Abstract
Background
Early and late outcomes after superior mesenteric-portal vein resection (VR) combined with pancreaticoduodenectomy, major hepatectomy, or both for pancreaticobiliary carcinoma were retrospectively evaluated. VR is the most frequently used vascular procedure in this field, but an exact role of VR has not been compared according to the primary site of tumor.
Materials and Methods
Postoperative outcomes were compared between surgery with and without VR in each of the three disease-based groups: hilar cholangiocarcinoma and intrahepatic cholangiocarcinoma with hilar extension (HIC, 56), middle and distal cholangiocarcinoma and gallbladder carcinoma (DGC, 118), and pancreatic head adenocarcinoma (PHC, 77).
Results
VR was performed in 19.6% of HIC, 8.5% of DGC, and 45.5% of PHC. In-hospital death was 7.1% (4 of 56) patients with VR (3 of DGC and 1 of PHC). Operations with VR in DGC showed a larger amount of blood loss and more increased ratio of R1operation than those with no VR. In HIC, DGC, and PHC, median survival time of patients with VR was 37, 6.8, and 20 months and that of patients without VR was 42.9, 28.6, and 20.3 months, respectively. VR did not affect survival either in HIC or in PHC; however, in DGC, VR was accompanied with dismal outcome compared with no VR (p = 0.001).
Conclusions
Aggressive surgery with VR can be justified both in HIC and in PHC but should not be recommended for DGC. Surgical outcomes of VR differed considerably, depending on the sites of the primary tumor.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Resection of superior mesenteric-portal vein (VR) is the most frequently used vascular procedure in aggressive surgery for cholangiocarcinoma,1–8 gallbladder cancer,8,9 and pancreatic cancer.10–26 Especially in surgery for pancreatic cancer, VR is an indispensable surgical technique and VR itself does not worsen the postoperative survival.15,16,18–25 However, clear discrimination from tumor adherence to cancer invasion is often difficult.11,15,22 Several reports pointed out that the surgical outcome after VR is closely related to the depth of cancer invasion into the wall of the portal vein,11,12,26,27 and patient survival after VR is preferable to cases without microscopic invasion compared to those with the invasion.16,20,28 Furthermore, it was reported that tumors requiring VR increases the likelihood of association with margin-positive resection.21,19 Considerable variance regarding the incidence of concomitant VR, 0–28%, was pointed out from a domestic survey of seven large volume centers in Germany.29 This variance may involve differences in surgical strategies for pancreatic cancer.30,13
Similarly, in hilar cholangiocarcinoma, the incidence of VR combined with aggressive surgery varied among large-volume studies, ranging from 6.3 to 43%.2,3,5,6,31–34 As for survival after VR, Neuhaus et al.3,4 said that VR more frequently occurred in left-sided hepatectomy and was accompanied by favorable outcome when compared with no VR. Also, Hemming et al.6 revealed that there was no difference in survival between patients who had VR and those who did not. Contrary to this view, Ebata et al. demonstrated in their series, which included the largest number of VRs, that there was negative prognostic factor regardless of the presence or absence of microscopic invasion.3 In gallbladder cancer and distal-sided bile duct cancer, a few studies focus on VR.7–9,35
Although serious complications related to VR were documented only in a few reports,24,36,37 it is generally considered a safe vascular procedure that does not exacerbate short-term results. Aggressive surgery for cholangiocarcinoma, gallbladder carcinoma, and pancreatic head adenocarcinoma involve the potential risk of VR intrinsically. However, differences in postoperative outcomes after VR have not been compared based on the site of the primary tumor. In the present study, we have evaluated short- and long-term outcomes of VR combined with aggressive surgery for biliary tract and pancreatic carcinomas, and we have discussed the variance of clinical implication of VR based on differences in the primary disease.
Materials and Methods
From 1987 to 2005, 56 patients underwent superior mesenteric and portal vein resection combined with radical surgery for cholangiocarcinoma, gallbladder carcinoma, and invasive ductal carcinoma of pancreas. Operations performed concomitant with 56 VRs were major hepatectomy (more than 2 hepatic sections) with hilar dissection (n = 11), pancreaticoduodenectomy with or without gastrectomy (n = 38), or hepatopancreaticoduodenectomy (n = 7). For comparative analyses of morbidity, mortality, postoperative liver function, and survival outcomes in the 56 patients with VR, 195 patients who underwent major hepatectomy (62), pancreaticoduodenectomy (118), or hepatopancreaticoduodenectomy (15) without VR during the same period were reviewed and investigated as the control. Operations with only minimal probability or necessity for VR were excluded from the analyses to ensure fair and accurate comparison: bile duct resection, cholecystectomy with partial hepatectomy, or partial hepatectomy without the hilar dissection. Totally, this retrospective study included 251 patients (56 with VR and 195 without VR) who underwent major hepatectomy, pancreaticoduodenectomy, or hepatopancreaticoduodenectomy with curative intent.
This study focused on VR and investigated the difference in surgical results of VR according to site of the primary tumor. For this, the 251 tumors were firstly dichotomized to pancreatic head carcinoma (PHC, n = 77) and biliary tract carcinoma (174), and then the latter was divided into two disease-based groups: HIC (n = 56), hilar cholangiocarcinoma (49) and intrahepatic cholangiocarcinoma involving the porta hepatis (7), and DGC (118), middle and distal cholangiocarcinoma (68) and gallbladder carcinoma (50). Preoperative variables, surgical findings, postoperative complications within the same hospital stay, and survival were analyzed and compared between patients with VR and those without in each of the three disease-based groups. Operative mortality and in-hospital deaths were defined as death within 30 days and within the same hospital admission, respectively.
Pathologic characteristics of primary tumor, including extent of tumor, lymph node metastasis, final tumor stage, surgical margin status, and tumor differentiation were described according to the American Joint Commission on Cancer (AJCC) classification. Microscopic invasion of the vein was defined as positive when a tumor infiltrated into the adventitia of the vein or beyond it. Continuous variables were compared using the Mann–Whitney U test and categorical variables with a chi-square test or Fisher’s exact test. Survival probabilities were calculated from date of surgery and estimated using the Kaplan–Meier method and compared by the log-rank test (significant difference, p < 0.05). Cox regression was used to determine independent predictors of outcome, using survival as the dependent variable and factors significant on univariate analysis as covariates. Operative mortality was excluded from survival analyses. Statistical calculations were performed using Statistical Package for the Social Sciences (SPSS), version 9.0 (SPSS, Chicago, IL, USA).
Vascular Procedures for Portal Vein
The type of surgery according to the site of the primary tumor is listed in Table 1. VR was performed when the obvious involvement of the vein was demonstrated by preoperative imaging examination or when the tumorous invasion to the vein wall was suspected during surgery. To perform an en-bloc resection, the tight adhesion of the vein to tumor was not separated before the vein resection. VR was carried out in 11 (19.6%) patients of HIC, in 10 (11.8%) of DGC (5 each in the middle and distal cholangiocarcinoma and in the gallbladder carcinoma), and in 35 (45.5%) of PHC (Table 1); 44 (78.6%) were segmental resections and 12 (21.5%) were tangential resections. About 75% of 56 vascular procedures were performed by the first author (I.K.). Vein graft was used for reconstruction in two patients. A median length ± standard deviation of excised portal vein was 3.0 ± 1.2 cm (1–6 cm) in 40 segmental resections (length of the remaining four cases before 1994 were not stated in the operation record). Median time of the portal clamping was 20 ± 5.7 min (11–40 min) in 35 patients (the clamping time was not available in 9 cases before 1994). In all 44 patients who underwent the segmental resection, the end-to-end anastomosis of the vein was carried out by the running suture technique with 5–0 or 6–0 nonabsorbable threads.
In this series, preoperative portal embolization technique was not used. In addition, the intraoperative catheterization into both hepatic artery and portal vein was performed for the adjuvant liver perfusion chemotherapy with 5FU in 14 patients with pancreatic carcinoma: 4 patients (11.4%) of VR group and 10 (23.8%) of no VR group.
Results
Preoperative and Operative Findings
The average age, male-to-female ratio, percent of patients with jaundice (total bilirubin level >3 mg/dl), hemoglobin concentration, and serum total protein and albumin levels were similar between patients with VR and those without, in each of the three disease-based groups (Table 2). In DGC, the frequency of VR did not differ from gallbladder carcinoma (10%) to middle and distal cholangiocarcinoma (7.4%). Hepatopancreaticoduodenectomy was carried out in a total of 22 patients, in whom 32% (7) underwent combined portal vein resection. Of the 22 hepatopancreaticoduodenectomy, 16 (73%) were carried out for DGC: 7 (10.3%) for middle or distal cholangiocarcinoma and 9 (18.0%) for gallbladder carcinoma (no significant difference). The estimated blood loss in DGC was significantly higher in patients with VR compared with those without (p = 0.027).
Liver Function After Surgery
The maximal levels of serum aspartate aminotransferate (AST) and alanine aminotransferate (ALT) in VR group were 366 and 310 IU/l in HIC, 148 and 119 IU/l in DGC, and 69 and 65 IU/l in PHC, respectively. Maximal total bilirubin (TB) levels were 3.4 mg/dl in HIC, 3.1 mg/dl in DGC, and 69 and 65 IU/L in PHC. Regardless of VR or no VR, the maximal AST and ALT values were higher in HIC and DGC compared with that in PHC. When dividing the 251 patients into two groups who underwent surgery with major hepatectomy (156) or without major hepatectomy (95), median values of AST, ALT, and TB showed a significant increase in patients with major hepatectomy (380, 325 IU/l, and 5.7 mg/dl) compared to those without (210, 208 IU/l, and 3.9 mg/dl; p = 0.001, 0.030, and <0.001, respectively). However, VR did not influence maximal values of AST, ALT, and TB after surgery in any one of the three disease-based groups (Table 3).
Complications After Surgery
Of the 251 patients, 6% (15) had operative or in-hospital deaths. The operative death was recorded in two (3.6%) patients of VR group and in four (2.1%) patients of no VR, and in-hospital death was observed in two (3.6%) patients of VR and in seven (3.6%) patients of no VR; there was no statistical difference of incidence between VR and no VR. In VR group, two operative deaths (one each in the gallbladder carcinoma and in PHC) were due to intra-abdominal hemorrhage, and two in-hospital deaths were caused by early recurrence of the gallbladder carcinoma. According to disease-based group, the in-hospital death including operative mortality occurred more frequently in HIC (8.9%) and in DGC (7.6%) compared to that in PHC (1.3%), although there were no statistical differences (p = 0.092 and 0.082, respectively; Table 3). Especially in the gallbladder carcinoma, three of the five patients who required VR died early after surgery, although surgery-related mortality was only one; two deaths were caused by tumor recurrence. Of 45 gallbladder carcinomas in no VR group, the surgery-related death was recorded in a patient (2.2%).
Overall morbidity was significantly higher in HIC among the three disease-based groups but did not differ between VR and no VR in any of the three disease-based groups. Only the pulmonary disorder requiring intensive treatment and acute renal failure developed frequently in VR group compared with no VR group (DGC; Table 3). Occurrence of intra-abdominal hemorrhage after surgery was not affected by the portal vein resection because the incidence was 3.6% (2) in VR group and 7.2% (14) in no VR (not significant difference). The hemorrhage in the two patients who underwent VR was caused by the rupture of pseudoaneurysm. Gastrointestinal hemorrhage from peptic ulcer after VR occurred in 9.1% of HIC and 5.7% of PHC; the figures were not statistically different to the incidence in no VR.
Regardless of VR or no VR, the pancreatic fistula after pancreatic resection was more frequent in DGC (20.0%, 19 of the 95 patients), compared with that in PHC (3.9%, n = 3, p = 0.004). However, VR itself did not influence the occurrence of pancreatic fistula (Table 3). The occurrence of bile leakage also did not differ between VR and no VR. The hyperbilirubinemia >10 mg/dl occurred in 3.6% (2) of the 56 patients with VR and in 8.2% (16) of the 195 patients without VR, with no statistical difference (p = 0.378; Table 3). Reoperation was performed in 8.9% (five) after surgery with VR, for adhesive ileus, intra-abdominal hemorrhage, intra-abdominal abscess, peritonitis due to the small bowel perforation, and leakage of colo-colostomy. Any causes for reoperations were not related to vascular procedure.
No early complication specific to VR was observed. Intrahepatic portal vein thrombosis occurred in two patients in whom the plastic tube was placed in the portal vein for liver perfusion chemotherapy; one (1.8%) was in VR group and another (0.5%) was in no VR group (no significant difference; Table 3). The thrombosis disappeared immediately after removal of the tube and anticoagulant therapy.
A symptomatic late complication specific to the portal vein resection during long-term follow-up period has been rarely observed in this series. In VR group, there was a patient who had sinistral portal hypertension due to tumor recurrence.
Pathologic Features
Positive rates of lymphatic permeation, microvenous permeation, perineural invasion, and lymph node metastasis were similar between VR and no VR groups in each of the three disease-based groups (Table 4). In DGC, VR group was accompanied with higher positivity of surgical margin compared with no VR (p = 0.008). When analyzing tumors of DGC separately, the middle and distal cholangiocarcinoma in VR group showed 60% (three of the five tumors) of positive surgical margin, whereas that in no VR was 15.9% (p = 0.045). Also in gallbladder carcinoma, margin positivity was so high in VR (60% of the five tumors), but there was not statistical difference compared with no VR (22.2%, p = 0.064).
In PHC, no significant difference was observed in all the parameters evaluated between VR and no VR. The tumor size of pancreatic adenocarcinoma also did not differ between tumors excised with VR and without (a mean value ± SD, 38.4 ± 12.2 mm and 35.5 ± 13.2 mm, respectively, p = 0.323). Microscopic invasion of the vein was more frequently observed in DGC (70%) among the three disease-based groups (45.5% in HIC and 42.9% in PHC); however, there were no statistical differences.Positivity of microscopic invasion did not differ between middle-distal cholangiocarcinoma and gallbladder carcinoma.
Survival Analyses
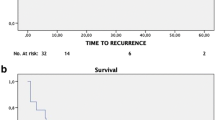
Among the three disease-based groups, PHC was associated with significantly worse median survival time (20.1 months) compared to others (41.8 months in HIC and 27.7 months in DGC, Fig. 1a). When analyzing the 54 patients who underwent VR, survival probabilities of DGC and of PHC were inverted, and DGC showed most dismal outcome (a median of 6.8 months) among the three groups (37.0 months in HIC and 20.0 months in PHC; p = 0.0016 and p = 0.0316 to DGC, respectively, Fig. 1b). In DGC with VR, five patients with middle or distal cholangiocarcinoma all died of tumor recurrence within 14 months after surgery, and also four patients with gallbladder carcinoma were succumbed to the disease at 37, 29, 4, and 3 months after surgery, respectively.
Survival curves in the three disease-based groups. In analyses for all patients (a), a median survival time (95% CI, months) was 41.8 months (36.4–47.3) in HIC (black line), 27.7 months (18.9–36.5) in DGC (dotted line), and 20.1 months (14.2–26.3) in PHC group (broken line). Statistical significances were HIC vs PHC, 0.003; DGC vs PHC, 0.0368; and HIC vs DGC, 0.2151. In analysis of patients who underwent VR (b), DGC showed significantly worse survival of a median of 6.8 months among the three disease-based groups (37.0 months in HIC and 20.0 months in PHC; p = 0.0016 and p = 0.0316, respectively). There was also a significant difference in survival between PHC and HIC (p = 0.0307).
In Table 5, univariate analyses for multiple prognostic parameters were calculated. Positive surgical margin and lymph node metastasis were important prognostic factors common to the three disease-based groups. The negative prognostic value of VR itself was prominent in DGC (surgeries with VR and without, p = 0.001) but was not demonstrated in HIC or in PHC (Fig. 2). In DGC, VR was a negative prognostic factor regardless of positive or negative microscopic invasion of the vein (Table 5). When performing subgroup analyses, portal vein invasion showed striking negative impact in the middle-distal cholangiocarcinoma (p = 0.001), whereas it was marginal difference in the gallbladder carcinoma (p = 0.055).
Postoperative survival in each of the three disease-based groups. A median survival time of patients without VR (dotted line) was 42.9 months (95%CI, 37–48.8 months) in HIC, 28.6 months (95% CI, 13.3–43.8 months) in DGC, and 20.3 months (95%CI., 11.4–29.1 months) in PHC. A median survival time of patients with VR (black line) is described in Fig. 1. Statistical difference in survival between surgeries with and without VR was observed only in DGC (p = 0.0001).
In PHC, microscopic invasion was a significant prognostic factor, but a median survival time of VR group without microscopic invasion was similar to that of no VR (Table 5). In HIC, median survival time in VR with microscopic invasion was shorter than that in no VR, although no statistical difference (27.5 months with 95%C.I.; 17–37 vs 41.8 months with 36–48). The median survival time in VR without microscopic invasion was 38.1 months, 95% confidence interval (CI) 36.6–39.4, with no significant difference to that in no VR. Multivariate analyses demonstrated two negative independent predictors each in DGC and in PHC, respectively: positive surgical margin and positive nodal metastasis, and positive surgical margin and histological differentiation (Table 6). The depth of tumor infiltration into the vein was evaluated in PHC; median survival time in nine tumors infiltrating into the tunica media or intima [11.1 months with 95%CI, 7–15.1] was significantly lesser than that in 25 tumors infiltrating up to the tunica adventitia (21.8 months with 95%CI, 14.4–29.2, p = 0.0301). The survival difference was not observed between the patient’s group of PHC with liver perfusion chemotherapy and that without in this series.
When analyzing all 54 patients who underwent VR, univariate analyses revealed 9 prognostic parameters with statistical difference as shown in Table 7. Among these parameters, multivariate analyses disclosed four negative prognostic predictors: site of the primary tumor (no HIC), surgical margin, microvenous permeation, and microscopic invasion to the vein (Table 8).
Discussion
Portal Vein Resection in Pancreatic Head Adenocarcinoma
VR has been widely performed for pancreas carcinoma since the report of the regional pancreatectomy,10 but its survival benefit has been still controversial. In general, incidence of VR seems to be inversely proportional to that of microscopic tumor invasion; more than 40% of VR rate was associated with 50–60% of microscopic vein wall invasion,12,20,27,38 whereas less than 40% of VR rate was accompanied by more than 70% of microscopic invasion.16,17,22,26,39 Although much variance was seen in the incidence of VR, the true venous infiltration was not so widely distributed; estimated figures calculated from several reports were 16–33%.12,16,17,20,22,26,27,38,39 Nevertheless, the low probability of true infiltration could not preclude the aggressive attitude to pancreaticoduodenectomy combined with VR.
Increased intraoperative blood loss with VR was pointed out,13,22,24 but the operative morbidity and mortality did not differ between operation with VR and without.14,22,25 In a recent report by Carrere et al.,14 VR did not influence the blood loss, but 22% of reoperation rate and 15% of postoperative hemorrhage rate after VR seems to be somewhat high because of 5.5 and 2.9% in our series, respectively. The incidence of pancreatic fistula significantly decreased in patients who underwent VR.14,28 More advanced pancreatic tumors and more decreased pancreatic function may reduce the probability of pancreatic fistula. However, pancreatic fistula after pancreaticoduodenectomy for pancreatic carcinoma is generally less frequent, compared to that for biliary tract carcinoma with normal pancreas. The vascular procedure showed no impact on increased risk of pancreatic fistula. On the other hand, superior mesenteric ischemia,22 bowel edema caused by prolonged venous occlusion time,18 or sinistral portal hypertension24,37 appear to be infrequent complications after VR. Leach et al.24 reported that the venous occlusion after VR occurred in 22% (7) of 31 patients: 5 were asymptomatic and the remaining 2 died of the condition. Although we experienced portal thrombosis with liver perfusion chemotherapy, the vein occlusion or sinistral portal hypertension caused by VR itself was not encountered. VR for pancreatic carcinoma is a safe vascular procedure, but we should take care of unexpected pathologic conditions related to the vascular procedure.
Exact correlation between long-term survival and concomitant VR remains unclear. Several reports have stated that true microscopic invasion into the vein wall was accompanied by lower probability of survival.11,12,16,20,26,27 Furthermore, the depth of tumor infiltration into the vein wall also affected postoperative survival.11,12,26,27 In the present study, VR itself showed no disadvantage on postoperative survival, but the probability of prognosis decreased when microscopic invasion was positive or when tumor infiltrated beyond the tunica adventitia. Fuhrman et al.13 stated that the portal vein involvement was a function of tumor location rather than aggressiveness of cancer biology. However, microscopic true infiltration should be considered as an indicator that reflects the local invasiveness of the primary tumor and poor prognosis. Interestingly, Hartel et al.16 mentioned that survival of the patients who underwent VR for a lesion with no microscopic invasion was superior to that of patients who did not undergo VR, whereas Shimada et al.28 described the results opposite to that of Hartel el al. In general, R0/R1 ratio did not differ between surgeries with and without VR, and en-bloc resection permits extirpation with potentially negative margins and may reduce the risk of local recurrence.13,20,22,24 In the report by Shimada et al.,28 the higher positivity of R1 operation, extrapancreatic neural invasion, and widespread nodal diseases in the VR group seems to influence their surgical outcomes. In treatment for pancreatic tumors with portal vein invasion, it was reported from the randomized control trial that resection surgery was superior to chemoradiotherapy alone.40 On the basis of safe performance in vascular procedure, VR combined with aggressive surgery can be justified in cases with potential risk of vein invasion.
Portal Vein Resection in Biliary Tract Carcinoma
In many studies for hilar cholangiocarcinoma, in-hospital mortality after major hepatectomy with VR ranged from 9 to 17%, with no significant difference compared to that with no VR.2,6,41 Zero mortality series with 40 consecutive major hepatectomies was reported by Kondo et al.,5 in which 14 patients underwent concomitant VR. In our series, in-hospital deaths were not observed after major hepatectomy with VR in HIC. Morbidity with VR was similar to that with no VR.2,5,6 In gallbladder cancer, it is reported that major hepatectomy combined with VR for cases with obstructive jaundice was accompanied with high in-hospital mortality of 20–36% due to postoperative hepatic coma.9,41 Also in our series, mortality significantly increased in surgery with VR than in without VR, but we did not encounter hepatic coma as the primary presentation of postoperative morbidities. Portal vein embolization was not carried out in our institution until 2005, but this technique is thought to be a modality of choice for improving postoperative outcome regardless of VR or no VR.42,43
The incidence of VR combined with hepatectomy for hilar cholangiocarcinoma widely ranged from 6.3 to 43%.2–6,8,31,33,34 Similarly in pancreatic cancer surgery, the difference in the treatment strategy seems to be a possible explanation for this variance. Neuhaus et al.3 reported that VR improved long-term survival, and only VR was identified as an independent predictor in patients who underwent R0 operation. Although microscopic infiltration of the portal vein was approximately 20% in their series, the curative right trisectionectomy with VR yielded a surprising outcome of 72% 5-year survival.4 On the other hand, Ebata et al.2 stated that macroscopic involvement of the portal vein affected postoperative survival statistically, but absence or presence of microscopic involvement had less impact on survival. More recently, Kondo et al.5 and Hemming et al.6 mentioned that there was no difference in survival between surgeries with and without VR, and our study also showed a similar tendency. An en-bloc resection with VR appears to enhance surgical clearance of tumor cells in porta hepatic.3,44 A routine use of VR is not standardized in the current status, but VR should not be precluded in cases with portal vein involvement detected before or during operation.
With regard to gallbladder carcinoma, only a few studies focused on the surgical outcome of surgery with VR and reported its unfavorable results.1,8,9,45 More than 3-year survival was rarely encountered even with aggressive surgery.1,9,45 In several studies about middle and distal cholangiocarcinoma amenable to pancreaticoduodenectomy, the description of VR was lacking46,47 or only the number of cases with VR was provided.48,49 Reported figures of 13,46 13.5,47 and 18%35 appear to be higher than in many other studies. Tseng et al.18 described that distal cholangiocarcinoma was found only in 2% (three) of 141 patients who underwent pancreaticoduodenectomy with VR but was carried out in 79% of the 141 patients with pancreatic head adenocarcinoma. Roder et al.35 stated that seven cases with pancreaticoduodenectomy with VR showed no survival benefit because of high incidence of positive surgical margin (71%) and of limited survival of less than 12 months. Tashiro et al.7 reported two patients who had widespread nodal disease and died of tumor recurrence at 3 and 25 months after surgery, respectively. In gallbladder carcinoma and middle-distal cholangiocarcinoma, lymph node metastasis and surgical margin status are well-established prognostic factors.50,51 Adjuvant chemotherapy after aggressive surgery seems to be a practical and promising strategy that can improve the prognosis,52 but the indication of an extensive surgery with vascular procedure is limited when tumors have obvious negative prognostic predictors.
Portal Vein Involvement in Pancreatic and Biliary Tract Carcinoma
In gallbladder carcinoma, portal vein involvement occurs in the far advancing margin of tumor extension, and true vascular invasion is seen more frequently compared to hilar cholangiocarcinoma.9 In surgery for advanced gallbladder carcinoma, we seldom encounter solitary portal vein involvement, and multiple visceral resections are required for tumor resection. In middle and distal cholangiocarcinoma, tumors with deep invasion were associated with poor prognosis compared with those with superficial invasion.53 Furthermore, the depth of invasion of the primary tumor correlated well with patient survival in middle and distal cholangiocarcinoma, whereas it did not in hilar lesion.54 Considering these biological characteristics, portal vein invasion in these lesions should be regarded as the depth of invasion of the primary tumor. In DGC, the clinical requirement of VR itself is thought to represent a high malignant potential with the primary tumor.
Both in HIC and in PHC, VR was associated with no survival disadvantage in cases of tumor infiltration within the tunica adventitia of vein. The superior mesenteric vein, portal vein, or its tributaries run closely across the pancreatic head and proximal bile duct, and these veins are in direct contact with pancreatic parenchyma or with structures of porta hepatis, respectively. Because of this anatomical proximity, the vein can be regarded as a regional vessel of “porta hepatic” or “pancreatic head.” Hence, the tumorous infiltration up to the most superficial layer of the vein does not seem to show strong impact on survival.
Conclusions
The superior mesenteric-portal vein resection combined with major hepatectomy, pancreaticoduodenectomy, or both was technically feasible without complications specific to vascular procedures. However, surgery with portal vein resection for middle-distal cholangiocarcinoma and gallbladder carcinoma was accompanied by a dismal outcome; these operations should not be recommended for lesions with obvious noncurative factors. In hilar cholangiocarcinoma and pancreatic head carcinoma, the vein resection is not contraindicated because of minimal adverse effects on postoperative outcome. In the pancreatic and biliary tract adenocarcinoma, surgical outcomes after aggressive surgery with VR differed considerably, depending on the sites of the primary tumor. It is suggested that difference in the anatomical relationship between the primary tumor and superior mesenteric-portal vein is a probable reason for the explanation of variance in surgical outcome after vein resection.
References
Nimura Y, Hayakawa N, Kamiya J, Maeda S, Kondo S, Yasui A, Shionoya S. Combined portal vein and liver resection for carcinoma of the biliary tract. Br J Surg. 1991;78:727–731.
Ebata T, Nagino M, Kamiya J, Uesaka K, Nagasaka T, Nimura Y. Hepatectomy with portal vein resection for hilar cholangiocarcinoma: audit of 52 consecutive cases. Ann Surg. 2003;238:720–727.
Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, Wex C, Lobeck H, Hintze R. Extended resections for hilar cholangiocarcinoma. Ann Surg. 1999;230:808–818.
Neuhaus P, Jonas S, Settmacher U, Thelen A, Benckert C, Lopez-Hänninen E, Hintze RE. Surgical management of proximal bile duct cancer: extended right lobe resection increases resectability and radicality. Langenbecks Arch Surg. 2003;388:194–200.
Kondo S, Hirano S, Ambo Y, Tanaka E, Okushiba S, Morikawa T, Katoh H. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: results of a prospective study. Ann Surg. 2004;240:95–101.
Hemming AW, Reed AI, Fujita S, Foley DP, Howard RJ. Surgical management of hilar cholangiocarcinoma. Ann Surg. 2005;241:693–699.
Tashiro S, Uchino R, Hiraoka T, Tsuji T, Kawamoto S, Saitoh N, Yamasaki K, Miyauchi Y. Surgical indication and significance of portal vein resection in biliary and pancreatic cancer. Surgery. 1991;109:481–487.
Shimada H, Endo I, Sugita M, Masunari H, Fujii Y, Tanaka K, Misuta K, Sekido H, Togo S. Hepatic resection combined with portal vein or hepatic artery reconstruction for advanced carcinoma of the hilar bile duct and gallbladder. World J Surg. 2003;27:1137–1142.
Kondo S, Nimura Y, Kamiya J, Nagino M, Kanai M, Uesaka K, Yuasa N, Sano T, Hayakawa N. Factors influencing postoperative hospital mortality and long-term survival after radical resection for stage IV gallbladder carcinoma. World J Surg. 2003;27:272–277.
Fortner JG, Kim DK, Cubilla A, Turnbull A, Pahnke LD, Shils ME. Regional pancreatectomy: en bloc pancreatic, portal vein and lymph node resection. Ann Surg. 1977;186:42–50.
Ishikawa O, Ohigashi H, Imaoka S, Furukawa H, Sasaki Y, Fujita M, Kuroda C, Iwanaga T. Preoperative indications for extended pancreatectomy for locally advanced pancreas cancer involving the portal vein. Ann Surg. 1992;215:231–236.
Nakao A, Harada A, Nonami T, Kaneko T, Inoue S, Takagi H. Clinical significance of portal invasion by pancreatic head carcinoma. Surgery. 1995;117:50–55.
Fuhrman GM, Leach SD, Staley CA, Cusack JC, Charnsangavej C, Cleary KR, El-Naggar AK, Fenoglio CJ, Lee JE, Evans DB. Rationale for en bloc vein resection in the treatment of pancreatic adenocarcinoma adherent to the superior mesenteric-portal vein confluence. Pancreatic Tumor Study Group. Ann Surg. 1996;223:154–162.
Carrere N, Sauvanet A, Goere D, Kianmanesh R, Vullierme MP, Couvelard A, Ruszniewski P, Belghiti J. Pancreaticoduodenectomy with mesentericoportal vein resection for adenocarcinoma of the pancreatic head. World J Surg. 2006;30:1526–1535.
van Geenen RC, ten Kate FJ, de Wit LT, van Gulik TM, Obertop H, Gouma DJ. Segmental resection and wedge excision of the portal or superior mesenteric vein during pancreatoduodenectomy. Surgery. 2001;129:158–163.
Hartel M, Niedergethmann M, Farag-Soliman M, Sturm JW, Richter A, Trede M, Post S. Benefit of venous resection for ductal adenocarcinoma of the pancreatic head. Eur J Surg. 2002;168:707–712.
Henne-Bruns D, Vogel I, Luttges J, Kloppel G, Kremer B. Surgery for ductal adenocarcinoma of the pancreatic head: staging, complications, and survival after regional versus extended lymphadenectomy. World J Surg. 2000;24:595–601.
Tseng JF, Raut CP, Lee JE, Pisters PW, Vauthey JN, Abdalla EK, Gomez HF, Sun CC, Crane CH, Wolff RA, Evans DB. Pancreaticoduodenectomy with vascular resection: margin status and survival duration. J Gastrointest Surg. 2004;8:935–949.
Capussotti L, Massucco P, Ribero D, Viganò L, Muratore A, Calgaro M. Extended lymphadenectomy and vein resection for pancreatic head cancer: outcomes and implications for therapy. Arch Surg. 2003;138:1316–1322.
Nakagohri T, Kinoshita T, Konishi M, Inoue K, Takahashi S. Survival benefits of portal vein resection for pancreatic cancer. Am J Surg. 2003;186:149–153.
Sasson AR, Hoffman JP, Ross EA, Kagan SA, Pingpank JF, Eisenberg BL. En bloc resection for locally advanced cancer of the pancreas: is it worthwhile? J Gastrointest Surg. 2002;6:147–157.
Bachellier P, Nakano H, Oussoultzoglou PD, Weber JC, Boudjema K, Wolf PD, Jaeck D. Is pancreaticoduodenectomy with mesentericoportal venous resection safe and worthwhile? Am J Surg. 2001;182:120–129.
Shibata K, Matsumoto T, Yada K, Sasaki A, Ohta M, Kitano S. Factors predicting recurrence after resection of pancreatic ductal carcinoma. Pancreas. 2005;31:69–73.
Leach SD, Lee JE, Charnsangavej C, Cleary KR, Lowy AM, Fenoglio CJ, Pisters PW, Evans DB. Survival following pancreaticoduodenectomy with resection of the superior mesenteric-portal vein confluence for adenocarcinoma of the pancreatic head. Br J Surg. 1998;85:611–617.
Riediger H, Makowiec F, Fischer E, Adam U, Hopt UT. Postoperative morbidity and long-term survival after pancreaticoduodenectomy with superior mesenterico-portal vein resection. J Gastrointest Surg. 2006;10:1106–1115.
Fukuda S, Oussoultzoglou E, Bachellier P, Rosso E, Nakano H, Audet M, Jaeck D. Significance of the depth of portal vein wall invasion after curative resection for pancreatic adenocarcinoma. Arch Surg. 2007;142:172–179.
Takahashi S, Ogata Y, Tsuzuki T. Combined resection of the pancreas and portal vein for pancreatic cancer. Br J Surg. 1994;81:1190–1193.
Shimada K, Sano T, Sakamoto Y, Kosuge T. Clinical implications of combined portal vein resection as a palliative procedure in patients undergoing pancreaticoduodenectomy for pancreatic head carcinoma. Ann Surg Oncol. 2006;13:1569–1578.
Makowiec F, Post S, Saeger HD, Senninger N, Becker H, Betzler M, Buhr HJ, Hopt UT. Current practice patterns in pancreatic surgery: results of a multi-institutional analysis of seven large surgical departments in Germany with 1454 pancreatic head resections, 1999 to 2004 (German Advanced Surgical Treatment study group). J Gastrointest Surg. 2005;9:1080–1086.
Howard TJ, Villanustre N, Moore SA, DeWitt J, LeBlanc J, Maglinte D, McHenry L. Efficacy of venous reconstruction in patients with adenocarcinoma of the pancreatic head. J Gastrointest Surg. 2003;7:1089–1095.
Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BSJ, Youssef BAM, Klimstra D, Blumgart LH. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 2001;234:507–517.
Launois B, Stasik C, Bardaxoglou E, Meunier B, Campion JP, Greco L, Sutherland F. Who benefits from portal vein resection during pancreaticoduodenectomy for pancreatic cancer? World J Surg. 1999;23:926–929.
Kawasaki S, Imamura H, Kobayashi A, Noike T, Miwa S, Miyagawa S. Results of surgical resection for patients with hilar bile duct cancer: application of extended hepatectomy after biliary drainage and hemihepatic portal vein embolization. Ann Surg. 2003;238:84–92.
Seyama Y, Kubota K, Sano K, Takayama T, Kosuge T, Makuuchi M. Long-term outcome of extended hemihepatectomy for hilar bile duct cancer with no mortality and high survival rate. Ann Surg. 2003;238:73–83.
Roder JD, Stein HJ, Siewert JR. Carcinoma of the periampullary region: who benefits from portal vein resection? Am J Surg. 1996;171:170–174.
Lang H, Sotiropoulos GC, Fruhauf NR, Domland M, Paul A, Kind EM, Malago M, Broelsch CE. Extended hepatectomy for intrahepatic cholangiocellular carcinoma (ICC): when is it worthwhile? Single center experience with 27 resections in 50 patients over a 5-year period. Ann Surg. 2005;241:134–143.
Misuta K, Shimada H, Miura Y, Kunihiro O, Kubota T, Endo I, Sekido H, Togo S. The role of splenomesenteric vein anastomosis after division of the splenic vein in pancreatoduodenectomy. J Gastrointest Surg. 2005;9:245–253.
Imaizumi T, Hanyu F, Harada N, Hatori T, Fukuda A. Extended radical Whipple resection for cancer of the pancreatic head: operative procedure and results. Dig Surg. 1998;15:299–307.
Klempnauer J, Ridder GJ, Bektas H, Hatori T, Fukuda A. Extended resections of ductal pancreatic cancer—impact on operative risk and prognosis. Oncology. 1996;53:47–53.
Imamura M, Doi R, Imaizumi T, Funakoshi A, Wakasugi H, Sunamura M, Ogata Y, Hishinuma S, Asano T, Aikou T, Hosotani R, Maetani S. A randomized multicenter trial comparing resection and radiochemotherapy for resectable locally invasive pancreatic cancer. Surgery. 2004;136:1003–1011.
Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Shimizu Y, Kato A, Nakamura S, Omoto H, Nakajima N, Kimura F, Suwa T. Aggressive surgical approaches to hilar cholangiocarcinoma: hepatic or local resection? Surgery. 1998;123:131–136.
Imamura H, Shimada R, Kubota M, Matsuyama Y, Nakayama A, Miyagawa S, Makuuchi M, Kawasaki S. Preoperative portal vein embolization: an audit of 84 patients. Hepatology. 1999;29:1099–1105.
Nagino M, Kamiya J, Nishio H, Ebata T, Arai T, Nimura Y. Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer: surgical outcome and long-term follow-up. Ann Surg. 2006;243:364–372.
Kondo S, Katoh H, Hirano S, Ebata T, Arai T, Nimura Y. Portal vein resection and reconstruction prior to hepatic dissection during right hepatectomy and caudate lobectomy for hepatobiliary cancer. Br J Surg. 2003;90:694–697.
Sakaguchi S, Nakamura S. Surgery of the portal vein in resection of cancer of the hepatic hilus. Surgery. 1986;99:344–349.
Sakamoto Y, Kosuge T, Shimada K, Sano T, Ojima H, Yamamoto J, Yamasaki S, Takayama T, Makuuchi M. Prognostic factors of surgical resection in middle and distal bile duct cancer: an analysis of 55 patients concerning the significance of ductal and radial margins. Surgery. 2005;137:396–402.
Sasaki R, Takahashi M, Funato O, Nitta H, Murakami M, Kawamura H, Suto T, Kanno S, Saito K. Prognostic significance of lymph node involvement in middle and distal bile duct cancer. Surgery. 2001;129:677–683.
Kayahara M, Nagakawa T, Ohta T, Kitagawa H, Tajima H, Miwa K. Role of nodal involvement and the periductal soft-tissue margin in middle and distal bile duct cancer. Ann Surg. 1999;229:76–83.
Yoshida T, Matsumoto T, Sasaki A, Morii Y, Aramaki M, Kitano S. Prognostic factors after pancreatoduodenectomy with extended lymphadenectomy for distal bile duct cancer. Arch Surg. 2002;137:69–73.
Tsukada K, Kurosaki I, Uchida K, Shirai Y, Oohashi Y, Yokoyama N, Watanabe H, Hatakeyama K. Lymph node spread from carcinoma of the gallbladder. Cancer. 1997;80:661–667.
Kurosaki I, Tsukada K, Hatakeyama K, Muto T. The mode of lymphatic spread in carcinoma of the bile duct. Am J Surg. 1996;172:239–243.
Kelley ST, Bloomston M, Serafini F, Carey LC, Karl RC, Zervos E, Goldin S, Rosemurgy P, Rosemurgy AS. Cholangiocarcinoma: advocate an aggressive operative approach with adjuvant chemotherapy. Am Surg. 2004;70:743–748.
Hong SM, Kim MJ, Cho H, Pi DY, Jo D, Yu E, Ro JY. Superficial vs. deep pancreatic parenchymal invasion in the extrahepatic bile duct carcinomas: a significant prognostic factor. Mod Pathol. 2005;18:969–975.
Hasebe T, Konishi M, Iwasaki M, Endoh Y, Nakagohri T, Takahashi S, Kinoshita T, Ochiai A. Histological characteristics of tumor cells and stromal cells in vessels and lymph nodes are important prognostic parameters of extrahepatic bile duct carcinoma: a prospective study. Hum Pathol. 2005;36:655–664.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kurosaki, I., Hatakeyama, K., Minagawa, M. et al. Portal Vein Resection in Surgery for Cancer of Biliary Tract and Pancreas: Special Reference to the Relationship Between the Surgical Outcome and Site of Primary Tumor. J Gastrointest Surg 12, 907–918 (2008). https://doi.org/10.1007/s11605-007-0387-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0387-5