Abstract
Introduction
Limited information regarding the usefulness of bowel lengthening in adult patients with short bowel syndrome is available.
Methods
Retrospective review of a single center series of intestinal lengthening over 15-year period in patients ≥18 years old.
Results
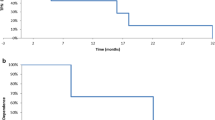
Twenty adult patients underwent Bianchi (n = 6) or serial transverse enteroplasty (STEP) (n = 15). Median age was 38 (18–66) years and 11 were female. Indications were (a) to increase the enteral caloric intake thereby reduce or wean parenteral nutrition (PN) (n = 14) or (b) for bacterial overgrowth (n = 6). Twelve patients required additional procedures to relieve the anatomical blockade. Median remnant bowel length prior to surgery, length gained and final bowel length was 60, 20, and 80 cm, respectively. Survival was 90% with mean follow-up of 4.1 years (range = 1–7.9 years). Two patients died during follow-up. Intestinal transplant salvage was required in one patient 4.8 years after STEP. Overall, of 17 patients, ten (59%) patients achieved enteral autonomy and were off PN. Of seven patients who are on PN, three patients showed significant improvement in enteral caloric intake. All except one showed significant improvement in symptoms of bacterial overgrowth.
Conclusions
Bowel lengthening is technically feasible and effectively leads to weaning from PN in more than half of the adult patients. Lengthening procedures may be an underutilized treatment for adults with short bowel syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With institution of multidisciplinary intestinal failure centers1 and with advances in intestinal transplantation (IT), survival of patients with short bowel syndrome (SBS) improved considerably during the past two decades.2 Survival after IT now approaches that of other solid organ allograft recipients and is similar to survival on long-term parenteral nutrition (PN). Despite these advances, IT is associated with a high risk for infection, rejection, and other complications related to immunosuppression.2 For this reason, when other medical and surgical alternatives are available for SBS, these should be maximized. Several medical and surgical management strategies have been described for SBS with variable results.3–6 The goals of surgical treatment are to improve function of the intestinal remnant, expand intestinal surface area and treat intestinal complications. Bowel lengthening procedures (Bianchi and recently the serial transverse enteroplasty (STEP)) are two of the surgical alternatives for SBS. Although bowel lengthening procedures have been used extensively in pediatric patients with excellent results,7 there is paucity of information in adults with SBS.7–10 This is the first study specifically describing surgical lengthening in adults. Patient characteristics are described and risk factors for survival and ability to wean from PN are examined.
Patients and Methods
We retrospectively reviewed the medical history including clinical and laboratory data, and operative records for all patients over 18 years of age who underwent intestinal lengthening procedures for short bowel syndrome between January 1993 and March 2008 at the University of Nebraska Medical Center. This study was approved by the Institutional Review Board.
All patients in the study were referred to our institution for evaluation for intestinal rehabilitation program or intestinal transplantation. All of them are on various degrees of PN for their total caloric requirement. Most of them had experienced various complications of SBS, which include bacterial overgrowth, diarrhea, weight loss, and recurrent septicemia. Patients were divided into two groups depending upon the predominant reason for surgical lengthening (a) to increase the enteral caloric intake (decrease/wean PN requirement) in patients with poor enteral progression/adaptation and had dilated small bowel loops on endoscopy or imaging studies (preferably ≥4 cm in diameter). (b) Intractable symptoms of bacterial overgrowth in the setting of SBS not controlled with antibiotics and had dilated small bowel loops. Patients who had anatomical causes of bowel obstruction were corrected at the time of bowel lengthening. Careful evaluation was performed to exclude patients with end-stage liver disease and/or complications of cirrhosis, who were likely better candidates for liver/small bowel transplantation.
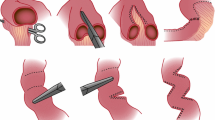
During the operation, an intraoperative measurement of the remnant small bowel from the ligament of Treitz to the ileocolonic junction/ostomy along the antimesenteric border was performed. In most cases, repeat measurement was performed after lengthening. The technical details of Bianchi-type bowel lengthening11 and STEP procedure12 have been previously described.
The endpoints of the analysis were resolution of primary symptoms in the patients as discussed above along with patient survival, weaning from PN, or need for intestinal transplantation.
Results
We performed 21 lengthening procedures (6 Bianchi and 15 STEP procedures) in 20 patients between January 1993 and March 2008. One patient underwent STEP and Bianchi procedures at the same time. There were nine males and 11 females. Median age of the patient population was 38 years (range, 18–66 years). The primary diagnosis responsible for SBS was listed in Table 1. The indications for lengthening procedure include inability to wean TPN (n = 14) and bacterial overgrowth (n = 6). Twelve patients required additional surgery to correct anatomical bowel pathology. There were two patients in this series who underwent STEP procedure after prior Bianchi, and two additional patients had a prior reversed intestinal segment procedure. Intestinal anatomy includes: initial length of remnant bowel, bowel length gained after the procedure, final length of bowel, percentage of small bowel length gained along with colon anatomy is shown in Table 2. Mean/median (range) remnant bowel length prior to surgery, length gained, and final bowel length was 71/60 (25–150), 29/20 (10–92), and 101/80 (38–172) cm, respectively.
Outcomes of Surgical Lengthening
Bacterial Overgrowth (n = 6)
One patient in this group required additional stricturoplasty. All except one showed significant improvement in symptoms. One patient had initial improvement with recurrence of symptoms and on further investigations found to have a stricture and this patient is being considered for re-STEP. In addition, three out of six patients were weaned of PN.
For Enteral Autonomy (n = 14)
Although every patient in our series was on some degree of PN dependence, 14 patients required surgery primarily to increase the enteral intake thereby reduce/wean PN. In these patients we were unable to advance enteral intake prior to surgery. In this group, two patients died during follow-up and one patient underwent transplantation and was off PN. Seven out of remaining 11 patients, were weaned off PN. Nine patients required operation for various types of intestinal obstruction, one patient required surgery for high ostomy output with the plan to do reversal of intestinal segment to reduce the stoma output, and one additional patient needed repair of enterocutaneous fistula from prior Bianchi procedure. All these patients had no further bowel obstructions, but one has developed enterocutaneous fistula which is being managed conservatively at the time of last follow-up. In the patient who was scheduled for reversal of intestinal segment during operation small bowel was very short (25 cm long). Additionally, this length of bowel was moderately dilated and after careful consideration, it was determined that patient may benefit from a STEP enteroplasty with a modest gain in length and perhaps slowing of her ostomy output. In subsequent months patient developed rapid worsening of her liver disease and was referred for liver and small intestine transplantation, but died after the patient elected not to pursue transplantation.
Overall, of the 17 patients, 10 (59%) patients achieved enteral autonomy and were off PN at last follow-up. Additionally, three patients, who had previously weaned from PN reverted back to PN dependence, at the time of last follow-up. Of seven patients who are on PN, four patients did not show any improvement in enteral caloric intake during follow-up, three patients showed significant improvement (enteral calories as percentage of total calories before/after = 10% vs 50%, 10% vs 50% and 30% vs 50%, respectively).
-
1.
Survival
Patient survival 90% with mean follow-up of 4.13 years (median, 3.8 years; range, 1–7.9 years). One adult died with liver failure and sepsis after refusing intestinal transplantation and another patient due to line sepsis.
-
2.
Intestinal Transplantation
Intestinal transplantation was performed in one patient in this series after 4.8 years after STEP enteroplasty (20.4 years after Bianchi). The indications for transplantation were continued dependence on PN, recurrent line related septicemia and development of PN induced end-stage liver disease. This patient underwent combined liver small bowel transplantation and is doing well at 2 years 3 months follow-up.
-
3.
Complications
A summary of early and late major postoperative complications that occurred after intestinal lengthening is listed in Table 2. Early complications occurred within a month after surgery. In addition, most of the patients experienced at least one episode of central line infection after lengthening and many had repeated episodes until the central venous catheter was removed. Many of the patients required hospitalization on multiple occasions for management of fluid and electrolyte balance and intravenous antibiotics, but generally the infections were not life threatening and were not attributable to the surgical lengthening per se. The re-hospitalizations were attributed to the short bowel syndrome and due to the ongoing need for central venous access and PN.
Discussion
Most of patients were referred to our center for evaluation in our intestinal rehabilitation program or for small bowel transplantation. Initial strategy was to maximize the enteral tolerance through feeding and gut adaptation. All patients were evaluated for clinical or laboratory evidence of liver disease prior to recommending lengthening procedures. In patients with complications of cirrhosis, lengthening was not offered and these patients were referred for intestinal transplantation. Bowel lengthening was done when patients did not show any further progression with enteral tolerance with persistent need for PN or patients, who had evidence of dilated small bowel loops on imaging studies and symptoms of bacterial overgrowth unresolved with antibiotics.
There is no published data on bowel lengthening procedure exclusively in adults. Most reported series describe exclusively the pediatric population8 or predominantly pediatric patients with some adults included in one series7 and two additional single case reports.9,10 In children, bowel dilatation may be due to natural adaptation and increased growth, but the mechanism is unclear. In several adults in this series, the major indication for the surgical intervention was bowel obstruction secondary to strictures. The obstruction, rather than adaptation may explain the relative rarity of lengthening procedures in adults when compared with children.
To aid the bowel dilatation to perform lengthening procedure later, Georgeson et al. constructed a nipple valve sufficiently obstructive to force proximal bowel dilatation but not enough to precipitate pathologic obstruction. After a period of time, he followed this up with a Bianchi procedure.14 Construction of the Georgeson valve requires potential sacrifice of a segment of small bowel in the already short bowel and may be difficult to calibrate the degree of bowel obstruction. At present we do not know whether this procedure is applicable in adult patients with non-dilated bowel. In two patients in this series, the creation of a prior reversed intestinal loop may have acted as a functional obstruction, although the intention was not deliberate to achieve “sequential lengthening”.
In the initial part of the study, we had patients with Bianchi procedure (historically because it was the only option) and from 2002, we started performing STEP. As we gained more experience with STEP, we now preferentially perform the STEP as a primary procedure. This is due to following reasons. (a) Some of our primary STEP patients were not candidates for a Bianchi lengthening due to loss of vascularity in one leaf of the mesentery from prior surgery and/or a foreshortened mesentery. (b) The Bianchi procedure can only be performed once, as the mesentery cannot be further divided safely after the leaves have been separated. But STEP procedure can be performed either after prior Bianchi or other intestinal procedures or after STEP successfully.13 In our study, two patients had prior Bianchi lengthening and two had prior reversed intestinal segment prior to STEP. (c) As noted previously, one advantage of STEP over Bianchi lengthening is the ability to increase the final bowel length by greater than 100% of the original length. In the present series we have three patients in the STEP series had bowel lengthened 1, 1.58, and 1.7 times from original length.
Overall, 59% of patients were completely weaned off PN in our series. Weaning from PN in our series is comparable with published results of Bianchi and STEP (comparable with overall 54% in Bianchi4,14–21 and better than the 48% reported in the STEP registry8). When we analyzed factors affecting the PN dependence, we noticed that final length of the bowel (p = 0.01) and length of the bowel added after lengthening procedure (p = 0.04) were statistically different between patients who are enterally independent and PN dependent.
Of the six patients who underwent the bowel lengthening for bacterial overgrowth, five have experienced complete resolution of their symptoms. In addition, three of these patients had achieved enteral autonomy. Similar experience reported in pediatric patients who had STEP procedure.9,10 In view of the discussion above, finding bowel lengthening has a role in SBS patients with intractable symptoms of bacterial overgrowth.
Patient survival in 132 patients who have undergone Bianchi lengthening reported in various publications in the English literature was 80% and 92% in 38 patients reported in the STEP registry,8 which is comparable with 90% in our series. Because of the small sample group, we did not study factors affecting survival.
This is the largest single center series at this time with experience of bowel lengthening in adults; the study has some inherent drawbacks. (1) The number of patients is small and this hampered the ability to identify potential risk factors for survival, weaning from PN or need for intestinal transplantation. (2) It is difficult to separate the contribution of the medical management from the results of surgical intervention due to the multidisciplinary nature of this intestinal rehabilitation program. (3) Retrospective nature of study. (4) Short follow-up of the STEP patients in this series prevents assessment of the durability of the STEP procedure as has been demonstrated for the Bianchi procedure.
Conclusions
Intestinal lengthening is feasible and efficacious in the management of SBS in adult patients. Intestinal obstruction is a common cause of bowel dilatation in these patients. Bowel lengthening procedures may be an underutilized treatment for adults with short bowel syndrome.
References
Torres C, Sudan D, Vanderhoof J, Grant W, Botha J, Raynor S,Langnas A. Role of an intestinal rehabilitation program in the treatment of advanced intestinal failure. J Pediatr Gastroenterol Nutr 2007; 45: 204–212.
Sudan DL. Treatment of intestinal failure: intestinal transplantation. Nat Clin Pract Gastroenterol Hepatol 2007; 4: 503–510.
Pigot F, Messing B, Chaussade S, Pfeiffer A, Pouliquen X, Jian R. Severe short bowel syndrome with a surgically reversed small bowel segment. Dig Dis Sci 1990; 35: 137–144.
Thompson JS, Langnas AN, Pinch LW, Kaufman S, Quigley EM, Vanderhoof JA. Surgical approach to short-bowel syndrome. Experience in a population of 160 patients. Ann Surg 1995; 222: 600–605; discussion 605–607.
Garcia VF, Templeton JM, Eichelberger MR, Koop CE, Vinograd I. Colon interposition for the short bowel syndrome. J Pediatr Surg 1981; 16: 994–995.
Devine RM, Kelly KA. Surgical therapy of the short bowel syndrome. Gastroenterol Clin North Am 1989; 18: 603–618.
Sudan D, Thompson J, Botha J, Grant W, Antonson D, Raynor S, Langnas A. Comparison of intestinal lengthening procedures for patients with short bowel syndrome. Ann Surg 2007; 246: 593–601; discussion 601–594.
Modi BP, Javid PJ, Jaksic T, Piper H, Langer M, Duggan C, Kamin D, Kim HB. First report of the international serial transverse enteroplasty data registry: indications, efficacy, and complications. J Am Coll Surg 2007; 204: 365–371.
Uen YH, Liang AI, Lee HH, Hsu YH. Long-term outcome of intestinal lengthening procedure for short-bowel syndrome: a case report. Surgery 1999; 125: 117–120.
Modi BP, Langer M, Duggan C, Kim HB, Jaksic T. Serial transverse enteroplasty for management of refractory D-lactic acidosis in short-bowel syndrome. J Pediatr Gastroenterol Nutr 2006; 43: 395–397.
Bianchi A. Intestinal loop lengthening—a technique for increasing small intestinal length. J Pediatr Surg 1980; 15: 145–151.
Kim HB, Lee PW, Garza J, Duggan C, Fauza D, Jaksic T. Serial transverse enteroplasty for short bowel syndrome: a case report. J Pediatr Surg 2003; 38: 881–885.
Andres AM, Thompson J, Grant W, Botha J, Sunderman B, Antonson D, Langnas A, Sudan D. Repeat surgical bowel lengthening with the STEP procedure. Transplantation 2008; 85: 1294–1299.
Georgeson K, Halpin D, Figueroa R, Vincente Y, Hardin W, Jr. Sequential intestinal lengthening procedures for refractory short bowel syndrome. J Pediatr Surg 1994; 29: 316–320; discussion 320–311.
Aigrain Y, Cornet D, Cezard JP, Boureau M. Longitudinal division of small intestine: a surgical possibility for children with the very short bowel syndrome. Z Kinderchir 1985; 40: 233–236.
Boeckman CR, Traylor R. Bowel lengthening for short gut syndrome. J Pediatr Surg 1981; 16: 996–997.
Sudan D, DiBaise J, Torres C, Thompson J, Raynor S, Gilroy R, Horslen S, Grant W, Botha J, Langnas A. A multidisciplinary approach to the treatment of intestinal failure. J Gastrointest Surg 2005; 9: 165–176; discussion 176–167.
Pokorny WJ, Fowler CL. Isoperistaltic intestinal lengthening for short bowel syndrome. Surg Gynecol Obstet 1991; 172: 39–43.
Bianchi A. Longitudinal intestinal lengthening and tailoring: results in 20 children. J R Soc Med 1997; 90: 429–432.
Weber TR. Isoperistaltic bowel lengthening for short bowel syndrome in children. Am J Surg 1999; 178: 600–604.
Waag KL, Hosie S, Wessel L. What do children look like after longitudinal intestinal lengthening. Eur J Pediatr Surg 1999; 9: 260–262.
Acknowledgments
The authors acknowledge the help of Becky Weseman, IRP dietician, who assisted in collection of the data described in this manuscript. They also thank Robin High for assistance in the statistical analysis.
Grant Support
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yannam, G.R., Sudan, D.L., Grant, W. et al. Intestinal Lengthening in Adult Patients with Short Bowel Syndrome. J Gastrointest Surg 14, 1931–1936 (2010). https://doi.org/10.1007/s11605-010-1291-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-010-1291-y