Abstract
Summary
The aim of this study was to examine the prospective association between symptoms of anxiety and depression and risk of fracture in older people. Results showed that men, but not women, with probable anxiety at baseline had an increased risk of fracture.
Introduction
The use of psychotropic drugs has been linked with an increased risk of fracture in older people, but there are indications that the conditions for which these drugs were prescribed may themselves influence fracture risk. The aim of this study was to investigate the relation between symptoms of anxiety and depression and risk of fracture in older people. The study design is a prospective cohort study.
Methods
One thousand eighty-seven men and 1,050 women aged 59–73 years completed the Hospital Anxiety and Depression Scale (HADS). Data on incident fracture during an average follow-up period of 5.6 years were collected through interview and a postal questionnaire.
Results
Compared to men with no or few symptoms of anxiety (score ≤7 on the HADS anxiety subscale), men with probable anxiety (score ≥11) had an increased risk of fracture: After adjustment for age and potential confounding factors, the odds ratio (OR) (95 % confidence interval) was 4.03 (1.55, 10.5). There were no associations between levels of anxiety and fracture risk in women. Few men or women had probable depression at baseline (score ≥11 on the HADS depression subscale). Amongst men with possible depression (score 8–10), there was an increased risk of fracture that was of borderline significance: multivariate-adjusted OR 3.57 (0.99, 12.9). There was no association between possible depression and fracture risk in women.
Conclusions
High levels of anxiety in older men may increase their risk of fracture. Future research needs to replicate this finding in other populations and investigate the underlying mechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is considerable evidence to link use of psychotropic drugs, such as antidepressants, antipsychotics, anxiolytics or sedatives, with an increased risk of fracture in older people [1–6]. The underlying mechanisms are unclear. One explanation might be that such drugs affect postural balance leading to a greater likelihood of falls [7]—there is evidence from a randomized controlled trial that withdrawal of psychotropic drugs reduces the risk of falling in older people [8]. Another explanation might be that some such drugs have an adverse influence on bone physiology and strength. Recent findings suggest that selective serotonin re-uptake inhibitors may decrease bone mineral density (BMD) in animals [9] and humans [1].
However, there are indications that the pharmacological properties of psychotropic drugs may be less important in determining fracture risk than the mental disorder or symptoms of psychological distress for which these drugs are being taken. A substantial reduction in the use of benzodiazepines amongst older people in New York after a statewide policy change on prescribing in its Medicaid programme showed no change in the incidence of hip fracture [10]. Consistent with this, a case–control study of fractures in the Danish population found that an increase in fracture risk was present with both current and past use of anxiolytics or sedatives, suggesting that it was the underlying condition for which the drugs were prescribed that was responsible rather than the drugs themselves [11]. Further indications of the importance of the underlying mental disorder in influencing fracture risk came from a study of lithium use and fractures amongst patients in the UK General Practice Research Database: Here, current users of lithium had a decreased risk of fracture—for reasons that remain unclear—but past use of lithium was associated with an increased risk and this rose with length of time since the drug was discontinued [12].
Studies that have examined whether common mental disorders increase risk of fracture have concentrated on depression. Their findings have been inconsistent. Higher levels of depressive symptoms were linked with increased incidence of hip fractures in people aged 25–74 years in NHANES 1 [13] and with an increased risk of vertebral and non-vertebral fracture [14] or any fracture [15] in two prospective study of older women, but in a cohort of >93,000 postmenopausal women, depressive symptoms were not associated with risk of hip, wrist or spine fractures and only weakly linked with an increased likelihood of fractures at ‘other’ sites [16], and in a large Canadian cohort of older people, there was no indication that those with higher levels of depressive symptoms had an increased risk of fracture [17]. Very little is known about the relation between symptoms of anxiety and fracture risk.
The aims of this study were to examine the associations between symptoms of anxiety and depression and subsequent risk of fracture in a cohort of community-dwelling older men and women and to explore whether the use of anxiolytics, sedatives or antidepressant drugs affects these associations.
Materials and methods
In 1998–2004, men and women born in Hertfordshire between 1931 and 1939 and still living in the county were recruited to take part in a cohort study to evaluate interactions between the genome, the intrauterine and early postnatal environment and adult lifestyle in the aetiology of chronic disorders of later life. A description of the setting up of the Hertfordshire Cohort Study has been published previously [18].
In total, 7,106 men and women born in the county between 1931 and 1939 and still living there were traced using the NHS Central Register. Of these, 3,225 (45 %) people consented to be visited at home. A research nurse administered a structured questionnaire that enquired about medical history, history of fractures since age 45 years, current medications, cigarette smoking, alcohol consumption and current or last job. A question about history of falls in the last year was included in the home interview part way through the study; falls data were therefore only collected for 2,339 people. Information on current or most recent job (in the case of married women, their husband’s job) was later used to derive social class categorized in six groups according to the OPCS Occupational Classification scheme. Diet was assessed using a food frequency questionnaire (FFQ) that was based on the EPIC questionnaire [19]. The FFQ includes 129 foods and food groups and was used to assess an average frequency of consumption of the listed foods over a 3-month period preceding the home interview. Calcium intake was calculated by multiplying the frequency of consumption of a portion of each food by its calcium content according to the UK national food composition database or manufacturers’ composition data [20]. Use of calcium supplements over the preceding 3 months was also recorded, and calcium intake from dietary supplements was calculated using the frequency and dose reported by the participant and manufacturers’ composition data. Physical activity was assessed using a previously validated questionnaire that asked about frequency of gardening, housework, climbing stairs and carrying loads in a typical week [21]. Symptoms of depression and anxiety were assessed using the Hospital Anxiety and Depression Scale (HADS) [22]. This scale was designed to identify cases of depression and anxiety using two sub-scales each of seven items. Scores range from 0 to 21, with higher scores indicating more severe symptoms. The authors of the HADS suggest cut-points for scores according to possible (8–10) or probable (≥11) depression or anxiety. Subsequently, 2,997 of those interviewed at home (93 %) attended a clinic where handgrip strength was measured three times on each side with a Jamar dynamometer. The highest of these six measurements was used to characterise muscle strength. Participants who were eligible—in this case, not taking drugs known to alter bone metabolism, such as bisphosphonates—were invited to return for bone density measurements. In total, 966 people attended for measurement of BMD using dual energy X-ray absorptiometry (DXA) at the lumbar spine and proximal femur using a Hologic QDR 4500 instrument (Vertec Scientific, Reading, UK). Measurement precision error, expressed as coefficient of variation, was 1.55 % for lumbar spine BMD, 1.45 % for total femur and 1.83 % for femoral neck BMD for the Hologic QDR 4500.
Information on fractures that occurred after the initial survey was obtained from two sources. In 2004–2005, a subset of participants resident in East Herts took part in a survey of musculoskeletal health during which they were asked “Have you broken any bones since we saw you last?” In 2007, all surviving participants who took part in the initial survey were sent a postal questionnaire in which they were asked the same question. Data from these two sources were then combined into a single variable to indicate the incidence of fracture since the initial survey. In total, 2,147 people (67 % those who took part in the initial survey) provided information about fractures that had occurred after that date. Compared to people who provided information on incident fractures at follow-up, men and women with missing data had a higher BMI (p = 0.01), were less physically active (p < 0.001), more likely to be a smoker (p < 0.001) and to be depressed (p < 0.001). Men who had missing data on incident fracture were more likely to be anxious (p = 0.01), but this difference was not present in women (p = 0.383). There were no differences in age, history of fracture or falls or alcohol and calcium intake between those with and without data on incident fracture.
The study had ethical approval from the Bedfordshire & Hertfordshire Local Research Ethics Committee and the West Hertfordshire Local Research Ethics Committee. All participants gave written informed consent.
Statistical analysis
We used the t test, chi-square test and Kruskal–Wallis test to examine differences in baseline characteristics between men and women with and without an incident fracture. We used logistic regression to examine the relation between anxiety and depression and risk of fracture, controlling for potentially confounding factors (age, BMI, physical activity, dietary calcium intake, smoking status, alcohol consumption, use of bisphosphonate drugs and history of previous fracture). As use of antidepressant or anxiolytic/sedative drugs might reduce symptoms, thereby potentially obscuring any association between symptoms of depression or anxiety and fracture, we also carried out analyses in the subsets of people who were not using antidepressants or anxiolytic/sedative drugs at baseline. The main analyses are based on 2,137 people (1,087 men and 1,050 women) with complete data on incident fracture, anxiety and depression and the covariates. Finally, we carried out some additional analyses in subsets of participants who had data on BMD, history of falls and grip strength at baseline in order to investigate whether these factors helped explain the association between anxiety and fracture. We present results for men and women separately as preliminary analyses suggested that the relation between probable anxiety and fracture risk was stronger in men than in women (p for interaction term = 0.07).
Results
During the follow-up period, 47 men and 116 women experienced an incident fracture. Table 1 shows the baseline characteristics of the men and women in this study according to whether they had an incident fracture. In both sexes, incident fracture occurred more frequently in people with a history of previous fracture. In men, fracture occurred more frequently in those with a history of smoking and in those with higher anxiety scores. There were borderline significant associations in men between younger age and lower BMI and greater frequency of fracture. In women, fracture occurred more frequently in those with a higher BMI, in those with a history of falling in the year prior to the baseline survey and in those who were taking antidepressant drugs; there was a borderline significant association between older age and greater frequency of fracture. No other characteristics were significantly associated with incident fracture in either sex.
Anxiety
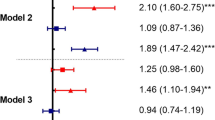
Table 2 shows the odds ratios (95 % confidence intervals) for having a fracture in men and women separately according to symptoms of anxiety at baseline. Results are shown adjusted for age and then with further adjustment for BMI, physical activity, alcohol intake, smoking status, bisphosphonate use and history of previous fracture at baseline. Men who had probable anxiety at baseline, as defined by a score of 11 or more on the HADS anxiety subscale, had a significantly increased risk of having a fracture during the follow-up period compared to those no or few symptoms of anxiety (score of 7 or less): After adjustment for age, the odds ratio (OR) (95 % confidence interval, 95 % CI) was 3.52 (1.40, 8.33). Further adjustment for potential confounding factors strengthened this association: multivariate-adjusted OR (95 % CI) 4.03 (1.55, 10.5). Only 18 men were taking anxiolytic drugs at baseline. Use of this drug was not significantly associated with risk of fracture (age-adjusted OR 1.42 (0.18, 11.0)), but exclusion of men taking these drugs strengthened the association between symptoms of anxiety and fracture: multivariate-adjusted OR (95 % CI) 4.18 (1.60, 10.9). Men whose score on the HADS anxiety subscale indicated possible anxiety (score 8–10) did not have an increased risk of fracture. In women, there was no significant difference in risk of fracture according to levels of anxiety at baseline, though there was a suggestion of higher risk amongst women with probable anxiety at baseline: age-adjusted OR (95 % CI) 1.30 (0.71, 2.39). The use of anxiolytic/sedative drugs was not associated with fracture risk in women: age-adjusted OR 1.10 (0.49, 2.50), and the association between symptoms of anxiety and fracture risk changed very little when women taking anxiolytic/sedative drugs at baseline were excluded.
In the subset of people who had reported a history of fracture since age 45 at the baseline interview (141 men, 247 women), we examined whether anxiety was associated with an increased risk of having a second fracture. Out of the 141 men with a past history of fracture, six had scores suggestive of probable anxiety at baseline and two of these experienced a second fracture during follow-up. Compared to men with no or few symptoms of anxiety at baseline, men with probable anxiety were over six times more likely to experience a second fracture: age-adjusted OR (95 % CI) 6.55 (1.01, 42.4). In the 247 women with a past history of fracture, there was no indication that probable anxiety increased the risk of having a second fracture: age-adjusted OR (95 % CI) 1.01 (0.35, 2.94).
Depression
Table 3 shows the odds ratios (95 % confidence intervals) for having a fracture in men and women separately according to symptoms of depression at baseline. Numbers of men or women with probable depression were very small, and there were too few cases of incident fracture amongst them for separate analysis. In men, there was a borderline association between having possible depression at baseline (scores on the HADS depression sub-scales 8–10) and risk of fracture: age-adjusted OR (95 % CI) 3.19 (0.90, 11.1). This was strengthened by adjustment for potential confounding factors: multivariate-adjusted OR (95 % CI) 3.57 (0.99, 12.9). There were too few men taking antidepressants drugs at baseline to allow calculation of the risk of fracture associated with use of these drugs, but exclusion of these men slightly strengthened the association between possible depression and risk of fracture: multivariate-adjusted OR (95 % CI) 3.74 (1.03, 13.6). In women, there was no significant association between having possible depression at baseline and risk of fracture: age-adjusted OR (95 % CI) 1.35 (0.56, 3.28). There was a significant association in age-adjusted analysis between use of antidepressant drugs and risk of fracture in women (OR 2.30 (1.11, 4.77)), but this was no longer significant after multivariate adjustment (OR 2.03 (0.95, 4.35)). The relation between possible depression and risk of fracture changed very little when women who were taking antidepressants at baseline were excluded.
Potential mechanisms
In subsets of men who had data on BMD, grip strength or history of falls at baseline, we investigated potential mechanisms that might explain why men with higher levels of anxiety had an increased risk of subsequent fracture. In age-adjusted regression analysis based on 347 men who had DXA scans, there was no significant linear trend between levels of anxiety and total femoral BMD (p for trend = 0.26) or lumbar spine BMD (p for trend = 0.78). There was a weak linear association between levels of anxiety and grip strength in age-adjusted analysis (p for trend = 0.04), such that men with higher anxiety levels had poorer grip strength. There was a stronger association between anxiety and falls. Likelihood of having fallen in the past year rose with increasing symptoms of anxiety: In a subset of 939 men with these data, compared to men with no or few symptoms of anxiety, the age-adjusted OR (95 % CI) for having a history of falls was 1.34 (0.76, 2.35) in men with possible anxiety and 2.10 (1.06, 4.17) in men with probable anxiety. Adjustment for history of falls did not attenuate the association between probable anxiety and incident fracture, but we may have had too few cases for accurate assessment of this inter-relationship: In the subset of 624 men with information on all three factors, there were only 23 cases of incident fracture, and none of these occurred amongst the six men who had probable anxiety and a positive history of falls at baseline.
Discussion
In this prospective study of people aged 59 to 73 years, men who had probable anxiety at baseline, as defined by a score of 11 or more on the HADS anxiety subscale, were over four times more likely to experience a fracture during the follow-up period than those who had few or no symptoms of anxiety, after adjusting for potential confounding factors. This association was strengthened by the exclusion of men taking anxiolytic or sedative drugs at baseline. Men with possible anxiety (scores 8–10 on the HADS anxiety subscale) did not have an increased risk of fracture. There was no significant association between levels of anxiety and risk of fracture in women. There were too few people with probable depression at baseline for separate analysis, but possible depression (scores 8–10 on the HADS depression subscale) was associated with an increased risk of fracture in men that was of borderline statistical significance. There was no such association in women.
We were unable to identify any previous studies that had examined the relation between anxiety per se and subsequent risk of fracture. Existing evidence from prospective studies of common mental disorders and fracture risk is almost exclusively about depression. This evidence is inconsistent, with three large studies finding that risk of fracture was increased in people with higher levels of depressive symptoms [13–15], but two other studies—equally large—finding no such association [16, 17]. One study of over 18,000 older women found that those who gained high scores on an index of mental distress—a measure that included items on symptoms of anxiety and depression—had an increased risk of subsequent fracture compared to those with low scores [23].
One mechanism that could plausibly underlie any link between anxiety or depression and subsequent fracture is bone loss. There is now a considerable body of evidence that people with depression show dysregulation of the hypothalamic–pituitary–adrenal (HPA) axis [24]. There has been less research on the relation between anxiety and the HPA axis, but some studies have found higher salivary cortisol levels in people with anxiety disorders compared to those without such symptoms [24, 25]. This dysregulation of the HPA axis may have implications for osteoporosis: In small samples of older people, higher plasma cortisol was associated with lower baseline BMD and greater rate of bone loss over a 4-year period [26, 27]. In the present study, we examined whether lower BMD might account for the association between probable anxiety and fracture in men, but we found no evidence of a trend between increasing symptoms of anxiety and lower BMD.
Another mechanism that could potentially help to explain associations between anxiety or depression and risk of fracture in older people is a propensity to fall. In prospective studies of patients with dementia and of older people in general, high levels of anxiety or depression have been linked with an increased risk of falling [28–31]. We found that men with high levels of anxiety were over twice as likely to report a history of falling in the past year as those with few or no symptoms of anxiety. It is impossible to be certain about the direction of effect in this cross-sectional analysis: The anxiety might be a consequence rather than a cause of the fall. Nevertheless, previous evidence that anxiety can predict falls, plus the observation in this study that muscle strength tended to be poorer in the men with higher anxiety, suggests that susceptibility to falling may be the main explanation for our finding that men with high levels of anxiety has an increased risk of fracture.
The fact that we found a strong association between probable anxiety and fracture in men but not in women is surprising. The epidemiology of non-vertebral fractures in men is still poorly understood [32], so the extent to which risk factors are common to both sexes remains unclear [33]. Men are more likely than women to die after hip fracture [34], suggesting greater physical frailty at the time of fracture. It may be that differences in frailty between men and women in our study play some part in our findings. It is also possible that sex differences in behavioural responses to anxiety might play a part. Further studies of the role of anxiety in fracture risk in other populations of older men and women are needed to determine whether the sex difference found here is real. Given the small size of our sample, it could be a chance finding.
Our study has a number of limitations. Firstly, the fractures were self-reported and have not been validated. Self-reports are subject to errors of recall. However, in a large study that assessed the validity of self-reported non-spine fracture using medical records, in men and women aged over 60 only 8 % of self-reported fractures proved to be false-positives and an even smaller proportion turned out to be false-negatives [35]. Secondly, our sample size is small. At the baseline survey, only a small number of participants had symptoms suggestive of probable depression so we unable to examine whether these were linked with subsequent risk of fracture. Furthermore, numbers with fracture during the follow-up period were small, particularly amongst men. This resulted in wide confidence intervals around some of our estimates of the relation between anxiety levels and fracture risk and made it impossible for us to establish with certainty whether susceptibility to falls or osteoporosis was the main underlying mechanism. Thirdly, we had no information on the date of fractures so we were unable to draw any inferences on the timing of fracture. Finally, our study is based on older people with an average age of 66 years; whether our findings apply to younger populations is uncertain.
In summary, we have shown that older men, but not women, with probable anxiety have a greater than four-fold risk of experiencing a fracture that was not explained by use of anxiolytic or sedative drugs. The reasons for this link are unclear, but it seems likely that falls and perhaps the neuromuscular ability to protect against falls [36] play a major part. Future research will need to replicate this finding in other populations of older men and women and establish the underlying mechanisms.
References
Richards JB, Papaioannou A, Adachi JD, Joseph L, Whitson HE, Prior JC et al (2007) Effect of selective serotonin reuptake inhibitors on the risk of fracture. Arch Intern Med 167(2):188–194
van den Brand MW, Pouwels S, Samson MM, van Staa TP, Thio B, Cooper C et al (2009) Use of anti-depressants and the risk of fracture of the hip or femur. Osteoporos Int 20(10):1705–1713
Pouwels S, van Staa TP, Egberts AC, Leufkens HG, Cooper C, de Vries F (2009) Antipsychotic use and the risk of hip/femur fracture: a population-based case–control study. Osteoporos Int 20(9):1499–1506
Verdel BM, Souverein PC, Egberts TC, van Staa TP, Leufkens HG, de Vries F (2010) Use of antidepressant drugs and risk of osteoporotic and non-osteoporotic fractures. Bone 47(3):604–609
Vestergaard P, Rejnmark L, Mosekilde L (2006) Anxiolytics, sedatives, antidepressants, neuroleptics and the risk of fracture. Osteoporos Int 17(6):807–816
Cumming RG, Le Couteur DG (2003) Benzodiazepines and risk of hip fractures in older people: a review of the evidence. CNS Drugs 17(11):825–837
Woolcott JC, Richardson KJ, Wiens MO, Patel B, Marin J, Khan KM et al (2009) Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med 169(21):1952–1960
Campbell AJ, Robertson MC, Gardner MM, Norton RN, Buchner DM (1999) Psychotropic medication withdrawal and a home-based exercise program to prevent falls: a randomized, controlled trial. J Am Geriatr Soc 47(7):850–853
Warden SJ, Robling AG, Sanders MS, Bliziotes MM, Turner CH (2005) Inhibition of the serotonin (5-hydroxytryptamine) transporter reduces bone accrual during growth. Endocrinology 146(2):685–693
Wagner AK, Ross-Degnan D, Gurwitz JH, Zhang F, Gilden DB, Cosler L et al (2007) Effect of New York State regulatory action on benzodiazepine prescribing and hip fracture rates. Ann Intern Med 146(2):96–103
Vestergaard P, Rejnmark L, Mosekilde L (2008) Anxiolytics and sedatives and risk of fractures: effects of half-life. Calcif Tissue Int 82(1):34–43
Wilting I, de Vries F, Thio BM, Cooper C, Heerdink ER, Leufkens HG et al (2007) Lithium use and the risk of fractures. Bone 40(5):1252–1258
Mussolino ME (2005) Depression and hip fracture risk: the NHANES I epidemiologic follow-up study. Public Health Rep 120(1):71–75
Whooley MA, Kip KE, Cauley JA, Ensrud KE, Nevitt MC, Browner WS (1999) Depression, falls, and risk of fracture in older women. Study of Osteoporotic Fractures Research Group. Arch Intern Med 159(5):484–490
Tolea MI, Black SA, Carter-Pokras OD, Kling MA (2007) Depressive symptoms as a risk factor for osteoporosis and fractures in older Mexican American women. Osteoporos Int 18(3):315–322
Spangler L, Scholes D, Brunner RL, Robbins J, Reed SD, Newton KM et al (2008) Depressive symptoms, bone loss, and fractures in postmenopausal women. J Gen Intern Med 23(5):567–574
Whitson HE, Sanders L, Pieper CF, Gold DT, Papaioannou A, Richards JB et al (2008) Depressive symptomatology and fracture risk in community-dwelling older men and women. Aging Clin Exp Res 20(6):585–592
Syddall HE, Sayer AA, Dennison EM, Martin HJ, Barker DJ, Cooper C (2005) Cohort profile: the Hertfordshire Cohort Study. Int J Epidemiol 34:1234–1242
Bingham SA, Gill C, Welch A, Day K, Cassidy A, Khaw KT et al (1994) Comparison of dietary assessment methods in nutritional epidemiology: weighed records v. 24 h recalls, food-frequency questionnaires and estimated-diet records. Br J Nutr 72(4):619–643
Robinson S, Syddall H, Jameson K, Batelaan S, Martin H, Dennison EM et al (2009) Current patterns of diet in community-dwelling older men and women: results from the Hertfordshire Cohort Study. Age Ageing 38(5):594–599
Dallosso HM, Morgan K, Bassey EJ, Ebrahim SB, Fentem PH, Arie TH (1988) Levels of customary physical activity among the old and the very old living at home. J Epidemiol Community Health 42(2):121–127
Zigmond AS, Snaith RP (1983) The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 67(6):361–370
Forsen L, Meyer HE, Sogaard AJ, Naess S, Schei B, Edna TH (1999) Mental distress and risk of hip fracture. Do broken hearts lead to broken bones? J Epidemiol Community Health 53(6):343–347
Stetler C, Miller GE (2011) Depression and hypothalamic–pituitary–adrenal activation: a quantitative summary of four decades of research. Psychosom Med 73(2):114–126
Chaudieu I, Beluche I, Norton J, Boulenger JP, Ritchie K, Ancelin ML (2008) Abnormal reactions to environmental stress in elderly persons with anxiety disorders: evidence from a population study of diurnal cortisol changes. J Affect Disord 106(3):307–313
Dennison E, Hindmarsh P, Fall C, Kellingray S, Barker D, Phillips D et al (1999) Profiles of endogenous circulating cortisol and bone mineral density in healthy elderly men. J Clin Endocrinol Metab 84(9):3058–3063
Reynolds RM, Dennison EM, Walker BR, Syddall HE, Wood PJ, Andrew R et al (2005) Cortisol secretion and rate of bone loss in a population-based cohort of elderly men and women. Calcif Tissue Int 77(3):134–138
Eriksson S, Strandberg S, Gustafson Y, Lundin-Olsson L (2009) Circumstances surrounding falls in patients with dementia in a psychogeriatric ward. Arch Gerontol Geriatr 49(1):80–87
Tinetti ME, Inouye SK, Gill TM, Doucette JT (1995) Shared risk factors for falls, incontinence, and functional dependence. Unifying the approach to geriatric syndromes. JAMA 273(17):1348–1353
Hong GR, Cho SH, Tak Y (2010) Falls among Koreans 45 years of age and older: incidence and risk factors. J Adv Nurs 66(9):2014–2024
Allan LM, Ballard CG, Rowan EN, Kenny RA (2009) Incidence and prediction of falls in dementia: a prospective study in older people. PLoS One 4(5):e5521
Seeman E, Bianchi G, Khosla S, Kanis JA, Orwoll E (2006) Bone fragility in men—where are we? Osteoporos Int 17(11):1577–1583
Geusens P, Dinant G (2007) Integrating a gender dimension into osteoporosis and fracture risk research. Gend Med 4(Suppl B):S147–S161
Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B (2010) Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing 39(2):203–209
Ismail AA, O’Neill TW, Cockerill W, Finn JD, Cannata JB, Hoszowski K et al (2000) Validity of self-report of fractures: results from a prospective study in men and women across Europe. EPOS Study Group. European Prospective Osteoporosis Study Group. Osteoporos Int 11(3):248–254
Close JC, Lord SL, Menz HB, Sherrington C (2005) What is the role of falls? Best Pract Res Clin Rheumatol 19(6):913–935
Acknowledgments
The Hertfordshire Cohort Study was funded by the Medical Research Council, the Arthritis Research Campaign, the British Heart Foundation, the National Osteoporosis Society, Wellcome Trust, the University of Southampton, the NIHR Musculoskeletal Biomedical Research Unit at the University of Oxford and the NIHR Nutrition Biomedical Research Unit at the University of Southampton.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gale, C.R., Dennison, E.M., Edwards, M. et al. Symptoms of anxiety or depression and risk of fracture in older people: the Hertfordshire Cohort Study. Arch Osteoporos 7, 59–65 (2012). https://doi.org/10.1007/s11657-012-0080-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11657-012-0080-5