Abstract
Background
It is not uncommon for medical specialists to predominantly care for patients with certain chronic conditions rather than primary care physicians (PCPs), yet the resource implications from such patterns of care are not well understood.
Objective
To assess resource use of diabetes patients who predominantly visit a PCP versus a medical specialist.
Design
Retrospective cohort study of diabetes patients aging into the traditional Medicare program. Patients were attributed to a PCP or medical specialist annually based on a preponderance of ambulatory care visits and categorized according to whether attribution changed year to year. Propensity score weighting was used to balance baseline demographic characteristics, diabetes complications, and underlying health conditions between patients attributed to PCPs and to medical specialists. Spending and utilization were measured up to 3 patient-years.
Subjects
A total of 141,558 patient-years.
Main Measures
Total visits, unique physicians, hospital admissions, emergency department visits, procedures, imaging, and tests.
Key Results
Each year, roughly 70% of patients maintained attribution to a PCP and 15% to a medical specialist relative to the previous year. After propensity weighting, patients continuously attributed to a PCP versus medical specialist from 1 year to the next had lower average total payer payments ($10,326 [SD $57,386] versus $14,971 [SD $74,112], P<0.0001) and lower total patient out-of-pocket payments ($1,707 [SD $6,020] versus $2,443 [SD $7,984], P<0.0001). Rates of hospitalization, emergency department visits, procedures, imaging, and tests were lower among patients attributed to PCPs as well.
Conclusions
Older adults with diabetes who receive more of their ambulatory care from a PCP instead of a medical specialist show evidence of lower resource use.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
INTRODUCTION
Primary care is commonly upheld as a fundamental component of the health care system and a comprehensive source of patients’ preventive, treatment, and management care needs.1,2,3 While primary care physicians (PCPs) have traditionally addressed patients’ primary care needs, medical specialists may also function as a source of primary care.4, 5
Roughly half of traditional Medicare patients predominantly visit a clinician who is not a PCP,6 and approximately 1 in 5 of them receive a majority of their ambulatory care from medical specialists.7 While patients may rely on the expertise of specialists for specific health needs, they may also do so for their general health needs.8, 9 Specialists may have a more intense practice style compared with PCPs,10 but they may also be able to deliver higher quality condition-specific care.5, 11, 12
It is challenging to study the effects of PCPs and medical specialists on resource use because sicker patients tend to need more care, which is why receiving more of their care from specialists may be warranted.9 Thoroughly accounting for patients’ illness burden is difficult in observational studies since secondary data may not fully capture differences in health status across patients.11 In an effort to address as much patient heterogeneity as possible, this study focuses on patients who newly entered the Medicare program at age 65 and have diabetes, which has complications that are well captured in administrative data and can be treated by PCPs or certain medical specialists such as endocrinologists or nephrologists.13 Our hypothesis is that spending and utilization are greater when a diabetes patient predominantly visits a medical specialist.
METHODS
Using administrative data, a cohort of fee-for-service Medicare beneficiaries was identified who entered the program at age 65 with an active diagnosis of diabetes mellitus. Then, each beneficiary’s visit patterns were tracked up to 5 years to determine whether a PCP or a medical specialist was the beneficiary’s predominant physician each year. Resource use was measured over 3 years while accounting for each beneficiary’s underlying conditions and diabetes complications. Limiting the study population to diabetes beneficiaries who aged into the Medicare program in the same year created a relatively homogenous cohort with a medical history captured by claims data covering approximately the same period of time.
Study Population
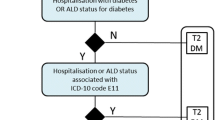
Non-disabled beneficiaries who did not have end-stage renal disease and who became eligible for Medicare coverage at age 65 in 2011 were identified from the 20% sample of beneficiaries in the Master Beneficiary Summary File (MBSF) of the Chronic Conditions Warehouse (CCW).14 Beneficiaries were restricted to those alive and continuously enrolled in full fee-for-service Medicare from the time of enrollment in 2011 through the end of 2012 and further restricted to those who ever had a diabetes diagnosis through 2012 according to the CCW. The resource use of the resulting cohort was measured from 2013 through 2015 or until death or loss of full fee-for-service coverage.
Physician Identification and Patient Attribution
The physician specialty code most billed by a unique national provider identifier (NPI) in the 20% sample of Carrier claims from 2011 through 2015 was used to identify PCPs and medical specialists for purposes of patient attribution (Supplemental Table 1). If a physician had an equal number of bills under a PCP or specialist specialty code, then the physician was deemed a specialist.
Each patient eligible for attribution to a physician must have had at least 1 ambulatory evaluation and management visit with a PCP or medical specialist in Carrier claims data or a visit to a rural health center or federally qualified health clinic in outpatient claims data (Supplemental Table 2). Patients were initially attributed to an individual PCP or medical specialist based on a plurality of visits starting when a patient enrolled in Medicare in 2011 through the end of 2012, which has been shown to be a robust method of attribution to a usual care physician for diabetes patients.15, 16 Then, the cohort’s visits continued to be tracked in 2013, 2014, and 2015 to allow attribution to an individual PCP or medical specialist in each year.
We did not restrict patient attribution to a certain type of medical specialist. Visits with more than 1 physician could occur the same day, but multiple visits with the same physician on the same day were counted only once. In cases where a patient had an equal number of visits with a PCP and a medical specialist, the patient was attributed to the specialist. If a patient had no visits in 1 year, then his or her attribution to a PCP or medical specialist continued from the prior year. Patients attributed to a PCP or medical specialist in more than 1 year were not necessarily attributed to the same physician. A patient observed for a partial year from loss of fee-for-service Medicare coverage could be observed in subsequent years if coverage was regained.
After annual attribution, each patient’s PCP and medical specialist attribution patterns between years were categorized into a 4-category variable to capture any changes in attribution over time (Fig. 1). A patient’s current-year attribution was compared against the previous year’s attribution to determine whether the patient (1) maintained attribution to a PCP, (2) maintained attribution to a medical specialist, (3) switched attribution from a PCP to a medical specialist, or (4) switched attribution from a medical specialist to a PCP. This variable was created for 2013 with initial attribution in 2011–2012 considered the previous year, for 2014 with 2013 as its previous year, and for 2015 with 2014 as its previous year. While all attribution categories were compared, the focus of the analysis was on the comparison between patients maintaining attribution to a PCP and those maintaining attribution to a medical specialist since switching attribution likely represents changing health status and would be expected to result in changes in resource use.
Measuring Utilization and Spending Outcomes
Visit patterns were measured each year in 2013, 2014, and 2015 to capture patients’ total visits with PCPs, medical specialists, surgical specialists, and other specialists as well as the number of unique PCPs, medical specialists, surgical specialists, and other specialists visited (Supplemental Table 1).
Other utilization and spending measures were gleaned from the annual CCW Cost and Use File for 2013, 2014, and 2015. Utilization included acute inpatient stays, emergency department (ED) visits, and the major Berenson-Eggers Type of Service (BETOS) categories of imaging, tests, and procedures. ED visits were counted as visits alone or as inpatient admissions through the ED. Part A and Part B Medicare payments, add-on payments, and other primary payer payments were aggregated across all care settings to produce total payer payments; patient coinsurance and deductible (out-of-pocket) payments were tabulated separately.
All utilization and spending measures were measured in each of the 3 years between 2013 and 2015 and scaled by the number of months patients had fee-for-service coverage so that those who were alive or enrolled in fee-for-service Medicare for only some months of a year were measured on an equivalent basis with patients enrolled a full year.
Patient Baseline Characteristics
A patient-year data set was created where patients appeared up to 3 years in the data to study the relationships between combinations of PCP and specialist attribution patterns in a current and previous year and their annual outcomes. Outcomes included total payer payments and patient payments; total number of visits and unique physicians; inpatient admissions; ED visits; and imaging, tests, and procedures. Each payment type was Winsorized at its 99th percentile across all observations.
The 2012 MBSF was used to source the patient characteristics sex (female versus not) and race or ethnicity (Black, Hispanic, Asian, or other race versus non-Hispanic White). Medicaid dual-eligible status was defined according to whether a patient had at least 1 month of Medicaid coverage through 2015, as determined by the 2011–2015 MBSF. Patient Zip Code in 2012 from the MBSF was used to determine median household income from the US Census at the Zip Code Tabulation Area level to control for the possibility that patients with greater financial means may have better access to specialists and hospital referral region (HRR) to control for regional treatment intensity.17, 18
Diabetes complications were flagged using diagnosis codes in 2011 and 2012 inpatient, outpatient, and Carrier claims data according to the diabetes complication and severe complication categories of a validated algorithm (Supplemental Table 3).13 To capture chronic illness burden, 22 chronic illnesses diagnosed through 2012 from the Chronic Condition Summary File were grouped into 7 clinically similar condition categories (Supplemental Table 4). Occurrence of the acute conditions acute myocardial infarction, hip fracture, or stroke was flagged as well.
Statistical Analysis
Probability weights, or the inverse of the fraction of patients in each attribution pattern category, were used to account for large sample size imbalances across the 4 levels. These weights were applied to a multinomial logistic regression model, where the outcome was the 4-category attribution variable regressed on the following covariates: patients’ baseline demographic characteristics, diabetes complications, presence of acute or chronic conditions, and total number of chronic conditions. Year fixed effects as well as HRR fixed effects were included. The predicted probability that a patient was attributed to his or her actual attribution pattern category was used to calculate inverse propensity weights (IPWs), or the inverse of the given predicted probability, for each patient. These IPWs were applied to each covariate in the multinomial model to assess weighted covariate balance across attribution pattern categories at baseline, with ANOVA used to test for whether the weighted means significantly differed. We also applied the weights to calculate means of the outcomes across attribution pattern categories, using ANOVA to test for differences and a post hoc Scheffe test to specifically measure the difference in weighted means between the continuous PCP and medical specialist categories.
All analyses were performed using SAS-EG (version 7.15), with the multinomial logistic regression model run using the CATMOD procedure.
RESULTS
Among the 141,558 patient-years in the study sample, the majority were attributed continuously to PCPs (70.8%) from 1 year to the next; almost 15% had continuous attribution to a medical specialist; and about 15% had attribution that switched, either from a medical specialist or from a PCP (Table 1). In the unweighted comparison of baseline patient characteristics across attribution pattern categories, all variables except female were significantly different (P<0.0001) (Supplemental Table 5). In particular, patients attributed to medical specialists had higher cardiovascular and renal disease and diabetes complications, as expected. After propensity weighting, all baseline variables, including illness measures, were balanced across categories and no longer statistically significant (P>0.05). A little more than half of the weighted sample was female, about 75% was White, and about 15% was dually eligible for Medicaid.
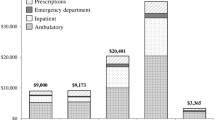
With propensity weighting, patients continuously attributed to PCPs had lower mean spending and utilization compared with those continuously attributed to medical specialists. Annual total payer payments averaged $10,326 for patients continuously attributed to a PCP, compared with $14,971 for those continuously attributed to a medical specialist (Table 2 and Fig. 2). Total patient out-of-pocket payments averaged $736 lower for patients continuously attributed to a PCP ($1,707 versus $2,443). Payments were highest for patients who switched from a PCP to a medical specialist (payer payments $17,350; patient payments $2,896).
Weighted means of PCP and medical specialist attribution patterns and spending from 2013 to 2015. Total number of patient-years in all models was 141,558. Weighted means after balancing patient demographic characteristics, diabetes complications, and comorbid conditions. Means shown with 95% confidence intervals; differences statistically significant (P<0.0001).
In terms of utilization, the weighted mean number of total visits was 11.7 for patients continuously attributed to PCPs and 13.2 for patients continuously attributed to medical specialists, with a similar mean number of physicians visited (5.2 and 5.9 physicians). As expected, patients with PCP attribution had more visits with PCPs, and those with medical specialist attribution had more visits with medical specialists. Patients continuously attributed to a PCP versus a medical specialist averaged a slightly lower rate of hospitalization (0.30 versus 0.39) and ED visit (0.61 versus 0.70). They had on average 1.7 fewer procedures, 1.0 fewer imaging services, and 4.2 fewer tests.
The weighted means of all outcomes were significantly different (P<0.05) between patients continuously attributed to a PCP versus a medical specialist according to the Scheffe test.
DISCUSSION
We found that soon after entering the Medicare program at age 65, diabetes patients were associated with more payer and patient spending and utilization when they consistently visited a medical specialist instead of a PCP. Why might patients who predominantly visit medical specialists be associated with more spending than those who visit PCPs? Patients who mainly visit a medical specialist may be subject to referrals to additional specialists and a more intense practice style, with higher frequency of ordering more discretionary services such as procedures, imaging, and tests and less conservative management of common medical symptoms.6, 10, 12, 19
At the same time, specialists are trained to treat patients with advanced health problems specific to their area of medical expertise and, thus, may lead PCPs to refer sicker patients to them.12, 20 Specialists may also provide higher quality disease-specific care; for example, patients of endocrinologists may have lower rates of foot ulcers and better performance on diabetes process of care measures.21, 22 Although we did not formally measure quality in this study, the difference in total spending between patients continuously attributed to PCPs and medical specialists appears to be driven by visits and discretionary services, with very small differences in hospital admissions and ED visits, which we believe are not clinically meaningful and, thus, may indicate residual confounding by disease severity and no substantive differences in quality of care.
Studying resource use between PCPs and medical specialists has been notoriously challenging because patient disease severity is difficult to precisely measure and, thus, know when more intense care from specialists is necessary. Our goal was to study this research question by designing the most rigorous, generalizable observational study with the data available. We selected a cohort that aged into the Medicare program during the same year to minimize differences in age-related health status and restricted to patients with diabetes because diabetes complications and co-occurring conditions are capture well in claims data. We further characterized patients who visited a PCP versus a medical specialist according to whether their attribution stayed the same or switched from year to year, focusing on the patients whose attribution was consistent across years. Finally, we weighted measurable patient demographic and health characteristics so that they were the same between patients who consistently visited a PCP or medical specialist or switched between them.
We did not have access to electronic health record data containing individual biologic or social measures such as social supports, formal education level, or housing environment, which might provide additional controls for health status but are not widely available. A randomized controlled trial would be ideal to study resource use between PCPs and medical specialists, although it may not be feasible in a real-world practice environment where patient preferences for visiting their personal physician may limit enrollment. Therefore, our study makes a valuable contribution toward better understanding the relationships between physician specialty and resource use that may not be able to be investigated with other research study designs.
We acknowledge that our study has a number of limitations. Foremost, we cannot assert a causal relationship between specialty type and resource use in this observational study. While we strove to minimize the confounding effects of patients’ diabetes complications and underlying conditions, some patients may have visited more specialists and had higher spending because they became sicker in ways that we could not adequately measure. That the highest levels of spending and utilization were for patients who switched from mainly visiting a PCP to a medical specialist emphasizes this point, as these patients likely experienced worsening severity of existing health conditions or had new diagnoses. Patients in the cohort were diagnosed with diabetes and all in their late 60s, so their results may not be generalizable to patients with other conditions or other age groups. Attributing patients each year to the most commonly visited specialty, rather than an individual physician, may underestimate the potential disruptions to longitudinal relationships that may be occurring at the individual physician level. Similarly, we did not include visits with physician assistants or nurse practitioners, who may have played a distinct role in a patient’s longitudinal care. Although our study was unable to identify physician practice affiliations, our results would be unchanged where patients predominantly visited different physicians within the same single-specialty practice across years.
Important for the implications of this study, we were unable to tease apart physician- or patient-related explanations for why some patients predominantly visit specialists and whether physicians or patients drive greater resource use. While differences in practice patterns between PCPs and specialists for similar patients may be one explanation, some patients may prefer specialists and more intensive testing and treatments. Much more investigation is needed to understand the relationships between patient-physician attribution and resource use. A nudge trial could test incentives that address physician referral patterns or patient care-seeking behavior to better understand whether physician practice patterns or patient preferences drive resource use. Patients may not fully understand the advantages of the generalist orientation of PCPs, namely comprehensive management of comorbid conditions,23,24,25 with coordination of care across specialists.9, 26,27,28 Providing patients with information about the different practice styles of PCPs and medical specialists might lessen their desire to seek care initially from medical specialists, particularly in the traditional Medicare program, where patients can seek care without any physician network constraints. Additionally, primary care models are being tested through the Center for Medicare & Medicaid Innovation,29 and payment reforms could shape the delivery of care around PCPs.
Yet if true, our findings hold implications for health policy. It appears that regularly visiting a PCP may affect a patient’s resource-use trajectory, specifically for older adults with diabetes enrolling in the Medicare program. Encouraging newly enrolled diabetes patients to seek their primary care from a PCP rather than a medical specialist could be a mechanism to reduce higher cost patterns of care, both for the Medicare program and for patients themselves.
References
Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q 2005;83(3)457-502.
Safran DG. Defining the future of primary care: what can we learn from patients? Ann Intern Med 2003;138(3):248-255.
Primary Care: American’s Health in a New Era. National Academy of Sciences. Institute of Medicine. 1996.
Friedberg MW, Hussey PS, Schneider EC. Primary care: A critical review of the evidence on quality and costs of health care. Health Aff 2010;29(5):5766-5772.
Harrold LR, Field TS, Gurwitz JH. Knowledge, patterns of care, and outcomes of care for generalists and specialists. J Gen Intern Med 1999;14(8):499-511.
Our Parents, Ourselves: Health Care for an Aging Population. The Dartmouth Institute of Health Policy & Clinical Practice. 2016. Available at: https://www.dartmouthatlas.org/downloads/reports/Our_Parents_Ourselves_021716.pdf. Accessed 10 March 2020.
Rosenblatt RA, Hart LG, Baldwin LM, Chan L, Schneeweiss R. The generalist role of specialty physicians: is there a hidden system of primary care? JAMA. 1998;279(17):1364-1370.
Fryer GE, Consoli R, Miyoshi TJ, Dovey SM, Phillips RL, Green LA. Specialist physicians providing primary care services in Colorado. J Am Board Fam Med 2004;17(2):81-90.
Bynum JPW, Chang C-H, Austin A, Carmichael D, Meara E. Outcomes in older adults with multimorbidity associated with predominant provider of care specialty. J Am Geriatr Soc 2017;65(9):1916-1923.
Grumbach K. The ramifications of specialty-dominated medicine. Health Aff 2002;21(1):155-157.
Smetana GW, Landon BE, Bindman AB, et al. A comparison of outcomes resulting from generalist vs specialist care for a single discrete medical condition: a systematic review and methodologic critique. Arch Intern Med 2007;167(1):10-20.
Donohoe MT. Comparing generalist and specialty care: discrepancies, deficiencies, and excesses. Arch Intern Med 1998;158:1596-1608.
Young BA, Lin E, Von Korff M, et al. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care 2005;14(1):15-23.
Chronic Conditions Data Warehouse. Medicare Claims. 2020. Available at: https://www2.ccwdata.org/web/guest/data-dictionaries. Accessed 16 April 2020.
DuGoff EH, Walden E, Ronk K, Palta M, Smith M. Can claims data algorithms identify the physician of record? Med Care 2018;56(3):e16-e20.
Shah BR, Hux JE, Laupacis A, Zinman B, Cauch-Dudek K, Booth GL. Administrative data algorithms can describe ambulatory physician utilization. Health Serv Res 2007;42(4):1783-1796.
U.S. Census. Microdata. 2020. Available at: data.census.gov. Accessed 16 April 2020.
van Doorslaer E, Wagstaff A, van der Burg H, et al. Equity in the delivery of health care in Europe and the US. J Health Econ 2000;19(5):553-583.
Greenfield S, Nelson EC, Zubkoff M, et al. Variations in resource utilization among medical specialties and systems of care: results from the medical outcomes study. JAMA. 1992;267(12):1624-1630.
Forrest CB. A typology of specialists’ clinical roles. Arch Intern Med 2009;169(11):1062-1068.
Greenfield S, Rogers W, Mangotich M, Carney MF, Tarlov AR. Outcomes of patients with hypertension and non-insulin-dependent diabetes mellitus treated by different systems and specialties: results from the medical outcomes study. JAMA. 1995;274(18):1436-1444.
Chin MH, Zhang JX, Merrell K. Specialty differences in the care of older patients with diabetes. Med Care 2000;38(2):131-140.
Enthoven AC, Crosson FJ, Shortell SM. Redefining health care: medical homes or archipelagos to navigate? Health Aff 2007;26(5):1366-1372.
Society of General Internal Medicine Task Force on the Domain of General Internal Medicine. Health care system chaos should spur innovation: summary of a report of the Society of General Internal Medicine Task Force on the Domain of General Internal Medicine. Ann Intern Med 2004;140(8):639-643.
Grumbach K. Chronic illness, comorbidities, and the need for medical generalism. Ann Fam Med 2003;1(1):4-7.
Stille CJ, Jerant A, Bell D, Meltzer D, Elmore JG. Coordinating care across diseases, settings, and clinicians: a key role for the generalist in practice. Ann Intern Med 2005;142(8):700-708.
Rothman AA, Wagner EH. Chronic illness management: what is the role of primary care? Ann Intern Med 2003;138(3):256-261.
Starfield B, Lemke KW, Bernhardt T, Foldes SS, Forrest CB, Weiner JP. Comorbidity: implications for the importance of primary care in “case” management. Ann Fam Med 2003;1(1):8-14.
Centers for Medicare & Medicaid Services. Primary Care First Model Options. Available at: https://innovation.cms.gov/innovation-models/primary-care-first-model-options. Accessed 29 Dec 2020.
Contributors
N/A
Funding
This research was supported in part by the National Institute on Aging (grant number PO1 AG19783).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The funder played no role in this study’s design, analysis, or interpretation, or in the preparation of the manuscript. This research was conducted while the lead author was an employee of the Centers for Medicare & Medicaid Services. This paper does not necessarily represent the official views of the US Department of Health and Human Services or any of its agencies.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior presentations
Poster at 2018 AcademyHealth Annual Research Meeting in Seattle, WA
Supplementary Information
ESM 1
(DOCX 34.8 kb)
Rights and permissions
About this article
Cite this article
Nyweide, D.J., Austin, A.M. & Bynum, J.P.W. Resource Use Among Diabetes Patients Who Mainly Visit Primary Care Physicians Versus Medical Specialists: a Retrospective Cohort Study. J GEN INTERN MED 37, 283–289 (2022). https://doi.org/10.1007/s11606-021-06710-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-06710-y