Abstract
Purpose
Sleep deprivation is associated with growth hormone deficiency and an elevated cortisol level, both of which have been linked to obesity. However, assessing sleep quality is often not established in the multidisciplinary peribariatric evaluation program. This study aimed to determine sleep quality in patients who are seeking or underwent bariatric surgery by using Pittsburgh Sleep Quality Index (PSQI) measurements.
Materials and Methods
In this observational study, patients who underwent or were seeking bariatric surgery between April and November 2021 were included. Self-reported patients’ demographics, operative techniques, and sleep quality measured by PSQI were collected. Baseline characteristics were compared between the preoperative group (PRE), patients who underwent surgery < 1.5 years ago (EARLY), and > 1.5 years ago (LATE). A multivariate linear regression model was built.
Results
In total, 270 patients filled out the questionnaire of which 100 (37.1%) were preoperative, 87 (32.2%) early, and 83 (30.7%) late postoperative. The PSQI significantly improved in the EARLY group compared to PRE (4.8 vs 6.1). This effect disappeared in the LATE group (6.1) even though their body mass index was less. Linear regression revealed that age (p = 0.004) and body mass index (p = 0.003) predicted worse sleep quality.
Conclusion
Sleep quality improves early after bariatric surgery; however, this benefit does not seem to last in the long term. Other factors than weight regain should be considered for this finding, future studies with longer follow-up periods are recommended, including other variables associated with sleep quality such as health conditions and socioeconomic status.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to clinical guidelines, sleep quality analysis should be part of the preoperative evaluation for bariatric surgery candidates [1]. There is a relationship between obesity and sleep deprivation, it causes metabolic changes in glucose metabolism, appetite, calorie intake, and energy expenditure [2,3,4,5,6,7,8]. More specifically, sleep deprivation might cause hyperphagia, possibly by reducing levels of leptin and increasing ghrelin and therefore increased food intake. Due to sleep deprivation, individuals have simply more time to eat and are physically less active as a consequence to fatigue, and it lowers body core temperature causing lower energy expenditure [3]. However, guidelines do not describe how sleep quality should be assessed. A commonly used method is determining the Pittsburgh Sleep Quality Index (PSQI) [9]. To date, there is no literature on the reference values of the PSQI in patients with obesity. The literature that investigated the PSQI preoperatively and postoperatively describes improvement in sleep quality postoperative; however, sample sizes are small, and whether this improvement remains has not been described yet [10,11,12]. Weight regain after bariatric surgery could influence these results [13,14,15]. According to Cooper et al., patients regain 21–29% of their lost weight after Roux-en-Y gastric bypass [16]. This could result in return of obesity-related comorbidities and decrease in health-related quality of life, which in turn might decrease sleep quality [17]. This study aimed to determine the sleep quality of patients in a bariatric surgery trajectory using the PSQI questionnaire in a large population both preoperatively as mid- to long-term postoperative.
Methods
In this observational study, patients who underwent or were seeking bariatric surgery between April and November 2021 were included. Self-reported patients’ demographics, operative techniques, and sleep quality measured by PSQI were collected. Patients who received revisional surgery were excluded from analysis. All potential candidates for bariatric surgery underwent screening before surgery and thereafter gain access to an eHealth platform on which informational videos, e-learning, and screening questionnaires were provided. The PSQI questionnaire was added to this list as a voluntary option, a self-administered questionnaire that assesses subjective sleep quality of the previous month. It comprises 19 items which evaluates 7 components: sleep duration, sleep disturbance, sleep latency, day dysfunction due to sleepiness, sleep efficiency, overall sleep quality, and the use of sleep medication. Using a formula, the PSQI could be calculated ranging from 0 to 21, with higher scores indicating worse sleep quality.
Both preoperative and postoperative patients had access to this platform and completed this questionnaire. In standard practice, follow-up aided by this platform is up to 5 years. Additionally, the difference between mid- and long-term postoperative was set on 1.5 years. This study was approved by the local Institutional Review Board and informed consent was retrieved for all participating patients.
Statistical Analysis
Baseline characteristics were compared between the preoperative group (PRE), patients who underwent surgery < 1.5 years ago (EARLY) and > 1.5 years ago (LATE). A multivariate linear regression model was built. The chi-square test for categorical data and one-way ANOVA were used for continuous data if normally distributed. The Kruskal–Wallis test was used if data was not normally distributed. The PSQI values were presented as categorical data and continuous data for better interpretation over time; a PSQI ≤ 5 is associated with good sleep quality, above 5 as poor sleep quality [9]. A multivariate linear regression model was built to correct for confounders and to estimate the relationship between the independent variables on sleep quality. Backward selection of the clinically relevant and univariate significant confounders was used (p < 0.1). Additionally, modification effects of included variables were investigated. Continuous variables in normally distributed data were presented as mean and standard deviation, not normally distributed data were reported as median and interquartile range.
Statistical analyses were performed using SPSS software (version 26). Significance levels were set for p-value < 0.05.
Results
A total of 270 patients filled out the questionnaire completely, of which 100 (37.1%) were in the preoperative phase, 87 (32.2%) in the early postoperative phase (< 1.5 years), and 83 (30.7%) in the late postoperative phase (> 1.5 years).
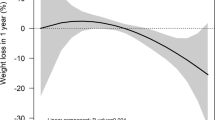
The majority was female 228 (84.4%), most of them aging between 45 and 54 years, 49% underwent a sleeve gastrectomy (SG) and 51% a Roux-en-Y gastric bypass (RYGB). The patient characteristics of all three groups, before and after surgery, are described in Table 1. There were significant differences between age groups and body mass index (BMI, kg/m2), as well as PSQI. The preoperative phase had a higher percentage of younger participants aging between 18 and 34 years old (26%) compared to the late postoperative phase which consisted of older participants aging between 55 and 64 years (42%). The BMI was significantly lower early postoperative but was even less in the late operative phase. The PSQI score improved in the early postoperative phase (4.8); however, it deteriorated after 1.5 years of surgery to the same score as preoperatively (both 6.1). The highest percentage of good sleep quality (PSQI ≤ 5) was observed in the early years (65.5%), the highest percentage of poor sleep quality in late years (49.4%). Comparing the two surgical techniques, the SG group had a mean PSQI of 5.13 compared to the RYGB group with a PSQI of 5.79.
Table 2 represents the univariate and multivariate linear regression model; there was no multicollinearity. In the univariate model, patients who were in the early phase significantly predicted higher sleep quality compared to the preoperative phase. In the multivariate model, the operative phase lost its significance when corrected for other included variables. Nevertheless, in this linear model, higher age and BMI significantly predict lower sleep quality. Although not significant, women had a higher median PSQI of 5 compared to men (4), suggesting poorer sleep quality.
Discussion
This observational study, including 270 patients who filled in the Pittsburgh Sleep Quality Index, showed the effect of different phases in bariatric surgery on sleep quality. It seems that sleep quality significantly improved early after surgery compared to preoperatively, however, deteriorated to the same score in long term. In an univariate linear model, patients in the early postoperative phase experienced significantly improved sleep quality compared to other preoperative patients. However, when other factors such as gender and BMI were added in the model, this variable lost its significance. Although it was anticipated patients would experience weight regain during follow-up and therefore possible decreased sleep quality, patients seem to continue to lose weight even after 1.5 years postoperatively as their BMI was 3 points lower compared to the early postoperative phase. An older study by Charuzi et al. investigated sleep apnea in 47 patients 1 year and 7 years after bariatric surgery, although regaining weight was associated with reappearance of sleep apnea the patients still felt that they slept better compared to before surgery, although excess weight was the main contributing factor for the severity of the syndrome [18]. Merged data from two randomized controlled trials evaluated 398 patients 5 years after RYGB and SG [19]. It appears that Roux-en-Y gastric bypass induced greater weight loss, but there was no difference in remission of obstructive sleep apnea. In a propensity score matching study, 285 patients were compared for surgical technique; there were no differences found for BMI reduction or sleep apnea [20]. Sleep quality seems to improve after bariatric surgery, but evidence if this improvement lasts in long term is lacking [10,11,12, 21]. To the best of our knowledge, the longest follow-up period on sleep quality after bariatric surgery is 6 months and therefore has not been investigated yet. In our study, theoretically patients could be up to 5 years postoperative. However, due to the questionnaire design, exact numbers are unavailable. Additionally, there was no literature found regarding the differences between surgical techniques and sleep quality.
Other studies investigated factors influencing sleep quality such as genetics, depressed mood, and physical illness [22, 23]. This might be an explanation for the contradicting results in our study, anticipating bariatric surgery would have a greater influence in predicting sleep quality. Sleep is a complex physiological process and affected by multiple factors including individual behavior, environment, socioeconomics, and physical well-being, and therefore hard to investigate in a cohort using questionnaires [23,24,25]. This study focused on the impact of weight loss on sleep quality. However, the literature also suggests that sleep disturbance itself plays an important role in obesity and thereby a bidirectional relationship [3, 26]. It is important to not only treat obesity by weight loss, but also include treatment of sleep deprivation.
Although higher age was a significant predictor for poorer sleep quality in the linear regression, age itself does not seem to be identified as a consistent, independent predictor of sleep disturbances according to multiple studies [23, 27, 28]. The differences in sleep quality in different age groups are hypothesized to be due to depressed mood and physical health problems. As for sex, our study describes higher PSQI scores in women. A cross-sectional study of 458 patients investigated whether the influence of sleep and BMI on the risk of developing metabolic syndrome differed by gender [29]. Yeom et al. found that the indirect effect of sleep quality on the risk of metabolic syndrome was significant in women, but not in men and therefore plays a greater role for women. Other studies found that women have a stronger inversely association between sleep duration and BMI and that women have higher PSQI scores which are more prominent to deteriorate over time [30,31,32]. Additionally, poor sleep quality is associated with altered gray matter volume in women which may develop cognitive deficits in contrast to men [33].
The study is limited by the lack of information on the presence of obstructive sleep apnea syndrome; the Pittsburgh Sleep Quality questionnaire does not cover this aspect nor was this information assessed when patients completed the questionnaire. According to a recent quality registry, covering 8157 patients with obesity 20% had been diagnosed with obstructive sleep apnea syndrome (OSAS) [34]. Multiple studies underline the effect of bariatric surgery on improvement of OSAS and therefore potentially sleep quality [35,36,37]. There was no evidence found on the relationship between sleep apnea and the PSQI. Additionally, to the limitations, the observational design is prone to selection bias. A random cohort was approached for filling out the questionnaire, rather than using a longitudinal design for follow-up of the same patient. A regression model was built to correct for variables, although included variables were scarce due to the short design of the questionnaire. Despite of its limitations, this study is one of the first to report on sleep quality using the PSQI in patients before and after bariatric surgery in the long term. For future studies, a longitudinal study is recommended, to observe the same patients and their sleep quality over time postoperatively, rather than comparing different individuals in this study as non-obese controls in other studies [11, 21, 38]. Additionally, it should take other variables into account influencing sleep quality such as the presence of sleep apnea and other physical conditions, socioeconomics, and mental disorders as sleep itself is a complex process.
Conclusion
In conclusion, sleep quality asses with a PSQI seems to improve after bariatric surgery and deteriorates in the long term to the same preoperative index. Although it does not seem to relate with weight regain as expected in the long term, this study encourages to focus on other factors associated with decreased sleep quality in postoperative patients. With this study, a starting point has been set for future studies, preferably with a prospective design.
References
Mechanick JI, Apovian C, Brethauer S, Garvey WT, Joffe AM, Kim J, et al. Clinical practice guidelines for the perioperative nutrition, metabolic, and nonsurgical support of patients undergoing bariatric procedures - 2019 update: cosponsored by American Association of Clinical Endocrinologists/American College of Endocrinology, The Obesity Society, American Society for Metabolic & Bariatric Surgery, Obesity Medicine Association, and American Society of Anesthesiologists. Surg Obes Relat Dis. 2020;16(2):175–247.
Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: a meta-analysis of prospective studies. Sleep Med. 2014;15(12):1456–62.
Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring). 2008;16(3):643–53.
Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–26.
Fatima Y, Doi SA, Mamun AA. Sleep quality and obesity in young subjects: a meta-analysis. Obes Rev. 2016;17(11):1154–66.
Lian Y, Yuan Q, Wang G, Tang F. Association between sleep quality and metabolic syndrome: a systematic review and meta-analysis. Psychiatry Res. 2019;274:66–74.
Shan Z, Ma H, Xie M, Yan P, Guo Y, Bao W, et al. Sleep duration and risk of type 2 diabetes: a meta-analysis of prospective studies. Diabetes Care. 2015;38(3):529–37.
Ogilvie RP, Patel SR. The epidemiology of sleep and obesity. Sleep Health. 2017;3(5):383–8.
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213.
Pinto TF, de Bruin PFC, de Bruin VMS, Lopes PM, Lemos FN. Obesity, hypersomnolence, and quality of sleep: the impact of bariatric surgery. Obes Surg. 2017;27(7):1775–9.
Toor P, Kim K, Buffington CK. Sleep quality and duration before and after bariatric surgery. Obes Surg. 2012;22(6):890–5.
Ghiasi F, GhalehSalami AB, Amra B, Kalidari B, Hedayat A, et al. Effects of laparoscopic sleeve gastrectomy and Roux-En-Y gastric bypass on the improvement of sleep quality, daytime sleepiness, and obstructive sleep apnea in a six-month follow-up. Tanaffos. 2020;19(1):50–9.
Kraljevic M, Kostler T, Susstrunk J, Lazaridis II, Taheri A, Zingg U, et al. Revisional surgery for insufficient loss or regain of weight after Roux-en-Y gastric bypass: biliopancreatic limb length matters. Obes Surg. 2020;30(3):804–11.
Romeijn MM, Uittenbogaart M, Janssen L, van Dielen FMH, Leclercq WKG. [Weight gain after bariatric surgery]. Ned Tijdschr Geneeskd. 2020;164.
Istfan NW, Lipartia M, Anderson WA, Hess DT, Apovian CM. Approach to the patient: management of the post-bariatric surgery patient with weight regain. J Clin Endocrinol Metab. 2021;106(1):251–63.
Cooper TC, Simmons EB, Webb K, Burns JL, Kushner RF. Trends in weight regain following Roux-en-Y gastric bypass (RYGB) bariatric surgery. Obes Surg. 2015;25(8):1474–81.
King WC, Hinerman AS, Belle SH, Wahed AS, Courcoulas AP. Comparison of the performance of common measures of weight regain after bariatric surgery for association with clinical outcomes. JAMA. 2018;320(15):1560–9.
Charuzi I, Lavie P, Peiser J, Peled R. Bariatric surgery in morbidly obese sleep-apnea patients: short- and long-term follow-up. Am J Clin Nutr. 1992;55(2 Suppl):594S-S596.
Wolnerhanssen BK, Peterli R, Hurme S, Bueter M, Helmio M, Juuti A, et al. Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy: 5-year outcomes of merged data from two randomized clinical trials (SLEEVEPASS and SM-BOSS). Br J Surg. 2021;108(1):49–57.
Thaher O, Hukauf M, Stroh C. Propensity score matching sleeve gastrectomy vs. gastric bypass with 5 years of follow-up. Obes Surg. 2021;31(12):5156–65.
Sivas F, Moran M, Yurdakul F, Ulucakoy Kocak R, Baskan B, Bodur H. Physical activity, musculoskeletal disorders, sleep, depression, and quality of life before and after bariatric surgery. Turk J Phys Med Rehabil. 2020;66(3):281–90.
Kocevska D, Barclay NL, Bramer WM, Gehrman PR, Van Someren EJW. Heritability of sleep duration and quality: a systematic review and meta-analysis. Sleep Med Rev. 2021;59:101448.
Smagula SF, Stone KL, Fabio A, Cauley JA. Risk factors for sleep disturbances in older adults: evidence from prospective studies. Sleep Med Rev. 2016;25:21–30.
Kocevska D, Lysen TS, Dotinga A, Koopman-Verhoeff ME, Luijk M, Antypa N, et al. Sleep characteristics across the lifespan in 1.1 million people from the Netherlands, United Kingdom and United States: a systematic review and meta-analysis. Nat Hum Behav. 2021;5(1):113-22
Grandner MA. Sleep, Health, and Society. Sleep Med Clin. 2022;17(2):117–39.
Muscogiuri G, Barrea L, Annunziata G, Di Somma C, Laudisio D, Colao A, et al. Obesity and sleep disturbance: the chicken or the egg? Crit Rev Food Sci Nutr. 2019;59(13):2158–65.
Roberts RE, Shema SJ, Kaplan GA. Prospective data on sleep complaints and associated risk factors in an older cohort. Psychosom Med. 1999;61(2):188–96.
Zdanys KF, Steffens DC. Sleep disturbances in the elderly. Psychiatr Clin North Am. 2015;38(4):723–41.
Yeom HE, Lee J. Sex differences in the influence of sleep on body mass index and risk of metabolic syndrome in middle-aged adults. Healthcare (Basel). 2020;8(4).
St-Onge MP, Perumean-Chaney S, Desmond R, Lewis CE, Yan LL, Person SD, et al. Gender differences in the association between sleep duration and body composition: the Cardia study. Int J Endocrinol. 2010;2010:726071.
Kim HJ, Kim REY, Kim S, Kim SA, Kim SE, Lee SK, et al. Sex differences in deterioration of sleep properties associated with aging: a 12-year longitudinal cohort study. J Clin Sleep Med. 2021;17(5):964–72.
Conklin AI, Guo SX, Tam AC, Richardson CG. Gender, stressful life events and interactions with sleep: a systematic review of determinants of adiposity in young people. BMJ Open. 2018;8(7):e019982.
Neumann N, Lotze M, Domin M. Sex-specific association of poor sleep quality with gray matter volume. Sleep. 2020;43(9).
Lodewijks Y, Akpinar E, van Montfort G, Nienhuijs S, G Dutch audit for treatment of obesity research. Impact of preoperative weight loss on postoperative weight loss revealed from a large nationwide quality registry. Obes Surg. 2022;32(1):26–32.
Zhang Y, Wang W, Yang C, Shen J, Shi M, Wang B. Improvement in nocturnal hypoxemia in obese patients with obstructive sleep apnea after bariatric surgery: a meta-analysis. Obes Surg. 2019;29(2):601–8.
Carneiro-Barrera A, Diaz-Roman A, Guillen-Riquelme A, Buela-Casal G. Weight loss and lifestyle interventions for obstructive sleep apnoea in adults: systematic review and meta-analysis. Obes Rev. 2019;20(5):750–62.
Ashrafian H, Toma T, Rowland SP, Harling L, Tan A, Efthimiou E, et al. Bariatric surgery or non-surgical weight loss for obstructive sleep apnoea? A systematic review and comparison of meta-analyses. Obes Surg. 2015;25(7):1239–50.
Salwen-Deremer JK, Schreyer C, Hymowitz GF, Montanari A, Smith MT, Coughlin JW. Sleep disturbance and insomnia in individuals seeking bariatric surgery. Surg Obes Relat Dis. 2020;16(7):940–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• Sleep quality is mostly not assessed in preoperative work up in bariatric surgery.
• The sleep quality significantly improved early after bariatric surgery.
• Age and body mass index predicted worse sleep quality.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lodewijks, Y., Schonck, F. & Nienhuijs, S. Sleep Quality Before and After Bariatric Surgery. OBES SURG 33, 279–283 (2023). https://doi.org/10.1007/s11695-022-06387-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06387-0