Abstract
Background
Portal vein thrombosis (PVT) is a common complication for patients with end-stage liver disease. The presence of PVT used to be a contraindication to living donor liver transplantation (LDLT). The aim of this study is to evaluate the influence of preoperative PVT on perioperative and long-term outcomes of the recipients after LDLT.
Methods
We reviewed the data of patients who underwent LDLT during the period between 2004 till 2017.
Results
During the study period, 500 cases underwent LDLT. Patients were divided into three groups. Group I included non-PVT, 446 patients (89.2%); group II included attenuated PV, 26 patients (5.2%); and group III included PVT, 28 patients (5.6%). Higher incidence of hematemesis and encephalopathy was detected in PVT (p = 0.001). Longer anhepatic phase was found in PVT (p = 0.013). There were no significant differences between regarding operation time, blood loss, transfusion requirements, ICU, and hospital stay. The 1-, 3-, and 5-year overall survival (OS) rates of non-PVT were 80.5%, 77.7%, and 75%, and for attenuated PV were 84.6%, 79.6%, and 73.5%, and for PVT were 88.3%, 64.4%, and 64.4%, respectively. There was no significant difference between the groups regarding OS rates (logrank 0.793).
Conclusion
Preoperative PVT increases the complexity of LDLT operation, but it does not reduce the OS rates of such patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Portal vein thrombosis (PVT) is a common complication for patients with end-stage liver disease (ESLD). The incidence of PVT in those patients varies from 0.6 to 26%, which increases with the severity of the liver disease.1,2 In patients with advanced stage of cirrhosis and those undergoing liver transplantation, the incidence varies from 5 to 16% in previous reports. 2, 3
The presence of PVT used to be a contraindication to living donor liver transplantation (LDLT).4,5 This is related to the technical difficulties of PV reconstruction, prolonged warm ischemia time, and operative blood loss. Also, the increased risk for postoperative PV anastomotic stenosis may cause relapse of PVT, affecting seriously the function of the liver graft and the recipient survival.6
The advancements of the surgical techniques and improvements of the surgical skills allowed safe LDLT for patients with PVT. Many centers, especially from Asia, no longer consider the presence of preoperative partial PVT as an absolute contraindication for LDLT.7,8,9 On the other hand, high grades PVT are still considered a relative contraindication for LDLT, especially in areas lacking bovine and cryopreserved vessel graft like Egypt.
Previous reports about LDLT for patients with PVT are quite heterogenous. Many reports have showed that the outcomes of patients with and without PVT are similar.5,10,11 Other reports have showed higher incidence of postoperative complications and dismal outcomes in patients with PVT.12,13,14
The aim of this study is to review our center experience of LDLT and analyze the influence of preoperative PVT on perioperative and long-term outcomes of the recipients.
Materials and Methods
Study Design
We reviewed the data of patients who underwent LDLT at Liver Transplantation Unit, Gastrointestinal Surgery Center, Mansoura University, Egypt during the period between May 2004 and March 2017.
Patient data were reviewed from a prospectively maintained database for all patients undergoing LDLT. A written informed consent for the surgical procedure was obtained from each patient. This study was approved by institutional review board and local ethical committee at the Faculty of Medicine, Mansoura University.
Preoperative Assessment
Preoperative evaluation protocol had been described previously.15 In summary, preoperative evaluation of potential recipients included four phases:
-
Phase I included blood group, basic laboratory evaluation including tumor markers, virological evaluation, radiological evaluation including triphasic computed tomography of the abdomen and portography (Figs. 1 and 2), and bone scan in case of suspected hepatocellular carcinoma (HCC), and anesthetic consultation.
-
Phase II included detailed cardiological and neurological evaluation. Also, autoimmune markers (ANA, ASMA, LKMA, AMA), and magnetic resonance cholangio-pancreatography if suspected sclerosing cholangitis.
-
Phase III included endoscopic evaluation including upper and lower gastrointestinal tract endoscopy.
-
Phase IV included routine consultations to excluded possible septic foci.
Operative Techniques
The operative technique had been described before.15 After recipient hepatectomy, eversion thrombectomy was attempted in patients with PVT. The PV was dissected as low as possible down to the retro-pancreatic part. A vascular clamp was placed to control the PV inflow. The edges of the PV were everted and the PV thrombus was held by a clamp and dissected from the PV wall in a circular manner. A blunt end clamp was used in dissection of the PV thrombus (Fig. 3). If the surgeon can reach below the PV thrombus, a vascular clamp was placed as far as possible on the dissected PV. If the PV is totally thrombosed or the thrombus is extending the superior mesenteric vein, no significant bleeding from the PV was noticed and the surgeon hand was used to control the SMV below the level of the thrombus.
Successful completion of PV thrombectomy was confirmed by adequate blood flushing from the PV. If the PV wall is attenuated or narrowed, a rectangular interposition patch graft was placed to the divided anterior wall of the PV (Fig. 4). The patch graft was obtained from recipient PV bifurcation, recanalized umbilical vein, or dissected middle or right hepatic veins from the liver explant.
The PV was reconstructed in end to end fashion to the graft right hepatic vein. Afterwards the PV flow was evaluated by Doppler ultrasound (US). If the PV flow was weak due to preexisting large porto-systemic collaterals, those collaterals were dissected and ligated to improve the PV flow.16
Postoperative Care
-
Intensive care unit (ICU) care
After surgery, all cases were transferred to the ICU for monitoring. Attempt to extubation was done based on hemodynamic stability, arterial blood gases, and the status of abdominal drains. Patients underwent detailed laboratory evaluation twice daily during the ICU stay. Oral intake and ambulation were allowed on the third postoperative day. Patients were transferred to the ward on the fifth postoperative day, depending upon clinical improvement.
-
Radiological Evaluation
Our postoperative protocol included Doppler ultrasound examinations once daily during the first week, day after other during the second and third weeks and before hospital discharge then once weekly during the following 2 months.
-
Follow-up
After discharge, patients were followed up regularly in outpatient visits. Patients were followed once every week in the first month, then every 2 weeks in the second and third months, then every month till the end of the first year, then every 3 months afterwards or on patient’s demand.
Follow-up visit included detailed history taking, clinical examination, detailed laboratory evaluation including trough level of immunosuppression drugs, and Doppler US evaluation of hepatic vasculature.
Definitions
PVT was classified according to the Yerdel grading system into four grades. Grade 1: the PV is minimally or partially thrombosed, <50% of the vessel lumen; Grade 2: more than 50% occlusion of the PV including total occlusion; Grade 3: complete thrombosis of both PV and proximal superior mesenteric vein (SMV); and Grade 4: complete thrombosis of the PV as well as proximal or distal SMV.17
Postoperative morbidities are defined as adverse events occurring during the postoperative course and graded according to Clavien-Dindo grades.18 Early mortality is defined as patient death during the first 90 days after transplantation. Overall survival (OS) is calculated from the date of surgery to the date of documented mortality or the last follow-up visit.
Statistical Analysis
Categorical variables were expressed as number (percentage), and continuous variables were expressed as median (range). Comparison between the three groups was done by chi-square or ANOVA test when appropriate. Comparison between each two groups was done by chi-square or Mann-Whitney test when appropriate. Survival rates were calculated by Kaplan-Meier method, and comparison between groups was done by Logrank test.
Statistical analysis was performed using the SPSS 20 software (IBM, Chicago, IL, USA). A p value less than 0.05 was considered statistically significant.
Results
During the study period, 500 cases underwent LDLT at Liver Transplantation Unit, Gastrointestinal Surgery Center, Mansoura University, Egypt. All of transplanted cases during the study period were included in our study.
Preoperative PVT was detected in 28 patients (5.6%). According to the Yerdel grading system, grade I PVT was detected in 24 patients (4.8%), while grade II PVT was detected in 3 patients (0.6%), and grade III PVT was detected in 1 patient (0.2%).
Patients were divided into three groups. Group I included patients without PVT, 446 patients (89.2%). Group II included patients with attenuated PV (PV diameter less than 8 mm), 26 patients (5.2%). Group III included patients with PVT, 28 patients (5.6%).
Demographic Data
Patients’ demographics are shown in Table 1. There were no significant differences between the study groups regarding preoperative demographics apart from preoperative presentation. Higher incidence of hematemesis and encephalopathy was detected in PVT group (p = 0.001).
Operative Data
Operative data are shown in Table 2. Longer anhepatic phase duration was found in PVT group (p = 0.013). There were no significant differences between the groups regarding overall operation time, blood loss, and transfusion requirements.
Postoperative Data
Postoperative data are shown in Table 2. There were no significant differences between the groups regarding ICU and hospital stay. There was no significant difference between the groups regarding postoperative biliary complications. Higher incidence of abdominal collections was found in attenuated PV group. Higher incidence of postoperative vascular complications was found in PVT group.
Survival Outcomes
The median OS for all study patients was 33 months (4–169). The median OS for Non-PVT group was 33.5 (4-169), for attenuated PV group was 31.5 months (4-87), and for PVT group was 22 months (4-79).
The 1-, 3-, and 5-year OS rates of non-PVT group were 80.5%, 77.7%, and 75% respectively. The 1-, 3-, and 5-year OS rates of attenuated PV group were 84.6%, 79.6%, and 73.5% respectively. The 1-, 3-, and 5-year OS rates of PVT group were 88.3%, 64.4%, and 64.4%, respectively (Fig. 5).
There was no significant difference between the groups regarding OS rates (Logrank, 0.793).
The 1-, 3-, and 5-year OS rates of Grade I PVT patients were 86.1%, 64.6%, and 64.4% respectively. The 1-, 3-, and 5-year OS rates of Grade II PVT patients were 100%, 66.7%, and 0% respectively. The 1-, 3-, and 5-year OS rates of Grade III PVT patients were 100%, 0%, and 0%, respectively (Fig. 5).
There was no significant difference between the different PVT grades regarding OS rates (Logrank, 0.256).
Discussion
PVT is a common complication in patients with ESLD. This is attributed to high hepatic vascular resistance, or previous history of splenectomy.19 Previous studies had shown that the incidence of PVT in ESLD patients varies from 0.6 to 26%, which is seven times higher than in general population. The incidence is directly related to patient age, and the degree of liver disease.1,2,20,21 In our study, the overall incidence of patients with preoperative PVT in patients undergoing LDLT was 5.6% (28 patients). The main indication of LDLT was HCV-related liver cirrhosis. Higher incidence of HCV-related cirrhosis had been found in PVT patients (60.4%) in comparison to non-PVT patients (54.2%), but this was not statistically significant.
Clinical presentation of patients with PVT is greatly heterogenous. It varies from accidental diagnosis during preliminary work-up, severe complications as variceal bleeding, intestinal ischemia, and hepatic encephalopathy.22 In our study, a significant higher incidence of hematemesis and melena was found in patients with attenuated PV and PVT groups requiring repeated endoscopic ablation. Also, higher incidence of hepatic encephalopathy was found in those groups.
Preoperative PVT is a technically challenging situation during liver transplantation. Previous studies had shown that preoperative PVT, and its severity, is a main determinant of the complexity of the transplantation operation, and its outcomes.17,20
Several techniques had been described for the maintenance of portal inflow after liver transplantation including eversion thrombectomy, interposition graft to the superior mesenteric vein or large collateral vessel, reno-portal anastomosis, and cavoportal hemi-transposition.23 The choice of appropriate method of reconstruction is depending on the extent of portal vein thrombosis and the availability of vascular grafts. We should stress on the importance of high quality multi-detector computed tomography with portography for evaluating the extent of thrombosis and presence of collaterals.
In our study, we utilized eversion thrombectomy for extraction of portal vein thrombus. It was successful in all of our patients and reconstruction of portal vein in end to end fashion between graft and donor portal veins. If the portal vein was markedly attenuated or teared from thrombectomy, a rectangular interposition graft was sutured to the anterior wall of the portal vein. In some cases, ligation of the porto-systemic collaterals was needed in some cases to improve the portal inflow. In Egypt, the lack of cryopreserved vascular grafts is a limiting factor for the use of interposition graft bypass for portal inflow reconstruction.
Several studies had found that preoperative PVT is a poor prognostic factor after liver transplantation. This is attributed to increased operation time, increased intraoperative blood loss and transfusion requirements, longer ICU and overall hospital stay, and higher incidence of postoperative complications.24,25,26 In our study, we found a significantly longer anhepatic phase duration in patients with preoperative PVT. Also, there were no significant differences between patients with and without preoperative PVT regarding the operation time, intraoperative blood loss, transfusion requirements, ICU, and hospital stay.
Doppler US is an essential tool to monitor such patients after liver transplantation for early detection of postoperative vascular complications. Our postoperative protocol involved routine Doppler US once daily during the first week, day after other during the second and third weeks.
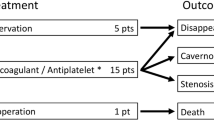
Postoperative PVT is one of the most severe complications for the patients. Previous studies had found that both early and late onset postoperative PVT rates are higher in the patients with preoperative PVT.6,8,10 In our study, there was a significant higher incidence of vascular complications in patients with preoperative PVT. Similarly, there was a significant higher incidence of postoperative PVT in PVT group. There was no significant difference between the groups regrading postoperative PVS.
Some authors recommended routine use of preventive therapies in patients with preoperative PVT to prevent recurrence of PVT after liver transplantation. Song et al. reported the routine use of aspirin during the early postoperative period .10 Gao et al. recommended the routine administration of low molecular heparin in the first postoperative week, and aspirin for at least 3 months after liver transplantation.6 Mori et al. advised tailored use of anticoagulation therapy for patients with good coagulation profile or slow portal flow.8 In our experience, we routinely administer prophylactic anticoagulation therapy to our patients including low molecular weight heparin for the first 2 weeks followed by acetylsalicylic acid for 3–6 month.
Previous studies showed that the long-term outcome after LDLT for patients with preoperative PVT, is comparable with that of patients without PVT.27,28,29 Song et al. found that 5 year OS rate was 67.2% in patients with preoperative PVT, which was inferior to patients without preoperative PVT.10 Mori et al. found that post-transplant OS rates of patients with preoperative PVT at 1 year and 5 years were comparable to patients without preoperative PVT (1 year, 81% vs. 77%, and 5 years, 81% vs. 73%).8 In our study, there was no significant difference between patients without and with preoperative PVT regarding 5 year OS survival rates (75 vs. 64.4%, respectively).
In conclusion, in this study, we reviewed our center study in LDLT for patients with preoperative portal vein troubles. We found that preoperative PVT increases the complexity of LDLT operation and the operative trauma to the patient, but it does not reduce the OS rates of such patients. Preoperative PVT is not an absolute contraindication for LDLT. Eversion thrombectomy is successful in patients with low-grade preoperative PVT, but extensive forms of preoperative PVT require more complex reconstruction of portal inflow.
References
Tsochatzis EA, Senzolo M, Germani G, et al. Systematic review: portal vein thrombosis in cirrhosis. Aliment Pharmacol Ther 2010;31:366–74.
Nonami T, Yokoyama I, Iwatsuki S, et al. The incidence of portal vein thrombosis at liver transplantation. Hepatology 1992;16:1195–8.
Harding DJ, Perera MT, Chen F, et al. Portal vein thrombosis in cirrhosis: controversies and latest developments. World J Gastroenterol 2015;21:6769–84.
Seijo S, García-Criado A, Darnell A, et al. Diagnosis and treatment of portal thrombosis in liver cirrhosis. Gastroenterol Hepatol 2012;35(9):660–6.
Charco R, Fuster J, Fondevila C, et al. Portal vein thrombosis in liver transplantation. Transplant Proc 2005;37(9):3904–5.
Gao PJ, Gao J, Li Z, et al. Liver transplantation in adults with portal vein thrombosis: Data from the China Liver Transplant Registry. Clin Res Hepatol Gastroenterol 2016;40(3):327–32.
Kim SJ, Kim DG, Park JH, et al. Clinical analysis of living donor liver transplantation in patients with portal vein thrombosis. Clin Transplant 2011;25:111–8.
Mori A, Iida T, Iwasaki J, et al. Portal vein reconstruction in adult living donor liver transplantation for patients with portal vein thrombosis in single center experience. J Hepatobiliary Pancreat Sci 2015;22:467–74.
Sato K, Sekiguchi S, Watanabe T, et al.. The use of recipient superficial femoral vein as a venous graft for portal vein reconstruction in right lobe living donor liver transplantation. Transplant Proc 2009;41:195–7.
Song S, Kwon CHD, Kim JM, et al. Single-center experience of living donor liver transplantation in patients with portal vein thrombosis. Clin Transplant 2016;30: 1146–51.
Levi Sandri GB, Lai Q, Berloco PB, et al. Portal vein thrombosis before liver transplant does not alter postoperative patient or graft survival. Exp Clin Transplant 2014;12(3):238–40.
Lladó L, Fabregat J, Castellote J, et al. Management of portal vein thrombosis in liver transplantation: influence on morbidity and mortality. Clin Transplant 2007;21(6):716–21.
Wu G, Liu YF, Liu SR, et al. Liver transplantation in end-stage liver disease with portal vein thrombosis. Zhonghua Wai Ke Za Zhi 2009;47(8):590–3.
Arcadipane A, Nadalin S, Gruttadauria S, et al. The recipient with portal thrombosis and/or previous surgery. Transplant Proc 2008;40(4):1183–6.
Wahab MA, Shehta A, Elshoubary M, et al. Living-Donor Liver Transplantation in Hepatitis C Virus Era: A Report of 500 Consecutive Cases in a Single Center. Transplant Proc 2018;50(5):1396–1406.
Elshobary M, Shehta A, Salah T, et al. Ligation of huge spontaneous porto-systemic collaterals to avoid portal inflow steal in adult living donor liver transplantation: A case-report. Int J Surg Case Rep 2017;31:214–7.
Yerdel MA, Gunson B, Mirza D, et al. Portal vein thrombosis in adults undergoing liver transplantation: Risk factors, screening, management, and outcome. Transplantation 2000;69:1873–81.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240(2):205.
Werner KT, Sando S, Carey EJ, et al. Portal vein thrombosis in patients with end stage liver disease awaiting liver transplantation: outcome of anticoagulation. Dig Dis Sci 2013;58(6):1776–80.
Robles R, Fernandez JA, Hernández Q, et al. Eversion thrombo-endovenectomy in organized portal vein thrombosis duringliver transplantation. Clin Transplant 2004;18(1):79–84.
Lendoire J, Raffin G, Cejas N, et al. Liver transplantation in adult patients with Portal vein thrombosis: risk factors, man-agement and outcome. HPB (Oxford) 2007;9(5):352–6.
von Köckritz L, De Gottardi A, Trebicka J, et al. Portal vein thrombosis in patients with cirrhosis. Gastroenterol Rep 2017;5(2):148–56.
Kuramitsu K, Fukumoto T, Kinoshita H, et al. Analysis of Portal Vein Reconstruction Technique with High-Grade Portal Vein Thrombus in Living Donor Liver Transplantation. Ann Transplant 2016;21:380–5.
Pan C, Shi Y, Zhang JJ, et al. Single-center experience of 253 portal vein thrombosis patients undergoing liver transplantation in China. Transplant Proc 2009;41:3761–5.
Doenecke A, Tsui TY, Zuelke C, et al. Pre-existent portal vein thrombosis in liver transplantation: influence of pre-operative disease severity. Clin Transplant 2010;24:48–55.
Montenovo M, Rahnemai-Azar A, Reyes J, et al. Clinical impact and risk factors of portal vein thrombosis for patients on wait list for liver transplant. Exp Clin Transplant 2018;16(2):166–71.
Saidi RF, Jabbour N, Li Y, et al. Outcomes of patients with portal vein thrombosis undergoing live donor liver transplantation. Int J Organ Transplant Med 2014;5(2):43–9.
Egawa H, Tanaka K, Kasahara M. Single center experience of 39 patients with preoperative portal vein thrombosis among 404 adult living donor liver transplantations. Liver Transpl 2006;12:1512–8.
Kumar N, Atkison P, Fortier M. Cavoportal Transposition for Portal Vein Thrombosis in a Pediatric Living-Related Liver Transplantation. Liver Transpl 2003;9:874–6.
Author information
Authors and Affiliations
Contributions
Conception and design of the work: Wahab MA, Shehta A.
Acquisition, analysis, or interpretation of data for the work: All authors.
Drafting the work or revising it critically for important intellectual content: All authors.
Final approval of the version to be published: All authors.
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: All authors.
Corresponding author
Ethics declarations
A written informed consent for the surgical procedure was obtained from each patient. This study was approved by institutional review board and local ethical committee at the Faculty of Medicine, Mansoura University.
Rights and permissions
About this article
Cite this article
Wahab, M.A., Shehta, A., Elshoubary, M. et al. Outcomes of Living Donor Liver Transplantation for Patients with Preoperative Portal Vein Problems. J Gastrointest Surg 22, 2055–2063 (2018). https://doi.org/10.1007/s11605-018-3876-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3876-9