Abstract
Introduction and hypothesis
Despite higher rates of depression, lower hormone replacement therapy (HRT) use, and inadequate knowledge of factors associated with osteoporosis, Mexican Americans have been understudied with regards to the association between depression, osteoporosis, and fractures. We hypothesized that depression increases the risk for osteoporosis and fractures among older Mexican American women.
Methods
Seven years of prospective data (1993–2001) from the Hispanic Established Populations for Epidemiologic Studies of the Elderly were analyzed for 1,350 women in the Southwest United States who had complete data for at least the first follow-up interview.
Results
Respondents (mean age:75) were generally poorly educated, had low income, and reported poor or fair health. High levels of depressive symptoms were reported by 31%, while new diagnosis of osteoporosis and new fractures were reported by 18 and 13%, respectively. Logistic regression analyses showed that predictors of newly diagnosed osteoporosis included age, high school (HS) education, ever having been an alcoholic, early menopause, hormone replacement therapy, and high levels of depressive symptoms. Factors predictive of new fractures included age, HS education, diabetes, early menopause, and high levels of depressive symptoms.
Conclusions
Depressive symptoms were associated with increased risk of osteoporosis and new fractures, even after controlling for other predictive factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The public health impact of osteoporosis and osteoporotic fracture is substantial. More than $10 billion are spent annually on osteoporotic fracture treatment in the US [1]. Since the number of older adults, particularly women, is projected to increase dramatically in the next three decades, the costs and impact of osteoporosis and fractures are likely to increase.
Many factors have been associated with an increased risk of osteoporosis or low bone mineral density (BMD). Being female, increasing age, low levels of estrogen, non-Hispanic White and Asian race, low weight and body mass index (BMI), family history of osteoporosis, hysterectomy, history of prior fracture, late menarche, and early menopause have all been consistently associated with low BMD [1]. Other lifestyle-related factors such as smoking, low calcium and vitamin D intake, and lack of exercise are associated with low BMD as well [1]. Certain diseases (e.g., thyroid or parathyroid disease, intestinal disease, chronic bronchitis, or emphysema) and medications (e.g., glucocorticoids) have been shown to increase the risk of developing osteoporosis [1, 2].
Several studies suggest that depression is associated with decreased BMD and osteoporosis [3–6], while others report no association [7–9]. Proposed biological mechanisms by which depression could be related to low BMD include: hypersecretion of cortisol during depressive episodes, hypogonadism, decreased growth hormone secretion or actions, and increased levels of proinflammatory cytokines such as interleukins 1 and 6 [5, 10].
Depression is also associated with falls and fractures. Depressed individuals are more likely to fall than the nondepressed [8], especially in the presence of environmental hazards such as poor lighting or uneven floors and gait problems [11]. Depressed women have a higher rate of nonvertebral and vertebral fractures even after adjustment for factors such as falls, chronic disease, and medications than nondepressed women [8]. A longitudinal study also reported high depressive symptomatology to be predictive of hip fracture after controlling for confounding factors [12]. Antidepressive medications, such as selective serotonin reuptake inhibitors (SSRI) and tricyclics, can lead to falls and their subsequent fractures [13], even when depression is included in the analysis [14].
The majority of these studies were limited by cross-sectional designs and small sample sizes, and only one study has examined this relationship in older Mexican Americans. Two studies performed follow-up measurements on a subgroup of their study population [3, 9], but reported different results. Schweiger and colleagues (2000) who compared 18 depressed patients with 21 controls reported greater bone loss among depressed participants and among men after at least a 2-year follow-up period [3]. Whooley and colleagues (2004) found no difference in mean percent change in hip and lumbar spine BMD between depressed and healthy older men after an average of 3.6 years follow-up [9]. These conflicting results could be explained by differences in study populations.
A statistically significant negative association between depression and total hip BMD was found in a relatively large sample of 1,566 Medicare enrollees, with depressed participants displaying significantly lower total hip BMD compared to nondepressed participants after controlling for BMI, age, physical activity, estrogen, gender, race, smoking, and alcohol use [4]. After stratification by gender and race, the relationship held for Caucasian women, but not Caucasian men or African Americans. In contrast to Robbins’s study [4], another large population-based study reported that major depression was associated with lower BMD for men, but not women [10]. Depression and low BMD were found to be associated in elderly Asian men as well.
Mexican Americans have been understudied with regards to the association between depression, osteoporosis, and fractures. Mexican American elderly tend to have lower hip fracture rates [15] despite similar fall rates when compared to non-Hispanic Whites [16], due possibly to body composition and a shorter hip axis [17]. Mexican Americans have higher hip fracture rates compared to African Americans [18] and other Hispanic groups such as Puerto Ricans [19]. Only one study has examined the relationship between hip fracture and depressive symptoms among older Mexican Americans. Hip fractures were not found to be predictive of depressive symptoms when controlling for other confounding factors in the cross-sectional baseline wave of the Hispanic Established Populations for the Epidemiologic Study of the Elderly (Hispanic EPESE) [20]. Proposed explanations included time lapsed since hip fracture diagnosis and increased availability of support, which can lead to speedy recovery or less functional decline.
The goal of the present study is to assess the relationship between depression, osteoporosis, and fractures using 7 years of longitudinal data from the Hispanic EPESE. This study is unique in that it takes advantage of a large community-dwelling elderly population (n = 1,350), a longitudinal design, and an understudied population: Mexican American elderly women. We hypothesize that depression increases the risk for osteoporosis and fractures in this population.
Methods
Sample
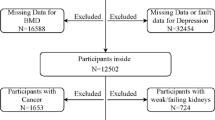
Data for this study came from the Hispanic EPESE, the first large-scale prospective cohort study of community-dwelling Mexican American elderly (for a more complete description of the methods and subject characteristics, see [21]). At baseline (1993–1994), area probability sampling resulted in a sample of 3,050 community-dwelling Mexican Americans ages 65 and over who resided in Texas, Colorado, New Mexico, Arizona, and California. These individuals represented approximately 500,000 Mexican Americans ages 65 and older who reside in the Southwest. The initial baseline wave of interviews was followed by three waves of follow-up conducted from 1995 to 1996, from 1998 to 1999, and from 2000 to 2001. Of the 3,050 baseline respondents, 1,759 were women. Since our two outcome measures (self-reported new diagnoses of osteoporosis or any fracture) were measured at the follow-up waves, the present sample included only 1,350 women who had complete data for at least the first follow-up interview. Those not included were either dead, too cognitively impaired, or too ill to complete the second interview.
Table 1 shows the distribution of sociodemographic and other health-related characteristics. At the first follow-up, the average age of the women was 75 years. Fewer than 10% had completed high school with an average formal education of 5 years. The majority (72.8%) was interviewed in Spanish. Over 45% immigrated from Mexico, and two-thirds (64.3%) had low levels of acculturation. Only 41% were currently married and 29% lived alone. Most of the women (83%) had annual household incomes less than $15,000, over half (55.1%) reported financial strain, and 6.4% had no health insurance. Almost two-thirds of the women (62.7%) rated their health as fair or poor. One-third were obese, 1.7% were alcoholic, and almost 21% were diabetic. The average number of pregnancies was six, and over 30% had a hysterectomy. Early menopause (before the age of 40) was reported by 10.9%. The overlap between these two events was minimal: less than 6% of the women had both a hysterectomy and early menopause. Hormone replacement therapy (HRT) use was recorded for 14.8% of the women and antidepressant use was recorded for 7.8%. High levels of depressive symptoms were reported by almost 31% (370 women). Fifteen women (0.8%) reported an osteoporosis diagnosis at baseline. About 18% (229 women) reported an osteoporosis diagnosis during follow-up and 13% (189 women) reported at least one new fracture during follow-up.
Measures
At all three follow-up interviews, women were asked if they had ever received a physician’s diagnosis of osteoporosis. Those who reported a diagnosis since the time of the baseline interview were coded as having newly diagnosed osteoporosis. The women were also asked if they had experienced new fractures. Those reporting fractures since the time of the baseline interview were coded as having new fractures. These included fractures of the hip, wrist, arm, shoulder, spine, foot, ankle, leg, knee, hand, or fingers.
Sociodemographic characteristics included age, years of education, language preference, level of acculturation, immigrant status, marital status, living arrangement, yearly household income, experience of financial strain, and lack of insurance coverage at baseline. Financial strain was assessed by asking how often the respondent did not have sufficient money to buy food or needed medicine at the end of the month.
Depressive symptoms were measured at baseline with the Center for Epidemiologic Studies Depression Scale (CES-D). The CES-D is the most frequently used survey of depressive symptomatology and has been found to be reliable and valid when used with the elderly. The scale includes 20 items that ask how often specific symptoms were experienced during the week prior to interview, and responses are scored on a 4-point scale, with potential total scores ranging from 0 to 60. Respondents scoring 16 or more were categorized as having a high level of depressive symptoms. Although not indicative of a diagnosis of clinical depression, this standard cutoff score has previously been shown to effectively identify individuals with clinically significant levels of depressive symptoms in other studies of older adults [22], as well as with this sample of older Mexican Americans [23].
The presence of diabetes was assessed at baseline by asking the respondents whether a physician had ever told them that they had diabetes. Persons reporting impaired glucose tolerance were not designated as having diabetes in the present analyses. Obesity was designated as those having a body mass index (BMI) of 30 or more at baseline. At the first follow-up, the women were asked their total number of pregnancies, if they ever had a hysterectomy, and the age at which they experienced menopause. Those reporting menopause prior to age 40 were categorized as having early menopause.
Self-rated health was measured at baseline with a four-item scale to ask how the respondent would rate their overall health (ranging from excellent to poor). The women were also administered the four-item CAGE, to assess having been a heavy or problem drinker at some point in their adult life. Those responding in the affirmative to one or more of the items were categorized as having been alcoholic. At baseline and the first follow-up, respondents were asked to show the prescription medications that they were currently using. Women were categorized as having hormone replacement therapy (HRT) or antidepressant medication.
Statistical analyses
The rates of self-reported newly diagnosed osteoporosis and fractures over the 7 years of study were assessed across sociodemographic characteristics, diabetic status, alcoholic status, obesity, self-rated health, number of pregnancies, hysterectomy, HRT and antidepressant use, and level of depressive symptoms. Differences were tested with chi-square analyses. Logistic regression models were used to assess first the main effect of depressive status alone, then the effect of depressive status controlling for other independent variables. All analyses incorporated weighted data and were adjusted for design effects using SUDAAN. Analyses predicting new fractures included 1,350 women, whereas analyses predicting new diagnoses of osteoporosis included only 1,335 women (15 women who had reported osteoporosis at baseline were excluded).
Results
Table 1 presents the rates of self-reported newly diagnosed osteoporosis and fractures across the sociodemographic and health-related measures. Osteoporosis was more common among those women who used antidepressant medication and those who reported high levels of depressive symptoms. Osteoporosis rates were significantly higher among 75- to 84-year-old women than either 67- to 74-year-old women or women at least 85 years of age. Osteoporosis rates were higher for women with higher education: 15.0% among those with less than 6 years of education versus 25.7% among those with 12 or more years of education. Newly diagnosed osteoporosis was also significantly more common among those women with poor or fair self-rated health, among those who had ever been alcoholic, among those who had had a hysterectomy, those who experienced early menopause, or those who used HRT. The rates of self-reported new fractures were associated with fewer measures: fractures were more common among those women who were diabetic, those who reported early menopause, and those who reported high levels of depressive symptoms.
Table 2 shows the results of logistic regression models predicting self-reported osteoporosis and new fractures. Model 1 assesses the risk of each outcome associated with high depressive symptoms alone. For both outcomes, high levels of depressive symptoms were found to be predictive: for self-reported osteoporosis, the odds ratio was 1.42 (95% confidence interval: 1.05, 1.92), and for self-reported new fractures, the odds ratio was 1.43 (95% confidence interval: 1.03, 1.99).
Model 2 assesses the risk for each outcome associated with high depressive symptoms controlling for the influence of other independent measures. Since not all independent measures were found to be predictive, the table presents more parsimonious models that include only key sociodemographic and health-related measures. As can be seen in the table, factors that proved predictive of newly diagnosed osteoporosis included age (OR:1.03, 95% confidence interval: 1.01, 1.06), high school education (OR:2.02, 95% confidence interval: 1.27, 3.21), ever having been alcoholic (OR:3.83, 95% confidence interval: 1.57, 9.36), having early menopause (OR:1.85, 95% confidence interval: 1.22, 2.81), using HRT (OR:1.46, 95% confidence interval: 1.02, 2.18), and having high levels of depressive symptoms (OR:1.39, 95% confidence interval: 1.02, 1.91). Factors that proved predictive of new fractures included age (OR:1.02, 95% confidence interval: 1.01, 1.05), high school education (OR:1.49, 95% confidence interval: 1.06, 2.54), self-report of previous diagnosis of diabetes (OR:1.58, 95% confidence interval: 1.12, 2.25), having early menopause (OR:1.62, 95% confidence interval: 1.10, 2.55), and having high levels of depressive symptoms (OR:1.39, 95% confidence level: 1.01, 1.95). The risk associated with high depressive symptoms was virtually the same for osteoporosis and new fractures and did not vary substantially between the univariate and multivariate models.
Discussion
Depressive symptomatology, our main independent variable, was found to consistently predict self-reported osteoporosis over time; even the inclusion of other significant predictors did not change its effect. Our findings support previous studies regarding this association. For example, Robbins and colleagues (2001) found depressive symptomatology to be negatively associated with total hip BMD in Caucasian women even after controlling for independent factors such as age, BMI, activity, smoking, estrogen intake, and alcohol consumption [4]. Our study also contributes evidence that depressive symptomatology is associated not only with low BMD but also with osteoporosis. Biological explanations have been proposed [1, 5, 7, 9, 10, 16]. As was the case with osteoporosis, depressive symptomatology remained a significant predictor of self-reported incident fractures. The effect of having high levels of depressive symptoms barely changed from 1.43 (model 1) to 1.39 (model 2) with the introduction of different covariates in the model. The inclusion of baseline osteoporosis in the multivariate model did not change this effect, suggesting that the association between depressive symptoms and fractures may be explained through an increased risk of falling, and not necessarily through low BMD [8, 24]. People suffering from depression may be more likely to not pay attention to how and where they walk, not turn on lights or take other needed safely precautions, potentially leading to falling.
Our study findings suggest that other factors that are associated with osteoporosis and fracture in older Mexican American women are similar to those reported for non-Hispanic Whites. Increased osteoporosis rates were found to be associated with increasing age, education, alcoholism, early menopause, and HRT medications. Experiencing new fractures was associated with increasing age and education, being diabetic, and having had an early menopause.
Women who acknowledged ever being an alcoholic or having a drinking problem during their adult life were almost four times more likely to be diagnosed with osteoporosis compared to women without a drinking problem. Human and animal studies suggest that heavy drinking compromises bone density and increases the risk of bone loss [25] and osteoporosis in females [26]. Alcohol may be toxic to osteoblasts [27] or may result in an uncoupling of bone resorption and bone formation [28]. The most pertinent explanation may be that the effect of heavy alcohol consumption on bone health cannot be reversed, so that alcoholic women are more likely to develop osteoporosis later in life, even if they stop drinking [26].
As expected [17, 29], increasing age significantly predicted the risk of osteoporosis among our cohort of elderly Mexican American women. Postmenopausal women with at least a high school education were twice as likely to report a diagnosis of osteoporosis compared with less educated women. These women are more likely to have health insurance, and thus be provided the opportunity for screening and diagnosis of osteoporosis.
Early menopause also significantly predicted osteoporosis, even when we controlled for other potential confounders. Women reporting early menopause had 85% increased odds of being diagnosed with osteoporosis during the follow-up period compared to women with normal menopause. This finding supports other findings of lower BMD among women with early menopause [30–33].
In our sample of older Mexican American women, participants who were currently on HRT were 50% more likely to report an osteoporosis diagnosis during the study follow-up period than women not on HRT. This finding was surprising, given that HRT is usually associated with increased BMD, acting thus as a protective factor [34]. The National Osteoporosis Risk Assessment study authors argue that use of HRT for less than 5 years does not preserve bone or reduce fracture risk later in life, while other authors propose against long-term HRT use due to an increased risk for breast cancer [35].
Most factors associated with osteoporosis were also found to be predictors of self-reported fracture in this sample. Early menopause seemed to be both directly and indirectly associated with fractures. These women had a 62% increased odds of reporting any new fractures compared to women with normal menopause, when osteoporosis at baseline was accounted for. An indirect effect is also possible, as these women have an increased risk for osteoporosis, which can lead to fractures. Our finding of a direct and independent effect of early menopause on incident fractures supports van der Klift et al.’s findings of an independent effect of early menopause on incident vertebral fractures among women apart from low BMD and prevalent vertebral fractures [36].
Participants who self-reported a previous physician diagnosis of diabetes were 58% more likely to also report any new fracture since baseline. Similar results were reported in the literature. Nicodemus and Folsom (2001), for example, conducted a prospective study of more than 32,000 postmenopausal women followed for 11 years [37]. Although participants with type 1 diabetes had a much higher risk of hip fracture, women with type 2 diabetes had a 1.7-fold increase in their risk for hip fractures compared to normal women. The authors proposed that the association between diabetes and hip fracture may be due to an increased risk of falling, as diabetic neuropathy or higher risk for hypoglycemia may lead to falling.
Women with at least a high school education were not only more likely to report osteoporosis, but to experience fractures as well. This effect was independent of osteoporosis, indicating that higher education may lead to an increased risk for fractures that is not related to bone mineral content. It could be that more educated women may be involved in more social activities, increasing their chances of falling and fracturing their bones.
Lastly, the older a woman is, the more likely she is to experience bone fractures. This can be due to low bone mass [2], due to an increased risk of falling [16], especially if the person is depressive [11] or cognitively impaired [14], although age-related mechanisms likely to affect bone fractures independently of BMD were also proposed [38]. This finding supports that of Espino and colleagues (2000) who, using the 1993–1996 Hispanic EPESE, showed that hip fractures were associated with increased age, although not independently of other risk factors [39].
One implication of our study is that more attention should be given to elderly Mexican American women. Due to higher rates of depression [23], lower use of HRT [40], and inadequate knowledge of factors associated with osteoporosis [41], elderly Mexican American women may be at increased risk of developing osteoporosis and fractures.
Study limitations include the use of self-reported diagnosis of osteoporosis and fractures, which will likely underestimate true levels of osteoporosis given the relatively low health insurance coverage and health care utilization by Mexican Americans compared to the general population [42, 43]. No objective measures were included in the Hispanic EPESE that we could use to confirm the presence of osteoporosis, fractures, or diabetes. We were also unable to distinguish between different types of fractures, given the small number of people for each type of fracture. Since this study represents a post hoc analysis of an already existing dataset, and the same data collection methods were used for both those with depressive symptoms and those without, potential bias in the assessment of the outcome and in the quality and extent of information obtained is minimal. Self-report of previous physician diagnosis is often used to assess the rate of osteoporosis, fractures, and/or diabetes in large-scale population studies.
Moreover, previous studies have found high sensitivity and specificity of fracture reports [44] and diabetes [45]. Similar studies are needed to assess the validity of self-reported measures of osteoporosis. Since osteoporosis can be silent for many years before it manifests as a fracture or upon dual-energy X-ray absorptiometry (DEXA) scanning, it is expected that the use of self-reported measures of osteoporosis will underestimate the true rate of osteoporosis in a population.
Another limitation of the Hispanic EPESE dataset is the lack of other health behavior variables (e.g., diet, vitamin D and calcium intake, exercise) that are risk factors for osteoporosis and fractures [20]. Assessment of vitamin D status through measurement of serum 25(OH) D level also was not performed. Although the study participants lived in the Southwest United States [20], and are likely to have received good sun exposure, this is not a guarantee of adequate vitamin D status [46].
Future research on the association between depression, osteoporosis, and fractures should consider inclusion of objective measures of vitamin D [e.g., serum 25(OH)D], cortisol status, calcium absorption, and inflammatory markers; additional questionnaire items on physical activity, sunlight exposure, and dietary intake of calcium and vitamin D; and, when feasible, direct measurement of bone mineral density using DEXA scanning. Due to the intricacy of these factors and other methodological issues in assessing calcium and vitamin D status, more extensive study is needed to further elucidate the biological mechanisms through which hypercortisolism associated with episodes of depression [5], or activation of inflammatory mechanisms, might be expected to be associated with impaired calcium absorption, vitamin D action, and/or bone homeostasis. The impact of ethnic background, specific genetic factors, local environmental conditions, and antidepressant medications on osteoporosis and fracture risk should also be explored more systematically.
In summary, this study reports a strong association between depressive symptomatology and osteoporosis and fractures, which is not changed by other factors associated with the outcomes. Depressive symptoms could be associated with fractures indirectly through their effect on osteoporosis, or directly potentially through falls. Other factors such as increasing age, higher education, and early menopause were also found to significantly and independently predict both incident osteoporosis and fractures. Programs to increase osteoporosis screening and prevent related fractures among postmenopausal Mexican American women are needed.
Abbreviations
- BMD:
-
bone mineral density
- BMI:
-
body mass index
- CES-D:
-
Center for Epidemiologic Studies Depression Scale
- Hispanic EPESE:
-
Hispanic Established Populations for the Epidemiologic Study of the Elderly
- HPA:
-
hypothalamic-pituitary-adrenocortical axis
- HRT:
-
hormone replacement therapy
- OR:
-
odds ratio
- SSRI:
-
selective serotonin reuptake inhibitors
References
NIH (2000) Consensus statement online: osteoporosis prevention, diagnosis, and therapy 17(1)
DiGiovanna A (2000) Human aging: biological perspectives. McGraw-Hill, New York
Schweiger U, Weber B, Deuschle M et al (2000) Lumbar bone mineral density in patients with major depression: evidence of increased bone loss at follow-up. Am J Psychiatry 157(1):118–120
Robbins J, Hirsch C, Whitmer R et al (2001) The association of bone mineral density and depression in an older population. J Am Geriatr Soc 49(6):732–736
Cizza G, Ravn P, Chrousos GP et al (2001) Depression: a major, unrecognized risk factor for osteoporosis? Trends Endocrinol Metab 12(5):198–203
Michelson D, Stratakis C, Hill L et al (1996) Bone mineral density in women with depression. N Engl J Med 335(16):1176–1181
Reginster JY, Deroisy R, Paul I et al (1999) Depressive vulnerability is not an independent risk factor for osteoporosis in postmenopausal women. Maturitas 33(2):133–137
Whooley MA, Kip KE, Cauley JA et al (1999) Depression, falls, and risk of fracture in older women. Study of Osteoporotic Fractures Research Group. Arch Intern Med 159(5):484–490
Whooley MA, Cauley JA, Zmuda JM, Haney EM, Glynn NW (2004) Depressive symptoms and bone mineral density in older men. J Geriatr Psychiatry Neurol 17:88–92
Alesci S, Martinez PE, Kelkar S et al (2005) Major depression is associated with significant diurnal elevations in plasma interleukin-6 levels, a shift of its circadian rhythm, and loss of physiological complexity in its secretion: clinical implications. J Clin Endocrinol Metab 90(5):2522–2530
Cesari M, Landi F, Torre S et al (2002) Prevalence and risk factors for falls in an older community-dwelling population. J Gerontol A Biol Sci Med Sci 57(11):M722–M726
Mussolino ME (2005) Depression and hip fracture risk: the NHANES III epidemiologic follow-up study. Public Health Rep 120(1):71–75
Liu B, Anderson G, Mittmann N et al (1998) Use of selective serotonin-reuptake inhibitors of tricyclic antidepressants and risk of hip fractures in elderly people. Lancet 351(9112):1303–1307
Tinetti ME, Speechley M, Ginter SF (1988) Risk factors for falls among elderly persons living in the community. N Engl J Med 319(26):1701–1707
Bauer RL, Diehl AK, Barton SA et al (1986) Risk of postmenopausal hip fracture in Mexican American women. Am J Public Health 76(8):1020–1021
Schwartz AV, Villa ML, Prill M et al (1999) Falls in older Mexican-American women. J Am Geriatr Soc 47(11):1371–1378
Villa ML, Marcus R, Ramirez Delay R et al (1995) Factors contributing to skeletal health of postmenopausal Mexican-American women. J Bone Miner Res 10(8):1233–1242
Bauer RL (1988) Ethnic differences in hip fracture: a reduced incidence in Mexican Americans. Am J Epidemiol 127(1):145–149
Lauderdale DS, Jacobsen SA, Furner SE et al (1998) Hip fracture incidence among elderly Hispanics. Am J Public Health 88(8):1245–1247
Black SA, Goodwin JS, Markides KS (1998) The association between chronic diseases and depressive symptomatology in older Mexican Americans. J Gerontol A Biol Sci Med Sci 53(3):M188–M194
Markides KS, Rudkin L, Angel RJ, Espino DV (1997) Health status of Hispanic elderly in the United States. In: LG Martin, BJ Soldo, K Foote (eds) Racial and ethnic differences in late life health in the United States. National Academy Press, Washington, DC, pp 285–300
Boyd JH, Weissman M, Thompson W, Myers JK (1982) Screening for depression in a community sample. Arch Gen Psychiatry 39:1195–1200
Black SA, Markides KS, Miller TQ (1998) Correlates of depressive symptomatology among older community-dwelling Mexican Americans: the Hispanic EPESE. J Gerontol B Psychol Sci Soc Sci 53(4):S198–S208
Lawlor DA, Patel R, Ebrahim S (2003) Association between falls in elderly women and chronic diseases and drug use: cross sectional study. BMJ 327(7417):712–717
Hannan MT, Felson DT, Dawson-Hughes B et al (2000) Risk factors for longitudinal bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res 15(4):710–720
Sampson HW (2002) Alcohol and other factors affecting osteoporosis risk in women. Alcohol Res Health 26(4):292–298
Labib M, Abdel-Kader M, Ranganath L et al (1989) Bone disease in chronic alcoholism: the value of plasma osteocalcin measurement. Alcohol Alcohol 24(2):141–144
Schnitzler CM, Solomon L (1984) Bone changes after alcohol abuse. S Afr Med J 66(19):730–734
Siris ES, Miller PD, Barrett-Connor E et al (2001) Identification and fracture outcomes of undiagnosed low bone mineral density in postmenopausal women: results from the National Osteoporosis Risk Assessment. JAMA 286(22):2815–2822
Ohta H, Sugimoto I, Masuda A et al (1996) Decreased bone mineral density associated with early menopause progresses for at least ten years: cross-sectional comparisons between early and normal menopausal women. Bone 18(3):227–231
Pouilles JM, Tremollieres F, Bonneu M et al (1994) Influence of early age at menopause on vertebral bone mass. J Bone Miner Res 9(3):311–315
Hadjidakis D, Kokkinakis E, Sfakianakis M et al (1999) The type and time of menopause as decisive factors for bone mass changes. Eur J Clin Invest 29(10):877–885
Hadjidakis DJ, Kokkinakis EP, Sfakianakis ME et al (2003) Bone density patterns after normal and premature menopause. Maturitas 44(4):279–286
Barrett-Connor E, Wehren LE, Siris ES et al (2003) Recency and duration of postmenopausal hormone therapy: effects on bone mineral density and fracture risk in the National Osteoporosis Risk Assessment (NORA) study. Menopause 10(5):412–419
Baber RJ, O’Hara JL, Boyle FM (2003) Hormone replacement therapy: to use or not to use? Med J Aust 178(12):630–633
van der Klift M, de Laet CE, McCloskey EV et al (2004) Risk factors for incident vertebral fractures in men and women: the Rotterdam Study. J Bone Miner Res 19(7):1172–1180
Nicodemus KK, Folsom AR (2001) Type 1 and type 2 diabetes and incident hip fractures in postmenopausal women. Diabetes Care 24(7):1192–1197
Huang C, Ross PD, Fujiwara S et al (1996) Determinants of vertebral fracture prevalence among native Japanese women and women of Japanese descent living in Hawaii. Bone 18(5):437–442
Espino DV, Palmer RF, Miles TP et al (2000) Prevalence, incidence, and risk factors associated with hip fractures in community-dwelling older Mexican Americans: results of the Hispanic EPESE study. Establish Population for the Epidemiologic Study for the Elderly. J Am Geriatr Soc 48(10):1252–1260
Newell DA, Markides KS, Ray LA et al (2001) Postmenopausal hormone replacement therapy use by older Mexican-American women. J Am Geriatr Soc 49(8):1046–1051
Orces CH, Casas C, Lee S, Garcia-Cavazos R, White W (2003) Determinants of osteoporosis prevention in low-income Mexican-American women. South Med J 96(5):458–464
Ray LA, Black SA (2003) Self-reported health services utilization. In: Black SA, Markides KS, Miranda M (eds) Established populations for epidemiologic studies of the elderly: the Hispanic EPESE resource data book. National Institute on Aging, Washington, DC
Carter-Pokras O, Zambrana RE (2001) Latino health status. In: Aguirre-Molina M, Molina CW, Zambrana RE (eds) Health issues in the Latino community. Jossey-Bass, San Francisco, CA
Chen Z, Kooperberg C, Pettinger MB et al (2004) Validity of self-report for fractures among a multiethnic cohort of postmenopausal women: results from the Women’s Health Initiative observational study and clinical trials. Menopause 11(3):264–274
Okura Y, Urban LH, Mahoney DW et al (2004) Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol 57(10):1096–1103
Lucas JA, Bolland MJ, Grey AB et al (2005) Determinants of vitamin D status in older women living in a subtropical climate. Osteoporos Int 16(12):1641–1648
Acknowledgement
Dr. Black gratefully acknowledges NIDDK (R01 DK51261) and National Institute on Aging (T32 AG00262) funding support during data analysis and preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Tolea, M.I., Black, S.A., Carter-Pokras, O.D. et al. Depressive symptoms as a risk factor for osteoporosis and fractures in older Mexican American women. Osteoporos Int 18, 315–322 (2007). https://doi.org/10.1007/s00198-006-0242-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-006-0242-7