Aim
To evaluate the efficacy of whole brain radiotherapy (WBRT) with or without other treatments in patients (pts) with 1–3 brain metastases (BM).
Materials and methods
Toxicities and survival of 134 pts treated between 2009 and 2013 with WBRT alone (58 pts), WBRT plus surgery (SUR-WBRT: 42 pts) or WBRT followed by stereotactic or integrated boost radiotherapy (SRT-WBRT: 34 pts) were analyzed. Differences in toxicity (acute and late) incidence and in overall (OS), disease-free (DFS) and disease-specific survival (DSS) were evaluated (χ2-test, uni- and multivariate analysis).
Results
Pts given intensified treatments (SUR- and SBRT-WBRT) had better 3-month local response compared to WBRT alone group (p < 0.045). Better 1-year local control was evident only in SRT-WBRT pts (p < 0.035). Univariate OS analysis confirmed, as favorable prognostic factors, RPA class I (p < 0.001), GPA class III and IV (p < 0.001), single metastasis (p = 0.045), stable primary disease (p = 0.03), intensified treatment (p = 0.000), systemic therapy after radiotherapy (p = 0.04) and response of metastatic lesions (p = 0.002). At multivariate analysis, OS was better in RPA class I pts (p = 0.002), who had more aggressive radiotherapy treatments (p = 0.001), chemotherapy after radiotherapy (p < 0.001) and response to RT (p = 0.003). Response to radiotherapy (p = 0.002) and BM number (p < 0.001) resulted independently prognostic for DFS. About 60 % of patients had mild acute toxicity (G1), especially headache (51 %) and fatigue (34 %); only 2 patients (2 %) had severe (G3) headache and 5 patients (4 %) severe fatigue (G3) reversible with oral steroids. No differences were evident between the different treatment groups. Among 80 pts followed up with MRI, 12 (15 %) had leukoencephalopathy (equally distributed across subgroups) and 5 (6 %) radionecroses, 4/5 asymptomatic, 5/5 in pts given intensified treatments.
Conclusions
This analysis confirms the known prognostic factors for BM, emphasizing the importance of intensified treatments in a population with favorable features.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Historically, the treatment of brain metastases entailed the use of exclusive whole brain radiotherapy (WBRT), to treat the sites of disease and to prevent the recurrence in other cerebral areas [1, 2]. Currently, this method appears to be the standard for patients with multiple brain metastases (BM). Instead, patients with 1–3 BM are often amenable to treatments alternative or integrated with WBRT such as surgery, stereotactic radiosurgery or concomitant fractionated integrated boost (SIB) [3]. The therapeutic choice is conditioned not only by the number of brain lesions but also by other prognostic factors: performance status, age, absence of extracranial metastases and control of primary tumor. These prognostic factors are all present in the Graded Prognostic Assessment (GPA) classification [4], whereas in the Recursive Partitioning Analysis (RPA) classification [5] the number of lesions is not considered.
The end-point of the study has been to evaluate the toxicities and survival in a retrospective series of 134 patients affected by 1–3 brain metastases and treated with three different modalities: WBRT alone (WBRT), surgery plus WBRT (SUR-WBRT) and stereotactic boost or simultaneous integrated boost radiotherapy plus WBRT (SRT-WBRT).
Materials and methods
From January 2009 to December 2013, 134 patients with 1–3 brain metastases, good performance status and stable primary disease or asymptomatic synchronous primary tumor were consecutively treated at the Radiation Oncology Department, Spedali Civili, Brescia University.
Whole brain radiotherapy was delivered with two parallel opposite fields and standard doses (3 Gy/fraction for 10 fractions or 4 Gy/fraction for 5 fractions); patients were immobilized with a 3-point thermoplastic mask (WBRT and SUR-WBRT).
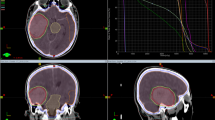
Stereotactic radiotherapy was provided with Tomotherapy©, with a single dose defined according to the volume to be treated as per RTOG protocol 90-05 (SRS) [6]. The single fraction stereotactic radiotherapy was delivered 30–45 days after WBRT. Patients treated with WBRT and concomitant integrated boost were also treated with Tomotherapy© in 10 fractions: for each fraction, 3 Gy were given to whole brain and 4.5 Gy to the metastatic site(s). Both the subsets of patients in this group (SRT-WBRT) were immobilized with a 5-point thermoplastic mask; the target definition was done after co-registration of brain magnetic resonance imaging (T1 contrast-enhanced sequence) with planning CT and GTV was expanded directly to PTV (3 mm-isotropic expansion).
The toxicity was considered acute if detected in the period between the start of radiotherapy up to 30 days after the end of the treatment, while late toxicity was registered from 90 days after the end of treatment until the last follow-up visit. Headache, nausea, vomiting and fatigue were considered acute toxicity and were classified according to the CTCAE v4.0 classification. The late toxicity, in terms of incidence of leukoencephalopathy and radiation necrosis, was evaluated only for patients who had neuroradiological follow-up with MRI (80 patients—60 %).
Local response and the pattern of local recurrence in the metastatic sites were evaluated at 3 and 12 months and correlated with treatment modalities, using Chi-square test. Overall survival (OS), “neurologic” disease-specific survival (DSS) and “neurologic” disease-free survival (DFS) were analyzed and compared, for the three treatment groups. The following events were considered to define, respectively, the three survival endpoints: death (OS), death caused by brain metastases (DSS) and brain disease progression (DFS).
Univariate analysis was done using the Kaplan–Meier estimator (log-rank test). Then the factors linked with significant differences in outcome at univariate analysis were entered into the multivariate stepwise Cox proportional hazard ratio model, along with the variables judged to be clinically relevant. Statistical analyses were obtained using the proprietary software SPSS17.0; a p value <0.05 was considered statistically significant.
Results
The characteristics of patients and disease are shown in Table 1.
In our series, 58 patients underwent WBRT alone, 42 surgery and radiotherapy (SUR-WBRT) and 34 more nonsurgical patients had WBRT and concurrent (21 patients) or sequential (13 patients) boost on the disease sites (SRT-WBRT).
The primary tumor type was lung adenocarcinoma in the majority of patients (58 %), breast cancer and melanoma contributed for 15 % each; different cancer types constituted the remaining 26 %. No differences in BM treatment modality according to the site of primary tumor were evident. In the whole series, about two-thirds of the patients had the diagnosis of brain metastases at the same time or within 1 year from that of the primary tumor (42 and 15 %, respectively); 32 and 11 % of them, respectively, from 1 to 5 years and more than 5 years after primary tumor diagnosis. No differences in BM treatment modality according to the time of onset of brain metastases were evident.
Although the patients of this series were selected according to the same criteria, those subjected to intensified treatments (SRT-WBRT and SUR-WBRT) had a significantly better performance status (p = 0.014) and, consequently, better RPA (p < 0.001) and GPA (p < 0.001) classes. They were also more frequently submitted to MRI at diagnosis (SUR-WBRT: 39 pts—93 %; SRT-WBRT: 34 pts—100 %; WBRT: 20 pts—34 %; p < 0.001). No differences were registered in the number of comorbidities and in the number of metastases among the different groups.
The patients in the surgery group had more frequent (95 %) clinical symptoms at onset (seizures, headache, motor or balance disorders) than those treated with radiation alone (WBRT—55 %—or SRT-WBRT—59 %—, p < 0.001). Patients in the SRT-WBRT group had systemic treatments for the primary tumor after radiotherapy more frequently (79 %) than those in the SUR-WBRT (48 %) and WBRT (52 %) groups (p = 0.035).
The total and fractional doses given for each treatment modality are shown in Table 2.
About 60 % of patients had mild acute toxicity (G1), especially headache (51 %) and fatigue (34 %); only 2 patients (2 %) had severe (G3) headache and 5 patients (4 %) severe fatigue (G3). All these symptoms subsided with the use of oral steroid and (1 case only) of osmotic diuretics. No differences in toxicity incidence were found according to treatment modality.
Late toxicity was evaluated in the group of 80 patients submitted to brain MRI in the follow-up (SRT-WBRT, n = 34; SUR-WBRT, n = 30; WBRT, n = 16).
Twelve cases (15 %) of leukoencephalopathy (G1) and 5 cases (6 %) of radiation necrosis were identified: all the leukoencephalopathies were diagnosed with MRI in asymptomatic patients and were equally distributed in the three treatment groups (p = ns). Only one case of radiation necrosis was submitted to surgical removal (SUR-WBRT group), the other four having been diagnosed with MRI in asymptomatic patients (they were all in the SRT-WBRT group). Leukoencephalopathy was defined as asymptomatic because detected during routine neuroradiological evaluation. No patients were submitted to MRI because of clinical worsening.
Some of these patients, especially in the more recent times, had neurocognitive assessment, but because of the retrospective nature of the study, it has not been reported and was not considered as an end-point of our analysis.
Response to treatment 3 months after the end of radiotherapy was significantly better in patients treated with intensified treatment compared to those treated with WBRT alone, with a greater number of complete or subtotal partial responses (p = 0.045, Table 3).
After one year from the end of treatment a better local control was evident only in patients treated with sequential or concurrent boost (p = 0.035, Table 3).
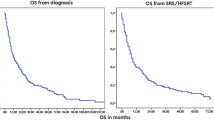
Overall survival was 58 % at 6 months and 36 % at 12 months; DFS was respectively 72 and 49 % at the same time intervals after radiotherapy.
Univariate analysis confirmed, as favorable prognostic factors for overall survival, RPA class I (p < 0.001), GPA class III and IV (p < 0.001), single metastasis (p = 0.045), stable primary disease (no other metastases or other stable metastases before brain progression) (p = 0.03), intensified treatment compared to WBRT alone (p < 0.001), systemic therapy after radiotherapy (p = 0.04), obtaining a complete or subtotal partial response of metastatic lesions after radiotherapy (p = 0.002) and having a primary tumor different from lung cancer (p = 0.035).
In the WBRT group the use of standard fractionation (30 Gy in 10 fractions) compared to “short course” treatment (20 Gy in 5 fractions) resulted in similar OS.
As far as DSS univariate analysis is concerned, the use of chemotherapy after radiotherapy (p = 0.05), a good response to treatment (p = 0.009) and a primary tumor different from lung cancer (p = 0.05) were confirmed as favorable prognostic factors.
The only favorable prognostic factor for DFS at univariate analysis resulted to be the presence of a single brain lesion at diagnosis (p < 0.001).
Since the clinical features of the three treatment groups were not homogeneous, we performed a subgroup analysis limited to patients belonging to RPA class II (n = 105): the intensified treatments resulted again related to a better overall survival compared to WBRT alone (p < 0.001). However, comparing the two intensified treatments (SUR-WBRT vs SRT-WBRT) a longer survival for patients in the SRT-WBRT group was evident (p = 0.05, Fig. 1).
No OS, DSS and DFS differences were evident between patients treated with the two stereotactic techniques (SIB and SRS boost, data not shown).
All the significant prognostic factors identified at univariate analysis and, in addition, the clinically relevant but not significant ones were included in the multivariate Cox regression model for OS, DSS and DFS: RPA class, GPA class, number of metastases, the presence of other metastases at diagnosis of brain progression, the primary tumor type, the use of chemotherapy after radiation therapy, radiotherapy modality and the tumor response.
Patients in RPA class I (p = 0.002), who had intensified treatments (p < 0.001), who were given systemic therapy after radiation therapy (p < 0.001) and who had a complete or subtotal partial response to radiotherapy (p = 0.003) have a longer OS. The complete response to radiotherapy remained the sole positive prognostic factor for DSS (p = 0.03), while response to radiotherapy (p = 0.002) and the number of metastases (p < 0.001) were significant in terms of DFS. Similar results in multivariate analysis were found in RPA II subgroup.
Discussion
The prognostic factors related to better survival for patients with brain metastases have been studied in numerous clinical trials; many prognostic classifications [7] have been proposed in the last two decades to define the prognosis and consequently the better therapeutic option. Performance status, age and presence of extracranial metastases were considered in all classifications. Some special parameters such as the interval between the appearance of metastases and primary tumor diagnosis [8], response to steroid therapy [9] and tumor volume [10] were considered only in rare cases. RPA [5] and GPA [4] classifications are the more relevant ones. The most important difference between these two systems is that the second one considers as a prognostic factor also the number of metastases and the primary site of disease [11]. The analysis of the present series has confirmed the prognostic significance of almost all the factors identified in the two classifications.
The use of different hypofractionated schedules for WBRT (30 Gy in 10 fractions vs 20 Gy in 5 fractions) was not related, in a few papers [12, 13], to a difference in overall survival but only to an increase in acute toxicity for the more “rapid” fractionation schedule. In the present series no survival differences were evident according to the fraction dose; however, an increase in acute toxicity with the shorter schedule was not documented.
Multimodal combined treatment with WBRT, for patients with 1–3 brain metastases, has become the standard in the last decades [14], thanks to advances in radiation techniques and to improvement of surgical techniques [15], with a marked reduction in peri- and post-operative mortality.
The efficacy of surgery followed by WBRT for single brain metastasis has been investigated in three randomized clinical trials. Patchell et al. [16] demonstrated that combined treatment (surgery plus WBRT) led to a longer survival, longer functional independence, and a lower recurrence rate compared to radiotherapy alone. Similar results were also published by Vecht et al. [17], who evidenced a better outcome of combined treatment in patients with stable extracranial disease. The third randomized trial [18] failed to demonstrate an improvement in survival for the patients treated with combined treatment; since patients with diffuse extracranial disease and poor performance status were recruited, it was confirmed that this group of poor prognosis patients, should not be offered an intensified treatment.
Literature data on survival have been confirmed in the present series: surgery followed by WBRT obtained longer overall survival and better response to treatment compared to WBRT alone; no differences were found in recurrence rate in metastasis site.
The efficacy of a stereotactic boost associated with WBRT has been shown in two randomized clinical trials. In the RTOG 9508 trial [19] 333 patients with 1–3 brain metastases were randomly allocated to either WBRT or SRT-WBRT: WBRT and stereotactic boost treatment improved functional autonomy for all patients and survival for patients with a single metastasis. In the secondary analysis performed after 10 years [20] 252 patients have been re-classified according to the GPA scale and re-analyzed. Survival advantage was found only in patients with high GPA score (3.5–4) regardless of whether they have 1, 2, or 3 brain metastases. A smaller trial [21] showed that combined WBRT and radiosurgery for patients with two to four brain metastases significantly improves control of brain disease, without improvement of survival.
Present analysis confirmed a better local control and a better response to treatment in patients treated with SRT-WBRT compared to WBRT alone, as documented in the literature, and a longer overall survival has been documented both in the whole series and in the RPA class II.
Almost two-thirds (n = 21) of the patients of the present series treated with stereotactic techniques had WBRT with concomitant integrated boost (SIB), as opposed to about a third (n = 13) treated with WBRT followed by sequential stereotactic boost (SRS). The scarce number of cases in the two subgroups hampers a proper comparison of the results. Unfortunately, there are few conclusive data also in the literature about the relative efficacy of SIB and SRS radiotherapy when integrated with WBRT. Rodrigues et al. [22] in 2013 published a retrospective review of 500 patients treated with SRS alone or SIB-WBRT: no differences in OS were found but SIB was associated with a reduced intracranial failure rate likely due to the WBRT component of the treatment; however, SRS patients did not have WBRT, at variance with the present series.
Few authors compared the different intensified treatments for 1–3 brain metastases. O’Neill et al. [23] compared neurosurgery versus stereotactic radiosurgery without WBRT and evidenced a higher recurrence rate in the surgical cavity. Rades [24] comparing SRT-WBRT and surgery-WBRT showed a better local control in the SRT group (at 1 year, 82 vs 66 %, p = 0.006). Overlapping data have been found in the present series: 1-year local control was 91 % in the SRT-WBRT group vs 67 % in the SUR-WBRT (p = 0.035). A better overall survival was documented but only in RPA class II.
The high rate of local recurrence after surgery alone has led many authors to add a stereotactic treatment targeting the surgical cavity only [25–28]. These studies have shown good tolerance to treatment and better 1 and 2 years local control, a lower risk of progression with other brain metastases, combined with a moderate increase in late toxicity (radiation necrosis in 5 % of cases) when compared to WBRT alone. Confirmatory Phase II and III randomized trials are needed.
This series cannot provide useful information on the neurocognitive effect mainly due to the retrospective nature of the study. Many clinical studies addressed the issue of a possible neurocognitive detrimental effect of WBRT [29] to justify the elimination of WBRT from the therapeutic options for brain metastases. The results are far from being definitive [30–32]. More detailed studies considering also the effect of disease recurrence or of the other treatments (e.g. steroids, anti-epileptic drugs, surgery, stereotactic radiotherapy) on neurocognitive changes observed after treatment of brain metastases need to be performed to confirm these reports.
Conclusions
The use of intensified treatment, both with surgery and radiotherapy, compared to WBRT alone determines a significantly longer survival and better response to treatment, with no increase in acute and late toxicity, for patients with 1–3 brain metastases. For patients in RPA class II, the group treated with WBRT plus a radiation therapy boost obtained an OS longer than the group treated with surgery plus WBRT. A better local control was also found in patients treated with stereotactic boost, either concurrent or sequential.
The high 1-year local recurrence risk in the surgical bed aroused the interest for radiation treatment of the surgical cavity and its margins, in the absence of large scale confirmatory trials [25–28].
With all the limitations of a retrospective case series, the present analysis confirms the already known prognostic factors for brain metastases radiotherapy, emphasizing the importance of intensified treatments in a population with favorable prognostic features (age, performance status, number of metastases under 3, primary tumor control, I–II RPA and GPA prognostic class).
Cognitive impairment possibly related to brain irradiation is an important issue. A prospective observational trial on neurocognitive function in relation to different radiotherapy modalities (WBRT, SRT-WBRT, SRS alone) and other disease and treatment variables is now ongoing in Italy, promoted by the Central Nervous System Study Group of Italian Association of Radiation Oncology (AIRO).
References
Posner JB (1992) Management of brain metastases. Rev Neurol (Paris) 148(6–7):477–487
Sundström JT, Minn H, Lertola KK, Nordman E (1998) Prognosis of patients treated for intracranial metastases with whole-brain irradiation. Ann Med 30(3):296–299
NCCN Guidelines Central Nervous System Cancers (version 2.2014) http://www.nccn.org/professionals/physician_gls/pdf/cns.pdf. Accessed 22 April 2015
Sperduto PW, Chao ST, Sneed PK, Luo X, Suh J, Roberge D, Bhatt A, Jensen AW, Brown PD, Shih H, Kirkpatrick J, Schwer A, Gaspar LE, Fiveash JB, Chiang V, Knisely J, Sperduto CM, Mehta M (2010) Diagnosis-specific prognostic factors, indexes, and treatment outcomes for patients with newly diagnosed brain metastases: a multi-institutional analysis of 4,259 patients. Int J Radiat Oncol Biol Phys 77(3):655–661
Gaspar L, Scott C, Rotman M, Asbell S, Phillips T, Wasserman T, McKenna WG, Byhardt R (1997) Partitioning analysis (RPA) of prognostic factors in three Radiation Therapy Oncology Group (RTOG) brain metastases trials. Int J Radiat Oncol Biol Phys 37(4):745–751 (recursive)
Shaw E, Scott C, Souhami L et al (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90-05. Int J Radiat Oncol Biol Phys 47:291–298
Zindler JD, Rodrigues G, Haasbeek CJ, De Haan PF, Meijer OW, Slotman BJ, Lagerwaard FJ (2013) The clinical utility of prognostic scoring systems in patients with brain metastases treated with radiosurgery. Radiother Oncol 106(3):370–374
Rades D, Dziggel L, Haatanen T, Veninga T, Lohynska R, Dunst J, Schild SE (2011) Scoring systems to estimate intracerebral control and survival rates of patients irradiated for brain metastases. Int J Radiat Oncol Biol Phys 80(4):1122–1127
Lagerwaard FJ, Levendag PC, Nowak PJ, Eijkenboom WM, Hanssens PE, Schmitz PI (1999) Identification of prognostic factors in patients with brain metastases: a review of 1292 patients. Int J Radiat Oncol Biol Phys 43(4):795–803
Weltman E, Salvajoli JV, Brandt RA, de Morais Hanriot R, Prisco FE, Cruz JC, de Oliveira Borges SUR, Wajsbrot DB (2000) Radiosurgery for brain metastases: a score index for predicting prognosis. Int J Radiat Oncol Biol Phys 46(5):1155–1161
Buglione M, Bandera L, Grisanti S, Pasinetti N, Borghetti P, Barbera F, Triggiani L, Costa L, Shehi B, Bonetti B, Magrini S (2012) The impact of tumour histology and recursive partitioning analysis classification on the prognosis of patients treated with whole-brain hypofractionated radiotherapy for brain metastases: analysis of 382 patients. Radiol Med 117(1):133–147
Priestman TJ, Dunn J, Brada M, Rampling R, Baker PG (1996) Final results of the Royal College of Radiologists’ trial comparing two different radiotherapy schedules in the treatment of cerebral metastases. Clin Oncol (R Coll Radiol) 8(5):308–315
Borgelt B, Gelber R, Kramer S, Brady LW, Chang CH, Davis LW, Perez CA, Hendrickson FR (1980) The palliation of brain metastases: final results of the first two studies by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys 6(1):1–9
Scoccianti S, Ricardi U (2012) Treatment of brain metastases: review of phase III randomized controlled trials. Radiother Oncol 102(2):168–179
Agnoletti A, Mencarani C, Panciani PP, Buffoni L, Ronchetti G, Spena G, Tartara F, Buglione M, Pagano M, Ducati A, Fontanella M, Garbossa D (2014) Surgery in cerebral metastases: are numbers so important? J Cancer Res Ther 10(1):79–83
Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, Markesbery WR, Macdonald JS, Young B (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322(8):494–500
Vecht CJ, Haaxma-Reiche H, Noordijk EM, Padberg GW, Voormolen JH, Hoekstra FH, Tans JT, Lambooij N, Metsaars JA, Wattendorff AR et al (1993) Treatment of single brain metastasis: radiotherapy alone or combined with neurosurgery? Ann Neurol 33(6):583–590
Mintz AH, Kestle J, Rathbone MP, Gaspar L, Hugenholtz H, Fisher B, Duncan G, Skingley P, Foster G, Levine M (1996) A randomized trial to assess the efficacy of surgery in addition to radiotherapy in patients with a single cerebral metastasis. Cancer 78(7):1470–1476
Andrews DW, Scott CB, Sperduto PW, Flanders AE, Gaspar LE, Schell MC, Werner-Wasik M, Demas W, Ryu J, Bahary JP, Souhami L, Rotman M, Mehta MP, Curran WJ Jr (2004) Whole brain radiation therapy with or without stereotactic radiosurgery boost for patients with one to three brain metastases: phase III results of the RTOG 9508 randomised trial. Lancet 363(9422):1665–1672
Sperduto PW, Shanley R, Luo X, Andrews D, Werner-Wasik M, Valicenti R, Bahary JP, Souhami L, Won M, Mehta M (2014) Secondary analysis of RTOG 9508, a phase 3 randomized trial of whole-brain radiation therapy versus WBRT plus stereotactic radiosurgery in patients with 1–3 brain metastases; poststratified by the graded prognostic assessment (GPA). Int J Radiat Oncol Biol Phys 90(3):526–531
Kondziolka D, Patel A, Lunsford LD, Kassam A, Flickinger JC (1999) Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys 45(2):427–434
Rodrigues G, Zindler J, Warner A, Bauman G, Senan S, Lagerwaard F (2013) Propensity-score matched pair comparison of whole brain with simultaneous in-field boost radiotherapy and stereotactic radiosurgery. Radiother Oncol 106(2):206–209
O’Neill BP, Iturria NJ, Link MJ, Pollock BE, Ballman KV, O’Fallon JR (2003) A comparison of surgical resection and stereotactic radiosurgery in the treatment of solitary brain metastases. Int J Radiat Oncol Biol Phys 55(5):1169–1176
Rades D, Kueter JD, Veninga T, Gliemroth J, Schild SE (2009) Whole brain radiotherapy plus stereotactic radiosurgery (WBRT + SURS) versus surgery plus whole brain radiotherapy (OP + WBRT) for 1–3 brain metastases: results of a matched pair analysis. Eur J Cancer 45(3):400–404
Gans JH, Raper DM, Shah AH, Bregy A, Heros D, Lally BE, Morcos JJ, Heros RC, Komotar RJ (2013) The role of radiosurgery to the tumor bed after resection of brain metastases. Neurosurgery 72(3):317–325
Brennan C, Yang TJ, Hilden P, Zhang Z, Chan K, Yamada Y, Chan TA, Lymberis SC, Narayana A, Tabar V, Gutin PH, Ballangrud Å, Lis E, Beal K (2014) A phase 2 trial of stereotactic radiosurgery boost after surgical resection for brain metastases. Int J Radiat Oncol Biol Phys 88(1):130–136
Roberge D, Parney I, Brown PD (2012) Radiosurgery to the postoperative surgical cavity: who needs evidence? Int J Radiat Oncol Biol Phys 83(2):486–493
Karlovits BJ, Quigley MR, Karlovits SM, Miller L, Johnson M, Gayou O, Fuhrer R (2009) Stereotactic radiosurgery boost to the resection bed for oligometastatic brain disease: challenging the tradition of adjuvant whole-brain radiotherapy. Neurosurg Focus 27(6):E7
Soffietti R, Kocher M, Abacioglu UM, Villa S, Fauchon F, Baumert BG, Fariselli L, Tzuk-Shina T, Kortmann RD, Carrie C, Ben Hassel M, Kouri M, Valeinis E, van den Berge D, Mueller RP, Tridello G, Collette L, Bottomley A (2013) A European Organisation for Research and Treatment of Cancer phase III trial of adjuvant whole-brain radiotherapy versus observation in patients with one to three brain metastases from solid tumors after surgical resection or radiosurgery: quality-of-life results. J Clin Oncol 31(1):65–72
McDuff SG, Taich ZJ, Lawson JD, Sanghvi P, Wong ET, Barker FG 2nd, Hochberg FH, Loeffler JS, Warnke PC, Murphy KT, Mundt AJ, Carter BS, McDonald CR, Chen CC (2013) Neurocognitive assessment following whole brain radiation therapy and radiosurgery for patients with cerebral metastases. J Neurol Neurosurg Psychiatry 84(12):1384–1391
Nakazaki K, Kano H (2013) Evaluation of mini-mental status examination score after gamma knife radiosurgery as the first radiation treatment for brain metastases. J Neurooncol 112(3):421–425
Welzel G, Fleckenstein K, Schaefer J, Hermann B, Kraus-Tiefenbacher U, Mai SK, Wenz F (2008) Memory function before and after whole brain radiotherapy in patients with and without brain metastases. Int J Radiat Oncol Biol Phys 72(5):1311–1318
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
For retrospective studies f ormal consent is not required.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the Neuro-Oncology Group, Spedali Civili Hospital and Brescia University.
Rights and permissions
About this article
Cite this article
Buglione, M., Pedretti, S., Gipponi, S. et al. The treatment of patients with 1–3 brain metastases: is there a place for whole brain radiotherapy alone, yet? A retrospective analysis. Radiol med 120, 1146–1152 (2015). https://doi.org/10.1007/s11547-015-0542-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-015-0542-0