Abstract
Background
The thrombosis of the main and intrahepatic branches of the portal vein (TMIP) is potentially lethal and deemed a common complication following laparoscopic splenectomy and azygoportal disconnection (LSD) in patients with cirrhosis and portal hypertension (PH). The predictors of TMIP after LSD remain unclear. The aim of this prospective study was to explore the predictive and risk factors for TMIP after LSD in cirrhotic patients with PH caused only by hepatitis B virus.
Methods
From September 2014 to March 2017, we enrolled 115 patients with hepatitis B cirrhosis and PH who successfully underwent LSD. Patients were subdivided into a TMIP group and a non-TMIP group. Univariate and multivariate logistic regression analysis was conducted on 24 items of demographic and preoperative data, to explore the risk factors of TMIP.
Results
Twenty-nine (25.22%) patients developed TMIP on postoperative day (POD) 7 and 26 (22.81%) patients developed TMIP on POD 30. From POD 7 to POD 30, 12 patients who did not have TMIP at POD 7 were newly diagnosed with TMIP, with portal vein diameter 15.05 ± 2.58 mm. Another 14 patients in whom TMIP had resolved had portal vein diameter 14.02 ± 1.76 mm. Univariate analysis and multivariate logistic regression revealed that portal vein diameter ≥ 13 mm [relative risk (RR) 5.533, 95% confidence interval (CI) 1.222–25.042; P = 0.026] and portal vein diameter ≥ 15 mm (RR 3.636, 95% CI 1.466–9.021; P = 0.005) were significant independent risk factors for TMIP on POD 7 and 30, respectively.
Conclusion
Portal vein diameter ≥ 13 mm and ≥ 15 mm were significant independent predictors for TMIP after LSD in patients with hepatitis B cirrhosis and PH on POD 7 and POD 30, respectively.
Trial registration
We registered our research at https://www.clinicaltrials.gov/. The name of research registered is “Warfarin Prevents Portal Vein Thrombosis in Patients After Laparoscopic Splenectomy and Azygoportal Disconnection.” The trial registration identifier at clinicaltrials.gov is NCT02247414.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Hepatitis B virus (HBV) is one of the main etiological factors in liver cirrhosis [1]. Although the etiology of cirrhosis is diverse, HBV infection is the leading risk for cirrhosis in Asia [2, 3]. In the stage of chronic cirrhosis, complications including approximately 30% of esophagogastric variceal bleeding and 30–50% of hypersplenism occur in patients owing to portal hypertension [4, 5].
In treating cirrhosis with hypersplenism and esophagogastric variceal bleeding, at present, liver transplantation is an effective method [6]. However, owing to the shortage of liver sources and high cost of transplantation, most patients do not have the option of receiving a liver transplant [7]. Additionally, despite the therapeutic effect of transjugular intrahepatic portosystemic shunt, patients are more likely to have restenosis or/and hepatic encephalopathy, with an incidence of more than 60% [8, 9].
In Asia, open splenectomy and azygoportal disconnection (OSD) has been widely used as an effective treatment [10, 11]. However, owing to hemodynamic changes and a sharp increase in platelets after surgery [12], patients are more prone to (portal vein system thrombosis) PVST, with incidence varying from 18.3 to 30.1% [13, 14]. In recent years, with remarkable progress in laparoscopic technology, laparoscopic splenectomy and azygoportal disconnection (LSD) has come to be considered a more ideal surgical treatment owing to its advantage of rapid recovery after surgery compared with OSD for patients with cirrhosis and esophagogastric varices and hypersplenism [15,16,17]. Even so, the occurrence of PVST remains troublesome and there are inevitable complications after LSD. In our previous study, PVST occurred in patients after LSD on postoperative day (POD) 7 at a proportion of 42.9% (24/56) [18]. Additionally, related research shows that the occurrence rate of PVST is significantly higher in patients who undergo LSD (50.0%, 40/80) than in those who receive OSD (30.1%, 22/71) [14].
PVST refers to thrombosis occurring in the main or intrahepatic portal vein branches, splenic vein, or superior mesenteric vein [19]. The formation of PVST contributes to a poor prognosis in patients with cirrhosis and is potentially life-threatening owing to a series of severe possible problems in patients with cirrhosis who have PVST, such as highly elevated portal venous pressure, progressive impairment of liver function [20], and development of ischemic intestinal necrosis [21].
Currently, the mechanism and risk factors of PVST in patients with cirrhosis remain poorly understood. Particularly in patients who undergo LSD, little is known regarding the occurrence of TMIP. In addition, there may be a significant correlation between the width of portal vein with TMIP. Moreover, they may be heterogeneous in the development of TMIP owing to liver cirrhosis between HBV and other etiologies; however, little research has specifically investigated this. Therefore, the aim of this study was to explore the predictors of TMIP after LSD in patients with cirrhosis and portal hypertension caused only by HBV, with the aim to develop preventative clinical treatment for patients with high risk of TMIP.
Materials and methods
Clinical data
In previous study, we sought to verify whether warfarin anticoagulation is effective in the prevention of PVST in patients with liver cirrhosis after LSD for portal hypertension. Between September 2014 and March 2017, a randomized controlled trial entitled “Warfarin Prevents Portal Vein Thrombosis in Patients After Laparoscopic Splenectomy and Azygoportal Disconnection” (Clinicaltrials.gov trial registration identifier NCT02247414) was carried out in our department. The present research was a subordinate branch of that previous study [22], with the aim to compare the curative effect of aspirin and warfarin for postoperative PVST.
On the basis of whether they met the inclusion criteria, patients were enrolled in this study. The predefined inclusion criteria were as follows: age 18–75 years; diagnosed with cirrhosis caused only by HBV clinically, radiologically, or histologically; Child–Pugh class A or B; splenomegaly with severe thrombocytopenia and/or leukopenia; and successful LSD without conversion to laparotomy. The exclusion criteria were patients with liver or any other malignancy; pulmonary embolism, deep venous thrombosis, and portal vein embolization confirmed by ultrasonography or computed tomography; uncontrolled hypertension; chronic renal failure; history of hemorrhagic stroke; hypercoagulable state not related to liver disease (e.g., malignancy, nephrotic syndrome, pregnancy); taking medication such as oral contraceptives, anticoagulants, and antiplatelet drugs; pregnancy; HIV infection; and refusal to participate in the study.
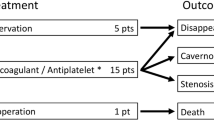
This study received the approval of the Ethics Committee of the Clinical Medical College of Yangzhou University. All patients provided written informed consent before surgery. Patients were randomized to receive treatment with oral administration of enteric-coated aspirin tablets (Bayer, Leverkusen, Germany) or warfarin sodium (Sine Pharmaceutical, Shanghai, China). In this study, from postoperative day (POD) 3, the warfarin group was given oral sodium warfarin until to postoperative 1 year. Patients were managed to adjust to reach a target international normalized ratio (INR) of 2–3, with an initial dose of 2.5 mg/day. If patients were found to have TMIP during the first year, the adjustment of the dose of warfarin was made to maintain the target INR of 2–3. Otherwise, the previous dose of warfarin remained unchanged regardless of whether or not the postoperative INR level increased step by step. The aspirin group were treated with 100 mg enteric-coated aspirin tablets (Bayer, Leverkusen, Germany) once daily for postoperative 1 year. Beginning on POD 3, both groups received low-molecular weight heparin (CS Bio, Hebei, China) subcutaneously (4.100 IU/day) for 5 days and 25 mg of oral dipyridamole (Henan Furen, Henan, China) three times daily for 3 months, as previously mentioned [22].
All patients’ preoperative data and clinical characteristics were prospectively collected, including age, sex, etiology of cirrhosis, hypertension, diabetes, Child–Pugh classification, body mass index, international normalized ratio (INR), anticoagulant therapy, serum albumin (ALB), d-dimer concentration, hemoglobin, blood urea nitrogen, white blood cell count, platelet count, total bilirubin, creatinine, splenic vein diameter, longitudinal diameter of the spleen, portal vein diameter, velocity of portal blood flow, and serum concentrations of liver fibrotic markers hyaluronidase (HA), laminin, procollagen type III (PC-III), and type IV collagen using a magnetic microbead chemiluminescence method, according to the manufacturer’s instructions (Snibe, Shenzhen, China). Additionally, all patients underwent ultrasound evaluation of TMIP on POD 7 and 30. Patients were divided into a TMIP group and a non-TMIP group, according to the absence or presence of postoperative TMIP.
Statistical analysis
The data are presented as mean (standard deviation) or median (interquartile range, IQR), where applicable, using an independent samples t test or the Mann–Whitney U test to compare two groups. Categorical data are presented as number (percentage), using the χ2 test for comparisons. Correlation analysis was used to identify significant cut-off values of candidate variables for predicting TMIP. Then, logistic multivariate regression with forward stepwise selection was used to analyze the influencing factors of TMIP by gradually eliminating non-significant variables. A value P < 0.05 was considered statistically significant. IBM SPSS 25.0 software (IBM Corp, Armonk, NY, USA) was used to analyze the collected data.
Results
A total of 210 patients with cirrhosis together with portal hypertensive bleeding and secondary hypersplenism were screened for study eligibility and 95 patients were excluded from the study. The trial profile is presented in Fig. 1.
Finally, 115 patients with cirrhosis and portal hypertension owing to HBV infection underwent LSD successfully (90 men and 25 women; mean age 51.15 ± 10.67 years, range 18–75 years). One patient died of esophagogastric variceal rebleeding within 1 month of surgery.
On POD 7, the proportion of PVST occurring in patients was 57.4% (66/115). Patients with TMIP accounted for 42.4% (28/66) of PVST cases, including 20 (30.3%) cases in the main portal vein, 2 (3.0%) in the intrahepatic branches of the portal vein (1 patient with the right branch and 1 patient with the left branch of the portal vein), and 6 (9.1%) cases in both the main and intrahepatic branches of the portal vein (4 patients with the main and right branch of the portal vein and 2 patients with main and left branch of the portal vein), which were verified using B-mode ultrasound examination. Demographic and preoperative clinical characteristics between the TMIP and non-TMIP groups on POD 7 are presented in Table 1. Significant differences were found in preoperative age, INR, d-dimer, ALB, portal vein diameter, and PC-III between the two groups (all P < 0.05).
Analysis of the relationship between portal vein diameter and TMIP on POD 7 was conducted using bivariate correlation analysis. With portal vein diameter ≥ 13 mm, the relationship presented the most significant levels according to the correlation coefficient (r = 0.227; P = 0.015), as shown in Table 2. Then, significant variables in univariate analysis were taken as the independent variable and events of TMIP on POD 7 as a dependent variable. Logistic multivariate regression revealed that portal vein diameter ≥ 13 mm was the only significant independent risk factor for TMIP on POD 7 [relative risk (RR) 5.328, 95% confidence interval (CI) 1.175–24.158; P = 0.030] (Table 3).
At follow-up on POD 30, 52 (45.6%) patients had developed PVST, among which 26 (50%) patients had TMIP. The outcomes were 17 (32.7%) cases, 2 (3.9%) cases, and 7 (13.5%) cases involving the main portal vein, intrahepatic branches of the portal vein (1 patient with the right branch and 1 patient with the left branch of the portal vein), and both the main and intrahepatic branches of the portal vein (5 patients with the main and right branch of the portal vein and 2 patients with main and left branch of the portal vein), respectively. The demographic data and preoperative clinical characteristics in the two groups are shown in Table 4. After POD 7 until to POD 30, 12 patients newly developed TMIP, which was confirmed on ultrasound examination; portal vein diameter was 15.05 ± 2.58 mm. From POD 7 to POD 30, TMIP was found to have resolved in 14 patients with portal vein diameter 14.02 ± 1.76 mm. And another 14 patients with persistent TMIP had a wider portal vein diameter that was 15.30 ± 2.05 mm. There was no significant difference of the portal vein diameter between two groups (P = 0.088).
Between the TMIP with non-TMIP groups, the portal vein diameter and HA showed significant differences (all P < 0.05; Table 4). According to bivariate correlation analysis, portal vein diameter ≥ 15 mm (r = 0.269; P = 0.004; Table 5) showed the optimal correlation coefficient associated with TMIP. Similarly, significant variables in univariate analysis were taken as independent variables and the events of TMIP on POD 30 as a dependent variable. Results from logistic multivariate regression revealed that portal vein diameter ≥ 15 mm on POD 30 was the only significant independent risk factor for TMIP (RR 3.636, 95% CI 1.466–9.021, P = 0.005), as shown in Table 3.
Discussion
Chronic hepatitis B cirrhosis may result in patients with varying degree of portal hypertension, which indicates increased portal vascular resistance [23]. Owing to HBV infection being the main cause of liver cirrhosis in Asia [2, 3], to ensure homogeneity in etiology for the formation of TMIP, this study was focused on patients with cirrhosis owing to HBV alone. Our findings will be helpful in providing accurate treatment for specific groups with a higher risk for TMIP after LSD owing to HBV infection.
Despite high rates of splenic vein thrombosis, this does not directly interfere with liver function in the short term. In addition, the incidence of mesenteric venous thrombosis in PVST is also infrequent, ranging from 0 (0/75) to 1.3% (1/80) [22, 24]. Thus, this study focused on TMIP after LSD.
The incidence of the thrombosis of the main and intrahepatic branches of the portal vein (TMIP) accounts for a relatively high proportion in PVST. It has been reported that in patients with cirrhosis who develop PVST, TMIP ranges from 61.7 (132/214) to 64.6% (51/79) [25, 26]. As for patients with cirrhosis who have undergone LS, Ikeda et al. reported that postoperative PVST occurred in 12 patients, among whom 8 (66.7%) had TMIP [27]. A previous study also showed that main trunk thrombosis and splenic vein thrombosis were major events in PVST after LSD and found that although patients received anticoagulation therapy, including aspirin tablets or warfarin sodium, the incidence rates of PVST were 47.1% and 41.2% on POD 7 and 52.2% and 41.3% on POD 30, respectively [18].
Although OSD can relieve portal venous pressure, the incidence of PVST after OSD ranges from 18.3 to 30.0% [13, 14]. Furthermore, LSD not only reduces portal venous pressure but it also has the advantages of minimal invasiveness, rapid rehabilitation, and reducing inflammatory responses in comparison with OSD [15,16,17]. It is worth noting that the rate of PVST is higher after LSD, ranging from 42.6 to 50.0%, as compared with OSD [14, 18]. In particular, the formation of TMIP after LSD or OSD accounts for a higher proportion of PVST cases, ranging from 30 to 52.2% [14, 18]. This pathological process in TMIP concurrently leads to significantly increased portal vein pressure and blockage of perfusion to the liver from the portal vein, which directly exacerbates damage to the liver [21]. In previous research, the occurrence rate of TMIP in postoperative PVST was 41.3% on POD 7 and 58.7% on POD 30 in patients who had undergone LSD [24]. Similarly, in this study, the incidence of TMIP in patients with postoperative PVST on POD 7 reached 42.4% and 50% on POD 30. Therefore, we should pay greater attention to preventing TMIP in patients with a higher risk of developing TMIP after LSD.
The causes of TMIP after LSD remain controversial. Several factors are thought to be responsible for the development of postoperative TMIP, as follows. During the procedure of laparoscopy, the application of CO2 in the pneumoperitoneum leads to a hypercoagulable state, which may contribute to TMIP [28, 29]. Additionally, the use of the LigaSure vessel sealing device (Covidien, Boulder, CO, USA) and harmonic shears (Ethicon, Cincinnati, OH, USA) may result in damage to the venous intima owing to heat energy or oscillation.
Hypersplenism is caused by increased portal blood flow to the splenic vein owing to cirrhosis [30]. When patients receive splenectomy and azygoportal disconnection, changes in the portal venous system hemodynamics will be reversed [12]. The velocity of blood flow in the portal vein will be slowed on account of loss of splenic vein perfusion to the portal vein [31]. Rapid elevation of postoperative thrombocytosis, coupled with the injury of the venous intima owing to energy-producing instruments and hemodynamic changes of the portal vein, are all pathogenic factors of PVST [29, 32, 33].
Enlarged splenic vein diameter has been reported as an independent risk factor for PVST in patients with cirrhosis who undergo splenectomy [34]. However, in this study, splenic vein diameter was not identified as a significant factor for TMIP. The reason for this might be that the portal vein diameter was not included as a variable in the statistical analysis of that previous study.
To a certain extent, the diameter of the portal vein is positively correlated with portal vein pressure in patients with cirrhosis. The larger the diameter of the portal vein, the higher the portal hypertension and the slower the flow velocity of the portal vein, sequentially. However, a larger portal vein diameter is often associated with injured venous intima. Therefore, enlarging the portal vein diameter can stimulate the formation of thrombosis, regardless of the surgical procedure performed [31, 34]. It has also been reported that the portal vein diameter can be used to accurately predict PVST after OSD [31]. In a previous study, portal vein diameter ≥ 13 mm was reported to be an independent factor for PVST after LS in patients with cirrhosis of various etiologies, including HBV, hepatitis C virus, schistosomiasis, and autoimmunity [35].
In this study, portal vein diameter ≥ 13 mm on POD 7 and ≥ 15 mm on POD 30 both showed a significant positive correlation with TMIP. Some studies have reported that PVST mainly occurs within 1 month after surgery [22, 36]. The question arises of why the independent risk factor of portal vein diameter ≥ 13 mm on POD 7 increased to ≥ 15 mm on POD 30. Some possible explanations concerning the change are as follows. First, with increased time after LSD, the influence of a hypercoagulable state owing to CO2 used in the pneumoperitoneum on postoperative PVST gradually weakens [28, 29]. What’s more, the gradual postoperative decline in platelet count and adjustment by the organism to the change in portal venous system hemodynamics are primary factors. Additionally, the damage to the vascular intima caused by heat energy or oscillation is gradually repaired. Owing to a combination of these factors, on POD 30 only the elevated portal vein diameter ≥ 15 mm reached the new threshold value for the formation of TMIP, which may be attributed to a broader portal vein diameter associated with lower velocity of the portal vein system and greater possibility of damage to the venous intima, thus contributing to the development of TMIP.
In addition, from POD 7 to POD 30, TMIP was found to be resolved in 14 patients, and another 14 patients with persistent TMIP had a wider portal vein diameter than that of 14 patients with resolved TMIP. Although there was no significant difference of the portal vein diameter between two groups, it may be due to small sample size (only 28 cases).
To the best of our knowledge, this study was the first to explore predictors for TMIP on POD 7 and POD 30 after LSD and also the first to focus on cirrhosis owing to HBV infection only. We found that portal vein diameter ≥ 13 mm and ≥ 15 mm could both effectively predict TMIP in patients with HBV infection after LSD on POD 7 and POD 30, respectively. The RR of TMIP was increased 5.328 times with portal vein diameter ≥ 13 mm compared with portal vein diameter < 13 mm on POD 7. Similarly, in comparison with portal vein diameter < 15 mm, the RR of TMIP was elevated 3.636 times with portal vein diameter ≥ 15 mm on POD 30. In our previous study, warfarin and aspirin both can effectively prevent the formation of TMIP after LSD. Therefore, anticoagulant therapy, such as aspirin and warfarin [22], should be used to prevent TMIP in patients with a high risk of TMIP after LSD. If patients with refractory TMIP, warfarin was more likely to achieve a satisfactory therapeutic effect. The relevant details message has been described in previous research [22]. The present findings will be beneficial in helping to reduce the incidence of TMIP as much as possible.
References
The Polaris Observatory Collaborators (2018) Global prevalence, treatment, and prevention of hepatitis B virus infection in 2016: a modelling study. Lancet Gastroenterol Hepatol 3:383–403
Li H, Yan L, Shi Y, Lv D, Shang J, Bai L, Tang H (2020) Hepatitis B Virus Infection: overview. Adv Exp Med Biol 1179:1–16
Zhang L, Chen Y, Zhang LJ, Wang M, Chang DL, Wan WW, Zhang BX, Zhang WG, Chen XP (2019) HBV induces different responses of the hepatocytes and oval cells during HBV-related hepatic cirrhosis. Cancer Lett 443:47–55
Wright AS, Rikkers LF (2005) Current management of portal hypertension. J Gastrointestinal Surg 9:992–1005
Bancu S, Borz C, Popescu G, Torok A, Mureşan A, Bancu L, Turcu M (2007) Spleno-renal distal and proximal shunts for hypersplenism due to hepatic cirrhosis. Chirurgia 102:665–668
Adam R, Karam V, Delvart V, O’Grady J, Mirza D, Klempnauer J, Castaing D, Neuhaus P, Jamieson N, Salizzoni M et al (2012) Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR). J Hepatol 57:675–688
Bodzin AS, Baker TB (2018) Liver transplantation today: where we are now and where we are going. Liver Transplant 24:1470–1475
Narahara Y, Kanazawa H, Fukuda T, Matsushita Y, Harimoto H, Kidokoro H, Katakura T, Atsukawa M, Taki Y, Kimura Y et al (2011) Transjugular intrahepatic portosystemic shunt versus paracentesis plus albumin in patients with refractory ascites who have good hepatic and renal function: a prospective randomized trial. J Gastroenterol 46:78–85
Salerno F, Merli M, Riggio O, Cazzaniga M, Valeriano V, Pozzi M, Nicolini A, Salvatori F (2004) Randomized controlled study of TIPS versus paracentesis plus albumin in cirrhosis with severe ascites. Hepatology 40:629–635
De Cleva R, Herman P, D’Albuquerque LA, Pugliese V, Santarem OL, Saad WA (2007) Pre- and postoperative systemic hemodynamic evaluation in patients subjected to esophagogastric devascularization plus splenectomy and distal splenorenal shunt: a comparative study in schistomomal portal hypertension. World J Gastroenterol 13:5471–5475
Yang Z, Qiu F (2000) Pericardial devascularization with splenectomy for the treatment of portal hypertension. Zhonghua wai ke za zhi [Chin J Surg] 38:645–648
Zhang Y, Wen T, Yan L, Chen Z, Yang H, Deng X, Liang G, Li G, Zhang X, Ran S, Liao Z (2009) The changes of hepatic hemodynamics and functional hepatic reserve after splenectomy with periesophagogastric devascularization. Hepatogastroenterology 56:835–839
Huang L, Yu Q, Wang J (2018) Association between changes in splanchnic hemodynamics and risk factors of portal venous system thrombosis after splenectomy with periesophagogastric devascularization. Med Sci Monit 24:4355–4362
Cheng Z, Li JW, Chen J, Fan YD, Bie P, Wang SG, Zheng SG (2013) Laparoscopic versus open splenectomy and esophagogastric devascularization for bleeding varices or severe hypersplenism: a comparative study. J Gastrointest Surg 17:654–659
Bai DS, Qian JJ, Chen P, Yao J, Wang XD, Jin SJ, Jiang GQ (2014) Modified laparoscopic and open splenectomy and azygoportal disconnection for portal hypertension. Surg Endosc 28:257–264
Yu H, Guo S, Wang L, Dong Y, Tian G, Mu S, Zhang H, Li D, Zhao S (2016) Laparoscopic splenectomy and esophagogastric devascularization for liver cirrhosis and portal hypertension is a safe, effective, and minimally invasive operation. J Laparoendosc Adv Surg Tech A 26:524–530
Jiang GQ, Chen P, Qian JJ, Yao J, Wang XD, Jin SJ, Bai DS (2014) Perioperative advantages of modified laparoscopic vs open splenectomy and azygoportal disconnection. World J Gastroenterol 20:9146–9153
Jiang GQ, Xia BL, Chen P, Qian JJ, Jin SJ, Zuo SQ, Bai DS (2016) Anticoagulation therapy with warfarin versus low-dose aspirin prevents portal vein thrombosis after laparoscopic splenectomy and azygoportal disconnection. J Laparoendosc Adv Surg Tech A 26:517–523
Parikh S, Shah R, Kapoor P (2010) Portal vein thrombosis. Am J Med 123:111–119
Anstee QM, Dhar A, Thursz MR (2011) The role of hypercoagulability in liver fibrogenesis. Clin Res Hepatol Gastroenterol 35:526–533
D’Amico G, De Franchis R (2003) Upper digestive bleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators. Hepatology 38:599–612
Bai DS, Xia BL, Zhang C, Ye J, Qian JJ, Jin SJ, Jiang GQ (2019) Warfarin versus aspirin prevents portal vein thrombosis after laparoscopic splenectomy and azygoportal disconnection: a randomized clinical trial. Int J Surg 64:16–23
Moriyasu F, Nishida O, Ban N, Nakamura T, Miura K, Sakai M, Miyake T, Uchino H (1986) Measurement of portal vascular resistance in patients with portal hypertension. Gastroenterology 90:710–717
Jiang GQ, Bai DS, Chen P, Xia BL, Qian JJ, Jin SJ (2016) Predictors of portal vein system thrombosis after laparoscopic splenectomy and azygoportal disconnection: a retrospective cohort study of 75 consecutive patients with 3-months follow-up. Int J Surg 30:143–149
Naymagon L, Tremblay D, Zubizarreta N, Moshier E, Mascarenhas J, Schiano T (2020) Safety, efficacy, and long-term outcomes of anticoagulation in cirrhotic portal vein thrombosis. Digest Dis Sci
Amitrano L, Guardascione MA, Brancaccio V, Margaglione M, Manguso F, Iannaccone L, Grandone E, Balzano A (2004) Risk factors and clinical presentation of portal vein thrombosis in patients with liver cirrhosis. J Hepatol 40:736–741
Ikeda M, Sekimoto M, Takiguchi S, Kubota M, Ikenaga M, Yamamoto H, Fujiwara Y, Ohue M, Yasuda T, Imamura H et al (2005) High incidence of thrombosis of the portal venous system after laparoscopic splenectomy: a prospective study with contrast-enhanced CT scan. Ann Surg 241:208–216
Lindberg F, Rasmussen I, Siegbahn A, Bergqvist D (2000) Coagulation activation after laparoscopic cholecystectomy in spite of thromboembolism prophylaxis. Surg Endosc 14:858–861
Pietrabissa A, Moretto C, Antonelli G, Morelli L, Marciano E, Mosca F (2004) Thrombosis in the portal venous system after elective laparoscopic splenectomy. Surg Endosc 18:1140–1143
La Villa G, Gentilini P (2008) Hemodynamic alterations in liver cirrhosis. Mol Aspects Med 29:112–118
Zhang Y, Wen TF, Yan LN, Yang HJ, Deng XF, Li C, Wang C, Liang GL (2012) Preoperative predictors of portal vein thrombosis after splenectomy with periesophagogastric devascularization. World J Gastroenterol 18:1834–1839
Crary SE, Buchanan GR (2009) Vascular complications after splenectomy for hematologic disorders. Blood 114:2861–2868
Watters JM, Sambasivan CN, Zink K, Kremenevskiy I, Englehart MS, Underwood SJ, Schreiber MA (2010) Splenectomy leads to a persistent hypercoagulable state after trauma. Am J Surg 199:646–651
Kinjo N, Kawanaka H, Akahoshi T, Tomikawa M, Yamashita N, Konishi K, Tanoue K, Shirabe K, Hashizume M, Maehara Y (2010) Risk factors for portal venous thrombosis after splenectomy in patients with cirrhosis and portal hypertension. Br J Surg 97:910–916
Jiang GQ, Bai DS, Chen P, Qian JJ, Jin SJ, Wang XH (2016) Risk factors for portal vein system thrombosis after laparoscopic splenectomy in cirrhotic patients with hypersplenism. J Laparoendosc Adv Surg Tech A 26:419–423
Wang LH, Lu W, Shen GJ, Yu YS, Zhu Ge YH, Hu YG, Wu XQ, Xu TS (2007) Portal vein thrombosis after devascularization procedures in patients with portal hypertension. Zhonghua PutongWaike Zazhi 22:616–618
Acknowledgements
This work was supported by the Project of Invigorating Health Care through Science, Technology and Education: Jiangsu Provincial Medical Youth Talent (QNRC2016331).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Longfei Wu, Dousheng Bai, Lin Shi, Shengjie Jin, Baohuan Zhou, and Guoqing Jiang have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, LF., Bai, DS., Shi, L. et al. Predictors of portal vein thrombosis after laparoscopic splenectomy and azygoportal disconnection in hepatitis B cirrhosis: a prospective study. Surg Endosc 36, 4090–4098 (2022). https://doi.org/10.1007/s00464-021-08730-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08730-5