Abstract
Purpose
The aim of our study was to evaluate factors influencing effectiveness of percutaneous microwave ablation (MWA) in patients with small hepatocellular carcinoma (HCC) (<3 cm).
Materials and methods
Between December 2007 and August 2015, 49 patients with 65 previously histological typed HCC were treated in a total of 61 sessions. Tumours were subdivided into central (>3 cm from the capsule) (n = 22) and peripheral (<3 cm from the capsule) (n = 43). Imaging follow-up was performed at 1, 3, 6, and 12 months after treatment, then annually. Mean follow-up period was 18 months (range 1–55). Location of the lesion, age, sex, and underlying disease of the patients was analyzed and related with efficacy.
Results
Technical success was obtained in all cases. Residual disease was registered in 21 lesions (32.3 %): 13 were peripheral and 8 were central. Twelve of them were retreated with percutaneous MWA. Local recurrence was recorded in 8 lesions (12.3 %): 5 were retreated with MWA. No significant difference in terms of effectiveness was observed in lesions located in a central position and those situated in the peripheral position. Age, sex, and underlying disease not influenced results. Only one major complication was observed. The rate of minor complications was 24.5 %. Mortality at 30 days was 0 %.
Conclusions
Our results encourage the role of MWA in the treatment of small HCC. More numerous series and randomized studies are necessary to state the role of MWA and to select cases in which MWA may be more effective and safer than RFA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Surgical resection and liver transplantation remain the most effective treatment strategies for small and oligonodular (five or fewer intrahepatic lesions) hepatocellular carcinomas (HCCs) [1].
However, surgical resection is only suitable for 9–27 % of patients with HCC because of their poor hepatic reserve due to the underlying chronic liver disease with significant portal hypertension and abnormal bilirubin levels [1]. Percutaneous local ablation (PLA) is being increasingly used in treatment of HCC not candidates for surgical intervention [2]. Due to selective ablation of liver tissue, PLA does not have the morbidity and mortality associated other major surgical procedures [2]. The indications for PLA includes HCC in BCLC A and B stages with Child–Pugh class A/B cirrhosis, an ECOG performance status of 0–1, tumour <5 cm (ideal < 3 cm), focal nodular lesion, solitary or multiple lesions [3].
Radiofrequency ablation (RFA) is now the most commonly utilized ablation technique worldwide [2].
Microwave ablation (MWA) is becoming increasingly popular. MWA has the advantages of having a higher thermal efficiency and is relatively a fast procedure. There is less heat sink effect. These factors yield a large ablation volume, and result in good local control and fewer complications [2]. In this study, different factors, including patients and tumours characteristics, and clinicopathologic factors, were analyzed and related with the outcomes. Therefore, the aim was to assess which factors might be used to predict the effectiveness of percutaneous MWA of small HCC.
Materials and methods
Informed consent was obtained from all patients, before each procedure. The Internal Review Board approved the study.
Between December 2007 and August 2015, 49 patients (38 men, 11 women), mean age years 71.8 (range 49–85), underwent percutaneous microwave ablation (MWA) of 65 HCC with a mean diameter of 2.04 cm (range 0.8–3 cm) (Table 1).
The inclusion criteria for percutaneous MWA treatment were age ≥18 y.o., hepatocellular carcinoma confirmed by an histologic report, tumours judged inoperable after surgical evaluation, HCC classified by Barcelona Clinic Liver Cancer (BCLC) Criteria as A and B stages with Child–Pugh class A/B cirrhosis, and on the basis of Eastern Cooperative Oncology Group (ECOG) patients with performance status of 0–1, focal nodular lesion, solitary or multiple lesions (≤3) [4, 5], normal coagulation parameters, patients refusing surgery, comorbidities (severe cardiovascular and/or respiratory diseases), and percutaneous accessibility.
The exclusion criteria were age ≤18 y.o., a known or suspected pregnancy, presence of vascular invasion, extrahepatic metastatic disease, sepsis, severe debilitation, Child–Pugh class C cirrhosis, uncorrectable coagulopathy abnormal results, or a tumour that was not accessible percutaneously. In all cases, an interventional radiologist (with more than 10 years of experience) evaluated the percutaneous accessibility of the tumours.
Metastatic HCC or lesions previously undergone other treatments were excluded from the study.
Sixty-five lesions were treated; distribution was as follows: central (>3 cm from the capsule) (n = 22) and peripheral (<3 cm from the capsule) (n = 43) (Table 1).
One week prior the ablation treatment, all patients underwent percutaneous biopsy under US guidance (Philips iU22, Best, NL), with histological confirmation for all lesions.
Indications, risks, and benefits of the procedure were discussed with all patients prior to treatment.
Baseline imaging
Pretreatment imaging consisted of an abdomen multi-detector row computed tomography (MDCT) scan (Aquilion 64, Toshiba, Japan) with and without contrast medium administration. Each MDCT scan was acquired with a thickness of 0.5 mm, voltage of 120 kV and tube current of 250 mA. The contrast-enhanced scans were acquired after injection of 100 ml of iodinated contrast agent (Visipaque 320, GE Healthcare, USA) at an injection rate of 3 ml/s, followed by injection of 40 ml saline at a rate of 2 ml/s.
Preoperative treatment
The coagulation profile was in the normal range for all patients. Patients undergoing anticoagulant and/or anti-aggregating therapy interrupted treatment at least 7 days before the procedure, with the introduction of fractionated heparin when necessary.
Complete blood count, serum bilirubin, and liver enzyme levels were performed before and after the treatment.
Adequate antibiotic prophylaxis was achieved with intravenous administration of 1 g of cefazolin sodium (Ancef, SmithKline Beecham Pharmaceuticals, Philadelphia, USA) given every 8 h for 3 days before the procedure till 2 days afterwards.
Percutaneous MWA procedure
MWA was performed with the patient under conscious sedation and analgesia induced by intravenous administration of propofol (0.5–2.0 mg/kg/h), alfentanil (1–2 μg/kg), and midazolam (0.07–0.08 mg/kg) immediately before the treatment. Heart rate, electrocardiographic trace, oxygen saturation, respiratory frequency, and blood pressure were continuously monitored by an anaesthesiologist.
Local anaesthesia at the antenna entrance site was achieved with subcutaneous injection of a 10-ml solution of 2 % Mepivacaine.
Percutaneous MWA was performed under US guidance (Philips iU22, Best, The Netherlands), in six cases associated with CBCT C-arm angiograph (Allura Xper FD20 with flat detector, Philips Medical System, Best, the Netherlands) with a dedicated workstation running guidance and volumetric planning software (XperGuide System, Philips Medical System, Best, the Netherlands).
The ablation system used consists in a microwave generator (EvidentTM MW Ablation System, Covidien Ltd, USA) capable of producing a power of 45 W at 915 MHz, connected by coaxial cable to a 14.5-gauge straight microwave antennas with a total length of 12 or 17 cm (VT 1237 and VT 1737 EvidentTM MW Ablation Percutaneous Antenna, Covidien Ltd, USA) with a 3.7- or 2-cm radiating section. The antennae were continuously perfused with saline solution at room temperature at 60 ml/min to avoid possible thermal damage along the proximal semi-axis of the antenna. According to manufacturer specifications, ablation was performed by inserting the antenna within the lesion and maintaining a power of 45 W for a total ablation time of 10 min to obtain the optimal necrosis volume. All the lesions of our series presented a maximum diameter less than 3 cm; therefore, only one antenna was deployed.
Clinical outcomes: technical success, safety, and efficacy of the technique, analysis of the factors influencing efficacy
Technical success was defined as the correct positioning of the antennae within the lesion.
Safety was defined as the frequency of complications.
All complications were recorded and classified as minor and major, and they were assessed according to CTCAE [6].
Major complications were defined as complications that, if untreated, might threaten the patient’s life, lead to substantial morbidity and disability, result in hospital admission or substantially lengthen hospital stay, as described by the International Working Group of Image Guided Tumour Ablation [7].
Minor complications included typical post-ablation syndrome symptoms (fever, pain, nausea, and vomiting) if present >4 days after the ablation procedure.
Complications were further divided into two causal categories: those secondary to MW antenna placement (pneumothorax, infection, and bleeding) and those secondary to thermal injury (damage to adjacent organs) [8]. Pain was evaluated with a validated visual analogue scale (VAS) for pain assessment and recording any use of analgesics. Moreover, values of laboratory tests (WCC, serum bilirubin, alkaline phosphatase, aspartate aminotransferase, and alanine aminotransferase) were evaluated before and after ablation session.
Efficacy of the technique was defined on the basis of the percentage of residual or recurrence of tumours. Local residual was defined as the presence of vital tissue around (<5 mm) and/or in the contest of treated nodule at CT scan performed at least after 1 month. If indications and risks were until valid, lesions with partial necrosis were treated with a second session of MWA. Local recurrence was defined as the presence of vital tissue around (<5 mm) and/or in the contest of treated nodule at CT scan performed at least after 3 months.
The effectiveness of the technique was evaluated on the basis of imaging characteristics, using RECIST criteria [9].
The total follow-up period was recorded in all patients as the time from the date of the procedure (first or second treatment) to the most recent CT scan.
Statistical analysis
Factors influencing MWA were evaluated using Fisher’s exact test and Chi-squared test.
Factors considered were: position of the lesion (central or peripheral) and patient characteristics (age, sex, cirrhosis HBV–HCV–alcohol–cryptogenic related).
Fisher’s exact test evaluated correlation between effectiveness of the procedure and the position of the lesion (central or peripheral).
To evaluate relationship between patient characteristics and effectiveness of MWA, patients were subdivided in three groups: patients with neither residual nor recurrence (Group 1), patients with residual disease (Group 2), and patients with recurrence (Group 3) (Table 2). Fisher’s exact test evaluated separately correlation between age and sex of the patients and effectiveness of the treatment. Chi-squared test evaluated correlation between aetiology of cirrhosis and efficacy of the procedure.
Results
Technical success was obtained in all cases (100 %).
At first control, 1 month later, residual disease was recorded in 21 lesions treated (32.3 %): 13 (61.9 %) were peripheral and 8 central (38.1 %).
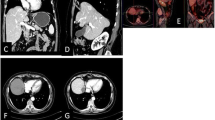
Twelve (57.1 %) residual lesions (4 central and 8 peripheral) were retreated with percutaneous MWA (Fig. 1a–c). Six lesions were treated with transarterial chemoembolization (TACE) and three were not suitable for any other treatment because of comorbidities and/or progression disease.
After 1 month, CT scan of the 12 tumours underwent to the second treatment with MWA showed residual tissue in four lesions (33.3 %) (2 central, 2 peripheral): one of these (peripheral lesion) was complicated by an intraparenchymal abscess. The third treatment with MWA was feasible for only one lesion (central lesion), because clinical condition of the patient was favourable; the remnant three lesions were not underwent to other treatment for progressive disease.
Local recurrence, measured at a distance of at least 6 months, was recorded in 8/65 lesions (12.3 %): 5 peripheral and 3 central.
Five (62.5 %) lesions were retreated with MWA (3 peripheral lesions and 2 central lesions); three lesions (37.5 %) were proposed for alternative treatments (radioembolization, TACE).
After the second treatment with MWA, two lesions (1 central, 1 peripheral) were completely ablate, in two lesions, residual disease was registered (1 central, 1 peripheral), and for one lesion, follow-up is not available.
In one case, residual tissue was proposed for TACE; the other one was not retreated for progression of the disease.
In thirty-six (36/65; 55.4 %) lesions, no residual or recurrent disease during follow-up was registered; 25 (69.4 %) were peripheral, and 11 (30.5 %) were central (Fig. 2a–c; Table 3).
Statistical results
Statistical analysis showed that there is not significant difference in the success of microwave ablation of the lesions located in a central position and those situated in the peripheral position (p = 0.60).
Moreover, there is no significant difference in terms of efficacy and patients characteristics analyzed separately (age, sex, and aetiology) (Table 4).
Complications
Major complications were identified in one case (1.6 %, 1/65) including liver abscess in a peripheral lesion (diameter 30 mm) treated with antibiotics and drainage.
The other complications observed were minor (24.5 %; 12/49), in particular fever and mild pain that did not required particular therapy.
The 30-day mortality rate was 0 %.
Discussion
In the last 20 years, RFA has gained great importance for the treatment of HCC because of the extent of its high effectiveness and minimal invasiveness [10]. RFA yields survival rates equivalent to those seen with surgical resection for small HCC tumours [11, 12]. As a result, RFA has been advocated as a first-line curative therapy for very early stage HCC [i.e., Barcelona clinical liver cancer (BCLC) stage 0] [5] or unresectable early stage HCC (BCLC stage A) [4, 5, 13, 14]. Although RFA is highly effective for treating small HCC tumours, application of the technique is potentially limited for large tumours (diameter > 3 cm), for tumours that are poorly visualized on ultrasonography (US) or tumours in high-risk or difficult to ablate locations [15].
MWA has been developed and improved greatly within the last several years. It has been widely used as an effective approach to small HCC due to the minimal damage to liver function, convenient manipulation, low complications, and mortality [16]. The two methods differ in their mechanism of action (RFA uses current as opposed to MWA that uses electromagnetic energy); MWA present more advantageous profile in terms of ablation volume, procedural time, and simultaneous treatment of multiple lesions [17].
The risk factors for tumour recurrence post-ablation therapy after treatment include tumour location, tumour size, multinodular tumours, and an insufficient safety margin.
Studies on comparing lesions treated by these two thermal ablative techniques have been carried out by several groups.
Vogh et al. [18] compared RFA and MWA in the treatment of HCC; they assessed that the end results of ablation therapy using RFA and MWA are influenced mainly by the inclusion and exclusion criteria of the ablation therapy as both techniques revealed no significant difference on the results of ablation.
However, at the time, not all expected results are satisfied after ablation. Different factors influence the effectiveness of ablation in terms of residual and recurrence disease observed during follow-up. To the best of our knowledge, no studies analyzed factors influencing efficacy of ablation.
Factors affecting the effectiveness of percutaneous ablation were analyzed by Francica et al. [19] after percutaneous laser ablation (PLA) under US guidance or by Mulier et al. [20] after RFA.
The size and location of tumoural lesions did not influenced efficacy of PLA.
Size of the tumour, pathology (HCC or metastasis), proximity to major vessel, location (subcapsular or not), and technical approach (percutaneous, laparoscopic, open) were the factors considered by Mulier et al. They concluded that RF by laparoscopy or laparotomy results is superior local control, independent of tumour size. The percutaneous route should mainly be reserved for patients who cannot tolerate a laparoscopy or laparotomy. The short-term benefits of less invasiveness for the percutaneous route do not outweigh the long-term higher risk of local recurrence.
The influence of the operator’s learning curve on achievement of complete ablation has only been addressed in one paper, namely, that by Poon et al. [21] dealing with RF ablation of primary and secondary liver tumours. In a prospective study, the authors demonstrated that the first 50 tumoural nodules were less efficiently ablated than the 50 lesions treated thereafter, ascribing these results to better selection of patients and refinements in ablative technique.
To the best of our knowledge no studies considered relationship between tumours and patients characteristics and efficacy of microwave ablation.
In this study, different factors, including patients and tumours characteristics, and clinicopathologic factors, were observed, and their relationship with outcome was assessed to determine whether any of these factors might be used to predict the prognosis of HCC.
Regarding location of the tumour (central or peripheral), in our series, no statistical differences were documented in terms of efficacy. This is an important result, because central tumours are usually near larger vessels or peripheral tumours may be adjacent to Glissonian capsule. In both cases, the same result was obtained after percutaneous MWA. Minor influence of heat sink effect of the technique utilized can be considered an explanation. Patient characteristics (age, sex, cirrhosis HBV–HCV–alcohol–cryptogenic related) were analyzed too, and no statistical differences in terms of efficacy (residual or recurrence disease) were registered.
A limitation of our study is the small number of patients included and the narrow size range of the lesions (<3 cm).
Therefore, it is conceivable that local recurrences represent a subgroup of biologically more aggressive neoplastic disease, much more difficult to control by local therapy. The infiltrating pattern of growth independently predicted incomplete ablation of HCC nodule is known. The same might be true for the appearance of new lesions. In our series of small HCC, the pattern of growth was not considered. Moreover, on imaging of small nodules, is not always clear the presence of capsule or not [19]. In conclusion, our results encourage the role of MWA in the treatment of small HCC. On the other hand, more numerous series are necessary to confirm our results. Moreover, randomized studies are necessary to state the role of MWA and to select the cases, which is more effective and safer MWA instead of RFA.
References
Yamagiwa K, Shiraki K, Yamakado K, Mizuno S, Hori T, Yagi S et al (2008) Survival rates according to the Cancer of the Liver Italian Program scores of 345 hepatocellular carcinoma patients after multimodality treatments during a 10-year period in a retrospective study. J Gastroenterol Hepatol 23(3):482–490
Thandassery RB, Goenka U, Goenka MK (2014) Role of local ablative therapy for hepatocellular carcinoma. J Clin Exp Hepatol 4:S104–S111
Tan CH, Low SC, Thng CH (2011) APASL and AASLD consensus guidelines on imaging diagnosis of hepatocellular carcinoma: a review. Int J Hepatol 2011:519783
Bruix J, Sherman M (2011) AASLD practice guideline, management of hepatocellular carcinoma: an update. Hepatology 53(3):1020–1022
European Association For The Study Of The Liver, European Organization For Research And Treatment Of Cancer (2012) EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 56:908–943
Common Terminology Criteria for Adverse Events (CTCAE) Version 4.0 (2010). The National Cancer Institute, Bethesda Approved after October 1, 2009
Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD 3rd, Dupuy DE et al (2009) Image-guided tumor ablation: standardization of terminology and reporting criteria. J Vasc Interv Radiol 20:S377–S390
Rhim H, Dodd GD 3rd, Chintapalli KN, Wood BJ, Dupuy DE, Hvizda JL et al (2004) Radiofrequency thermal ablation of abdominal tumors: lessons learned from complications. Radiographics 24:41–52
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R et al (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–247
Livraghi T, Meloni F, Di Stasi M, Rolle E, Solbiati L, Tinelli C et al (2008) Sustained complete response and complications rates after radiofrequency ablation of very early hepatocellular carcinoma in chirrosis: is resection still the treatment of choice? Hepatology 47:82–89
Huang J, Jan L, Cheng Z, Wu H, Du L, Wang J et al (2010) A randomized trial comparing radiofrequency ablationa and surgical resection for HCC conforming to the Milan criteria. Ann Surg 252:903–912
Chen MS, Li JQ, Zheng Y, Guo RP, Liang HH, Zhang YQ et al (2006) A prospective randomized trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Ann Surg 243:321–328
Omata M, Lesmana LA, Tateishi R, Chen PJ, Lin SM, Yoshida H et al (2010) Asian Pacific Association for the Study of the Liver consensus recommendation on hepatocellular carcinoma. Hepatol Int 4:439–474
Kudo M, Izumi N, Kokudo N, Matsui O, Sakamoto M, Nakashima O et al (2011) HCC expert panel of Japan Society of Hepatology. Management of hepatocellular carcinoma in Japan: consensus-based clinical practice guidelines proposed by the Japan Society of Hepatology (JSH) 2010 updated version. Dig Dis 29:339–364
Künzli BM, Abitabile P, Maurer CA (2011) Radio frequency ablation of liver tumors: actual limitations and potential solutions in the future. World J Hepatol 3:8–14
Wang ZL, Liang P, Dong BW, Yu XL, Yu DJ (2008) Prognostic factors and recurrence of small hepatocellular carcinoma after hepatic resection or microwave ablation: a retrospective study. J Gastrointest Surg 12:327–337
Poulou LS, Botsa E, Thanou I, Ziakas PD, Thanos L (2015) Percutaneous microwave ablation vs radiofrequency ablation in the treatment of hepatocellular carcinoma. World J Hepatol 7(8):1054–1063
Vogl TJ, Farshid P, Naguib NN, Zangos S, Bodelle B, Paul J et al (2015) Ablation therapy of hepatocellular carcinoma: a comparative study between radiofrequency and microwave ablation. Abdom Imaging 40(6):1829–1837
Francica G, Iodice G, Delle Cave M, Sarrantonio R, Lapiccirella G, Molese V et al (2007) Factors predicting complete necrosis rate after ultrasound-guided percutaneous laser thermoablation of smallhepatocellular carcinoma tumors in cirrhotic patients: a multivariate analysis. Acta Radiol 48(5):514–519
Mulier S, NiY, Iamart J, Ruers T, Marchal G, Michel R (2005) Local recurrence after hepatic radiofrequency coagulation: multivariate meta-analysis and review of contributing factors. Ann Surg 242(2):158–171
Poon RT, NgK K, Lam CM, Ai V, Yuen J, Fan ST, Wong J (2004) Learning curve for radiofrequency ablation of liver tumors: prospective analysis of initial 100 patients in a tertiary institution. Ann Surg 239:441–449
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Ierardi, A.M., Giorlando, F., Piacentino, F. et al. Factors predicting outcomes of microwave ablation of small hepatocellular carcinoma. Radiol med 122, 81–87 (2017). https://doi.org/10.1007/s11547-016-0694-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-016-0694-6