Abstract
Background
Shortened sleep duration causes hormonal and metabolic changes that favor fat accumulation and weight gain. Obesity, in turn, may reduce sleep quality and contribute to sleep loss. The purpose of this study was to evaluate the sleep durations of individuals with morbid obesity, compared to their nonobese counterparts, and to determine the effects of surgical weight reduction on sleep duration and sleep quality.
Methods
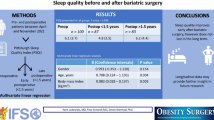
The study population included 45 bariatric (BA) surgical patients (mean body mass index [BMI] = 49) and 45 gender-matched nonobese controls (NC; BMI = 24). Self-reported sleep durations were obtained and overall sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI).
Results
The data show that average sleep durations of the preoperative BA patients were significantly (p < 0.0001) less than those of the NC, i.e., 6.0 and 7.2 h, respectively. Sleep loss for the BA patients was associated with poor sleep quality, along with an increased frequency of conditions that interfere with sleep, including coughing and snoring, difficulty breathing, feeling too hot, and experiencing pain. Overall, 78% of the BA patients, compared to 36% of the NC, had PSQI scores indicative of poor sleep quality. Surgery after 3 to 12 months resulted in significant (p < 0.0001) weight loss (percentage total change in BMI = 34) and improved sleep quality, i.e., PSQI = 8.8 preoperatively vs. 4.6 postoperatively. Sleep durations increased significantly (p < 0.0001) post-surgery from 6.0 to 6.8 h.
Conclusions
Individuals with extreme obesity, compared to the nonobese, obtain less sleep and experience poorer sleep quality. Bariatric surgery improves sleep duration and quality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep durations have progressively declined over the last several decades [1]. Recent data show that many Americans are sleeping for 6 h/day or less [2]. Shortened sleep duration increases the risk for all-cause mortality and a number of diseases, including obesity [3]. Studies find that adults who sleep for <7 h/day are at increased risk for obesity and weight gain over time [1, 3–9] and may lose less weight while on a diet [10].
Mechanisms responsible for the link between sleep loss and obesity are unclear. Investigators find that shortened sleep duration is associated with a number of hormonal changes that favors fat accumulation, including an increase in ghrelin, a reduction in leptin and in the ratio of leptin to ghrelin, an increase in evening cortisol, reduced insulin sensitivity, a decrease in growth hormone, and among certain ethnicities, a decline in adiponectin [1, 2, 11–18]. Altogether, such changes increase appetite, reduce energy expenditure, and alter fat metabolism in a manner that increases adiposity. In these ways, sleep loss contributes to weight gain and obesity. Obesity, in turn, causes physical, emotional, and environmental conditions that interfere with sleep quality and duration, setting in motion a vicious cycle whereby sleep loss “begets” obesity and obesity “begets” sleep loss.
For the bariatric (BA) patient, sleep loss may not only contribute to obesity progression and associated comorbidities prior to surgical intervention but also interfere with maximal weight loss success and long-term maintenance. To our knowledge, there are no studies of sleep duration and associated intervening factors in BA patients prior to or following surgical weight reduction. The purpose of this study was (1) to evaluate the sleep durations of morbidly obese surgical candidates and their nonobese controls (NC) and (2) to determine the effects of surgical weight reduction on sleep duration and factors contributing to sleep quality.
Methods
Study Subjects
The study population included BA patients with morbid obesity and their gender-matched NC. The BA participants were selected at random from the patient population of Florida Hospital Celebration Health Metabolic Medicine and Surgery Institute. The BA population included 45 patients (35 females/10 males) with a mean weight of 135.8 kg and an average body mass index (BMI) = 48.5. The NC population included 45 nonobese participants (35 females/10 males) with a mean weight of 71 kg and BMI = 24. There were no significant differences in age between the study populations, i.e., 45.8 ± 2.0 and 41.0 ± 2.4 years for the BA and NC groups, respectively. The study was approved by the Florida Hospital Institutional Review Board.
Overall Study Design
Sleep duration and quality of the BA patients were determined before and 3 months to 1 year after bariatric surgery. Surgery procedures included Roux-en-Y gastric bypass (n = 32) or sleeve gastrectomy (n = 13). Weight loss was expressed as percentage total change in BMI.
Methodology
Sleep duration was obtained and sleep quality was assessed by the Pittsburgh Sleep Quality Index (PSQI) [19]. The data collected included height, preoperative weight, postoperative weight, BMI, sleep duration, time to fall asleep, a series of causative factors leading to disruptive sleep, and additional questions concerning conditions associated with poor sleep quality. Sleep interruptions were scored according to frequency of occurrence over the course of 1 week, i.e., zero times, once, twice, three times, or more. Causative factors leading to sleep disruption included the following: (1) having trouble falling asleep within 30 min of going to bed, (2) waking up in the middle of the night or early morning and not being able to go back to sleep, (3) having to get up to use the restroom, (4) having difficulty breathing, (5) coughing or snoring loudly, (6) feeling too cold, (7) feeling too hot, (8) having bad dreams, and (9) experiencing pain. Conditions associated with poor sleep quality included frequency of the use of sleep medications, of daytime drowsiness, and of difficulty in keeping up enthusiasm. Perceived sleep quality was rated by subjects as “very good,” “fairly good,” “fairly bad,” and “very bad.” These subjective scales were weighted to obtain a global PSQI score that differentiates between “good” and “poor” quality of sleep. A global PSQI score of 5 or greater is considered “poor” quality.
Statistical Analysis
Comparative data is reported as the mean ± standard error of the mean. Unpaired Student’s t tests were used to determine differences between values for BA patients and NC, and paired t tests were used to identify differences between preoperative and postoperative values. Simple and multiple regression analyses were used to assess the relationships between variables and to explain or predict a dependent variable. Chi square (χ 2) was used for the assessment of categorical data. All statistical tests were two-sided at the 0.05 significance level. Statistical analyses were conducted using the SAS statistical software (SAS, Cary, NC, USA).
Results
The differences between the total sleep durations of the preoperative BA patients and their leaner counterparts are illustrated in Fig. 1a. Sleep durations of the preoperative patients were significantly less than those of the NC, i.e., means = 6.0 and 7.2 h, respectively. Among the BA patients, 71% slept for durations of <7 h, in comparison to 39% of the NC. BA patients and NC who slept <7 h weighed more and were more likely to have poor quality of sleep (higher PSQI scores) than their respective counterparts whose sleep durations were 7 h or longer (data not shown). Sleep durations of all study participants were inversely and significantly correlated to BMI and to PSQI scores (see Table 1). Both sleep quality (PSQI scores) and BMI of the combined populations were, according to multiple regression analyses, independent predictors of sleep duration, i.e., PSQI scores (p < 0.0001) and BMI (p = 0.0060), and accounted for 45% of the variability in sleep duration (R 2 = 0.45, p < 0.0001).
The difference between sleep quality of the BA patients and that of the controls is illustrated by Fig. 1b. Poor sleep quality, according to the criteria established by the PSQI, is a score of 5 or greater. The low PSQI scores of the BA and NC groups occurred in association with significant differences in the frequency of occurrence of a number of conditions associated with poor sleep quality, as reported in Table 2. These included, among the BA patients, a significantly greater (χ 2 p value ≤ 0.05) frequency of occurrence of the following causative factors of sleep disruption: difficulty breathing, coughing or loud snoring, feeling too hot, and experiencing pain. The BA vs. NC subjects were also more likely to be on sleep meds (χ 2 p value = 0.004) and to have greater difficulty keeping up enthusiasm (χ 2 p value = 0.011). In addition, a greater percentage (44%) of BA patients perceived their overall sleep quality to be poor in comparison to the NC subjects (12%; Fig. 2a, b).
Three to 12 months following surgery, patients lost an average of 45 kg body weight, with no difference between operative procedures (p > 0.05). Post-surgery “perceived” sleep quality improved, as illustrated by the greater percentage of individuals who rated their quality of sleep as “very good” or “fairly good” (see Fig. 2c). Bariatric surgery also led to significant (χ 2 p value ≤ 0.05) improvement in the frequency of occurrence of conditions that are associated with or cause disruptions of sleep quality (Table 2). Postoperatively, patients reported being more enthusiastic (χ 2 p value = 0.01) and had a tendency (χ 2 p value = 0.06) to require fewer sleep medications.
The reduced frequency of conditions associated with or causing sleep interruptions with weight loss surgery resulted in a highly significant improvement in sleep quality, according to the composite PSQI scores. As seen in Fig. 3a, overall PSQI scores declined from a mean of 8.8 before surgery to 4.6 after surgery. Changes in PSQI postoperatively were not significantly (p > 0.05) associated with surgery-induced changes in BMI, i.e., r = 0.11. However, changes in PSQI were significantly (p < 0.01) and inversely correlated (r = −0.49) to improvements in sleep duration (data not shown).
As seen in Fig. 3b, sleep durations increased significantly (p < 0.0001) following surgery. Sleep duration increased from a mean of 6.0 h preoperatively to 6.8 h postoperatively. Whereas only 29% of patients obtained seven or more hours of sleep prior to surgery, 66% slept for seven or more hours following surgery. Patients who reported sleeping for seven or more hours, compared to those who slept for <7 h, had significantly (p < 0.0001) better sleep quality scores, i.e., 2.70 vs. 7.30, respectively. Changes in both PSQI scores and BMI with surgery were, according to multiple regression analyses, independent predictors of postoperative improvement in sleep duration, i.e., change in PSQI (p = 0.0066) and change in BMI (p = 0.0285), and accounted for 35% of the variability in sleep duration (R 2 = 0.35, p = 0.0059).
Discussion
Our data show that sleep duration among BA patients is considerably less than that of individuals who are nonobese. BA patients prior to surgery obtained an average of 6 h of sleep per day. Such sleep durations are more than an hour less than those of their nonobese counterparts who slept for an average of 7.2 h. Sleep durations of the BA patients, of the NC, or of the combined groups were significantly and inversely associated with body size, such that individuals with the least amount of sleep were most likely to be overweight or obese. These findings are in agreement with a number of epidemiological studies that have reported associations between shortened sleep duration and a higher incidence of overweight and obesity [1, 3–9] among individuals of varying body sizes, socioeconomic status, age, and ethnicity.
According to epidemiological reports, the lowest risk for obesity occurs with a sleep duration of 7 to 8 h, and amounts of sleep that are <7 h are inversely correlated to body size (body weight, BMI, or percent body fat). One large cross-sectional population study (NHANES I) [5] found that people who sleep 4 h or less are 73% more likely to be obese than those who sleep for 7 to 9 h; individuals who obtain 5 h of sleep are 50% more likely to be obese; and people sleeping for 6 h have a 23% greater chance of obesity. Prospective studies have also found that sleeping for <7 h increases the risk for significant weight gain and fat accumulation over time [5–9]. A recent report, for instance, found that individuals who sleep between 5 and 6 h, compared to those who get 7 to 8 h, are 35% more likely to gain at least 5 kg of additional weight over the course of a 6-year period [9]. As regards these findings, it is of interest that a significantly large percentage of the extremely obese BA patients in the present study reported sleeping for durations of only 5 to 6 h.
The link between sleep loss and obesity has not been clearly delineated. Sleep restriction contributes to obesity, in part, by affecting changes in neuroendocrine regulation of appetite and energy expenditure. Population and controlled laboratory studies find with sleep loss an increase in production of the gut hormone, ghrelin, and decease in the adipose tissue product, leptin [1, 3, 11–18]. Ghrelin stimulates appetite and food consumption and reduces energy expenditure and fat oxidation. Leptin, a product of adipose tissue, has actions opposite to those of ghrelin on appetite and energy expenditure. Data [11] show that shortened sleep duration, even for brief periods (2 days), reduces the ratio of leptin to ghrelin, along with an increase in hunger, appetite, and cravings for calorie-dense high-carbohydrate foods (cake, candies, cookies, bread, pasta, and chips).
A reduced leptin-to-ghrelin ratio with sleep loss may also contribute to the expansion of adipose tissue and other hormonal and metabolic changes that occur with sleep restriction, including a reduction in insulin sensitivity, an increase in cortisol, a decrease in growth hormone, and in some ethnicities, a decline in adiponectin [1, 3, 11–18]. Thus, changes in hormone status and neuroendocrine regulation of appetite and energy expenditure may help to explain, in part, the link between sleep loss and obesity found in the present study and in numerous other reports.
Although sleep loss contributes to obesity, the reverse is also true, obesity causes sleep loss. Obesity produces a number of psychological and physical conditions that may interfere with sleep quality and duration. Physical disruptors of sleep duration may include difficulty breathing, coughing, snoring, body temperature dysregulation, urinary incontinence, pain, and more. In the present study, BA patients, compared to their nonobese counterparts, were reported having a greater frequency of occurrence of physical disruptors of sleep, contributing to poor overall sleep quality as assessed by their scores on the PSQI. Both sleep quality (PSQI scores) and degree of obesity were, according to multiple regression analyses, independent predictors of sleep duration.
Bariatric surgery produced massive weight loss and sleep quality dramatically improved. PSQI scores declined by nearly 50% post-surgery, along with highly significant reduction in the frequency of conditions causing sleep disruption. Such changes in overall sleep quality and associated sleep disruptors improved patients’ length of sleep by a mean duration of nearly an hour. The increase in sleep duration with surgery was significantly associated with surgery-related improvements in sleep quality and weight reduction.
A major limitation of this study is that a greater variety of potential predictors of sleep duration were not measured. Emotional or psychological status, for instance, may have contributed to sleep loss. Studies find that depression, anxiety, and poor quality of life are relatively common among bariatric surgical candidates [20–22] and these conditions adversely affect sleep quality and duration [23–25]. Surgery is associated with highly significant improvement in quality of life and overall psychological status for most BA patients [20–22], and these improvements may have contributed significantly to the greater sleep duration and quality of our bariatric population post-surgery.
Physical disruptors of sleep associated with obesity not evaluated by the PSQI could also have adversely affected sleep measures in our bariatric population. Potential effectors of sleep quality and duration worsened by obesity and improved by surgical weight loss include gastroesophageal reflux disease, gastritis, asthma, and other obesity comorbidities. Further investigations are in order to identify and determine the role of such physical and psychological conditions on sleep quality and duration before and after bariatric surgery.
Conclusion
In summary, sleep loss causes hormonal and metabolic changes that may result in weight gain and obesity. Weight gain and obesity, in turn, may cause physical and emotional conditions that interfere with sleep quality and shorten sleep duration. Bariatric surgical candidates have shortened sleep duration in association with a number of physical and emotional conditions that interfere with sleep quality. Surgical weight loss causes highly significant improvement in sleep quality in association with greater sleep duration. Such changes in sleep duration may play a role in the weight loss success of bariatric surgeries.
References
Knutson KL, Spiegel K, Penev P, et al. The metabolic consequences of sleep deprivation. Sleep Med Rev. 2007;11:163–78.
National Center for Health Statistics. Percentage of adults who reported an average of ≤6 hours of sleep per 24-hour period, by sex and age group—United States, 1985 and 2004. Morb Mortal Wkly Rep. 2005.
Taheri S, Lin L, Austin D, et al. Short sleep duration is associated with reduced leptin, elevated ghrelin and increased body mass index. PLoS Med. 2004;1:e62.
Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31:619–26.
Gangwisch JE, Malaspina D, Boden-Albala B, et al. Inadequate sleep as a risk factor for obesity: analysis of NHANES I. Sleep. 2005;28:1289–96.
Hasler G, Buysse DJ, Klaghofer R, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;27:661–6.
Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16:643–53.
Lopez-Garcia E, Faubel R, Leon-Munoz L, et al. Sleep duration, general and abdominal obesity, and weight change among the older adult population of Spain. Am J Clin Nutr. 2008;87:310–6.
Chaput JP, Despres JP, Bouchard C, et al. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep. 2008;31:517–23.
Nedeltcheva AV, Kilkus JM, Imperial J, et al. Insufficient sleep undermines dietary efforts to reduce adiposity. Ann Intern Med. 2010;153:435–41.
Spiegel K, Tasali E, Penev P, et al. Brief communication: sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels and increased hunger and appetite. Ann Intern Med. 2004;141:846–50.
Spiegel K, Leproult R, L’hermite-Baleriaux M, et al. Leptin levels are dependent on sleep duration: relationships with sympathovagal balance, carbohydrate regulation, cortisol and thyrotropin. J Clin Endocrinol Metab. 2004;89:5762–71.
Copinschi G. Metabolic and endocrine effects of sleep deprivation. Essent Psychopharmacol. 2005;6:341–7.
Van Cauter E, Holmback U, Knutson K, et al. Impact of sleep and sleep loss on neuroendocrine and metabolic function. Horm Res. 2007;67:2–9.
Morselli L, Leproult R, Balbo M, et al. Role of sleep duration in the regulation of glucose metabolism and appetite. Bes Prac Res Clin Endocrinol Metab. 2010;24:687–702.
Schmid SM, Hallschmid M, Jauch-Chara K, et al. A single night of sleep deprivation increases ghrelin levels and feelings of hunger in normal weight healthy men. J Sleep Res. 2008;17:331–4.
Kotani K, Sakane N, Saiga K, et al. Serum adiponectin levels and lifestyle factors in Japanese men. Hear Vessel. 2007;22:291–6.
Simpson NS, Banks S, Arroyo S, et al. Effects of sleep restriction on adiponectin levels in healthy men and women. Physiol Behav. 2010;101:693–8.
Buysse DJ, Reynolds 3rd CF, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213.
Maddi SR, Fox SR, Khoshaba DM, et al. Reduction in psychopathology following bariatric surgery for morbid obesity. Obes Surg. 2001;11:680–5.
Kolotkin RL, Crosby RD, Gress RE, et al. Two-year changes in health related quality of life in gastric bypass patients compared with severely obese controls. Surg Obes Relat Dis. 2009;5:250–6.
Friedman KE, Ashmore JA, Applegate KL. Recent experiences of weight-based stigmatization in a weight loss surgery population: psychological and behavioral correlates. Obesity (Silver Spring). 2008;16(2):69–74.
Szklo-Coxe M, Young T, Finn L, et al. Depression: relationships to sleep paralysis and other sleep disturbances in a community sample. J Sleep Res. 2007;16:297–312.
Vahtera J, Kivimaki M, Hublin C, et al. Liability to anxiety and severe life events as predictors of new-onset sleep disturbances. Sleep. 2007;30:1537–46.
Berk M. Sleep and depression—theory and practice. Aust Fam Physician. 2009;38:302–4.
Conflicts of Interest
Patricia Toor, Keith Kim, and Cynthia Buffington have no conflicts of interest regarding the content of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Toor, P., Kim, K. & Buffington, C.K. Sleep Quality and Duration Before and After Bariatric Surgery. OBES SURG 22, 890–895 (2012). https://doi.org/10.1007/s11695-011-0541-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-011-0541-8