Abstract
Purpose
Resource utilization and costs in Cushing’s disease (CD) patients have not been studied extensively. We compared CD patients with diabetes mellitus (DM) patients and population-based controls to characterize differences in utilization and costs.
Methods
Using 2008–2012 MarketScan® database, we identified three patient groups: (1) CD patients; (2) DM patients; and (3) population-based control patients without CD. DM and control patients were matched to CD patients by age, gender, region, and review year in a 2:1 ratio. Outcomes included annual healthcare resource utilization and costs.
Results
There were 1852 CD patients, 3704 DM patients and 3704 controls. Mean age was 42.9 years; 78.2 % were female. CD patients were hospitalized more frequently (19.3 %) than DM patients (11.0 %, p < .001) or controls (5.6 %, p < .001). CD patients visited the ED more frequently (25.4 %) than DM patients (21.1 %, p < .001) or controls (14.3 %, p < .001). CD patients had more office visits than DM patients (19.1 vs. 10.7, p < .001) or controls (7.1, p < .001). CD patients on average filled more prescriptions than DM patients (51.7 vs. 42.7, p < .001) or controls (20.5, p < .001). Mean total healthcare costs for CD patients were $26,269 versus $12,282 for DM patients (p < .001) and $5869 for controls (p < .001).
Conclusions
CD patients had significantly higher annual rates of healthcare resource utilization compared to matched DM patients and population controls without CD. CD patient costs were double DM costs and quadruple control costs. This study puts into context the additional burdens of CD over DM, a common, chronic endocrine condition affecting multiple organ systems, and population controls.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cushing’s disease (CD) is typically caused by a pituitary tumor producing excessive adrenocorticotropic hormone (ACTH), leading to exposure to excess cortisol [1]. CD has an estimated incidence of eight cases per million in the United States, and it is estimated to account for 70 % of all cases of Cushing’s syndrome [2, 3]. CD is associated with substantial morbidity, including obesity, hypertension, irregular menses, glucose intolerance, bone fractures, and kidney stones, as well as mortality [3, 4].
There are limited US data on CD-related healthcare costs and resource utilization. One prior study combining two US claims databases estimated mean overall costs at nearly $35,000 per patient, over 40 % of which was attributed to direct CD-related costs [5]. A prior analysis of MarketScan® and Medicare insurance databases from 2004 to 2008 found that patients with CD accrue significantly higher healthcare costs per annum compared to normal population-based controls and patients with non-secreting pituitary adenomas [6]. A study of the Optum Research Database found that monthly all-cause costs for CD patients were higher than for controls ($3224 vs. $485, p < .001) [7]. Another study examining the 1993–2002 Nationwide Inpatient Sample found that the average total charges of patients with CD undergoing transsphenoidal surgical resection of pituitary tumors were $25,732, with increasing costs based on the number of inpatient complications [8]. The paucity of information on healthcare costs and resource utilization in patients with CD represents an unmet clinical and research need.
Moreover, comparisons of outcomes between CD and other important conditions of the endocrine system, such as diabetes mellitus (DM), have not been previously published. Such studies would provide greater context to the burden of illness that patients with CD face. The goal of the current study was to compare the healthcare costs and resource utilization of patients with CD with two groups: patients with DM and population-based controls.
Methods
We conducted a retrospective matched cohort study using the Truven Health Analytics MarketScan® Database (Truven Health Analytics, Ann Arbor, MI), a Health Insurance Portability and Accountability Act (HIPAA)-compliant administrative claims database. The study timeframe was 1/1/2008 to 12/31/2012.
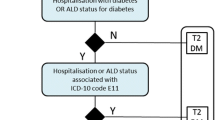
We identified three groups of patients from the database: (1) patients with CD; (2) patients with DM; and (3) population-based control patients without CD. First, we identified all patients with CD. Inclusion criteria for CD patients included the following [9]:
-
A medical claim with a diagnosis of Cushing’s syndrome (International Classification of Diseases, 9th Revision, Clinical Modification [ICD-9-CM]: 255.0); and
-
A medical claim associated with a diagnosis of pituitary neoplasm (ICD-9-CM: 227.3, 237.0); a pituitary disorder such as hyperfunction (ICD-9-CM: 253.1), hypothalamic control of anterior pituitary (ICD-9-CM: 253.9), syndromes of diencephalohypophyseal origin (ICD-9-CM: 253.8), and other anterior pituitary disorders (ICD-9-CM: 253.4); hypophysectomy (ICD-9-CM procedure: 07.61–07.65, 07.68, 07.69; Current Procedure Terminology [CPT]: 61546, 61548, 62165); cranial stereotactic radiosurgery (CPT: 61796-61799, 77371, 77372); or bilateral inferior petrosal sinus sampling (CPT: 36012, 75860) with cortisol or adrenocorticotropic hormone sampling (CPT: 82924, 82530, 82533); and
-
Continuous enrollment for one calendar year after the first CD-related claim (review period).
Population-based controls were obtained from a random 5 % sample of all enrollees in the database. Controls were defined as those who had no claim of Cushing’s syndrome or CD in the study timeframe and were continuously enrolled for at least one calendar year during the study timeframe. We matched control patients with CD patients by age (in years), gender, region, and year of the review period in a 2:1 ratio. CD patients without two control matches were excluded from the final cohort.
In a similar manner, DM patients without CD were obtained from a random 5 % sample of all enrollees in the database. Patients with DM were defined as those who had at least two claims with a diagnosis of DM (ICD-9-CM: 250.x), no claim of Cushing’s syndrome or CD in the study timeframe, and were continuously enrolled for one calendar year after the first DM-related claim. We matched DM patients with CD patients by age (in years), gender, region, and year of the review period in a 2:1 ratio. CD patients without two DM matches were excluded from the final cohort.
The primary outcome measures were healthcare utilization and costs, based on all claims occurring in the 1-year review period for each eligible patient. Healthcare utilization included the total number of hospitalizations, emergency department (ED) visits, and physician office visits, as well as the total number of prescription fills, standardized to 30 days of supply. Healthcare cost outcomes included total annual costs as well as pharmacy (derived from outpatient pharmacy claims) and non-pharmacy costs (derived from medical claims). All costs were adjusted to 2012 US dollars using the medical care components of the Consumer Price Index [10].
Additionally, we reported the following patient characteristics: demographics (age, gender, geographic region), Charlson comorbidity index [11, 12], number of chronic conditions [13], and CD-related complications, including infections, DM, osteoporosis, vertebral compression fractures, depression/anxiety, kidney stones, and cardiovascular disease/stroke (“Appendix”) [3, 6].
Descriptive statistics, including means, medians, standard deviations, and percentages, were reported for all study measures, and stratified by comparison group. We conducted pairwise comparisons between CD and non-CD (control) patients and between CD and DM patients. To compare the differences between cohorts, Chi square tests and t-tests were performed for categorical and continuous variables, respectively. All data transformations and statistical analyses were conducted using SAS® version 9.4 (SAS Institute, Cary, NC).
Results
Baseline characteristics
The 1852 patients with CD in the study were 42.9 years old on average, with nearly half of the group 45 years of age or older. 78.2 % were female and 38 % lived in the southern US (Table 1). Patients with CD, compared to population-based controls, had a higher number of chronic conditions (3.9 vs. 1.6, p < .001) and a higher Charlson Comorbidity Index (1.3 vs. .4, p < .001). Patients with CD, compared to DM patients, had a higher number of chronic conditions (3.9 vs. 2.9, p < .001); however, patients with CD had a lower Charlson Comorbidity Index (1.3 vs 1.7, p < .001). Individuals with CD had significantly higher rates of multiple comorbidities, including infections, osteoporosis, depression/anxiety, kidney stones, and cardiovascular disease, compared to the control or DM cohorts (Table 2).
Healthcare resource utilization
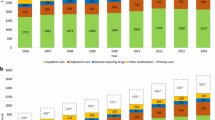
Patients with CD had higher rates of healthcare resource utilization compared to their matched counterparts (Table 3). Patients with CD were hospitalized more frequently (19.3 % with at least one hospitalization) compared to patients with DM (11.0 %, p < .001) or controls (5.6 %, p < .001). Patients with CD also visited the ED more frequently (25.4 % with at least one visit) compared to patients with DM (21.1 %, p < .001) or controls (14.3 %, p < .001). In addition, those with CD had a mean 19.1 office visits per year, more than patients with DM (10.7, p < .001) or controls (7.1, p < .001). Finally, patients with CD filled a mean of 51.7 prescriptions, more than patients with DM (42.7, p < .001) or controls (20.5, p < .001).
Healthcare costs
Patients with CD accrued significantly higher costs compared to patients with DM and controls (Table 4). Mean total healthcare costs for patients with CD ($26,269) were more than double those for patients with DM ($12,282, p < .001) and more than quadruple those for controls ($5869, p < .001). This disparity in costs was primarily due to non-pharmacy-related care. Non-pharmacy-related costs for CD patients ($21,704) were more than double analogous costs for patients with DM ($9263, p < .001) and quadruple those for controls ($4872, p < .001). To a lesser extent, pharmacy-related costs for CD patients ($4565) also exceeded those for patients with DM ($3019, p < .001) and controls ($997, p < .001).
Discussion
US patients with CD had significantly higher healthcare resource utilization rates compared to patients with DM or population-based controls. Our findings are consistent with the prior analysis by Swearingen et al., which identified higher volumes of inpatient, outpatient, and ED visits among patients with CD compared to controls or those with non-functional pituitary adenomas [6]. We also found that patients with CD accrue far higher costs than patients with DM or controls. This is again consistent with prior literature demonstrating that patients with CD have significantly higher costs of care than population-based controls or patients with nonfunctioning pituitary tumors [6].
A prior study of commercially insured patients with CD had calculated a mean $34,992 in total healthcare costs, $3597 of which were related to outpatient drug claims; the study also estimated direct CD-related costs at $14,310 [5]. However, that study did not distinguish between pharmacy and non-pharmacy claims. In our study, pharmacy-related costs comprised only 17 % of the total healthcare costs of patients with CD. Consequently, we were able to determine that the differences in costs among cohorts were primarily due to large differences in non-pharmacy related care ($12,441 between CD and DM patients; $16,832 between CD and control patients).
Our study calculated the mean total healthcare cost of patients with CD at $26,269, over $8700 less than a previously published estimate [5]. We attribute this difference to slightly different definitions of CD. The current study uses a more expansive definition that includes many additional procedure- and condition-based codes, as opposed to the specific hypophysectomy-based definition used by Broder et al. [5]. The older study definition would tend to capture patients who had recently undergone surgery, and others have demonstrated that immediate postsurgical costs of patients with CD often increase substantially, especially if the disease later does not go into remission [6]. Our broader definition of CD likely encompassed a wider range of patients, including those undergoing surgery either recently or remotely.
Additionally, we discovered that in this cohort of commercially insured patients, the annual cost of CD patient care was more than double that of DM patient care, a novel finding. DM is a well-characterized disease with major microvascular and macrovascular complications, and consequently high costs associated with care. The total cost of diagnosed DM in the US, including direct medical costs and reduced productivity, was an estimated $245 billion in 2012 [14]. That study also calculated annual per-person medical costs of about $13,700, which was similar to the $12,282 calculated in our analysis. Thus, our head-to-head comparison of two important endocrine disorders highlights the substantial burden of illness that patients with CD face.
Higher cost in patients with CD may be due to multiple causes. First, patients with CD on average had more chronic conditions than patients with DM. Comorbidities requiring treatment are a well-known contributor to overall increases in resource utilization and cost, as has been shown in other populations [15–17]. We noted that particularly serious comorbidities such as cardiovascular disease and stroke, when reviewed together, were significantly more common in the CD cohort compared to the DM cohort (11 vs. 8.2 %, p < .001). Given that microvascular and macrovascular conditions in diabetic patients are the largest contributors to the direct and indirect costs of DM [18], further research in additional studies and populations to investigate the possible impact of this set of conditions, particularly macrovascular conditions, in excess cost for CD over DM may also be very relevant. With respect to resource utilization, the severity of CD-related comorbidities may influence whether patients decide to visit their physician in the office or the ED; this also may influence cost and may be a future study topic.
Nearly all patients with CD undergo surgery, since transsphenoidal surgery (TSS) is considered first-line therapy in this population [19], while only 25 % of diabetic patients will require surgery [20]. Surgery may result in various burdens and cost in both CD and DM populations. Swearingen et al. demonstrated that patients with CD who had unsuccessful surgery had a substantial increase in cost in the year following surgery that could have been the result of adjunctive treatment, including a second TSS, adrenalectomy, radiotherapy, and pharmacotherapy [6]. Up to 35 % of patients undergoing TSS experience surgical failure or recurrence, and the one-time procedure cost of repeat TSS ($33,700) alone exceeds the $26,000 mean annual cost of care for patients with CD in our study [21]. Patil et al. demonstrated that greater numbers of complications during TSS increased length of hospitalization and total hospital charges for patients with CD [8]. Similarly, surgery in diabetic patients has been recently shown to be associated with increased hospital stay, complications, and 30-day mortality in surgical patients, which also may increase costs [22]. Where CD patients have much greater rates of surgery, particularly with the use of TSS as first-line therapy, than DM patients, this may also help to explain some of the excess per-patient costs observed in the present study for CD over DM.
Next, inadequate treatment of CD may contribute to prolonged effects of symptoms, increasing expenditures for medical care. CD is associated with a vast number of symptoms affecting multiple organ systems, including endocrine, integumentary, neurologic, reproductive, musculoskeletal, cardiovascular, and renal. In some instances, the effects of exposure to cortisol, such as hypertension and impaired cognition, are not easily reversible and require prolonged symptomatic treatment [3]. Treatment of CD may be further delayed by difficulty with diagnosis, as the symptoms associated with CD vary across patients and may even be cyclic [3, 23, 24].
Finally, CD may relapse and remain undiagnosed. Relapse of CD may reach 20–25 % at 10 years after surgical treatment of the primary pituitary tumor [25]. Delayed diagnosis of disease relapse not only means greater exposure to the sequelae of CD, but also the need for re-intervention, including repeat surgery, radiotherapy, and/or pharmacotherapy. Additional interventions to treat relapsed CD will increase costs of care. Swearingen et al. [6] demonstrated that patients with CD that failed to go into remission postoperatively have significantly higher overall costs after surgery compared to before surgery. Other authors have also discussed the issue of increased costs from managing the side effects of CD-related therapy [26].
In our study, patients with CD were diagnosed with more chronic conditions on average than patients with DM or matched controls, consistent with prior literature [6]. Patients with CD did have a lower Charlson comorbidity index in comparison to their matched counterparts. However, this unusual finding may be attributable to the definition of the Charlson index, which includes two DM-related categories and nothing related to CD. Consequently, patients with DM will always have a score of at least 1–2; patients with CD may have a score of 0 if they had no comorbid conditions.
Limitations of this study include the lack of ICD-9-CM codes specific to CD, which may result in cases being misidentified or missed. We used a previously published algorithm to minimize the risk of misidentification [9]. MarketScan is a retrospective healthcare claims database that is not specifically designed for research and lacks clinical information. Healthcare medication claims identified in our study represent medications purchased by patients and not necessarily those actually consumed; however, this was not a major concern since we were interested in costs and not drug adherence. Finally, this study only included patients with commercial insurance coverage, and so the results may not necessarily represent the general CD population.
Conclusions
US patients with CD had significantly higher annual rates of healthcare resource utilization compared to matched DM patients and population controls without CD. In addition, the costs of CD patient care were double that for DM patient care and quadruple that for controls. This current study puts into context the additional healthcare and economic burdens of CD over DM, a common, chronic endocrine condition affecting multiple organ systems, and US population controls.
References
Colao A, Boscaro M, Ferone D, Casanueva FF (2014) Managing Cushing’s disease: the state of the art. Endocrine 47(1):9–20
Broder MS, Neary MP, Chang E, Cherepanov D, Ludlam WH (2014) Incidence of Cushing’s syndrome and Cushing’s disease in commercially-insured patients <65 years old in the United States. Pituitary [Epub ahead of print]
Newell-Price J, Bertagna X, Grossman AB, Nieman LK (2006) Cushing’s syndrome. Lancet 367:1605–1617
Dekkers OM, Biermasz NR, Pereira AM, Roelfsema F, van Aken MO, Voormolen JH, Romijn JA (2007) Mortality in patients treated for Cushing’s disease is increased, compared with patients treated for nonfunctioning pituitary macroadenoma. J Clin Endocrinol Metab 92:976–981
Broder MS, Neary MP, Chang E, Ludlam WH, Cherepanov D (2013) Annual economic burden associated with Cushing’s disease in the United States. Presented at: ENDO 2013, 17 June 2013, San Francisco, CA
Swearingen B, Wu N, Chen SY, Pulgar S, Biller BM (2011) Health care resource use and costs among patients with Cushing disease. Endocr Pract 17:681–690
Burton T, Le Nestour E, Neary M, Ludlam WH (2014) Economic burden of Cushing’s disease in a large US managed care health care plan. Presented at: ENDO 2014, 21–24 June 2014, Chicago, IL
Patil CG, Lad SP, Harsh GR, Laws ER Jr, Boakye M (2007) National trends, complications, and outcomes following transsphenoidal surgery for Cushing’s disease from 1993 to 2002. Neurosurg Focus 23(3):E7
Burton TM, Rey GG, Neary MP, Ludlam WH, Le Nestour E (2013) Development of an algorithm to identify Cushing disease patients in a US administrative claims database. Presented at: 13th International Pituitary Congress, 12–14 June 2013, San Francisco, CA
Bureau of Labor Statistics. Consumer Price Index: Measuring Price Change for Medical Care in the CPI. http://www.bls.gov/cpi/cpifact4.htm. Last updated 12 April 2010. Last Accessed 29 April 2014
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Deyo RA, Cherkin DC, Ciol MA (1992) Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol 45:613–619
Hwang W, Weller W, Ireys H, Anderson G (2001) Out-of-pocket medical spending for care of chronic conditions. Health Aff 20:267–278
American Diabetes Association (2013) Economic costs of diabetes in the US in 2012. Diabetes Care 36:1033–1046
Brilleman SL, Purdy S, Salisbury C, Windmeijer F, Gravelle H, Hollinghurst S (2013) Implications of comorbidity for primary care costs in the UK: a retrospective observational study. Br J Gen Pract 63:e274–e282
Meyers JL, Parasuraman S, Bell KF, Graham JP, Candrilli SD (2014) The high-cost, type 2 diabetes mellitus patient: an analysis of managed care administrative data. Arch Public Health 72:6
O’Shea M, Teeling M, Bennett K (2013) The prevalence and ingredient cost of chronic comorbidity in the Irish elderly population with medication treated type 2 diabetes: a retrospective cross-sectional study using a national pharmacy claims database. BMC Health Serv Res 13:23
American Diabetes Association (2014) Standards of medical care in diabetes–2014. Diabetes Care 37(Suppl. 1):S14–S80
Buchfelder M, Schlaffer S (2010) Pituitary surgery for Cushing’s disease. Neuroendocrinology 92(Suppl 1):102–106
Loh-Trivedi M (2014) Perioperative management of the diabetic patient. Medscape from WebMD. http://emedicine.medscape.com/article/284451-overview. Last updated June 10, 2013. Accessed 16 Sept 2014
Patel DA, Maldonado M, Stephens JM, Pulgar S, Swearingen B (2011) Cost of second line non-pharmacologic interventions and their related complications in Cushing’s disease: A literature-based economic analysis. Presented at: 12th International Pituitary Congress, June 1–3, 2011, Boston, MA
Frisch A, Chandra P, Smiley D, Peng L, Rizzo M, Gatcliffe C, Hudson M, Mendoza J, Johnson R, Lin E, Umpierrez GE (2010) Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care 33:1783–1788
Aron DC (2010) Cushing’s syndrome: why is diagnosis so difficult? Rev Endocr Metab Disord 11:105–116
Bertagna X, Guignat L, Groussin L, Bertherat J (2009) Cushing’s disease. Best Pract Res Clin Endocrinol Metab 23:607–623
Tritos NA, Biller BM, Swearingen B (2011) Management of Cushing disease. Nat Rev Endocrinol 7:279–289
Feelders RA, Pulgar SJ, Kempel A, Pereira AM (2012) The burden of Cushing’s disease: clinical and health-related quality of life aspects. Eur J Endocrinol 167:311–326
Acknowledgments
The authors thank Gordon H. Sun, M.D., and Dasha Cherepanov, Ph.D., for assisting with the manuscript. This study was funded by Novartis Pharmaceuticals Corporation. Financial relationships with the organization that sponsored the research are as follows: Maureen P. Neary and William H. Ludlam are employees of Novartis Pharmaceuticals Corporation; Michael S. Broder and Eunice Chang are employees of Partnership for Health Analytic Research, LLC (PHAR), a health services research company that received funding for this research from Novartis. This study was presented at AMCP Nexus, Boston, MA, October 8–9, 2014.
Author information
Authors and Affiliations
Corresponding author
Appendix
Rights and permissions
About this article
Cite this article
Broder, M.S., Neary, M.P., Chang, E. et al. Incremental healthcare resource utilization and costs in US patients with Cushing’s disease compared with diabetes mellitus and population controls. Pituitary 18, 796–802 (2015). https://doi.org/10.1007/s11102-015-0654-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-015-0654-5