Abstract
Background
There is a growing consensus that bariatric surgery is currently the most efficacious and long-term treatment for clinically severe obesity. However, it remains to be determined whether poor physical fitness, an important characteristic of these patients, improves as well. The purpose of this pilot study is to investigate the effect of gastric bypass surgery on physical fitness and to determine if an exercise program in the first 4 months is beneficial.
Methods
Fifteen morbidly obese patients (BMI 43.0 kg/m2) were tested before and 4 months after gastric bypass surgery. Eight of them followed a combined endurance and strength training program. Before and after 4 months the operation, anthropometrical characteristics were measured, and an extensive assessment of physical fitness (strength, aerobic, and functional capacity) was performed.
Results
Large-scale weight loss through gastric bypass surgery results in a decrease in dynamic and static muscle strength and no improvement of aerobic capacity. In contrast, an intensive exercise program could prevent the decrease and even induced an increase in strength of most muscle groups. Together with an improvement in aerobic capacity, functional capacity increased significantly. Both groups evolved equally with regard to body composition (decrease in fat mass and fat-free mass).
Conclusions
An exercise training program in the first 4 months after bariatric surgery is effective and should be promoted, considering the fact that physical fitness does not improve by weight loss only.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number of bariatric surgery procedures has increased significantly over the past few decades, not only in the USA but also worldwide [1]. Two major reasons can be defined. First, the prevalence of morbid obesity increases rapidly, approaching 8% for some populations in the USA [2]. Secondly, there is a growing consensus that bariatric surgery is currently the most efficacious and long-term treatment for clinically severe obesity, accompanied with a low mortality rate [3–5]. Morbid obesity is associated with a number of comorbidities such as hypertension, dyslipidemia, type-2 diabetes or insulin resistance, sleep apnea, etc. [6–8]. In addition to fat mass reduction, bariatric surgery has pronounced effects on these comorbidities [3, 9], even before weight loss occurs [10, 11].
However, it remains to be determined whether poor physical fitness, a key factor in the vicious circle of obesity and physical inactivity [12] and an important characteristic of morbidly obese patients [13, 14], improves as well after bariatric surgery. There are some reasons to assume that this is not self-evident. To answer this question, we must keep in mind that physical fitness is a broad concept that covers not only muscle strength but also functional and aerobic capacity. First of all, we do know that large-scale weight loss always results in a decrease in fat-free mass (FFM). Carey et al. [15] reported that FFM loss accounts for 30–35% of the total weight loss over the first 6 months as a consequence of Roux-en-Y Gastric bypass. We can presume that the high amount of weight loss, the malabsorptive characteristic of the procedure, and the inadequate protein intake [16] induce this skeletal muscle atrophy, with a concomitant decrease in muscle strength. Muscle strength is an important aspect of functional capacity, e.g., knee extensor muscle strength has been associated with gait speed, stair climbing, getting up from a seated position, postural stability, and even to the occurrence of falls in a number of investigations [17, 18]. Maffiuletti et al. [19, 20] indicated the importance of a decreased relative knee extensor muscle strength in terms of body weight in obese patients by contributing to reduced functional capacity during daily living activities. Until today, only two articles have been published to evaluate changes in functional capacity following bariatric surgery. A prospective 1-year study by Maniscalco et al. [21] showed an improvement of the distance walked in 6 min (6MWD) from 475.7 to 626.3 m in 15 female morbidly obese patients 1 year after laparoscopic adjustable gastric banding. Tompkins et al. [22] confirmed these results and added normative values, namely presurgical walking distance was 55% of normative values and improved up to 75% 6 months after the operation. Both studies conclude that functional capacity improves because the 6-min walking distance improves. The main reason is that less adipose tissue around the legs is more mechanically efficient, which makes walking less exhausting. Additionally, they suggest that aerobic capacity improves as well. However, we believe that this is partly true. Poor aerobic fitness in morbidly obese subjects is explained by both reduced cardiovascular function [23] as well as a low oxidative capacity of skeletal muscle [24–26]. Indeed, weight loss ameliorates cardiovascular function, but this cannot be adopted for the oxidative capacity of the obese muscle. It is known that weight loss alone, accomplished by low-calorie diets, does not improve mitochondrial content and electron chain transport activity in skeletal muscle of sedentary obese subjects [27], it even decreases mitochondrial size. Further, a high proportion of fast glycolytic type II muscle fibers and thus a low portion of oxidative type I muscle fibers are characteristic for the obese muscle [28]. Again, weight loss alone cannot change skeletal muscle fiber type. Therefore, there is no reason to assume that the extreme poor aerobic capacity will improve by gastric bypass surgery alone.
A first goal of the present study is to investigate the effect of gastric bypass surgery on physical fitness with a many-sided physical performance battery (muscle strength, aerobic, and functional capacity).
An additional goal of this study is to examine the feasibility and effectiveness of an exercise program in morbidly obese patients after gastric bypass surgery. To our knowledge, no studies have been reported that examine the effect of aerobic and resistance exercise in the period following bariatric surgery. Rice et al. [29] and Janssen et al. [30] reported that a low-calorie diet (energy deficit of 1,000 kcal/day) combined with either aerobic exercise or resistance exercise results in respectively an increased aerobic capacity (VO2 max) and muscle strength in lower and upper body. The diet group without exercise had no amelioration in aerobic capacity nor in muscle strength; furthermore, a significant loss of FFM was present while not in the exercise groups. It remains to be determined whether these data on low-calorie diets can be extrapolated toward the first postoperative period following gastric bypass surgery. We, therefore, hypothesize that exercise training during the months following a gastric bypass procedure can improve aerobic capacity and prevent the decline in muscle mass and muscle strength, with implications to functional impairment.
Materials and Methods
Subjects
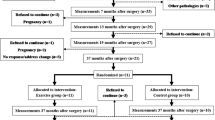
Nineteen gastric bypass patients were recruited for the study after checking the exclusion and inclusion criteria. Exclusion criteria were diabetes, severe cardiovascular diseases, and exercise-limiting comorbidities such as musculoskeletal impairments. To be included, patients must undergo gastric bypass surgery, a mixed restrictive and malabsorptive form of bariatric surgery. Also, conversions from a gastric banding to a gastric bypass procedure were allowed. The subjects gave their informed consent, and the study was approved by the local Ethics Committee (Ghent University Hospital, Ghent, Belgium).
All patients were able to make the choice between the intervention group (exercise program after gastric bypass “GB+E,” “the trained patients”) or the control group (only gastric bypass “GB,” “the untrained patients”). There was a dropout of four patients (two of GB and two of GB+E), so that finally, 15 morbidly obese patients (BMI 42.5 ± 6.6 kg/m2, age 40.5 ± 8.1 years, four men and 11 women) finished the study, of which seven patients in “GB” and eight patients in “GB+E.” The characteristics of the groups are shown in Table 1.
Reasons of refusal were domicile distance and a demanding job and household. Reasons of dropout were also a demanding job, household, or education.
Study Protocol
Both the patients of “GB” and “GB+E” underwent the same measurements before and 4 months after the operation. Only the patients of “GB+E” started 1 month after the operation with an exercise program during 3 months.
Exercise Program
The patients in group “GB+E” exercised three times a week for 12 weeks (36 sessions). Each training session lasted 75 min and included 10 min of cardiovascular warming up, 25 min of strength training, 30 min of endurance training, and 10 min of cooling-down period. During each session, patients were individually guided and supervised by Masters in Movement and Rehabilitation Sciences.
Strength exercises were performed using stack-weight equipment (elbow flexion and extension and knee flexion and extension). Intensity of strength training was calculated from one repetition maximum (1RM) values. The starting level was 60% of 1RM, which increased up to 75% of 1RM. Patients were habituated to the exercises and equipment during the first three training sessions. In the next 15 sessions, two sets of 15 repetitions at 60% of 1RM were done. In the final 18 sessions, three sets of 10 repetitions at 75% were done. Resting periods between repetition sets were approximately 60 s.
Endurance training consisted of cycling (10 min), walking (10 min), and stepping (10 min). Exercise intensity was initially set at 60% of heart rate reserve (HRR, defined as the difference between resting heart rate and peak heart rate) and was gradually increased up to 75% of HRR at the end of the training period. Stationary bicycles, treadmills, and steppers were used in a rehabilitation training room of the University Hospital of Ghent (Belgium). During the training sessions, heart rate was monitored by Polar Heart Watches.
Measurements
-
1.
Anthropometric variables and body composition
BMI (weight/ height2) and waist circumference (at the level of the biggest circumference, near the umbilicus) were determined using a digital balance scale, a stadiometer, and a tape meter. Body composition was assessed by bio-impedance (Bodystat 1500 MDD; Bodystat Ltd., Douglas, Isle of Man, UK). Patients were in supine position for at least 5 min. Surface electrodes were attached to the right hand (red lead: behind the knuckle of the middle finger; black lead: on the wrist to the ulnar head) and foot (red lead: behind the second toe next to the big toe; black lead: On the ankle at the level of and between the medial and lateral malleoli). Total body water (TBW) was calculated from the measured impedance using the following gender-specific formula: females: TBW = 0.382 × (height2/impedance) + 0.105 × bodyweight + 8.315 and men: TBW = 0.396 × (height2/impedance) + 0.143 × bodyweight + 8.399 [31]. FFM was then calculated from the TBW by assuming 73.2% hydration of FFM: FFM = TBW/0.732 [32]. Body fat mass (FM) was calculated using a two compartment model: body weight = FFM + FM.
-
2.
Physical fitness test battery
-
a.
Dynamic muscle strength
1RM was determined unilaterally with the indirect Holten method using commercially available stack weight and fitness equipment for biceps, triceps, quadriceps, and hamstrings. For each patient, a test weight was defined so that patients would be able to achieve maximal six to 12 repetitions. From this number of repetitions, the 1RM was calculated using the Holten diagram. The Holten diagram relates the number of repetitions to the percentage of maximum strength. The global score (kg) for the biceps, triceps, quadriceps, and hamstrings exercise was calculated by taking the sum of the right and left arm or leg.
-
b.
Static muscle strength
Static muscle strength was evaluated by measuring the handgrip strength with a handgrip dynamometer (JAMAR). Subjects were standing in the anatomical position, with the arm flexed at 90°, without touching the body. The participant was asked to squeeze as hard as possible. Three trials were made with a pause of about 10–20 s between each trial to avoid the effects of muscle fatigue. Left and right hand were alternated. The best score (in kilograms) was registered.
-
c.
Muscle fatigue
The participant was in the same position as described in “b. static muscle strength.” He/she had to squeeze the dynamometer with the strongest hand (determined in b) with as much force as possible and as long as possible. The test was finished when grip strength dropped to 50% of its maximum during sustained contraction. The seconds were registered.
-
d.
Functional capacity
-
Sit-to-stand STS test
This test measured the maximum number of times that a patient could rise to a full stand from a seated position within 30 s, without pushing off with the arms. The number of completed stands (up–down) was considered the patient’s score. This assessment has high test–retest reliability.
-
6MWD
All patients performed a standardized, self-paced 6MWD in a 20-m long corridor. They were instructed to cover as much distance as possible within 6 min without running. Patients were allowed to stop at every moment of the test but were encouraged to restart as soon as possible. During the test, patients were instructed as described by Enright et al. [33]. Covered distance after 6 min was measured to the nearest meter. Heart rates were monitored during the test by Polar Heart Watches.
-
-
e.
Maximal cardiopulmonary exercise test
Patients performed a maximal cardiopulmonary bicycle test on a cyclo-ergometer (Gymna). A gradual protocol was used, starting at 30 W with gradual increase of 15 W/min, with the subjects cycling at 60–70 rpm. Patients continued cycling until self-determined limits of their functional capacities or until the physician stopped the test because of potentially threatening symptoms. After the patients reached their maximum, subjects cycled during 3 min for active recovery at 1/3 of their maximal work load. Heart rates were continuously determined by electrocardiogram, whereas blood pressure was measured with a manual sphygmomanometer every 2 min. During the test, gas exchange was measured continuously using a portable mixing chamber system (MetaLyzer II, Cortex, Leipzig, Germany). The oxygen consumption (VO2), carbon dioxide production (VCO2), minute ventilation (VE), and respiratory exchange ratio (RER) were registered every 30 s. Peak VO2 is determined as the highest attained VO2 over 30 s during the test and expressed in both absolute values (peak VO2, ml/min), relative to body weight (peak VO2/kgBW, ml/kg/min), and relative to fat-free mass (peak VO2/kg FFM, ml/kg/min). The ventilatory equivalent method was used to determine the ventilatory anaerobic threshold (VAT), described by Wasserman [34]. This is based on the principle that ventilation increases promptly at the anaerobic threshold in proportion to the increase in CO2 produced from HCO −3 buffering of lactic acid. This results in an increase in the ventilatory equivalent for O2 (VE/VO2) without an increase in the ventilatory equivalent for CO2 (VE/VCO2). The time of occurrence (seconds) of VAT, together with the workload (power output) and oxygen uptake at that moment, are registered.
-
a.
Statistical Analyses
Interaction and time effects were evaluated using a repeated-measures ANOVA. To evaluate time effects within groups, paired t tests were performed. Data are expressed as mean (± standard deviation) and are analyzed with a commercially available statistical software program (SPSS 16.0, SPSS Inc, Chicago, IL, USA). Data are significant when p < 0.05.
Results
Anthropometric Variables and Body Composition Pre- and 4 Months Postoperative
The trained patients (GB+E) as well as the untrained patients (GB) had the same decrease in weight (GB = −26.6 ± 14.6 kg; GB+E = −22.7 ± 5.7 kg), BMI (GB = −8.3 ± 4.1 kg/m2; GB = −8.1 ± 2.5 kg/m2), and waist circumference (GB = −20.3 ± 11.6 cm; GB+E = −17.2 ± 8.1 cm). Weight loss resulted largely from significant decrease not only in fat mass (GB = −19.0 ± 10.2 kg; GB+E = −17.3 ± 4.6 kg) but also in fat-free mass (GB = −7.6 ± 4.7 kg; GB+E = 5.4 ± 2.6 kg) decreased significantly 4 months after the gastric bypass operation. No interaction effects were found (Table 2).
Results of the Physical Fitness Test Battery
Muscle Strength
The untrained patients (GB) had a pronounced decrease in dynamic muscle strength 4 months after the operation. They lost 16% of their quadriceps strength, 36% of their biceps strength, and 39% of their triceps strength. By contrast, an exercise program (strength+endurance) could prevent this decrease concerning biceps strength (Pre = 21.8 ± 8.0 kg; Post = 25.9 ± 13.0 kg) and triceps strength (Pre = 24.3 ± 10.1 kg; Post = 30.7 ± 23.0 kg) and even increased quadriceps strength with 72% and hamstrings strength with 27%.
Static muscle strength, measured as handgrip strength, decreased in both GB and GB+E 4 months after gastric bypass surgery, respectively, with 18% and 7%. No interaction effects could be reported (Table 3).
Muscle fatigue, also measured with the handgrip dynamometer, was not influenced by gastric bypass surgery, nor by an additional exercise program.
Functional Capacity
Patients were also subjected to two tests that evaluated functional capacity. There was a tendency for an interaction effect concerning the sit-to-stand (STS) test (p = 0.08). The trained patients (GB+E) improved their number of times to rise to a full stand from a seated position within 30 s (Pre = 13 ± 3 times to Post = 16 ± 4 times; p = 0.045), whereas the untrained patients (GB) did not (Pre = 15 ± 4 times to Post = 15 ± 3 times; p = 0.862). The 6-min-walk distance, another important test that evaluates functional capacity, improved for both groups together. Further analyses showed us that the increase in the 6MWD is mainly attributed to the increase in the training intervention group, namely GB+E = +52 ± 30 m and GB = +30 ± 68 m. The heart frequency on the end of the 6MWD declined significantly for both groups.
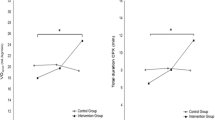
(Maximal) Aerobic Capacity
In the maximal bicycle ergometer test, before the operation, both groups reached their VAT at the power (GB = 93 ± 24 W; GB+E = 90 ± 24 W) with an equal time of occurrence (GB = 270 ± 107 s; GB+E = 266 ± 133 s). Gastric bypass surgery, with a weight loss of average 25 kg after 4 months, did not improve time of occurrence of VAT and power at VAT. However, when patients followed an exercise program (GB+E), they could delay the time of occurrence of VAT (time of occurrence of VAT = 349 ± 149 s) (Fig. 1). To conclude, %VO2 at VAT/VO2 peak (the percentage oxygen uptake at VAT relative to the oxygen uptake at peak, also a measurement to define aerobic capacity in relation to total exercise capacity) revealed an interaction effect, meaning that both groups evolved differently considering exercise versus no exercise (Table 4).
Time of occurrence (seconds) of VAT during the maximal bicycle ergometer test. Comparison between GB and GB+E. GB group with only gastric bypass surgery, GB+E gastric bypass surgery and exercise program; empty bars preoperative, filled bars postoperative. *p < 0.05 versus preoperatively. VAT ventilatory anaerobic threshold
Also, peak exercise capacity parameters were recorded. Preoperatively, the morbidly obese subjects reached a peak oxygen uptake of 17.4 ± 4.9 ml/kg/min (GB) and 17.6 ± 3.2 ml/kg/min (GB+E), which can be defined as an extreme poor physical fitness (<23 ml/kg/min). Surprisingly, absolute peak oxygen uptake (ml/min) and power (W) were not improved 4 months after an intensive training program, nor by bariatric surgery. When expressed relative to body weight, peak oxygen uptake and peak power increased in both groups; however, peak oxygen uptake relative to fat-free mass remained unchanged (Table 5).
Discussion
Muscle Strength and Muscle Mass
The present study indicates that gastric bypass surgery results in a considerable decrease in dynamic muscle strength 4 months after the operation (−16% of quadriceps strength, −36% of biceps strength, −39% of triceps strength). The most plausible explanation can be found in the decrease in muscle mass. The untrained patients (GB) lost 7.6 kg muscle mass, which is 29.7% of total body weight loss (−26.6 kg). Two extensive reviews have been published by Stiegler et al. [35] and Chaston TB et al. [36] that confirm the positive relationship between weight loss and fat-free mass loss (FFML). Moreover, very low caloric diets result in greater FFML compared to low caloric diets and bariatric surgery results in greater FFML than very low caloric diets. Webster et al. [37] was the first to demonstrate that loss in FFM should not be more than 22% of total weight loss because of its function in resting metabolic rate, maintenance of functional capacity as the body ages, thermoregulation, oxidative capacity of the body, and weight management.
Exercise training can attenuate muscle atrophy or can even maintain FFM during weight loss in diet studies [35, 36], but the value of a standardized exercise program after bariatric surgery, or specifically after gastric bypass surgery, has not been investigated. We now show that a 3×/week combined aerobic and resistance exercise program could not prevent the loss in FFM, with no significant differences compared to the untrained patients. However, the decline in FFM seemed less severe (absolute, −5.4 kg; relative, 22.4% of total weight loss) and was brought within the acceptable limits as determined by Webster et al. [37]. Interestingly, although exercise training (GB+E) could not prevent FFML, it completely prevented strength loss and even induced a significant increase in dynamic strength of most muscle groups (+72% quadriceps strength, +27% hamstrings strength, and a tendency of +12% biceps strength; Table 3). The apparent discrepancy between a decline in FFM and an increase in strength in the GB+E group can mainly be attributed to the accepted feature that during the early stages of a training program neurological factors have the greatest contribution in the increase in muscle strength [38].
Besides dynamic muscle strength, we also measured peripheral static muscle strength by a handgrip strength test (HGS). Surprisingly, peripheral static muscle strength evolved differently compared to dynamic muscle strength. There was an overall time effect in the decrease of HGS, meaning that the untrained (GB) as well as the trained patients (GB+E) lost HGS 4 months after gastric bypass surgery (GB = −18%, GB+E = −7%). Probably, training specificity can give an explanation. In our study, no static muscle strength exercises were included in the training program, and it is known that the exercise must be specific to the type of strength required [38].
In general, we can debate about the question, “is a decrease in muscle strength a problem for morbidly obese patients after weight loss?”. It is known that obese patients have higher absolute muscle strength compared to lean subjects, but they have lower relative muscle strength (in terms of total body weight) [19, 39–41]. The latter gives the patients an impaired functional capacity, meaning that more strength is necessary to handle their heavier body. Although morbidly obese patients lose weight after bariatric surgery, they often remain, relatively speaking, less strong. Therefore, it seems important to prevent a decrease in muscle strength after bariatric surgery.
Functional Capacity
Muscle strength and muscle mass are important in functional capacity. In our study, we subjected the patients to two functional exercises. With regard to our first test, the STS test, the trained patients (GB+E) improved their number of times to rise to a full stand from a seated position within 30 s whereas the untrained patients (GB) did not. According to literature, quadriceps strength and % body fat mainly determine the sit-to-stand test [42, 43].This is in line with our results, where “GB+E” has 72% increase in quadriceps muscle strength and “GB” has a decrease of 16%. Percentage body fat could not further explain the difference in STS between the two groups, because both groups lost the same amount of body fat.
The 6MWD is the only test where both the trained and the untrained patients improved. However, further analyses showed us that the increase is mainly attributed to the increase in “GB+E.” It is known that walking distance is reduced in obese patients compared to lean subjects [44]. According to Tompkins et al. [22], bariatric surgery leads to an improvement up to 75% of normative values 6 months after the operation. Indeed, weight loss (especially % body fat) makes walking less exhausting, which can be noticed in our results by a decreased rating of perceived exertion and heart frequency at the end of the test. Not only percentage body fat but also maximal oxygen uptake (VO2 max) and quadriceps muscle strength are important predictors as well in the 6MWD [44–46]. As the first two parameters evolved equally in both groups, quadriceps muscle strength is likely responsible for the more pronounced increase in 6MWD for the trained patients.
Exercise Capacity and Oxidative Capacity
Aerobic capacity can be evaluated by a maximal incremental bicycle ergometer test, where the anaerobic threshold (AT) reflects true aerobic capacity and where maximal oxygen uptake (VO2 peak) reflects exercise capacity (maximal aerobic capacity).
VO2 peak (ml/min), as well as other peak exercise capacity parameters (peak work, peak heart rate, and peak RER), did not change 4 months after the operation, and there were no differences between the untrained and trained patients. To interpret these results, we must know that literature about the effect of weight loss on peak exercise capacity parameters in obese patients is equivocal. Depending on the presence of obesity-related disorders, peak exercise capacity will evolve differently. Healthy obese subjects undergoing weight loss will likely experience a decrease in VO2 max and peak work output because of a decreased muscle mass [47] and because the daily elevated cardiac stress, which is a training for the heart, fades away [48]. In contrast, many obese patients struggle with obesity-related disorders, such as impaired cardiac function (impaired left ventricular function and diastolic indices) [49, 50], inefficient ventilatory work (added mass on the chest wall and increased pressure in the abdomen) [51], and decreased intramyocellular lipid oxidation [25, 52], which are associated with reduced exercise capacity. During weight loss, cardiac and pulmonary systems will restore and will probably overwhelm the negative effect of a decreased muscle mass. This balance can result in a stabilization or even an improvement in maximal oxygen uptake [50].
To neutralize the effect of body weight and fat-free mass, VO2 divided by respectively body weight and FFM, is frequently used. Peak VO2/kg BW improved in both trained and untrained patients and can be explained by an improved body composition (decreased %FM and increased %FFM). Surprisingly, peak VO2/kg FFM did not change, meaning that neither weight loss nor added exercise training could improve the ability of fat-free mass to take up oxygen 4 months after surgery.
With regard to peak power output, the trained patients (GB+E) could produce more work relative to body weight, whereas the control group (GB) remained unchanged. We assume that “GB+E” could clear the effect of a decreased muscle mass by a more efficient energy expenditure during cycling and a better use of cardiac reserve [48].
While maximal oxygen uptake is equally determined by the oxygen transport system (pulmonary, cardiac, and vascular system) and the oxidative capacity of the skeletal muscle (O2 use in the mitochondria), the anaerobic threshold is mostly determined by the latter (if no severe complications of the first are detected). In our study, several measurements at VAT indicate that aerobic capacity does not improve 4 months after bariatric surgery. However, it is possible to elicit training effects during large-scale weight loss. Power and time of occurrence at VAT evolved positive in “GB+E” and remained the same for “GB” (Fig. 1 and Table 3). Further, the percentage oxygen uptake at VAT relative to the oxygen uptake at peak (% VO2 at VAT/VO2 peak) showed an interaction effect between the intervention group and the control group (Table 3). It has been reported that weight loss alone can improve metabolic flexibility (increased insulin sensitivity and reduced IMTG accumulation) [52], but recent diet studies showed that only weight loss combined with exercise can improve aerobic capacity, mitochondrial content, and electron chain transport activity in skeletal muscle of sedentary obese subjects [27].
Conclusion
To summarize, we could demonstrate that large-scale weight loss through gastric bypass surgery results in a decrease in dynamic and peripheral static muscle strength and no improvement in aerobic capacity. As a consequence, most components of functional capacity did not improve. In contrast, a 3×/week endurance and resistance exercise program could prevent the decrease and even induce an increase in strength in most muscle groups. Together with an improvement in submaximal aerobic capacity (ventilatory threshold), functional capacity increased significantly. Implementation of an exercise training program in the first 4 months after bariatric surgery is effective and should be promoted.
References
Buchwald H, Williams SE. Bariatric surgery worldwide 2003. Obes Surg. 2004;14:1157–64.
Hedley AA, Ogden CL, Johnson CL, et al. Prevalence of overweight and obesity among us children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–50.
Bult MJ, Van DT, Muller AF. Surgical treatment of obesity. Eur J Endocrinol. 2008;158:135–45.
Elder KA, Wolfe BM. Bariatric surgery: a review of procedures and outcomes. Gastroenterology. 2007;132:2253–71.
Farrell TM, Haggerty SP, Overby DW, et al. Clinical application of laparoscopic bariatric surgery: an evidence-based review. Surg Endosc. 2009;23:930–49.
Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–9.
Bray GA. Medical consequences of obesity. J Clin Endocrinol Metab. 2004;89:2583–9.
National Task Force on the Prevention and Treatment of Obesity. Overweight, obesity, and health risk. Arch Intern Med. 2000;160:898–904.
Kral JG, Naslund E. Surgical treatment of obesity. Nat Clin Pract Endocrinol Metab. 2007;3:574–83.
Torquati A, Lutfi R, Abumrad N, et al. Is Roux-En-Y gastric bypass surgery the most effective treatment for type 2 diabetes mellitus in morbidly obese patients? J Gastrointest Surg. 2005;9:1112–6.
Clements RH, Gonzalez QH, Long CI, et al. Hormonal changes after Roux-En Y gastric bypass for morbid obesity and the control of type-II diabetes mellitus. Am Surg. 2004;70:1–4.
Pietilainen KH, Kaprio J, Borg P, et al. Physical inactivity and obesity: a vicious circle. Obesity (Silver Spring). 2008;16:409–14.
Telford RD. Low physical activity and obesity: causes of chronic disease or simply predictors? Med Sci Sports Exerc. 2007;39:1233–40.
Stefan MA, Hopman WM, Smythe JF. Effect of activity restriction owing to heart disease on obesity. Arch Pediatr Adolesc Med. 2005;159:477–81.
Carey DG, Pliego GJ, Raymond RL, et al. Body composition and metabolic changes following bariatric surgery: effects on fat mass, lean mass and basal metabolic rate. Obes Surg. 2006;16:469–77.
Poitou BC, Ciangura C, Coupaye M, et al. Nutritional deficiency after gastric bypass: diagnosis, prevention and treatment. Diabetes Metab. 2007;33:13–24.
Brown M, Sinacore DR, Host HH. The relationship of strength to function in the older adult. J Gerontol A Biol Sci Med Sci. 1995;50:55–9.
Wolfson L, Judge J, Whipple R, et al. Strength is a major factor in balance, gait, and the occurrence of falls. J Gerontol A Biol Sci Med Sci. 1995;50:64–7.
Maffiuletti NA, Jubeau M, Munzinger U, et al. Differences in quadriceps muscle strength and fatigue between lean and obese subjects. Eur J Appl Physiol. 2007;101:51–9.
Maffiuletti NA, Jubeau M, Agosti F, et al. Quadriceps muscle function characteristics in severely obese and nonobese adolescents. Eur J Appl Physiol. 2008;103:481–4.
Maniscalco M, Zedda A, Giardiello C, et al. Effect of bariatric surgery on the six-minute walk test in severe uncomplicated obesity. Obes Surg. 2006;16:836–41.
Tompkins J, Bosch PR, Chenowith R, et al. Changes in functional walking distance and health-related quality of life after gastric bypass surgery. Phys Ther. 2008;88:928–35.
Mathier MA, Ramanathan RC. Impact of obesity and bariatric surgery on cardiovascular disease. Med Clin North Am. 2007;91:415–31.
He J, Watkins S, Kelley DE. Skeletal muscle lipid content and oxidative enzyme activity in relation to muscle fiber type in type 2 diabetes and obesity. Diabetes. 2001;50:817–23.
Houmard JA. Intramuscular lipid oxidation and obesity. Am J Physiol Regul Integr Comp Physiol. 2008;294:R1111–6.
Kelley DE. Skeletal muscle fat oxidation: timing and flexibility are everything. J Clin Invest. 2005;115:1699–702.
Toledo FG, Menshikova EV, Azuma K, et al. Mitochondrial capacity in skeletal muscle is not stimulated by weight loss despite increases in insulin action and decreases in intramyocellular lipid content. Diabetes. 2008;57:987–94.
Tanner CJ, Barakat HA, Dohm GL, et al. Muscle fiber type is associated with obesity and weight loss. Am J Physiol Endocrinol Metab. 2002;282:E1191–96.
Rice B, Janssen I, Hudson R, et al. Effects of aerobic or resistance exercise and/or diet on glucose tolerance and plasma insulin levels in obese men. Diabetes Care. 1999;22:684–91.
Janssen I, Fortier A, Hudson R, et al. Effects of an energy-restrictive diet with or without exercise on abdominal fat, intermuscular fat, and metabolic risk factors in obese women. Diabetes Care. 2002;25:431–8.
Kushner RF, Schoeller DA. Estimation of total body water by bioelectrical impedance analysis. Am J Clin Nutr. 1986;44:417–24.
Pace HV, Rathbun EN. Studies on body composition, body water and chemically combined nitrogen content in relation to fat content. J Biol Chem. 2009;158:685–91.
Enright PL. The six-minute walk test. Respir Care. 2003;48:783–5.
Wasserman K, Whipp BJ, Koyl SN, et al. Anaerobic threshold and respiratory gas exchange during exercise. J Appl Physiol. 1973;35:236–43.
Stiegler P, Cunliffe A. The role of diet and exercise for the maintenance of fat-free mass and resting metabolic rate during weight loss. Sports Med. 2006;36:239–62.
Chaston TB, Dixon JB, O'brien PE. Changes in fat-free mass during significant weight loss: a systematic review. Int J Obes (Lond). 2007;31:743–50.
Webster JD, Hesp R, Garrow JS. The composition of excess weight in obese women estimated by body density, total body water and total body potassium. Hum Nutr Clin Nutr. 1984;38:299–306.
Folland JP. AG. The adaptations to strength training: morphological and neurological contributions to increased strength. Sports Med. 2007;37:145–68.
Blimkie CJ, Sale DG, Bar-Or O. Voluntary strength, evoked twitch contractile properties and motor unit activation of knee extensors in obese and non-obese adolescent males. Eur J Appl Physiol Occup Physiol. 1990;61:313–8.
Pescatello LS, Kelsey BK, Price TB, et al. The muscle strength and size response to upper arm, unilateral resistance training among adults who are overweight and obese. J Strength Cond Res. 2007;21:307–13.
Hulens M, Vansant G, Lysens R, et al. Study of differences in peripheral muscle strength of lean versus obese women: an allometric approach. Int J Obes Relat Metab Disord. 2001;25:676–81.
Bohannon RW. Body weight-normalized knee extension strength explains sit-to-stand independence: a validation study. J Strength Cond Res. 2009;23:309–11.
Bohannon RW. Knee extension strength and body weight determine sit-to-stand independence after stroke. J Strength Cond Res. 2007;23:309–11.
Hulens M, Vansant G, Claessens AL, et al. Predictors of 6-minute walk test results in lean, obese and morbidly obese women. Scand J Med Sci Sports. 2003;13:98–105.
Laukkanen R, Oja P, Pasanen M, et al. Validity of a two kilometre walking test for estimating maximal aerobic power in overweight adults. Int J Obes Relat Metab Disord. 1992;16:263–8.
Mattsson E, Larsson UE, Rossner S. Is walking for exercise too exhausting for obese women? Int J Obes Relat Metab Disord. 1997;21:380–6.
Goran M, Fields DA, Hunter GR, et al. Total body fat does not influence maximal aerobic capacity. Int J Obes Relat Metab Disord. 2000;24:841–8.
Seres L, Lopez-Ayerbe J, Coll R, et al. Increased exercise capacity after surgically induced weight loss in morbid obesity. Obesity (Silver Spring). 2006;14:273–9.
Carroll S, Marshall P, Borkoles E, et al. Efficacy of lifestyle intervention on peak exercise cardiac power output and reserve in premenopausal obese females: a randomised pilot study. Int J Cardiol. 2007;119:147–55.
Kanoupakis E, Michaloudis D, Fraidakis O, et al. Left ventricular function and cardiopulmonary performance following surgical treatment of morbid obesity. Obes Surg. 2001;11:552–8.
Gilbert R, Sipple JH, Auchincloss JH Jr. Respiratory control and work of breathing in obese subjects. J Appl Physiol. 1961;16:21–6.
Corpeleijn E, Saris WH, Blaak EE. Metabolic flexibility in the development of insulin resistance and type 2 diabetes: effects of lifestyle. Obes Rev. 2009;10:178–93.
Acknowledgments
This study was financially supported by a grant from the University Ghent (BOF-project, NR. 01J07007) and by Ethicon Endo-Surgery (A Johnson & Johnson Company). Patients were recruited from the University Hospital Ghent, Belgium (Europe) and from AZ Nikolaas, Sint-Niklaas, Belgium (Europe).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stegen, S., Derave, W., Calders, P. et al. Physical Fitness in Morbidly Obese Patients: Effect of Gastric Bypass Surgery and Exercise Training. OBES SURG 21, 61–70 (2011). https://doi.org/10.1007/s11695-009-0045-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-009-0045-y