery, food and water intake, body weight, and glucose level were similar among the five groups of rats. The procedures posed severe metabolic challenges in all the treated groups. One week after surgery, food and water intake, body weight, and glucose level all significantly decreased, except the NC group (Fig. 1). The decrease in food and water intake was especially pronounced in RYTG and TG groups, with roughly 90 % reduction (Fig. 1a, b). Two weeks after surgery, SO and NC rats gradually resumed their normal food and water intake, and their body weight steadily increased. Their plasma glucose returned to their preoperative level, although SO rats remained slightly lower than the NC rats. Compared to SO and NC rats, food and water intake for RYTG and TG rats remained significantly lower after surgery.
Along with reduced food and water intake, the body weight for RYTG and TG rats remained low and even continued decreasing weekly, with almost 100 g lower than the SO and NC rats at 8 weeks after surgery (Fig. 1c). However, the significant reduction in body weight in TG and RYTG rats was not associated with reduced glucose level. As shown in Fig. 1d, the glucose level in TG and RYTG rats, with initial reduction shortly after surgery, slowly increased, and eventually reached comparable levels to SO and NC rats at 8 weeks. The food intake and body weight remained significantly lower in RYGB rats after surgery (Fig. 1a, c), which is also accompanied by significantly reduced plasma glucose level (Fig. 1d), compared to other four groups of rats.
Oral Glucose Tolerance Test (OGTT)
As an important indicator for glucose metabolism and insulin sensitivity, OGTT was performed on the rats at three time periods: before surgery, 4 and 8 weeks after surgery. All the rats were fasted for 12 h prior to the tests. Following gavage feeding of 25 % glucose solution at 1 g glucose/kg body weight, plasma glucose level was determined at selected intervals. Before surgery, the plasma glucose level gradually increased after glucose administration, peaked at 30 min, and then slowly returned to the basal level at 2 h post gavage feeding (Fig. 2a).
Oral glucose tolerance tests (OGTT). Following 12 h of fasting, OGTT was performed before surgery (a), and at 4 weeks (b) or 8 weeks (c) after surgery, by administering 1 g glucose per kilogram body weight through gavage feeding. Blood samples were collected through tail vein at indicated intervals. Area under the curves (AUC) was calculated for OGTT performed at 4 weeks (d) or 8 weeks (e) after surgery. *P < 0.05; **P < 0.01; ***P < 0.001; n = 8 rats per group
OGTT was then performed at 4 and 8 weeks after surgery. Before glucose administration, basal glucose level in TG, RYTG, and RYGB rats was significantly lower, compared to SO and NC rats. During OGTT, the glucose level in TG and RYTG rats reached comparable level to SO, NC rats, and TG rats had even higher level at time points from 45 min to 2 h. The glucose level in RYGB remained significantly lower throughout the test, compared to the rest of the rats (Fig. 2b). This effect was better presented by calculating area under the curve (AUC), indicating improved glucose metabolic signaling in RYGB group, but a compromised metabolic profile for TG rats (Fig. 2d).
The difference in OGTT among the five groups was even more pronounced at 8 weeks after surgery. RYGB rats showed even more significant reduction in blood glucose at all the time points, indicating markedly improved glucose tolerance, compared to NC and SO groups. TG and RYTG rats, in contrast, showed significantly increased glucose level during OGTT, especially between 45 min and 2 h, indicating more compromised glucose tolerance (Fig. 2c). This result was also confirmed by calculating AUC, showing significant increase in TG and RYTG, but around 30 % reduction in RYGB rats (Fig. 2e).
Plasma Hormone Levels
In order to further identify the mechanism by which glucose tolerance was altered in the treated rats, three hormones, glucagon-like peptide 1 (GLP-1), insulin, and ghrelin, were measured before, and at 2, 4, 6, and 8 weeks after surgery (data listed in Table 1). For SO and NC rats, GLP-1 and insulin remained unchanged for all the five time points, while ghrelin gradually increased weekly. At 2 weeks after surgery, TG, RYTG, and RYGB rats all had significantly higher GLP-1, with RYTG rats showing the highest response. However, GLP-1 level in TG rats gradually decreased after 2 weeks, and eventually fell to lower level than SO and NC groups. RYTG and RYGB rats maintained significantly higher level of GLP-1, compared to other groups. Insulin level in SO, NC, and RYGB groups was similar, and remained unchanged throughout the test, while TG and RYTG rats had significantly lower insulin after surgery. Ghrelin was significantly decreased in TG and RYTG groups, compared to SO and NC groups, with almost 90 % reduction at 8 weeks after surgery. Ghrelin in RYGB rats had a temporary increase at 2 weeks after surgery, but then returned to similar level to SO and NC rats for the rest of the time points.
Discussion
Our study compared the effectiveness of TG, RYTG, and RYGB on glycemic control and metabolic hormone production in a non-obese diabetic rat model, GK rats. TG and RYTG completely removed the stomach in the rats, which significantly reduced their food and water intake, which led to dramatic decrease in body weight. However, their glucose metabolic profile was not improved. During OGTT at 4 and 8 weeks after surgery, TG and RYTG rats showed even slower glucose clearance rate, compared to SO and NC rats. Their compromised glucose metabolism was accompanied by significantly reduced insulin and ghrelin production. RYGB rats, with partially limited stomach size, only had a mild reduction in food intake and body weight. However, RYGB rats had significantly lower glucose level and better glucose tolerance after surgery, compared to other groups. The improved metabolic profile in RYGB rats was associated with higher GLP-1 production, but insulin and ghrelin level was not significantly altered, compared to SO and NC rats.
As a genetically diabetic animal model, GK rats exhibit similar features to non-obese type II diabetes patients, evidenced by reduced β-cell mass and alterations in microenvironment in islets [10]. Therefore, it is a valuable tool to investigate the effect of various surgeries on glucose metabolism and insulin signaling in non-obese subjects. Interestingly, despite the improved glucose metabolism in RYGB rats, their insulin level was not altered, indicating the elevated glucose clearance rate in RYGB rats may not be solely dependent on increased insulin secretion from the β-cells. Both TG and RYTG rats had about 50 % reduction in insulin, compared to SO and NC rats. Impaired insulin secretion was previously reported in mice undergoing TG, which is consistent with our observation [11]. It is possible that reduced food intake caused by TG/RYTG led to impaired glucose-stimulated insulin production from the β-cells, suggesting potential gastro-pancreatic signaling.
GLP-1 is a gut hormone secreted by the L cells of the distal bowel in response to intestinal nutrients [12]. Previous study suggests that GLP-1 promotes pancreas function and stimulates insulin secretion by promoting proliferation and inhibiting apoptosis of β cells [13]. GLP-1 also reduces insulin resistance through activating on central GLP-1 receptors [14]. A GLP-1 agonist, Exenatide (marketed as Byetta or Bydureon), has been approved in clinic for managing type II diabetes. However, in RYGB rats, increased GLP-1 level was not associated with higher insulin secretion. Interestingly, similar to RYGB rats, RYTG rats also had higher level of GLP-1 after surgery. The elevated GLP-1 in RYTG rats was not able to recover their dramatically decreased insulin or ghrelin, which further supports the importance of gastric system in regulating glucose homeostasis. A previous clinic study showed gastric bypass increased GLP-1 induced postprandial insulin secretion in human [15]. Since our study focused on hormone levels during fasting stage, future experiment will investigate postprandial hormone secretion in the treated rats.
Ghrelin is a peptide secreted from the fundus of the stomach and the proximal intestine [16]. In response to food ingestion, ghrelin level increases prior to meals and decreases postprandially. The effect of RYGB on fasting or postprandial ghrelin level has been inconsistent in previous studies. For obese individuals, hyperinsulinemia and insulin resistances are likely to be associated with reduced ghrelin production [17]. In our study using non-obese diabetic rats, there was an early onset of increased ghrelin level at 2 weeks post-RYGB surgery, which gradually returned to the same level as SO and NC rats (Fig. 2c). Insulin level remained unchanged in RYGB rats throughout the study, indicating the short-term increase of ghrelin secretion was not triggered by insulin. In TG and RYTG rats, ghrelin level was significantly reduced by over 70 %, compared to SO and NC rats, indicating severely inhibited appetite in these rats. In TG and RYTG rats, in addition to stomach removal, the significantly lower ghrelin level synergized to further reduce food intake. RYGB rats, with smaller stomach pouch, were able to maintain normal level of ghrelin production and pancreatic insulin secretion.
Regarding the mechanisms by which bariatric surgeries modulate glucose metabolism, two major theories were purposed previously, foregut and hindgut hypotheses. In “foregut hypothesis”, the bariatric procedures exclude duodenum and proximal jejunum from the delivery of nutrients, preventing secretion of gastric molecules that could potentially trigger insulin resistance [18, 19], although the specific target molecules have not yet been characterized. As an alternative theory, the “hindgut hypothesis” purposes that, the expedited delivery of nutrients to the distal intestine activates physiological signal and gastric hormone secretion, which promotes glucose metabolism [12, 20, 21]. Potential candidate molecules supporting the “hindgut theory” are GLP-1 and peptide tyrosine tyrosine (PYY) [22]. An elegant study conducted by Rubino et al. compared these two theories by using two models, duodenal-jejunal bypass (DJB) and gastrojejunostomy (GJ), and showed DJB was more effective in improving glucose metabolism [23]. Their results potentially support a more dominant role of “foregut hypothesis”. According to “foregut hypothesis”, it is possible that RYGB may promote glucose metabolism and insulin signaling by rerouting the nutrients through the bowel. This is consistent with our finding that RYGB rats had significantly increased GLP-1, but insulin level remained unchanged. It is likely that yet unknown factors secreted by the duodenum and proximal jejunum may interfere insulin sensitivity. Therefore, our study may also have provided evidence to further support the ‘foregut theory’.
In summary, our study suggests better outcome of RYGB in managing glucose homeostasis in a non-diabetic rat model, compared to TG and RYTG. The dramatic weight loss in TG and RYTG rats failed to improve their metabolic profile, likely due to compromised gastric hormone secretion after complete stomach removal. RYGB, with partially remaining stomach and moderate weight loss, showed significant improvement in glucose metabolism. These results indicate the important role of gastric system in metabolic signaling through regulating secretion of key hormones. For obesity-related diabetic patients, bariatric surgeries are proven to be effective; however, for non-obese diabetic patients, the physiological regulation by bariatric surgeries is far more complicated. Cautious examination and evaluation is necessary regarding each bariatric procedure in these patients. Our study, for the first time, used animal model to provide insight for the selection of surgical procedures in non-obese diabetic patients. Further study is needed to determine the effect of bariatric surgeries on the regulation on β-cell function, insulin sensitivity and whole body energy homeostasis.
References
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292(14):1724–37.
An JY, Kim YM, Yun MA, et al. Improvement of type 2 diabetes mellitus after gastric cancer surgery: short-term outcome analysis after gastrectomy. World J Gastroenterol. 2013;19(48):9410–7.
Yamamoto H, Tsuchihashi H, Akabori H, et al. Postprandial hyperglycemia after a gastrectomy and the prediabetic state: a comparison between a distal and total gastrectomy. Surg Today. 2008;38(8):685–90.
Zervos EE, Agle SC, Warren AJ, et al. Amelioration of insulin requirement in patients undergoing duodenal bypass for reasons other than obesity implicates foregut factors in the pathophysiology of type II diabetes. J Am Coll Surg. 2010;210(5): 564-72, 572-4.
Roslin MS, Dudiy Y, Brownlee A, et al. Response to glucose tolerance testing and solid high carbohydrate challenge: comparison between Roux-en-Y gastric bypass, vertical sleeve gastrectomy, and duodenal switch. Surg Endosc. 2014;28(1):91–9.
Allen RE, Hughes TD, Ng JL, et al. Mechanisms behind the immediate effects of Roux-en-Y gastric bypass surgery on type 2 diabetes. Theor Biol Med Model. 2013;10:45.
Movassat J, Saulnier C, Serradas P, et al. Impaired development of pancreatic beta-cell mass is a primary event during the progression to diabetes in the GK rat. Diabetologia. 1997;40(8):916–25.
Zittel TT, Glatzle J, Muller M, et al. Total gastrectomy severely alters the central regulation of food intake in rats. Ann Surg. 2002;236(2):166–76.
Rubino F, Marescaux J. Effect of duodenal-jejunal exclusion in a non-obese animal model of type 2 diabetes: a new perspective for an old disease. Ann Surg. 2004;239(1):1–11.
Lacraz G, Figeac F, Movassat J, et al. Diabetic beta-cells can achieve self-protection against oxidative stress through an adaptive up-regulation of their antioxidant defenses. PLoS One. 2009;4(8):e6500.
Salehi A, Chen D, Hakanson R, et al. Gastrectomy induces impaired insulin and glucagon secretion: evidence for a gastro-insular axis in mice. J Physiol. 1999;514(Pt 2):579–91.
Mason EE. The mechanisms of surgical treatment of type 2 diabetes. Obes Surg. 2005;15(4):459–61.
Farilla L, Bulotta A, Hirshberg B, et al. Glucagon-like peptide 1 inhibits cell apoptosis and improves glucose responsiveness of freshly isolated human islets. Endocrinology. 2003;144(12):5149–58.
Parlevliet ET, de Leeuw van Weenen JE, Romijn JA, et al. GLP-1 treatment reduces endogenous insulin resistance via activation of central GLP-1 receptors in mice fed a high-fat diet. Am J Physiol Endocrinol Metab. 2010;299(2):E318–24.
Salehi M, Prigeon RL, D’Alessio DA. Gastric bypass surgery enhances glucagon-like peptide-1 stimulated postprandial insulin secretion in humans. Diabetes. 2011;60(9):2308–14.
Kojima M, Hosoda H, Date Y, et al. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 1999;402(6762):656–60.
McLaughlin T, Abbasi F, Lamendola C, et al. Plasma ghrelin concentrations are decreased in insulin-resistant obese adults relative to equally obese insulin-sensitive controls. J Clin Endocrinol Metab. 2004;89(4):1630–5.
Pories WJ, Albrecht RJ. Etiology of type II diabetes mellitus: role of the foregut. World J Surg. 2001;25(4):527–31.
Rubino F, Gagner M, Gentileschi P, et al. The early effect of the Roux-en-Y gastric bypass on hormones involved in body weight regulation and glucose metabolism. Ann Surg. 2004;240(2):236–42.
Cummings DE, Overduin J, Foster-Schubert KE. Gastric bypass for obesity: mechanisms of weight loss and diabetes resolution. J Clin Endocrinol Metab. 2004;89(6):2608–15.
Patriti A, Facchiano E, Sanna A, et al. The enteroinsular axis and the recovery from type 2 diabetes after bariatric surgery. Obes Surg. 2004;14(6):840–8.
Thomas S, Schauer P. Bariatric surgery and the gut hormone response. Nutr Clin Pract. 2010;25(2):175–82.
Rubino F, Forgione A, Cummings DE, et al. The mechanism of diabetes control after gastrointestinal bypass surgery reveals a role of the proximal small intestine in the pathophysiology of type 2 diabetes. Ann Surg. 2006;244(5):741–9.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All applicable institutional and/or national guidelines for the care and use of animals were followed.
Informed Consent
Informed consent does not apply in this study.
Funding
The study was supported by the Natural Science Foundation of Shanghai Municipal Commission of Health and Family Planning, 20124293.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Donglei Zhou and Xun Jiang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhou, D., Jiang, X., Jian, W. et al. Comparing the Effectiveness of Total Gastrectomy and Gastric Bypass on Glucose Metabolism in Diabetic Rats. OBES SURG 26, 119–125 (2016). https://doi.org/10.1007/s11695-015-1730-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-015-1730-7