Abstract
Purpose
Nowadays, surgical excision is no longer justified for all B3 lesions and a minimally-invasive therapeutic treatment has been encouraged. The aim of this study was to evaluate the feasibility and the therapeutic efficacy of ultrasound-guided vacuum-assisted excision (US-VAE) for the treatment of selected breast lesions of uncertain malignant potential (B3).
Material and methods
From July 2018 to December 2019, 11/48 breast lesions classified as B3 after ultrasound-guided core needle biopsy were treated with US-VAE in our Institution. Inclusion criteria were: B3 nodules ultrasonographically detectable for which VAE is recommended by international guidelines2, size ranging between 5 and 25 mm, circumscribed margins, and lesion position at least 5 mm from the skin and the nipple. A radiological follow-up to evaluate the completeness of excision, the presence of post-procedural hematoma or of residual disease/recurrence was performed after 10 and 30 days and 6 and 12 months. 12-month ultrasound was considered the gold standard. All patients were asked to complete a satisfaction survey and a full assessment of the costs of US-VAE was performed.
Results
Complete excision was achieved in 81.8% of US-VAE. No lesions were upgraded to carcinoma and no patients had to undergo surgery. No complications occurred during or after US-VAE. All patients were satisfied with the procedure and the cosmetic result (100%). US-VAE cost approximately 422 Euros per procedure.
Conclusion
US-VAE has proven to be an optimal tool for the therapeutic excision of selected B3 lesions, with high success rate, good patient compliance and considerable money savings compared to surgery. This technique has the potential to reduce unnecessary surgery and healthcare costs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Lesions of uncertain malignant potential in the breast (B3 lesions) correspond to a heterogeneous group of diagnostic entities that may present benign histology on percutaneous biopsy but with an increased risk of associated malignancy (9.9–35.1%) [1, 2]. B3 lesions represent approximately 3–21% of all breast lesions, although their incidence varies among countries [3, 4].
The lesions more frequently included into B3 category are: atypical ductal hyperplasia (ADH), flat epithelial atypia (FEA), classical lobular neoplasia (LN), papillary lesions (PL), phyllodes tumor (PT), and radial scars (RS)/complex sclerosing lesions (CSL).
These lesions are considered as risk factors or non-obligate precursors of malignancy, since they can upgrade into ductal carcinoma in situ (DCIS) and low-grade invasive tumors [3]. The overall positive predictive value for breast cancer is around 25% [5], with the level of risk varying for the different B3 entities. In particular, the upgrade rate to malignancy is significantly associated with the presence of atypia: for this reason they are further classified into B3a and B3b depending on the absence or presence of atypia (upgrade rate of 4.8–7% and 24–36%, respectively) [6,7,8].
Because of the association with malignancy, the traditional approach to this kind of lesions was surgical excision. With the advent of vacuum assisted biopsy (VAB), however, VAB devices have been proposed and increasingly used as a safe and effective alternative to surgery for the therapeutic removal of benign breast lesions [9, 10]. VAB devices allow to obtain multiple and contiguous tissue samples with a single needle introduction [10]. Vacuum-assisted excision (VAE) uses the same method to remove entire lesions, providing large amounts of tissue, comparable to that of a surgical excision specimen (approximately 4 g ) [11, 12].
As a consequence, it was suggested that VAE (under ultrasound or stereotactic guidance) might be a sufficient treatment of B3 breast lesions and in 2018 the Second International Consensus Conference on lesions of uncertain malignant potential in the breast [2] recommendations established that VAE is an appropriate alternative to first-line open excision in most B3 lesions, with reduced complications, good cosmetic results and healthcare costs savings.
In this scenario, the aim of this preliminary study was to evaluate the feasibility and the therapeutic efficacy of ultrasound-guided VAE (US-VAE) for the treatment of selected B3 breast lesions in our Institution, in terms of incidence of complete removal of the lesion, complication rate, patient satisfaction and money saving.
Materials and methods
Study population
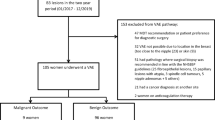
From July 2018 to December 2019, out of 652 breast ultrasound-guided core needle biopsies (CNB) performed in our Institution, 48 breast lesions were classified as B3.
Inclusion criteria for the US-VAE procedure were: B3 breast nodules well detectable at ultrasound examination (US) with circumscribed or slightly indistinct margins, size ranging between 5 and 25 mm, and localized at least 5 mm from the skin, the nipple or the pectoralis muscle. Consequently, the number of lesions suitable for the procedure was 37.
B3 lesions characterized by high-risk features for which international guidelines [2] recommend surgical excision, patients with previous or current history of cancer, and cases of incomplete imaging or histological information were excluded.
All cases were discussed during our institutional Breast Unit multidisciplinary meeting prior to offering US-VAE and 4 more patients were excluded because of imaging-histology discrepancy (n = 2) or because a close follow-up program was preferred (n = 2), considering the advanced age of the patients (> 80 years old) (see Fig. 1).
Therefore, 11 lesions were considered for our prospective evaluation of US-VAE procedure.
The study was conducted according to Good Clinical Practice guidelines and obtained the approval of our institutional review board. A dedicated informed consent was signed by every patient.
All patients underwent appropriate coagulation tests and were asked to interrupt any anticoagulant therapy for 3–5 days before the procedure.
US-VAE procedure
All procedures were performed in our Institution by a breast interventional radiologist with more than 15 years of experience, with a 8-Gauge VAB device (Mammotome; Ethicon Endo-surgery, Cincinnati, USA) under US guidance, using a 12 MHz linear probe (SSA-700A; Toshiba, Tokyo, Japan).
The procedure was preceded by a preliminary US to identify the lesion and to find the most comfortable position for both patient and operator. The larger diameter and the distance from the skin were measured for each lesion. Subsequently, 10 ml mepivacaine was injected in the breast segment containing the lesion to induce local anaesthesia and a few millimetres incision was made with a scalpel to facilitate the introduction of the needle. The procedure ended when the lesion was no longer detectable at US or due to intercurrent complications or patient’s request (Fig. 2). A marker clip was released into the procedure site to easily locate it during follow-up. The skin incision was closed using steri-strips, and a manual compression (5–10 min long) followed by a dry ice pack was applied to reduce post-procedural hematoma.
All the specimens were evaluated by an experienced pathologist according to standardized protocols. In case of evidence of malignancy even in a single core the patient would have been referred for surgery in order to perform a wider excision.
Finally, the costs of US-VAE were calculated.
Satisfaction survey and follow-up
10 days after US-VAE patients were invited to complete an evaluation survey to assess the degree of personal satisfaction with the procedure and the cosmetic result, to investigate the pain felt during treatment, the requirement for analgesic or antibiotic therapy, and the presence of bruising or residual palpable lesions. Finally, each patient was asked if she would recommend US-VAE and if she would choose this procedure again (Fig. 3).
The follow-up program, to evaluate possible post-procedural hematoma (or other fluid collection), residual or recurrent disease, included: physical examination and breast US 10 and 30 days after the procedure; physical examination, breast US and mammography 6 and 12 months after.
Hematoma was considered significant if greater than 3 cm [13]. The detection of new nodules in the region of previous excision was classified as recurrent disease.
In 6 cases the radiological follow-up continued for up to 24 months (mean = 16.9 months, SD = 5.0).
Clinical and pathological results of US-VAE were compared to 12-month US follow-up that was considered the gold standard.
Results
A total of 11 US-VAE procedures were performed for as many B3 breast lesions over a period of 18 months (see Table 1). The lesions included 5 PL without atypia (45.4%), 3 FEA (27.3%), 2 RS (18.2%), and 1 CSL (9.1%). Mean age at diagnosis was 53.9 years (SD = 11.4; range 41–82 years).
All the lesions appeared at US as hypoechoic masses, with regular or slightly indistinct margins. Lesions’ maximum size ranged between 5 and 21 mm (mean = 12.4 mm, SD = 5.2). The distance from the skin ranged between 5 and 16 mm (mean = 7.9 mm, SD = 3.0). The number of cores collected for each patient varied from 3 to 8 (mean = 4.8 cores, SD = 1.6), based on lesion size. Samples had a mean size of 18 × 3 mm (length × diameter). The duration of the entire procedure was about 25 min (mean = 25.6 min, SD = 6.3; range 17–35 min).
The procedure was completed without interruptions in all patients except 1 (9.1%), who asked to stop it prematurely.
A complete lesion removal after VAE occurred in 81.8% of cases (9/11). In 2 cases (18.2%) the excision resulted incomplete, with US evidence of millimetric residual disease.
No lesions were upgraded to DCIS or invasive carcinoma after histological examination and no patients had to undergo surgery after US-VAE.
There were no post-procedural infections.
The first follow-up (10 days after US-VAE) documented the presence of a non-significant post-procedural hematoma in all patients, with a mean size of 14.9 mm (SD = 5.5; range 7–24 mm). 30 days after the procedure the hematoma had spontaneously resolved in 5 cases (45.5%), while in the remaining 6 it was still evident at US but significantly reduced in volume (mean size = 8.5 mm, SD = 3.1; range 5–13). After 6 months post-procedural hematoma was no longer detectable in any patient (Fig. 4).
a US shows a 10 mm hypoechoic nodule (FEA) treated with US-VAE. b 10-day US follow-up shows the hyperechoic marker clip in the middle of a post-procedural hematoma. c 6-month US follow-up confirms the presence of the marker clip in the sampling site (arrow), but neither the lesion nor the hematoma are appreciable
The 2 cases of residual disease remained unchanged in size and morphology during follow-up (12 and 18 months, respectively); imaging surveillance is continuing, anyway.
Neither recurrences in or near the treated area nor significant US or mammographic alteration (e.g. posterior acoustic shadowing, scars or architectural distortions) were observed during follow-up.
No significant skin scars or keloids were seen at clinical examination.
Satisfaction survey
All the questionnaires were administered 10 days after US-VAE.
100% of patients were completely satisfied with the procedure and the cosmetic result.
90.9% of patients reported no or mild pain (score = 1–2/5) during the procedure, 1 patient (9.1%) experienced moderate pain (score = 3/5). 2 patients required analgesic therapy the day after the procedure, while no patient took antibiotics.
Local bruising occurred in all patients (mild in 36.4% of cases, moderate in 45.4%, and severe in 18.2%).
All patients declared that they would recommend the procedure and that they would rather have a further US-VAE than surgical excision.
Cost analysis
The cost of US-VAE was approximately 422 Euros per procedure, including the costs of the Mammotome® device (300 Euros), of the marker clip (112 Euros) and of disposable sanitary and dressing material (about 10 Euros), such as anaesthetic drugs, sterile gloves, scalpels, steri-strips etc.
The staff employed during the procedure included a breast radiologist and a nurse.
Discussion
B3 lesions represent 3–21% of all breast lesions [3, 4] and 4–9% of all CNB results [14] but, although uncommon, their management has always represented a challenge. Due to the uncertain malignant potential associated with this heterogeneous group of breast lesions, open surgery has been recommended over the past years. However, more recent studies have demonstrated that surgical excision is no longer justified for all cases, since the risk of upgrade to malignancy is low and depending on the subcategory of B3 [2, 6, 12, 15]. The First International Consensus Conference on lesions of uncertain malignant potential in the breast [14] recommended VAE (under ultrasound or stereotactic guidance) as the gold standard for the therapeutic management of the majority of B3 lesions. In 2018, the Second International Consensus Conference endorsed those recommendations, confirming that the minimally invasive approach of VAE is a valid alternative method to first-line open surgery in most cases (except ADH, PT [2] and papilloma with atypia [12]). The purpose of VAE is to obtain samplings that are enough representative to exclude the presence of associated malignancy and to remove an amount of tissue comparable to that of a diagnostic surgical biopsy (approximately 4 g) [10,11,12].
At the state of art, there are only few studies regarding the feasibility of US-VAE for the therapeutic excision of B3 nodules [6, 16,17,18,19], since VAE has mostly been used for removing benign breast lesions [20,21,22] or in the second-line excisional treatment of biopsy-proven B3 calcifications [23], and its application to clinical practice varies from country to country.
The success rate of US-VAE for the treatment of B3 lesions has reached 81.8% in our study, and is comparable to that of similar experiences performed on benign breast nodules (70–100%) [9, 13, 19, 24, 25]. As already suggested [9, 13, 17, 20], the effectiveness of the treatment seems to be favoured by the US features of the nodule, the lesion size, and the distance from the skin. Therefore, it is fundamental to consider all these factors before proposing a therapeutic US-VAE. Perretta et al. [17] have affirmed that regular shape, circumscribed margins, and the absence of posterior features at US are significantly associated with a complete excision. Multiple Authors have reported increased rates of residual disease in masses larger than 2.5 cm [13, 17], while they are reduced in nodules < 2 cm, with success rates of 95–100% [9, 20]. Moreover, a too close distance from the skin, the nipple or the pectoralis muscle reduces the manoeuvring space during procedure, with the risk of skin tear and residual disease [13]. These data are in agreement with our experience: in one case of incomplete excision the lesion was too close to the skin (5 mm) while in the other the lump measured 2.1 cm (the biggest of the series) and the procedure was interrupted following the aforementioned patient’s request. However, other studies have not observed a relationship between lesion size and success rate [20, 21].
The use of 8 Gauge-needles guarantees the removal of about 300 mg of tissue (vs. about 100 mg collectable using 11 Gauge-needles) [10, 26] that allows to reduce sampling errors and to decrease the risk of histological underestimation or imaging-histology discrepancy.
Although we have collected less than 4 g of tissue per procedure, most of the lesions treated were small (< 15 mm) and the US-guidance ensured a real-time monitoring of the excisional process until the complete removal of the lesion. Moreover, we did a close follow-up.
In this regard, Perretta et al. [17] have reported high concordance rates between the histological diagnosis on the surgical specimen and the results of US-VAE, highlighting that this technique is associated with a very low risk of underestimation of B3 lesions. Our results support their outcome, since there was no upgrade to DCIS or invasive carcinoma after histological examination and surgery was avoided after US-VAE in cases with no residual disease. Furthermore, no recurrences or suspicious imaging features were observed during follow-up, confirming the substantially low risk of malignancy of these lesions.
In the 2 cases of residual disease, our Breast Unit multidisciplinary team decided to avoid surgery considering the absence of atypia and the fact that the lesions remained unchanged in size and morphology during follow-up (12 and 18 months, respectively); imaging surveillance is still in progress, anyway.
Giannotti and al. [6] did not found malignancies in the 47 B3a lesions (at the initial core biopsy) undergoing VAE included in their study. In their experience 40.7% of women with a B3 lesion were suitable for a mini-invasive VAE than an open surgical biopsy.
A reported advantage of VAE is the considerable money and time saving compared to surgery. Alonso-Bartolome et al. [27] have reported that the costs related to VAE are 82% lower than a surgical biopsy. We found that the overall cost of US-VAE is approximately 20% of that of a classic excisional biopsy of a B3 lesion (for which the costs related to the operating room and the significant number of health workers involved must be considered), with a net saving of about 1900 Euros per procedure, in our Institution. However, costs may vary among countries. In our experience, the overall procedure was completed in about 25 min. Other Authors have reported a similar duration (range = 20–30 min) [13, 17, 18, 20, 22].
US-VAE is a minimally invasive procedure with excellent aesthetic results and minimal side effe cts. As documented by our experience, all patients were completely satisfied with the procedure and the cosmetic result, with a reduction of psychological impact. The appearance of post-procedure local bruising was expectable and self-limiting, as for the standard VAB.
The main disadvantages of VAE are an incomplete excision, that has been associated with 2–38% of procedures [20], and the segmentation of the specimen collected that does not allow the same pathological assessments as surgical samples (e.g. the evaluation of the exeresis margins) [28]. Lee et al. [19] detected 12.7% residual nodules and 2.3% recurrences on 910 VAE-treated benign lesions, while another study including 51 fibroadenomas showed residual disease in 19% of patients [20]. Perretta et al. [17] reported 6.3% incomplete excision on 63 B3 lesions. These results are consistent with ours (residual disease = 18.2%, no recurrences), although based on a small population.
The operator's experience seems to be directly related to the success rate [17].
Considering this was a pilot study, we decided to do a close follow-up, although not necessary in routine clinical practice where an annual mammography should be sufficient as others Authors have suggested [12].
In our experience US-VAE has proven to be a valid and safe mini-invasive procedure for the therapeutic treatment of selected B3 lesions, with excellent outcomes in terms of efficacy and exceptionally well tolerated by patients.
In spite of the interesting results, our main limitation is certainly the small cohort of patients, even if, as already mentioned, B3 lesions represent less that 10% of all CNB results [14, 28] and only selected subcategories are eligible for VAE. In addition, suitable cases must be discussed within a multidisciplinary team and approved, and the number of patients included in other similar studies was not much different [16, 18]. Moreover, no direct comparison was made between US-VAE and surgery, to avoid overtreatment [2], and residual disease was assessed ultrasonographically and not histologically.
In conclusion, US-VAE has demonstrated to be a valid and safe technique for the therapeutic excision of selected B3 lesions, showing high accuracy and high success rates. As a consequence, this procedure should be promoted during multidisciplinary meetings, as it has the potential to reduce unnecessary open surgery and the associated risks, and offers the significant advantage of decreasing healthcare costs. Moreover, US-VAE has a lower aesthetic and psychological impact and is well tolerated by patients. Complete excision rates seem to depend on US features, size and localization of the lesion, therefore these factors should be considered before proposing a therapeutic US-VAE.
Further multi-institutional studies are needed to validate our results.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
HNSBCS and the Royal College of Pathologist guidelines for non-operative procedures and reporting in breast cancer screening (2017). https://www.rcpath.org/uploads/assets/4b16f19c-f7bd-456c-b212f557f8040f66/G150-Non-op-reporting-breast-cancer-screening-Feb17.pdf. Accessed 10 Feb 2021.
Rageth CJ, O’Flynn EAM, Pinker K et al (2019) Second international consensus conference on lesions of uncertain malignant potential in the breast (B3 lesions). Breast Cancer Res Treat 174:279–296. https://doi.org/10.1007/s10549-018-05071-1
Catanzariti F, Avendano D, Cicero G et al (2021) High-risk lesions of the breast: concurrent diagnostic tools and management recommendations. Insights Imaging 12(1):63. https://doi.org/10.1186/s13244-021-01005-6
Shaaban AM, Sharma N (2019) Management of B3 lesions-practical issues. Curr Breast Cancer Rep 11:83–88. https://doi.org/10.1007/s12609-019-0310-6
Documento di consenso sulle procedure diagnostiche preoperatorie nelle lesioni mammarie (2016) GISMa Gruppo Italiano Screening Mammografico.
Giannotti E, James JJ, Chen Y et al (2021) Effectiveness of percutaneous vacuum-assisted excision (VAE) of breast lesions of uncertain malignant potential (B3 lesions) as an alternative to open surgical biopsy. Eur Radiol. https://doi.org/10.1007/s00330-021-08060-z
Rakha EA, Lee AHS, Jenkins JA et al (2011) Characterization and outcome of breast needle core biopsy diagnoses of lesions of uncertain malignant potential (B3) abnormalities detected by mammographic screening. Int J Cancer 129:1417–1424. https://doi.org/10.1002/ijc.25801
Mayer S, Kayser G, Rucker G et al (2017) Absence of epithelial atypia in B3-lesions of the breast is associated with decreased risk of malignancy. Breast 31:144–149. https://doi.org/10.1016/j.breast.2016.11.007
Bennett IC (2017) The changing role of vacuum-assisted biopsy of the breast: a new prototype of minimally invasive breast surgery. Clin Breast Cancer 17:323–325. https://doi.org/10.1016/j.clbc.2017.03.001
Bennett IC, Saboo A (2019) The evolving role of vacuum assisted biopsy of the breast: a progression from fine-needle aspiration biopsy. World J Surg 43:1054–1061. https://doi.org/10.1007/s00268-018-04892-x
O’Flynn EA, Wilson AR, Michell MJ (2010) Image-guided breast biopsy: state-of-the-art. Clin Radiol 65:259–270. https://doi.org/10.1016/j.crad.2010.01.008
Pinder SE, Shaaban A, Deb R et al (2018) NHS Breast Screening multidisciplinary working group guidelines for the diagnosis and management of breast lesions of uncertain malignant potential on core biopsy (B3 lesions). Clin Radiol 73:682–692. https://doi.org/10.1016/j.crad.2018.04.004
Salazar JP, Miranda I, de Torres J et al (2019) Percutaneous ultrasound-guided vacuum-assisted excision of benign breast lesions: a learning curve to assess outcomes. Br J Radiol 92:20180626. https://doi.org/10.1259/bjr.20180626
Rageth CJ, O’Flynn EA, Comstock C et al (2016) First international consensus conference on lesions of uncertain malignant potential in the breast (B3 lesions). Breast Cancer Res Treat 159:203–213. https://doi.org/10.1007/s10549-016-3935-4
Lucioni M, Rossi C, Lomoro P et al (2021) Positive predictive value for malignancy of uncertain malignant potential (B3) breast lesions diagnosed on vacuum-assisted biopsy (VAB): is surgical excision still recommended? Eur Radiol 31:920–927. https://doi.org/10.1007/s00330-020-07161-5
Tennant SL, Evans A, Hamilton LJ et al (2008) Vacuum-assisted excision of breast lesions of uncertain malignant potential (B3)-an alternative to surgery in selected cases. Breast 17:546–549. https://doi.org/10.1016/j.breast.2008.08.005
Perretta T, Lamacchia F, Ferrari D et al (2020) Evaluation of ultrasound-guided 8-Gauge vacuum-assisted excision system for the removal of US-detectable breast lesions. Anticancer Res 40:1719–1729. https://doi.org/10.21873/anticanres.14125
Ko KH, Jung HK, Youk JH et al (2012) Potential application of ultrasound-guided vacuum-assisted excision for well-selected intraductal papillomas of the breast: single-institutional experiences. Ann Surg Oncol 19:908–913. https://doi.org/10.1245/s10434-011-2050-3
Lee SH, Kim EK, Kim MJ et al (2014) Vacuum-assisted breast biopsy under ultrasonographic guidance: analysis of a 10-year experience. Ultrasonography 33:259–266. https://doi.org/10.14366/usg.14020
Buğdaycı O, Kaya H, Arıbal E (2017) Ultrasound guided therapeutic excisional vacuum-assisted biopsy in breast fibroadenomas. J Breast Health 13:74–76. https://doi.org/10.5152/tjbh.2017.3038
Thurley P, Evans A, Hamilton L et al (2009) Patient satisfaction and efficacy of vacuum-assisted excision biopsy of fibroadenomas. Clin Radiol 64:381–385. https://doi.org/10.1016/j.crad.2008.09.013
Shang QJ, Li N, Zhang MK et al (2020) Ultrasound-guided vacuum-assisted excisional biopsy to treat benign phyllodes tumors. Breast 49:242–245. https://doi.org/10.1016/j.breast.2019.12.008
McMahon MA, Haigh I, Chen Y et al (2020) Role of vacuum-assisted excision in minimising overtreatment of ductal atypias. Eur J Radiol 131:109258. https://doi.org/10.1016/j.ejrad.2020.109258
Fine RE, Boyd BA, Whitworth PW et al (2002) Percutaneous removal of benign breast masses using a vacuum-assisted handheld device with ultrasound guidance. Am J Surg 184:332–336. https://doi.org/10.1016/s0002-9610(02)00951-0
Kim MJ, Park BW, Kim SI et al (2010) Long-term follow-up results for ultrasound-guided vacuum-assisted removal of benign palpable breast mass. Am J Surg 199:1–7. https://doi.org/10.1016/j.amjsurg.2008.11.037
Povoski SP, Jimenez RE (2007) A comprehensive evaluation of the 8-gauge vacuum-assisted Mammotome® system for ultrasound-guided diagnostic biopsy and selective excision of breast lesions. World J Surg Oncol 5:83. https://doi.org/10.1186/1477-7819-5-83
Alonso-Bartolome P, Vega-Bolıvar A, Torres-Tabanera M et al (2004) Sonographically-guided 11-G directional vacuum-assisted breast biopsy as an alternative to surgical excision: utility and cost study in probably benign lesions. Acta Radiol 45:390–396. https://doi.org/10.1080/02841850410005633
Park HL, Hong J (2014) Vacuum-assisted breast biopsy for breast cancer. Gland Surg 3:120–127. https://doi.org/10.3978/j.issn.2227-684X.2014.02.03
Funding
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Giovanna Panzironi, Giuliana Moffa and Federica Pediconi. The first draft of the manuscript was written by Giovanna Panzironi and Giuliana Moffa and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All procedures performed were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study. Verbal informed consent was obtained prior to the satisfaction interview.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Panzironi, G., Moffa, G., Galati, F. et al. Ultrasound-guided 8-Gauge vacuum-assisted excision for selected B3 breast lesions: a preliminary experience. Radiol med 127, 57–64 (2022). https://doi.org/10.1007/s11547-021-01429-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-021-01429-6