Abstract
Background
To optimize bariatric surgery results, experts recommend regular practice of physical activity. However, no precise recommendations are available for the pre-surgical period. We aimed to evaluate, in this pilot study, the feasibility of a supervised Pre-Surgical Exercise Training (PreSET) and its short-term clinical impacts in subjects awaiting bariatric surgery.
Methods
In addition to the usual interdisciplinary lifestyle management, eight women and four men [40.8 (37.6–47.5) years old, BMI = 51.4 (43.8–53.1) kg/m2] underwent the PreSET, which combined both endurance and strength training. They were instructed to perform three physical activity sessions per week during 12 weeks, with at least two sessions per week on site and the possibility to complete missed sessions at home. Before and after the PreSET, anthropometric measures, body composition, physical fitness, quality of life, and physical exercise beliefs were assessed.
Results
The subjects participated in 57.3 % of the total supervised exercise sessions proposed and presented high satisfaction rates. Our program resulted in a significant improvement in weight (p = 0.007), physical fitness (p ≤ 0.05), and quality of life score (p = 0.012) as well as for the emotions, social interactions, and sexual life subscales (p < 0.03). Fear of injury (p = 0.028) and embarrassment during physical activity (p = 0.028) were significantly decreased, whereas no significant change in confidence in athletic ability and in beliefs in exercise benefits were noticed after the program.
Conclusions
PreSET is feasible in subjects awaiting bariatric surgery and, combined with an interdisciplinary management, results in several short-term benefits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity, considered as a worldwide epidemic by the WHO [1], is a major public health problem in North America. The class II and III of obesity are the weight classes that increased most rapidly over the past 25 years in Canada and USA [2, 3]. This alarming situation has significantly increased the number of bariatric interventions performed [4]. Bariatric surgery has demonstrated its long-term efficacy in maintaining significant weight loss and in lowering mortality [5, 6], while reducing the health-care costs of obesity [7, 8]. It also greatly improves comorbidities, quality of life, and physical capacity of individuals with severe obesity [7, 9–12]. In order to optimize the results of bariatric surgery and to decrease perioperative morbidity, various experts recommend the introduction of a healthier lifestyle, which may begin before or after surgery [13–15]. Thus, the regular practice of physical activity (PA) is strongly recommended in the multidisciplinary medical and surgical management of people with severe obesity. Indeed, the literature highlights that individuals who practice regular physical activity before and after surgery achieve better weight loss and maintenance [16–18]. In addition, a few interventional studies show that exercise training after bariatric surgery benefits both the health and physical fitness of the subjects with morbid obesity [19–22]. Recently, Parikh et al. concluded that the participation in a medically supervised weight management program that includes monthly behavior modification visits over 6 months did have a positive effect on physical activity practice postoperatively [23]. This study reinforces the recommendations, which advocate the modification of the practice of physical activity before surgery. In addition, according to Bond et al. [24], the motivation to participate in regular moderate physical activity and the involvement in various intensities of physical activity increased significantly close to the date of bariatric surgery compared to a measurement carried out 3 months earlier. Moreover, the effectiveness of bariatric surgery and the number of perioperative complications are influenced by various factors such as initial weight or physical fitness [25–27]. The pre-surgery period could thus be an ideal starting point for exercise training and lifestyle intervention, but evidences of the short- and long-term benefits of such programs should be strengthened before implementation. Knowing that the incorporation of exercise as a consistent lifestyle behavior is not easy for many individuals with obesity because of poor exercise tolerance and enjoyment [28–30], optimal interventions are necessary to improve these parameters in order to increase regular PA levels in individuals awaiting bariatric surgery. In addition, Brandenburg et al. concluded that after their pre-bariatric surgery behavior modification program, patients indicated that they would like more specific information about exercise provided by a trained exercise specialist [31]. However, to our knowledge, only two small studies in pre-bariatric surgery subjects have evaluated the effects of resistance exercise training during 4 weeks (n = 4) and the effects of 12 weeks of aquatic exercise intervention (n = 7) [32, 33].
Our pilot study thus aimed to evaluate the feasibility of a supervised Pre-Surgical Exercise Training (PreSET) and the short-term impacts of the PreSET combined with usual interdisciplinary lifestyle management in subjects awaiting bariatric surgery. We hypothesized that the 12-week PreSET plus the interdisciplinary lifestyle management will improve the subjects’ satisfaction, physical fitness, quality of life, and physical exercise beliefs.
Materials and Methods
Population
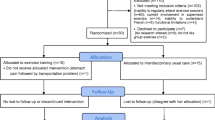
Participants were recruited in the medico-surgical clinic for the treatment of obesity of the Centre Hospitalier Universitaire de Sherbrooke (CHUS) in October and November 2011. The study was approved by the Institutional Ethics Review Board of research on humans of the CHUS and Université de Sherbrooke (project 11-120), and each subject provided written informed consent to participate in the study. Twelve bariatric surgery candidates [aged ≥18 years old; body mass index (BMI) ≥35 with comorbidities or ≥40 kg/m2], who were expected to be operated on within 3 to 6 months, and who practiced no regular supervised exercise training, were included in the study. Candidates were excluded if they were not able to regularly attend the supervised sessions, had medical contraindication to physical activity practice, had important functional limitations not allowing them to complete the 6-minute walking test (6MWT) or had uncontrolled neuropsychiatric illnesses. We contacted 31 subjects, of which three refused to participate and 16 were excluded due to their inability to regularly attend supervised sessions (n = 11), inability to understand French (n = 1), functional limitations (n = 1), early surgery date (n = 1), current involvement in supervised exercise (n = 1), and withdrawal from surgery waitlist (n = 1).
Experimental Design
Subjects were evaluated at baseline (visit 1 and 2) and after the 12 weeks of intervention (visit 3). During the first visit, a symptom-limited cardiac exercise test was performed using a treadmill. For the second and third visits, anthropometric variables, body composition, physical fitness, quality of life, and physical exercise beliefs were assessed. The satisfaction questionnaire was completed during the third visit at the end of the PreSET.
Intervention
Subjects continued to benefit from interdisciplinary usual care from the medico-surgical clinic for the treatment of obesity at the CHUS. This includes individual counselling sessions every 6–8 weeks with a dietitian and a physical activity specialist, and access to group educational sessions [34]. In addition to the interdisciplinary lifestyle management, they underwent the PreSET, which aimed to improve physical fitness using enjoyable activities without focusing on weight loss. The PreSET either lasted 12 weeks or was stopped 2 weeks before surgery because of the preoperative diet. After a needs and availability assessment, subjects were instructed to attend supervised evening exercise sessions in the gymnasium of the CHUS at least twice a week for the three sessions proposed and to complete the missed sessions at home. The physical exercise sessions consisted of 10 min of warm up, 30 min of endurance activity (treadmill, walking circuit, arm-ergocycle, elliptical), 20 to 30 min of strength exercises, and 10 min of cool-down period. The group sessions were supervised by a physical activity specialist and/or completed independently at home. The intensity of the endurance training was determined using the heart rate reserve (HRR) method [(peak HR − resting HR) × 55 to 85 % + resting HR] and using data from the previously performed symptom-limited cardiac treadmill test. The progression of endurance intensity and duration is shown in Table 1. Electronic pulse monitors (Polar F4™) were used to control endurance exercise intensity during supervised sessions and at home. Patients reported their HR in a logbook for each session realized.
Strength exercises were performed with small equipment easily available at home: dumbbells, elastic bands, and sticks. Three mini-circuits (upper body, lower body, and trunk) each associated with three exercises were repeated by subjects according to their prescription. The progression of series, repetitions, and load are presented in Table 2.
Subjects started their endurance and strength training at a difficulty level determined by the physical activity specialist according to their physical fitness and physical activity levels (Tables 1 and 2). The level of training was increased progressively according to the ease of performance. Moreover, for the exercise training at home, illustrated prescriptions and instructions for strength exercises were given in a workbook. To make the training more enjoyable, we proposed a variety of activities for the 30 min of endurance training including dance/aerobic exercises, badminton or ball games when suitable and collective games in warm-up. Subjects also participated in an aquagym session offered once a month based on the same modalities of exercise as the other exercise sessions.
Feasibility and Acceptability
The feasibility was evaluated using the attrition rate, the rate of sessions completed at home and/or at the hospital. A satisfaction questionnaire using five-point Likert scales evaluated acceptability.
Anthropometric Measures and Body Composition
Height was obtained using a standard stadiometer to the nearest 0.1 cm and body mass was measured to the nearest 0.1 kg with a calibrated scale (Tanita TBF-310®). Neck circumference was measured twice using a measurement tape placed horizontally above the Adam’s apple, while the investigator was facing the subject [35]. The mean of two measurements was used for analyses. Body mass index (BMI) was calculated as weight (kg) divided by squared height (m2). Body composition was measured with a bipodal bioelectrical impedance scale (Tanita TBF-310®) always at the same time of the day and in the conditions recommended by the manufacturer to improve reproducibility, i.e., not eating or drinking 4 h before the test, not having exercised in the last 12 h, urinating within 30 min before the test, standing for at least 10 min before the test, and not consuming alcohol in the last 48 h [36, 37].
Physical Fitness
A symptom-limited cardiac exercise test was performed to assess cardiac risk and to obtain peak HR for the determination of individualized endurance exercise intensity. After 1 min of warm-up at 1 mph, we used the modified Bruce treadmill protocol for 11 subjects and the Bruce protocol for one subject [38]. After reaching their maximum functional capacity, subjects finished with 2 min of active recovery at 1 mph and a passive recovery of 3 min of sitting. Test termination criteria included patient request, increasing chest or leg pain, abnormal cardiovascular parameters (i.e., abnormal electrocardiogram, hypertension, or hypotension), and patient reaching the predicted maximal HR (220 − age). HR and electrocardiogram tracing were recorded during the entire test under the surveillance of a cardiologist. Blood pressure measurements were taken manually at rest, at the end of each stage of exercise, and during the recovery period. The metabolic equivalent of task (MET) of the peak exercise was estimated from treadmill speed and elevation using the standardized equations [39], and the duration of effort was recorded.
The 6MWT, which has been validated in obese populations [40–42] and often used in individuals with morbid obesity [10, 12], was performed to evaluate functional capacity. As advised in the ATS statement [43], the test was administered on an indoor 30-m course and subjects were instructed to walk as far as they could in 6 min. To allow for potential learning effects, subjects unfamiliar with the 6MWT completed two tests, each separated by 30 min of rest. With a slight modification in the ATS guidelines, subjects were informed of the time elapsed when encouraged. After 6 min, the distance covered was measured to the nearest meter. Electronic pulse monitors (Polar F4™) were used to record HR at standing rest and throughout the test. Mean HR during the 6MWT was calculated from the HR recorded during the last 3 min. Heart cost that reflects relative exercise intensity was calculated using the 6MWT distance divided by 6MWT mean HR, as previously reported [44]. The 6MWT was performed at the same time of day before and after exercise training. The percentage of the theoretical 6MWT distance (6MWTD) reached was calculated using the regression equation [6MWD = 868.8 − (2.99 × age (years)) − (74.7 × gender), where men = 0 and women = 1] developed by Gibbons et al. [45] for the estimation of 6MWT distance in healthy individuals between 20 and 80 years of age.
Three different tests were used to assess muscular endurance of the upper and lower limbs: the sit-to-stand test, the half-squat test, and the arm curl test. The sit-to-stand test, which has already been used in individuals with morbid obesity [21], is a rapid test for assessing dynamic muscular endurance and dynamic balance [46, 47]. The subjects stand up and sit down on a chair as many times as possible in 30 s with their arms crossed on the chest to prevent their use for assistance. The number of full movement completed (buttocks against the chair and full extension of knees) during the 30 s is recorded as the score for this test.
The half-squat test, which to our knowledge has never been reported in subjects with morbid obesity, was performed to evaluate the leg muscle endurance because it avoids the pain caused by dynamic movements [48]. The subjects hold the position as long as possible this position: back against the wall, arms crossed on chest, and flexion of 90° between thighs and calves. The time the position was maintained was recorded.
The arm curl test was developed and validated in the elderly to assess the muscle strength of the upper limbs [49]. Given its simplicity and its use in population with decreased physical work capacity, we used it to evaluate the dynamic muscular endurance of the biceps in our population. The test aims to achieve the highest number of flexion–extension of the dominant arm within a 30-s time frame with a dumbbell of 2.3 kg for women and 3.6 kg for men. The number of full curls completed in 30 s with good form was recorded as the score for this test.
Health-Related Quality of Life (HRQOL)
HRQOL was assessed by the self-administered Laval questionnaire, validated in subjects with morbid obesity and sensitive to treatment-induced changes [50]. It includes 44 questions divided into six domains: symptoms, activity/mobility, personal hygiene/clothing, emotions, social interactions, and sexual life. The answers to each question are expressed on a Likert scale of seven points: the highest score means better HRQOL. We transformed these scores into percentage of maximal score for the analyses and created a total score by adding all the sub-scales’ scores.
Physical Exercise Beliefs
To assess the benefits and the psychological barriers perceived by our subjects, we used the Physical Exercise Belief Questionnaire (PEBQ), validated in a morbidly obese population [51], which focuses on the major psychological barriers encountered in individuals with obesity to practice physical activity [52]. We performed a French translation following WHO recommendations [53] using back-translation into English by an expert. This questionnaire, partly resulting from the Tampa scale for assessing kinesiophobia, consists of 16 questions divided into four areas: benefits of exercise, confidence in athletic ability and barriers to physical activity with embarrassment, and fear of injury. The answer to each question is expressed from 1 to 5: 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = somewhat agree, and 5 = strongly agree. We transformed these scores into percentages of maximal score for the analyses.
Statistical Analyses
The results are presented as median values (25–75th percentile). The normality of the samples was evaluated with histogram distribution which showed a non-Gaussian distribution for all parameters. The effects of training were tested with signed rank Wilcoxon tests. The percentage of attendance to the supervised exercise sessions was calculated by dividing the number of sessions realized in the hospital by the total number of supervised sessions proposed until the pre-surgery diet or the end of the program (12 weeks). The total percentage of exercise sessions realized was calculated by dividing the number of sessions realized (at home or at the hospital) by the number sessions required (3/week) until the pre-surgery diet or the end of the program. Data were analyzed with SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). The null hypothesis was rejected at p ≤0.05.
Results
Population
All 12 subjects, aged 40.8 (37.6–47.5) years old, had at least one comorbidity: five had hypertension, two dyslipidemia, two type 2 diabetes, eight sleep apnea, two osteoarthritis, one bipolar disorder, and one fibromyalgia. Eight subjects suffered from knee pain and two from back pain. One subject was a current smoker and five were former smokers. The vast majority lived in Sherbrooke and worked full time. Only three subjects did not practice at least 30 min of physical activity per day before the beginning of the PreSET.
Feasibility
No subject abandoned the PreSET before their bariatric surgery. We proposed 35 supervised exercise sessions in 12 weeks; seven subjects completed the full program duration and five had their bariatric surgery before the end of the program (after 5, 6, 7.5, 9.5, or 10.5 weeks of the PreSET). The subjects attended a median of 57.3 % (32.5–77.6 %) of the total supervised exercise sessions and 64.5 % (47.5–79.9 %) of the total exercise sessions required at home or at the hospital. Two subjects came only one time to the hospital and completed their exercise at home or a fitness center. The initial and final difficulty level of the subjects’ training are presented in Table 1 for endurance training and Table 2 for strength training. Each subject improved at least one level for endurance training and two levels for strength training during the program. The increase obviously appears greater in subjects who trained longer. All the patients were very satisfied or satisfied by the coaching and the advices provided by the physical activity specialist during the lifestyle management and the PreSET. They were also satisfied with the training infrastructure, the duration, the frequency, the intensity, and the level of difficulty of the PreSET. However, we noticed that 8.3 % of subjects were only moderately satisfied by the evening schedule and 16.7 % by the available materials. They would have liked at least one session of exercises during the day and more treadmills and ergocycles.
Anthropometric and Body Composition
The effects of the intervention on anthropometric measures and body composition parameters are shown in Table 3. There was a significant decrease of 3.9 % of the initial body weight, accompanied by a decrease in fat mass.
Physical Fitness
All the subjects completed the baseline symptom limited treadmill test with a median duration of 11.5 (11.1–12.4) min, representing an effort of 9.9 (9.3–10.7) METS. No major cardiac complication preventing the subjects to practice physical activity was noted. The results of the evaluations of physical fitness are presented in Table 4. Data for these tests are missing for one subject in post-training since he was already in pre-surgery diet and consequently too exhausted to realize his final physical fitness evaluation. No subject reached the theoretical 6MWTD (Table 4). The 6MWTD, theoretical 6MWTD reached, heart cost, time of half-squat test, and the number of flexion during the arm curl test were all significantly increased (p ≤ 0.05) after our intervention, but no significant variation in the number of lifts during the sit-to-stand test was noticed (Table 4).
Health-Related Quality of Life
We noted a significant improvement in the total HRQOL (p = 0.012), emotions (p = 0.002), social interactions (p = 0.025), and sexual life (p = 0.003) scores. However, no significant change in symptoms (p = 0.25), activity/mobility (p = 0.07), and personal hygiene/clothing (p = 0.078) scores was observed after our intervention (Fig. 1).
Physical Exercise Beliefs
Fear of injury (p = 0.03) and embarrassment during physical activity (p = 0.03) were significantly decreased, whereas no significant change in confidence in athletic ability (p = 1) and in beliefs in exercise benefits (p = 0.24) were noticed after our program (Fig. 2).
Fear of injury, embarrassment during physical activity, confidence in athletic ability, and beliefs in exercise benefits before and after the supervised exercise training in 12 subjects awaiting bariatric surgery. PreSET Pre-surgical Exercise Training; *p < 0.03. Data are presented as median (25–75th percentile)
Discussion
Our results show that our PreSET is feasible and acceptable since subjects participated in almost 60 % of the supervised exercise sessions proposed and presented a great satisfaction rate. The PreSET, in addition to an interdisciplinary lifestyle management, resulted in short-term significant improvements in weight, physical fitness indicators, quality of life, emotions, social interactions and sexual life scores, and fear of injury and embarrassment during physical activity.
There are no standardized guidelines to determine the appropriate type and amount of physical activity for the preoperative bariatric surgery patients. Our results suggest that our program was well received by the participants as no subject abandoned, all the patients were satisfied, and a good attendance rate (64.5 % including sessions completed at home) was noted. Previous studies have reported an attendance rate for exercise training ranging from 46 % to 93 % among people with morbid obesity [22, 54, 55]. The different modalities of exercise (group vs. individual, low vs. high practice frequency) and accessibility to facilities may explain the variation between the studies. In addition, we suspect that it was difficult for participants to complete the replacement exercise sessions at home since the percentage of total exercise sessions was modestly improved compared to the percentage of the supervised exercise sessions (64.5 % vs. 57.3 %).
Weight loss was not our primary goal, as our team focused on improving pre-surgery fitness, healthy lifestyle habits, and weight maintenance. However, the subjects still experienced a modest weight loss (−3.9%; −4.1 kg) explained by a decrease in fat mass, with no significant change in fat free mass. Our results are in accordance with the literature, which indicates that weight loss induced by physical activity alone in obese populations ranges from 0.1 kg to 5.2 kg, with most studies showing weight loss of only 1 to 3 kg [56]. The fact that our result is in the higher range might be explained by the combination of individualized intervention by the interdisciplinary team and the PreSET.
Our population presented a decreased 6MWTD compared to healthy subjects of the same age since they reached only 69.4 % of their theoretical walking distance. This difference can be explained by obesity, reduced aerobic capacity, sedentary lifestyle, and perceived discomfort and pain during walking [29]. However, the subjects included in our study had good fitness capacity compared to the entire population with morbid obesity. Indeed, two studies have found that subjects awaiting bariatric surgery reached respectively only 55 % and 60 % of the normative values [10, 57]. This difference can be explained by our participants’ motivation to practice regular physical activity and their absence of medical contraindication. Nevertheless, the 6MWTD in our study are in the same range with that in the other studies which proposed supervised exercise training in people with morbid obesity (432.0–492.6 m) [19, 32].
Many physical fitness indicators (6MWTD, theoretical 6MWTD reached, heart cost, time of half-squat test, and the number of flexion during the arm curl test) were significantly improved after our intervention. The increase of 28 m during the 6MWT after the intervention is difficult to compare with the other two studies proposing exercise training before bariatric surgery [32, 33] since they do not specify the exact methodology of the 6MWT and have a very small number of subjects. This increase can be considered clinically significant based on recent studies of patients with chronic obstructive pulmonary disease or coronary artery disease, which found a 6MWT improvement of 25 m to be the minimal clinically significant improvement [58, 59]. However, this should be interpreted with caution since the minimal clinically significant distance for 6MWT improvement has not yet been established in morbidly obese subjects. Considering all these results, we conclude that our intervention resulted in increased physical fitness in subjects awaiting bariatric surgery, which is an important consideration in obesity treatment. Indeed, epidemiological data have shown that higher physical fitness was associated with reduced risk of cardiovascular disease and premature mortality in individuals with obesity [60].
After training, we observed a significant increase in the total HRQOL, emotions, social interactions, and sexual life scores. Similar to our findings, other studies reported an improvement in HRQOL after interdisciplinary rehabilitation or exercise training in individuals with morbid obesity [33, 61]. The greatest improvement was noted in emotions, social interactions, and sexual life scores. This may be explained by the fact that the initial scores in these categories were the most impaired compared to the other HRQOL scores. It also reinforces the evidence on the benefit of exercise on the psychosocial dimensions. Moreover, group exercise training could play a key role in these improvements since it created social relationships and a support network between people with similar conditions. Such improvements in HRQOL are particularly relevant for subjects with obesity who presented an impaired HRQOL [62]. However, no significant change in symptoms, activity/mobility, and personal hygiene/clothing scores was observed after our intervention probably because of our limited sample size or the absence of massive weight loss, which is considered as an essential component of the improvement in HRQOL [9, 10, 63].
We found a significant decrease in the fear of injury and embarrassment during physical activity after our intervention without a significant change in confidence in athletic ability and in beliefs in exercise benefits. After 6 weeks of aquajogging in obese subjects, Wouters et al. [64] concluded that a significant improvement in exercise embarrassment and perceptions of exercise benefits, but not in the fear of injury and confidence in athletic ability, was observed. The fact that we found a decrease in fear of injury contrary to this study may be due to a longer intervention, which proposed different types of physical activities and individual meetings to help change lifestyle. Our population presented a high percentage of beliefs in exercise benefits at baseline and after the intervention. This may partly explain our subjects’ willingness to participate in this study. Therefore, we think that beliefs related to exercise benefits are not necessarily a barrier to the practice of physical activity. As previously shown by Wouters et al. [64], no significant increase in confidence was noticed after our program. Massive weight loss may be an essential component of the improvement in confidence since bariatric surgery increases the confidence in athletic ability, like the other physical exercise beliefs [65].
Our study is the first study to examine the feasibility and positive impacts of a supervised exercise training on endurance and strength in subjects awaiting bariatric surgery. However, several limitations should be considered when interpreting results. First, because of the small sample size of this pilot study and the elevated motivation to practice physical activity of the subjects, the findings might not be generalizable to the whole obese population awaiting bariatric surgery. Second, the PreSET requires regular visits to the hospital and therefore is limited to the subjects who were able to come frequently to the facility. Third, it was impossible to distinguish the specific effects of the PreSET from that of the usual care due to the absence of a control group. Finally, the duration of participation in PreSET varied because it was not possible to know in advance the surgery date. This makes it difficult to conclude on the optimal training duration and may have reduced the effects of our intervention.
Conclusion
Our data suggest that the 12-week PreSET is feasible and acceptable to morbidly obese patients. When combined with an interdisciplinary lifestyle management, it is effective in improving patient’s weight, physical fitness, HRQOL, and physical exercise beliefs in subjects awaiting bariatric surgery. Controlled studies with larger cohorts are now required to confirm these findings and demonstrate the relevance of the interdisciplinary lifestyle management with supervised exercise training for the individuals awaiting bariatric surgery. Post-surgery outcome evaluations and follow-up is equally necessary to eventually determine if pre-surgical exercise training may impact on the recovery, the lifestyle, and the health of the patients in the post-surgery period.
References
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii, 1–253.
Tjepkema M. Measured Obesity Adult obesity in Canada: Measured height and weight. Nutrition: Findings from the Canadian Community Health Survey. 2005: Statistics Canada Catalogue.
Sturm R. Increases in morbid obesity in the USA: 2000–2005. Public Health. 2007;121:492–6.
Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2008. Obes Surg. 2009;19:1605–11.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–52.
Picot J, Jones J, Colquitt JL, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13:1–190, 215–357, iii–iv.
Sampalis JS, Liberman M, Auger S, et al. The impact of weight reduction surgery on health-care costs in morbidly obese patients. Obes Surg. 2004;14:939–47.
Karlsson J, Taft C, Ryden A, et al. Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: the SOS intervention study. Int J Obes (Lond). 2007;31:1248–61.
Tompkins J, Bosch PR, Chenowith R, et al. Changes in functional walking distance and health-related quality of life after gastric bypass surgery. Phys Ther. 2008;88:928–35.
Maniscalco M, Zedda A, Giardiello C, et al. Effect of bariatric surgery on the six-minute walk test in severe uncomplicated obesity. Obes Surg. 2006;16:836–41.
de Souza SA, Faintuch J, Fabris SM, et al. Six-minute walk test: functional capacity of severely obese before and after bariatric surgery. Surg Obes Relat Dis. 2009;5:540–3.
Mechanick JI, Kushner RF, Sugerman HJ, et al. American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery Medical Guidelines for Clinical Practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Surg Obes Relat Dis. 2008;4:S109–84.
Poirier P, Cornier MA, Mazzone T, et al. Bariatric surgery and cardiovascular risk factors: a scientific statement from the American Heart Association. Circulation. 2011;123:1683–701.
Blackburn GL, Hutter MM, Harvey AM, et al. Expert panel on weight loss surgery: executive report update. Obesity (Silver Spring). 2009;17:842–62.
Jacobi D, Ciangura C, Couet C, et al. Physical activity and weight loss following bariatric surgery. Obes Rev. 2011;12:366–77.
Metcalf B, Rabkin RA, Rabkin JM, et al. Weight loss composition: the effects of exercise following obesity surgery as measured by bioelectrical impedance analysis. Obes Surg. 2005;15:183–6.
Livhits M, Mercado C, Yermilov I, et al. Exercise following bariatric surgery: systematic review. Obes Surg. 2010;20:657–65.
Castello V, Simoes RP, Bassi D, et al. Impact of aerobic exercise training on heart rate variability and functional capacity in obese women after gastric bypass surgery. Obes Surg. 2011;21:1739–49.
Shah M, Snell PG, Rao S, et al. High-volume exercise program in obese bariatric surgery patients: a randomized, controlled trial. Obesity. 2011;19:1826–34.
Stegen S, Derave W, Calders P, et al. Physical fitness in morbidly obese patients: effect of gastric bypass surgery and exercise training. Obes Surg. 2011;21:61–70.
Shang E, Hasenberg T. Aerobic endurance training improves weight loss, body composition, and co-morbidities in patients after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2010;6:260–6.
Parikh M, Dasari M, McMacken M, et al. Does a preoperative medically supervised weight loss program improve bariatric surgery outcomes? A pilot randomized study. Surg Endosc. 2012;26:853–61.
Bond DS, Evans RK, DeMaria E, et al. Physical activity and quality of life improvements before obesity surgery. Am J Health Behav. 2006;30:422–34.
McCullough PA, Gallagher MJ, Dejong AT, et al. Cardiorespiratory fitness and short-term complications after bariatric surgery. Chest. 2006;130:517–25.
Hatoum IJ, Stein HK, Merrifield BF, et al. Capacity for physical activity predicts weight loss after Roux-en-Y gastric bypass. Obesity (Silver Spring). 2009;17:92–9.
Flum DR, Belle SH, King WC, et al. Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med. 2009;361:445–54.
Ekkekakis P, Lind E. Exercise does not feel the same when you are overweight: the impact of self-selected and imposed intensity on affect and exertion. Int J Obes (Lond). 2006;30:652–60.
Hulens M, Muls E, Lysens R, et al. Predictors of 6-minute walk test results in lean, obese and morbidly obese women. Scand J Med Sci Sports. 2003;13:98–105.
Gallagher MJ, Franklin BA, Ehrman JK, et al. Comparative impact of morbid obesity vs heart failure on cardiorespiratory fitness. Chest. 2005;127:2197–203.
Brandenburg D, Kotlowski R. Practice makes perfect? Patient response to a prebariatric surgery behavior modification program. Obes Surg. 2005;15:125–32.
Adair JD, Wollner SB, DaCosta ME, et al. Progressive resistance training for patients with class III obesity. Obesity and Weight Management. 2010;6:115–18.
Funderburk JA, Callis S. Aquatic intervention effect on quality of life prior to obesity surgery: a pilot study. Annu Ther Recreation. 2010;18:66–78.
Gagnon C, Brown C, Couture C, et al. A cost-effective moderate-intensity interdisciplinary weight-management programme for individuals with prediabetes. Diabetes Metab. 2011;37:410–8.
Ben-Noun L, Sohar E, Laor A. Neck circumference as a simple screening measure for identifying overweight and obese patients. Obes Res. 2001;9:470–7.
Jebb SA, Cole TJ, Doman D, et al. Evaluation of the novel Tanita body-fat analyser to measure body composition by comparison with a four-compartment model. Br J Nutr. 2000;83:115–22.
Boneva-Asiova Z, Boyanov MA. Body composition analysis by leg-to-leg bioelectrical impedance and dual-energy X-ray absorptiometry in non-obese and obese individuals. Diabetes Obes Metab. 2008;10:1012–8.
Bruce RA, Blackmon JR, Jones JW, et al. exercising testing in adult normal subjects and cardiac patients. Pediatrics. 1963;32:742–56.
American College of Sports Medicine Guidelines for Exercise Testing and Prescription. 2010; 8th ed. Baltimore: Williams & Wilkins.
Baillot A, Vibarel-Rebot N, Lecoq A, et al. Six-minute walking test in obese female: reproducibility, relative intensity and relationship with quality of life. Sci Sports. 2009;24:1–8.
Beriault K, Carpentier AC, Gagnon C, et al. Reproducibility of the 6-minute walk test in obese adults. Int J Sports Med. 2009;30:725–7.
Larsson UE, Reynisdottir S. The six-minute walk test in outpatients with obesity: reproducibility and known group validity. Physiother Res Int. 2008;13:84–93.
ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7.
Baillot A, Vibarel-Rebot N, Amiot V, et al. Effects of an 8-week aerobic exercise training on saliva steroid hormones, physical capacity, and quality of life in diabetic obese men. Horm Metab Res. 2012;44:146–51.
Gibbons WJ, Fruchter N, Sloan S, et al. Reference values for a multiple repetition 6-minute walk test in healthy adults older than 20 years. J Cardiopulm Rehabil. 2001;21:87–93.
Bohannon RW. Sit-to-stand test for measuring performance of lower extremity muscles. Percept Mot Skills. 1995;80:163–6.
Guralnik JM, Seeman TE, Tinetti ME, et al. Validation and use of performance measures of functioning in a non-disabled older population: MacArthur studies of successful aging. Aging (Milano). 1994;6:410–9.
McIntosh G, Wilson L, Affleck M, et al. Trunk and lower extremity muscle endurance: normative data for adults. J Rehabil Outcome Measures. 1998;2:20–39.
Dunsky A, Ayalon M, Netz Y. Arm-curl field test for older women: is it a measure of arm strength? J Strength Cond Res. 2011;25:193–7.
Therrien F, Marceau P, Turgeon N, et al. The laval questionnaire: a new instrument to measure quality of life in morbid obesity. Health Qual Life Outcomes. 2011;9:66.
Larsen JK, Geenen R, van Ramshorst B, et al. Binge eating and exercise behavior after surgery for severe obesity: a structural equation model. Int J Eat Disord. 2006;39:369–75.
Biddle SJ, Fox KR. Motivation for physical activity and weight management. Int J Obes Relat Metab Disord. 1998;22 Suppl 2:S39–47.
World Health Organisation. Process of translation and adaptation of instruments. 2012. (14/05/2012).http://www.who.int/substance_abuse/research_tools/translation/en/
Annesi JJ, Gorjala S. Changes in theory-based psychological factors predict weight loss in women with class III obesity initiating supported exercise. J Obes. 2010;2010:1–4.
Annesi JJ. Relations of mood with body mass index changes in severely obese women enrolled in a supported physical activity treatment. Obesity Facts. 2008;1:88–92.
Catenacci VA, Wyatt HR. The role of physical activity in producing and maintaining weight loss. Nat Clin Pract Endocrinol Metab. 2007;3:518–29.
Tessier A, Zavorsky GS, Kim do J, et al. Understanding the determinants of weight-related quality of life among bariatric surgery candidates. J Obes. 2012;2012:713426.
Gremeaux V, Troisgros O, Benaim S, et al. Determining the minimal clinically important difference for the six-minute walk test and the 200-meter fast-walk test during cardiac rehabilitation program in coronary artery disease patients after acute coronary syndrome. Arch Phys Med Rehabil. 2011;92:611–9.
Holland AE, Hill CJ, Rasekaba T, et al. Updating the minimal important difference for six-minute walk distance in patients with chronic obstructive pulmonary disease. Arch Phys Med Rehabil. 2010;91:221–5.
Katzmarzyk PT, Church TS, Janssen I, et al. Metabolic syndrome, obesity, and mortality: impact of cardiorespiratory fitness. Diabetes Care. 2005;28:391–7.
Clini E, Prato F, Nobile M, et al. Interdisciplinary rehabilitation in morbidly obese subjects: an observational pilot study. Monaldi Arch Chest Dis. 2006;65:89–95.
Duval K, Marceau P, Lescelleur O, et al. Health-related quality of life in morbid obesity. Obes Surg. 2006;16:574–9.
Kolotkin RL, Crosby RD, Gress RE, et al. Two-year changes in health-related quality of life in gastric bypass patients compared with severely obese controls. Surg Obes Relat Dis. 2009;5:250–6.
Wouters EJ, Van Nunen AM, Geenen R, et al. Effects of aquajogging in obese adults: a pilot study. J Obes. 2010;2010:1–7
Wouters EJ, Larsen JK, Zijlstra H, et al. Physical activity after surgery for severe obesity: the role of exercise cognitions. Obes Surg. 2011;21:1894–9.
Acknowledgments
The investigators aregrateful to the subjects for their cheerful participation. In addition, we thank the healthprofessional of the clinique medico-chirurgicale du traitement de l’obésité of the CHUS.We appreciate the contribution of Katherine Boisvert-Vigneault, student in SherbrookeUniversity (Canada) and Marine Asselin, student in Orléans University (France) for helpwith the supervised exercise training. Marie-France Langlois is the recipient of careeraward from the Fonds de la recherche Québécois en santé (FRQ-S). The Étienne-LeBelClinical Research Center is an FRQ-S funded research center.
Conflict of interest
The other authors declared no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baillot, A., Mampuya, W.M., Comeau, E. et al. Feasibility and Impacts of Supervised Exercise Training in Subjects with Obesity Awaiting Bariatric Surgery: a Pilot Study. OBES SURG 23, 882–891 (2013). https://doi.org/10.1007/s11695-013-0875-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-013-0875-5