Abstract
Housing instability, a growing public health problem, may be an independent environmental risk factor for hypertension, but limited prospective data exist. We sought to determine the independent association of housing instability in early adulthood (year 5, 1990–1991) and incident hypertension over the subsequent 15 years of follow-up (years 7, 10, 15, and 20) in the Coronary Artery Risk Development in Young Adults (CARDIA) study (N = 5,115). Because causes of inadequate housing and its effects on health are thought to vary by race and sex, we hypothesized that housing instability would exert a differential effect on incident hypertension by race and sex. At year 5, all CARDIA participants were asked about housing and those free of hypertension were analyzed (N = 4,342). We defined housing instability as living in overcrowded housing, moving frequently, or living doubled up. Of the 4,342 participants, 8.5 % were living in unstable housing. Across all participants, housing instability was not associated with incident hypertension (incidence rate ratio (IRR), 1.1; 95 % CI, 0.9–1.5) after adjusting for demographics, socioeconomic status, substance use, social factors, body mass index, and study site. However, the association varied by race and sex (p value for interaction, <0.001). Unstably housed white women had a hypertension incidence rate 4.7 times (IRR, 4.7; 95 % CI, 2.4–9.2) that of stably housed white women in adjusted analysis. There was no association among white men, black women, or black men. These findings suggest that housing instability may be a more important risk factor among white women, and may act independently or as a marker for other psychosocial stressors (e.g., stress from intimate partner violence) leading to development of hypertension. Studies that examine the role of these psychosocial stressors in development of hypertension risk among unstably housed white women are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
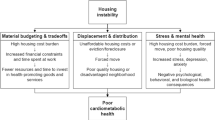
Housing instability, a precursor to homelessness, may be an independent risk factor for poor health. Housing instability is described in the sociological literature but lacks a standard definition. Definitions include living doubled up with family or friends or moving frequently due to an inability to pay rent, living in overcrowded conditions, or spending more than 50 % of household income on rent.1–6
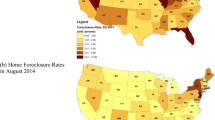
Housing instability, a growing public health problem, has received national attention because of the lack of affordable low-income housing, the foreclosure crisis, and rising unemployment.7,8 The number of people living doubled up (one definition of housing instability) increased by 5 % from 4.6 million in 2005 to 4.8 million adults in 2008.9 In 2009, when poverty rates reached a 15-year high, the number of people living doubled up with family or friends increased by 11.6 % compared to 2008.8,10
Recurrent housing instability can lead to homelessness.4 Blacks and men are disproportionately represented among homeless adults.11 While white women are least likely to experience homelessness, those who are homeless comprise a uniquely vulnerable group with respect to psychosocial risk factors that are distinct from being black or male.12,13
Homeless adults face barriers to receiving health care,14,15 suffer from chronic medical conditions including hypertension,16–18 and experience premature mortality from cardiovascular disease.19,20 Studies among unstably housed adults demonstrate similar barriers to receiving health care,1,21 but little is known about health outcomes.
Hypertension is common among economically disadvantaged individuals.22,23 Social and environmental stressors of poverty may contribute to hypertension by augmenting physiological stress, or affecting diet and physical activity, and access to health care.24 Known social and environmental stressors associated with incident and prevalent hypertension include poor neighborhood conditions,25 homelessness,26 job insecurity,27 daily interpersonal conflicts,28 incarceration,29 and racial discrimination.30
We hypothesized that housing instability is an important independent social and environmental risk factor for incident hypertension. We sought to determine the independent association of housing instability at year 5 and incident hypertension at years 7, 10, 15, and 20 in the Coronary Artery Risk Development In young Adults (CARDIA) study. Because causes of housing instability and its effects on health may vary by race and sex, we hypothesized, a priori, that the association between housing instability and incident hypertension would differ by race and sex. As access to care is important for treatment of hypertension, we also examined if housing instability was associated prospectively with barriers to receiving health care.
Methods
The CARDIA study is a longitudinal cohort study examining the development of clinical and subclinical cardiovascular disease.31,32 In 1985–1986, 5,115 black and white men and women aged 18–30 years were recruited from four US cities (Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and Oakland, California). Sampling rates were controlled to balance the cohort by age (45 % aged 18–24 years and 55 % aged 25–30 years), sex (55 % male and 45 % female), race (52 % black and 48 % white), and education level (40 % with ≤high school and 60 % ≥high school). Participants were asked to return for follow-up examinations during 1987–1988 (year 2), 1990–1991 (year 5), 1992–1993 (year 7), 1995–1996 (year 10), 2000–2001 (year 15), and 2005–2006 (year 20) at each center. Retention rates were 91 % at year 2, 86 % at year 5, 81 % at year 7, 79 % at year 10, 74 % at year 15, and 72 % at year 20. Because questions on housing were asked at year 5 (1990–91) in CARDIA, this year served as the baseline for this analysis. Of the 5,115 participants recruited in 1985–1986, 4,342 who completed the year 5 examination and were free of hypertension at that time were analyzed.
Housing Instability
At year 5 (1990–1991), CARDIA participants were asked about frequent moves, housing crowding, and occupying a place without rent or money. We created a composite measure of housing instability, which we defined as >2 persons per bedroom (total number of people living in the household including children/number of bedrooms in the household),33 or moving frequently (eight or more moves in the past 2 years, excluding people who were currently in school, college or graduate school) or currently occupying a place without paying rent or money as a proxy for living doubled up.1–5 For the latter component, participants were asked, “Is the home where you live: owned or being bought by you (or someone else in the household), rented for money, or occupied without paying rent or money?” Participants who reported living in a home that was occupied without paying rent or money were considered as living doubled up.
Incident Hypertension
At each CARDIA exam, trained and certified research staff measured right-arm blood pressure using a random-zero sphygmomanometer until the year 20 exam, when concerns about mercury in the apparatus required a switch to the OmROn sphygmomanometer. We used the average of the second and third blood pressure readings and defined hypertension as systolic blood pressure of ≥140 mmHg, diastolic blood pressure of ≥90 mmHg, or self-reported use of anti-hypertensive medications. We used incident hypertension at years 7, 10, 15, and 20 as the primary, discrete-time survival outcome for this analysis among study participants who did not meet the definition at any earlier visit.
Access to Health Care
We created three indicators of lack of access to health care: lack of a usual place to receive care, an unmet need for medical care, and lack of health insurance. Participants were asked at years 7, 10, 15, and 20, “Do you have a usual source of medical care? By that, we mean the place you go if you need a check-up or if you are ill?” Persons answering no to this question or reporting walk-in clinic or emergency room as their usual source of care were coded as lacking a usual source of care. Participants were coded as having an unmet need for medical care if they answered yes to the question, “Was there anytime during the past two years when you did not seek medical care because it was too expensive or health insurance did not cover it?” Participants were coded as lacking health insurance if they answered no to the question, “In the past two years have you always had health insurance or other medical coverage for health care?” We measured access to health care outcomes at years 7, 10, 15, and 20.
Potential Confounders
We used time-varying covariates from all examinations between years 5 and 20 for all potential confounders of the association of housing instability and incident hypertension. We defined socioeconomic status by both education (≤high school or >high school) and annual income. The latter was based on combined family pre-tax income for the past 12 months, including income from wages, veteran’s benefits, help from relatives, and rental receipts from properties. “Low-income” was defined as less than $24,999 (i.e., <200 % of the federal poverty level for one-person households in 2010).34
We created a dichotomous variable for married/partnered versus not (single, widowed, divorced, or separated). We defined presence of children as a three-level categorical variable: having no children or stepchildren, having children and/or stepchildren not living at home, or having children and/or stepchildren living at home.
Current smokers were those who reported smoking at least five cigarettes weekly for the last 3 months, in contrast to former and never smokers. Excess alcohol use, based on a consumption survey,35 was defined as >7 drinks/week for women, and >14 drinks/week for men, with a drink defined as 360 ml of beer, 150 ml of wine, or 45 ml of liquor.36 Current use of cocaine or amphetamines was based on self-report of any consumption in the past 30 days, versus former use (ever used, but not in last 30 days), or never having used.
Body mass index (BMI) was calculated as weight in kilograms divided by height in square meters, and used as continuous variable. Analysis included study site at year 5 (1990–1991) as housing instability could differ by city.
Potential Mediators
We examined depression as one potential mediator of the association of housing instability and incident hypertension. The CES-D instrument was used to obtain information on depressive symptoms at years 5, 10, 15, and 20.37–39 We categorized participants as having higher depressive symptoms when they had CES-D scores of ≥16, lower depressive symptoms when they had CES-D scores of ≤7, and intermediate symptoms when their scores fell in between these two cut-offs.37
Statistical Analysis
We considered year 5 (1990–1991) as the baseline for this analysis, and examined incident hypertension outcomes at years 7, 10, 15, and 20. Because we hypothesized that the effects of housing instability would vary by race and sex, we assessed potential differences in the effects of housing instability among white women, white men, black women, and black men. We compared study participants with and without housing instability using the t-test for continuous variables and chi-square test for categorical variables. Because we had interval-censored data, we used Poisson regression to estimate the unadjusted annual incidence of hypertension by housing status for the whole cohort and for each of the four race and sex groups. Using Poisson regression, we determined the adjusted incidence rate ratios (IRR) of hypertension by housing status, controlling for study site, sex, race, and other time-varying confounders such as age education, income, marital/partnered status, children, smoking, alcohol, cocaine, amphetamine use, and BMI. We tested for two-way interaction between housing instability and race and sex and examined the association between housing instability and incident hypertension for each of the four race and sex groups controlling for covariates and other time-varying confounders. Because definitions of housing instability vary, we repeated these analyses on the subset of unstably housed adults who were only living in crowded housing as a sensitivity analysis. To assess the effect of depression as a potential mediator, we first examined the association between housing instability and depression using ordinal logistic regression controlling for covariates and time-varying confounders, and then looked for attenuation of the IRR after adding depression to the model with incident hypertension, housing instability, and other confounders. To assess the independent effects of housing instability on lack of access to care at years 7, 10, 15, and 20, we used multivariable logistic regression, accounting for repeated measurements of the outcome and covariates, and adjusting for demographics, socioeconomic status, social factors, behavioral risk factors, and study site. We conducted all analyses using Stata, version 11 (Stata Corp, College Station, TX).
Results
Of the 4,342 participants, 370 (8.5 %) reported living in unstable housing at year 5 (Table 1). The prevalence of housing instability in white women was 5.0 % (59/1,179), white men 6.6 % (69/1,052), black women 11.7 % (142/1,212), and black men 11.1 % (100/899). The majority of adults living in unstable housing reported low annual incomes, with unstably housed white and black men and women more likely to report low annual incomes compared to their stably housed counterparts.
Among those who were stably housed at year 5, 21.4 % developed incident hypertension over the subsequent 15 years, with an unadjusted annual incidence of 1.2 %. In contrast, 27.4 % of unstably housed adults developed incident hypertension over this interval, with an unadjusted annual rate of 1.7 % (Table 2; Figure 1). Among all participants combined, after adjusting for potential confounders including demographics, socioeconomic status, social factors, behavioral factors, BMI, and study site, adults living in unstable housing had a hypertension incidence rate of 1.1 times greater than those in stable housing, though these results did not attain statistical significance (IRR, 1.1; 95 % CI, 0.9–1.5) (Table 2).
The association of housing instability and incident hypertension varied by race and sex (p value for interaction, <0.001), with incident hypertension more likely to occur in white women living in unstable housing relative to their stably housed counterparts. The unadjusted annual incidence rate of hypertension was 1.6 % for white women living in unstable housing compared with 0.5 % for white women in stable housing (Figure 1). After adjusting for potential confounders, unstably housed white women had an incidence rate four times (IRR, 4.7; 95 % CI, 2.4–9.2) that of stably housed white women (Table 2). For all other race and sex groups, rates of hypertension incidence did not vary by housing status.
In sensitivity analysis, we restricted the definition of housing instability to participants living in crowded housing (n = 181 at year 5) and found similar results. Across the whole cohort, adults living in crowded housing at baseline had 1.3 (IRR, 1.3; 95 % CI, 1.0–1.8) times the rate of incident hypertension relative to those living in un-crowded housing after adjusting for potential confounders, though this association did not attain significance. However, there were differences by race and sex (p value for interaction, <0.001). White women living in crowded housing had 7.4 times the rate of incident hypertension than white women living in un-crowded housing after adjusting for confounders (IRR, 7.4; 95 % CI, 3.5–15.4). There were no significant associations among white men (IRR, 1.8; 95 % CI, 0.4–7.5), black women (IRR, 1.0; 95 % CI, 0.7–1.6), or black men (IRR, 1.1; 95 % CI, 0.5–2.1).
We examined depression as a potential mediator of the association of housing instability and incident hypertension among white women. Depression was not significantly associated with housing instability among white women (adjusted odds ratio (AOR), 1.0; 95 % CI, 0.6–1.6). While it did decrease the magnitude of IRR for housing instability in the final model with incident hypertension (IRR, 3.6; 95 % CI, 1.8–7.4), depression was not significantly associated with incident hypertension (IRR, 1.1; 95 % CI, 0.8–1.4).
When examining access to health care as an outcome, participants who were unstably housed at year 5 were more likely to lack a usual source of care (AOR, 1.6; 95 % CI, 1.3–1.9) and report an unmet need for medical care (AOR, 1.6; 95 % CI, 1.2–2.0) after controlling for potential confounders (Table 3). Participants in unstable housing were not more likely to lack health insurance relative to their stably housed counterparts after adjusting for potential confounders (AOR, 1.0; 95 % CI, 0.8–1.3). Compared with those who were stably housed, unstably housed white women, white men, and black women were more likely to lack a usual source of care. Unstably housed white and black men had greater odds of an unmet need for medical care compared with their stably housed counterparts.
Discussion
In a well-characterized cohort of young adults living in four US cities, we examined the independent association between housing instability and incident hypertension. While there was no association between housing instability and incident hypertension across the cohort, there were significant interactions by race and sex. Unstably housed white women were at an increased risk of developing hypertension, whereas white men, black women and black men were not. The discordance by race and sex suggest that housing instability may reflect different phenomena and have differential effects on hypertension incidence among black and white men and women. To our knowledge, this is the first longitudinal study examining the long-term effects of housing instability on hypertension incidence and could further our understanding of the role of social and environmental risk factors in development of cardiovascular risk.
Stably housed white women in the CARDIA cohort had the lowest baseline annual incidence of hypertension compared with white men, black women, or black men. Blacks and men had elevated baseline annual incidence rates of hypertension that did not differ significantly by housing status. These estimates of annual incidence of hypertension in black and white men and women are similar to those reported in prior studies.40–43 Notably, unstably housed white women lost the protective advantage while living in stable housing and had annual incidence rates of hypertension that exceeded not only stably housed white women but also approached the high rates seen in black women and men.
The differential effect of housing instability on hypertension incidence among white women may be partly due to the uneven distribution of social, behavioral and childhood risk factors for homelessness across race and sex groups. Recurrent housing instability can lead to homelessness as a result of selective accumulation of these social, behavioral, and childhood risk factors over time.4,12 White homeless women, when compared with homeless women of other racial/ethnic minorities and all homeless men, are more likely to experience mental health and substance use disorders, intimate partner violence, problematic childhood experiences such as foster care or institutional placement, childhood sexual and physical abuse, and family disruptions.12,13,44 To some extent, homelessness among black or Latina women stem more from extreme poverty or an inability to afford low-income housing, than from social, behavioral, or childhood risk factors that are significantly more prevalent among white women.13,45 Because of the increased burden of these stressors, white homeless women report worse self-reported health status, increased medical concerns, and hospitalizations than homeless women of racial/ethnic minorities.13,44,46 Although these studies were done among homeless adults, we posit that similar processes that increase risk for poor health may apply to unstably housed adults.
In our study, we found a differential association between housing instability and hypertension risk despite controlling for some of the socioeconomic, social, and behavioral risk factors that contribute to the development of housing instability. These findings suggest that, among white women, housing instability itself may be an independent risk factor, or may serve as a marker for other associated social or childhood experiences such as intimate partner violence or childhood sexual or physical abuse leading to the development of hypertension. Prior studies have shown that women with intimate partner violence or childhood sexual or physical abuse have an increased prevalence of hypertension.47–50 These stressors are more prevalent among homeless white women than among homeless women of other racial/ethnic minorities.12,13,44 Because we did not have access to specific measures on intimate partner violence or childhood abuse, we were unable to examine the independent effects of these stressors on the association between housing instability and incident hypertension. Studies that examine these stressors in conjunction with housing and in relation to hypertension would advance this line of inquiry.
We examined depressive symptoms as a mediator of the association of housing instability and incident hypertension because of the increased prevalence of psychological distress and mental illness among homeless white women,13,44 and also because depression was associated with hypertension in prior longitudinal studies.37,51 Among white women, depression was not associated with housing instability. Adding depression to the final model did slightly attenuate the IRR, though it was not a significant independent predictor of incident hypertension, suggesting a lack of a mediating effect.
We did not observe an association between unstable housing and incident hypertension among black men or women. Biological factors such as increased salt sensitivity, and psychosocial factors such as stress related to severe poverty or discrimination are some of the postulated reasons for the higher rates of hypertension among blacks.52,53 Thus, housing instability, while disproportionate among blacks, may not reflect risk that exceeds other well-established biological causes and psychosocial stressors among black men and women.
Adults living in unstable housing had an increased likelihood of experiencing barriers to health care, and were more likely to lack a usual place of care and experience an unmet need for medical care compared with those who were stably housed. These findings are in agreement with prior studies linking housing instability with barriers to health care.1,21 In contrast to previous studies, there was no association between housing instability and access to health insurance after adjusting for potential confounders. As access to care is important for treatment and prevention of long-term complications of hypertension, these findings have implications for eliminating barriers to health care in this population.
We recognize several limitations. The components of our measure of housing instability are qualitatively different, potentially contributing to misclassification bias. We may have underestimated the number of people living doubled-up by excluding people living in a home that may have been bought or rented by someone else in their household, biasing our results towards the null. Measurements of housing instability and behavioral risk factors were by self-report, potentially resulting in underreporting that may differ by race and sex. We did not have information about housing status between years 7 and 20 limiting our ability to determine the duration and intensity of the exposure that may contribute to the development of hypertension. However, our data allowed us to estimate the effects of exposure to housing instability during early adulthood and provide evidence that an early-life stressful event may have downstream cardiovascular effects among certain groups. Understanding the mechanisms by which early adulthood stressors can lead to later development of cardiovascular risk can potentially stall the emergence of such risk factors. Because we had insufficient cases of incident hypertension at the earlier time points (years 7 and 10), we were unable to determine the effects of housing instability on transient hypertension. Being a white woman may not be the most salient descriptor of risk of hypertension among people experiencing housing instability. Other unmeasured risk factors for hypertension could discriminate a wider group of people across races in ways that are also associated with housing instability, and should be explored in future studies.
Despite these limitations, our data allowed us to calculate annual incidence of hypertension by housing status in a cohort of black and white men and women representative of the US population. Using two separate definitions of housing instability, we found an increased risk of hypertension among white women, but not in white men, black women, or black men, as well as barriers in access to care among all these groups. The inconsistency in our findings by race and sex suggests that housing instability may be a more important risk factor for hypertension in some groups. Unstably housed white women may be especially vulnerable to the development of hypertension due to psychosocial risk factors that are either unmeasured in this study and for which the severity may be worse than other race and sex groups. Understanding the effects of housing instability and associated psychosocial stressors on hypertension risk among unstably housed white women may offer insights into the phenomenon of housing instability overall, and provide opportunities to improve screening, treatment, and prevention of long-term complications of hypertension among this population.
References
Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006; 21(1): 71–77.
Bassuk EL, Weinreb LF, Buckner JC, Browne A, Salomon A, Bassuk SS. The characteristics and needs of sheltered homeless and low-income housed mothers. JAMA. 1996; 276(8): 640–646.
Appleby L, Desai P. Residential instability: a perspective on system imbalance. Am J Orthopsychiatry. 1987; 57(4): 515–524.
Rossi PH, Wright JD, Fisher GA, Willis G. The urban homeless: estimating composition and size. Science. 1987; 235(4794): 1336–1341.
Lawson SB. Housing instability: toward a better understanding of frequent residential mobility among America's urban poor. Washington, DC: Center for Housing Policy; 2010.
Cutts DB, Meyers AF, Black MM, et al. US Housing insecurity and the health of very young children. Am J Public Health. 2011; 101(8): 1508–1514.
Homelessness Research Institute. State of homelessness in America 2011. Washington, DC. Available at: http://www.endhomelessness.org/content/article/detail/3668. Accessed July 14, 2011.
Eckholm E. “Recession raises poverty rates to 15-year high”. New York Times, September 17, 2010 late ed.: A1. Print.
Homelessness Research Institute. Economic Bytes: Double up in the United States, 2010. Washington, DC. Available at: http://www.endhomelessness.org/content/article/detail/3024. Accessed July 14, 2011.
DeNavas-Walt C, Procter BD, Smith JC. Income, Poverty, and Health Insurance Coverage in the United States: 2009. Washington, DC: U.S. Census Bureau, Current Population Reports, P60–238; 2010.
The 2009 Annual Homeless Assessment Report to Congress. Washington, DC: U.S. Department of Housing and Urban Development, Office of Community Planning and Development; 2010.
Koegel P, Melamid E, Burnam A. Childhood risk factors for homelessness among homeless adults. Am J Public Health. 1995; 85(12): 1642–1649.
Stein JA, Andersen R, Gelberg L. Applying the Gelberg–Andersen behavioral model for vulnerable populations to health services utilization in homeless women. J Health Psychol. 2007; 12(5): 791–804.
Kushel MB, Vittinghoff E, Haas JS. Factors associated with the health care utilization of homeless persons. JAMA. 2001; 285(2): 200–206.
Baggett TP, O'Connell JJ, Singer DE, Rigotti NA. The unmet health care needs of homeless adults: a national study. Am J Public Health. 2010; 100(7): 1326–1333.
Gelberg L, Linn LS, Usatine RP, Smith MH. Health, homelessness, and poverty. A study of clinic users. Arch Intern Med. 1990; 150(11): 2325–2330.
Hwang SW. Homelessness and health. CMAJ. 2001; 164(2): 229–233.
Szerlip MI, Szerlip HM. Identification of cardiovascular risk factors in homeless adults. Am J Med Sci. 2002; 324(5): 243–246.
Hwang SW, Wilkins R, Tjepkema M, O'Campo PJ, Dunn JR. Mortality among residents of shelters, rooming houses, and hotels in Canada: 11 year follow-up study. BMJ. 2009; 339: b4036.
Hwang SW, Orav EJ, O'Connell JJ, Lebow JM, Brennan TA. Causes of death in homeless adults in Boston. Ann Intern Med. 1997; 126(8): 625–628.
Ma CT, Gee L, Kushel MB. Associations between housing instability and food insecurity with health care access in low-income children. Ambul Pediatr. 2008; 8(1): 50–57.
Diez-Roux AV, Northridge ME, Morabia A, Bassett MT, Shea S. Prevalence and social correlates of cardiovascular disease risk factors in Harlem. Am J Public Health. 1999; 89(3): 302–307.
Matthews KA, Kiefe CI, Lewis CE, Liu K, Sidney S, Yunis C. Socioeconomic trajectories and incident hypertension in a biracial cohort of young adults. Hypertension. 2002; 39(3): 772–776.
Diez Roux AV. Residential environments and cardiovascular risk. J Urban Health. 2003; 80(4): 569–589.
Mujahid MS, Diez Roux AV, Morenoff JD, et al. Neighborhood characteristics and hypertension. Epidemiology. 2008; 19(4): 590–598.
Gelberg L, Linn LS. Assessing the physical health of homeless adults. JAMA. 1989; 262(14): 1973–1979.
Levenstein S, Smith MW, Kaplan GA. Psychosocial predictors of hypertension in men and women. Arch Intern Med. 2001; 161(10): 1341–1346.
Schoenthaler AM, Schwartz J, Cassells A, Tobin JN, Brondolo E. Daily interpersonal conflict predicts masked hypertension in an urban sample. Am J Hypertens. 2010; 23: 1982–1088.
Wang EA, Pletcher M, Lin F, et al. Incarceration, incident hypertension, and access to health care: findings from the coronary artery risk development in young adults (CARDIA) study. Arch Intern Med. 2009; 169(7): 687–693.
Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA study of young black and white adults. Am J Public Health. 1996; 86(10): 1370–1378.
Hughes GH, Cutter G, Donahue R, et al. Recruitment in the coronary artery disease risk development in young adults (CARDIA) study. Control Clin Trials. 1987; 8(4 Suppl): 68S–73S.
Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988; 41(11): 1105–1116.
Blake KS, Kellerson LR, and Simic A. Measuring overcrowding in housing. Washington, DC: US Department of Housing and Urban Development, Office of Policy Development and Research; 2007.
U.S. Department of Health and Human Services. Prior HHS Poverty Guidelines and Federal Register References.Washington, DC. Available at: http://aspe.hhs.gov/poverty/figures-fed-reg.shtml. Accessed July 14, 2011.
Pletcher MJ, Varosy P, Kiefe CI, Lewis CE, Sidney S, Hulley SB. Alcohol consumption, binge drinking, and early coronary calcification: findings from the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Epidemiol. 2005; 161(5): 423–433.
National Institute on Alcohol Abuse and Alcoholism. Helping patients who drink too much: a clinicians’ guide, 2005. Washington, DC. Available at: http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf. Accessed July 14, 2011.
Davidson K, Jonas BS, Dixon KE, Markovitz JH. Do depression symptoms predict early hypertension incidence in young adults in the CARDIA study? Coronary artery risk development in young adults. Arch Intern Med. 2000; 160(10): 1495–1500.
Radloff L. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Measure. 1977; 1: 385–401.
Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977; 106(3): 203–214.
Hajjar I, Kotchen JM, Kotchen TA. Hypertension: trends in prevalence, incidence, and control. Annu Rev Public Health. 2006; 27: 465–490.
Kramer H, Han C, Post W, et al. Racial/ethnic differences in hypertension and hypertension treatment and control in the multi-ethnic study of atherosclerosis (MESA). Am J Hypertens. 2004; 17(10): 963–970.
Diez Roux AV, Chambless L, Merkin SS, et al. Socioeconomic disadvantage and change in blood pressure associated with aging. Circulation. 2002; 106(6): 703–710.
Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA. 2003; 290(2): 199–206.
Austin EL, Andersen R, Gelberg L. Ethnic differences in the correlates of mental distress among homeless women. Womens Health Issues. 2008; 18(1): 26–34.
Teruya C, Longshore D, Andersen RM, et al. Health and health care disparities among homeless women. Women Health. 2010; 50(8): 719–736.
Gelberg L, Andersen R, Longshore D, et al. Hospitalizations among homeless women: are there ethnic and drug abuse disparities? J Behav Health Serv Res. 2009; 36(2): 212–232.
Riley EH, Wright RJ, Jun HJ, Hibert EN, Rich-Edwards JW. Hypertension in adult survivors of child abuse: observations from the Nurses' Health Study II. J Epidemiol Community Health. 2010; 64(5): 413–418.
Scott-Storey K, Wuest J, Ford-Gilboe M. Intimate partner violence and cardiovascular risk: is there a link? J Adv Nurs. 2009; 65(10): 2186–2197.
Cloutier S, Martin SL, Poole C. Sexual assault among North Carolina women: prevalence and health risk factors. J Epidemiol Community Health. 2002; 56(4): 265–271.
Danese A, Moffitt TE, Harrington H, et al. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Arch Pediatr Adolesc Med. 2009; 163(12): 1135–1143.
Nabi H, Chastang JF, Lefevre T, et al. Trajectories of depressive episodes and hypertension over 24 years: the Whitehall II prospective cohort study. Hypertens. 2011; 57(4): 710–716.
Anderson NB, Myers HF, Pickering T, Jackson JS. Hypertension in blacks: psychosocial and biological perspectives. J Hypertens. 1989; 7(3): 161–172.
Williams DR. Black–white differences in blood pressure: the role of social factors. Ethn Dis. 1992; 2(2): 126–141.
Acknowledgments
Dr. Vijayaraghavan was supported by the Department of Health and Human Services-Health Resources and Services Administration, Primary Care Research Fellowship grant (D55HP05165) at the University of California, San Francisco. Dr. Vijayaraghavan is currently supported by a post-doctoral fellowship at the Cancer Prevention and Control Program, Moores Cancer Center at the University of California, San Diego. Dr. Bibbins-Domingo was supported by grants from the Robert Wood Johnson Amos Faculty Development Program, a diversity supplement to the CARDIA study contract to the University of Alabama Coordinating Center (grant N01-HC-95095), and by a UCSF Hellman Family Faculty Award. Preliminary results from this study were presented at the UCSF Health Disparities Research Symposium, 22 October 2010, and the Annual Society of General Internal Medicine Conference, 4–7 May 2011. The authors would like to thank Tekeshe Mekonnen, MS, for providing administrative assistance in the submission of the manuscript.
Financial Sources
Work on this manuscript was supported (or partially supported) by contracts: University of Alabama at Birmingham, Coordinating Center, N01-HC-95095; University of Alabama at Birmingham, Field Center, N01-HC-48047; University of Minnesota, Field Center and Diet Reading Center (Year 20 Exam), N01-HC-48048; Northwestern University, Field Center, N01-HC-48049; Kaiser Foundation Research Institute, N01-HC-48050; University of California, Irvine, Echocardiography Reading Center (Year 5 and 10), N01-HC-45134; Harbor-UCLA Research Education Institute, Computed Tomography Reading Center (Year 15 Exam), N01-HC-05187; Wake Forest University (Year 20 Exam), N01-HC-45205; New England Medical Center (Year 20 Exam), N01-HC-45204 from the National Heart, Lung and Blood Institute. The funding organizations had no role in the design and conduct of the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vijayaraghavan, M., Kushel, M.B., Vittinghoff, E. et al. Housing Instability and Incident Hypertension in the CARDIA Cohort. J Urban Health 90, 427–441 (2013). https://doi.org/10.1007/s11524-012-9729-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-012-9729-z