Abstract
Cabozantinib is an inhibitor of multiple receptor tyrosine kinases (RTKs) with roles in cancer pathogenesis. This review focuses on data relevant to the use of cabozantinib tablets (Cabometyx®) in the treatment of hepatocellular carcinoma (HCC) in patients who have been previously treated with the multi-RTK inhibitor sorafenib, an indication for which cabozantinib tablets are approved in the EU and USA. Approval of cabozantinib in this setting was based largely on the findings of CELESTIAL, a phase 3 trial in adults with advanced HCC who had previously received sorafenib, had progressive disease after at least one systemic therapy and had received up to two systemic treatments for their advanced disease. Compared with placebo in this study, cabozantinib prolonged both overall survival and progression-free survival, with these findings largely unaffected by patient/disease characteristics. The tolerability profile of cabozantinib in CELESTIAL was acceptable and consistent with that of other multi-RTK inhibitors, with adverse events that were manageable with dose modification and supportive care. Thus, cabozantinib is a welcome additional treatment option for use in adults with HCC previously treated with sorafenib.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Inhibits several receptor tyrosine kinases, including MET, AXL and VEGFR1–3 |
Prolongs both overall and progression-free survival in adults with previously-treated advanced HCC |
Generally well tolerated, with manageable adverse events |
1 Introduction
Liver cancer is one of the most common causes of cancer-related death worldwide, with the majority of primary liver cancers being hepatocellular carcinomas (HCCs) [1]. Risk factors for HCC are numerous [2], with key causes including hepatitis B and C virus (HBV and HCV) infection [3] and most HCC cases occurring in individuals with cirrhosis and other histological liver abnormalities [2, 4]. The hepatocarcinogenic process of HCC is thought to involve the development of genetic derangements (via chronic inflammation, damage/regeneration and carcinogens) that often lead to various signalling pathways being overexpressed and/or constitutively activated, with the greatest number of poor prognostic gene signatures being seen in more aggressive HCC forms with higher levels of alpha-feta protein (AFP) [5].
Treatment options for HCC vary on the basis of tumor burden, liver function and patient performance status, and include resection, transplantation, local ablation, transarterial chemoembolization (TACE) and systemic therapy [3, 4, 6]. The first systemic agent available for HCC was sorafenib, a drug that impacts various tumor-signalling pathways via inhibition of multiple receptor tyrosine kinases (RTKs), including VEGFR1–3, PDGFR, KIT, and RET [7]. HCC is often advanced at diagnosis, and for years, sorafenib was the only systemic treatment available for advanced disease, leaving patients who progressed on the drug with no further systemic treatment options [7]. However, in recent years, the treatment landscape for advanced HCC has improved with the introduction of additional systemic therapies, one of which is cabozantinib.
Cabozantinib is a multi-RTK inhibitor with an RTK inhibition profile distinct from, but partially overlapping, that of sorafenib. This review focuses on data relevant to the use of cabozantinib tablets (Cabometyx®) in the treatment of HCC in patients who have been previously treated with sorafenib, an indication for which cabozantinib tablets are approved in the USA [8] and EU [9]. Discussion of the other indications for which cabozantinib tablets or cabozantinib capsules (Cometriq®) are approved is beyond the scope of this review.
2 Pharmacodynamic Properties of Cabozantinib
Cabozantinib is a potent inhibitor of several RTKs with roles in oncogenesis, angiogenesis, tumor growth, metastasis and various other pathological processes [8, 9]. These RTKs include the hepatocyte growth factor receptor MET, VEGFR-1, -2 and -3, AXL, FLT-3, KIT, MER, RET, ROS1, TIE-2, TRKB, and TYRO3 [8,9,10]. Cabozantinib inhibited the phosphorylation (activation) of MET and VEGFR-2 [10, 11] in vitro, as well as in mice (MET in liver [10] and tumor [10, 11] tissue and VEGFR-2 in lung tissue [11]), and likewise inhibited in vitro phosphorylation of AXL, FLT3 and KIT [10].
Cabozantinib displayed antiangiogenic effects in preclinical studies, inhibiting endothelial cell tubule formation in vitro [10], reducing tumor microvessel density in HCC xenografts [11] and disrupting the vasculature of MET- and VEGF-expressing tumors in mice [10]. The drug also had anti-proliferative effects in HCC [11] and other human cancer cell lines [10], inhibited tumor proliferation/growth in rodent xenograft models of HCC [11] and other cancers [10] and promoted tumor xenograft apoptosis [10, 11]. Note, cabozantinib appeared to be more potent against HCC xenografts that were positive for phosphorylated MET, indicating potential for the phosphorylated protein to be a marker of susceptibility to the drug [11].
Cabozantinib also inhibited hepatocyte growth factor-induced migration and invasion of HCC [11] and other tumor cells [10, 11] in vitro, and inhibited metastasis of HCC cells to the lungs and liver of mice [11]. In contrast, sorafenib (which targets VEGFR but not MET) increased lung and liver tumor burden in the metastasis model, possibly as a result of MET activity upregulation [11]. Thus, by targeting both VEGFR and MET, cabozantinib may block some pathways of metastatic escape.
3 Pharmacokinetic Properties of Cabozantinib
Cabozantinib reached maximum plasma concentrations in a median of 3–4 h in healthy adults who received a single 20, 40 or 60 mg dose of the drug as tablets; exposure to the drug increased dose-proportionally [12]. Cabozantinib tablets are not bioequivalent to cabozantinib capsules [12] and, consequently, the two formulations are not interchangeable [8, 9]. Cabozantinib should not be taken with food (Sect. 6) [8, 9], as administering a single 140 mg capsule dose in a fed versus a fasted state moderately increased exposure to the drug in healthy adults [13]. Cabozantinib has an oral volume of distribution of ≈ 319 L and displays high plasma protein binding (≥ 99.7%) [8]. In vitro data indicate that cabozantinib is metabolized by CYP3A4 [8, 9], with CYP2C9 contributing only minimally [9]. Elimination of the drug occurs via the feces and urine, with 54 and 27% of a single dose being recovered via these routes within 48 days of administration [8, 9]. Cabozantinib has a plasma terminal elimination half-life of ≈ 110 h and a mean estimated clearance at steady state of 2.48 L/h following oral doses of 20–140 mg [9].
Exposure to cabozantinib was not impacted to any clinically relevant degree by mild hepatic impairment in a population pharmacokinetic analysis [8], although was increased by 63% by moderate hepatic impairment (Child Pugh class B) in a dedicated pharmacokinetic study [14]. No dosage adjustment is necessary for mild hepatic impairment [8, 9], while moderate hepatic impairment requires dosage reduction in the USA [8]; close monitoring is advised in both populations in the EU [9]. Mild or moderate renal impairment (i.e. estimated glomerular filtration rate 60–89 or 30–59 mL/min/1.73 m2) increases cabozantinib exposure marginally [14] and requires no dosage adjustment [8, 9], although caution is recommended in the EU [9]. As the efficacy and safety of cabozantinib have not been determined in patients with severe renal or hepatic impairment, the drug is not recommended for use in these populations in the EU [9] and should be avoided in patients with severe hepatic impairment in the USA [8]. Cabozantinib pharmacokinetics do not appear to be impacted to any clinically relevant extent by age, race or sex [8].
3.1 Drug Interactions
As cabozantinib is a substrate of CYP3A4, drugs that inhibit or induce CYP3A4 may increase or decrease cabozantinib concentrations in plasma [15]; thus, if drugs must be taken in combination with cabozantinib, consider those with little or no potential to inhibit/induce this enzyme [9]. In cabozantinib recipients, strong inhibitors or inducers of CYP3A4 should be avoided in the USA [8] and chronic coadministration of strong CYP3A4 inducers should be avoided in the EU [9]. If coadministering cabozantinib with strong CYP3A4 inhibitors is necessary, caution is advised in the EU [9] and a reduction in cabozantinib dosage is recommended in the USA [8]. The cabozantinib dosage should be increased if coadministered with strong CYP3A4 inducers in the USA [8].
As cabozantinib is also an MRP2 substrate in vitro, drugs that inhibit this transporter could increase cabozantinib concentrations in the plasma [8, 9]; cautious concomitant use is advised in the EU [9]. By contrast, bile salt-sequestering agents may reduce exposure to cabozantinib by impacting its absorption or re-absorption; however, the clinical relevance of this potential interaction is not yet known [9].
Cabozantinib inhibits p-glycoprotein (p-gp) in vitro (and may thus increase plasma concentrations of drugs that are p-gp substrates [8, 9]) and induces CYP1A1 mRNA [8]. It is not known if these potential interactions are of any clinical significance [8], although patients should be cautioned about taking p-gp substrates and cabozantinib concomitantly [9]. Cabozantinib (because of its high plasma protein binding) may also interact with warfarin, warranting international normalization ratio monitoring [9]. Although it is not yet known if cabozantinib alters the pharmacokinetics of contraceptive steroids, use of additional methods of contraception is advised in the EU [9].
4 Therapeutic Efficacy of Cabozantinib
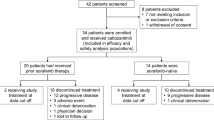
This section focuses on the clinical efficacy of oral cabozantinib in patients with previously-treated advanced HCC, as evaluated in a randomized, double-blind, phase 3 trial (CELESTIAL) [16]. This study was conducted on the basis of the findings of a randomized, phase 2, discontinuation trial that assessed the potential of cabozantinib in patients with advanced solid tumors (n = 526) [17]; however, given the limited number of evaluable HCC patients in this study (n = 41) [17, 18], it is not discussed further here. Some data are available as abstracts/posters [19,20,21,22,23,24,25].
Patients eligible for CELESTIAL were adults (aged ≥18 years) with pathologically confirmed HCC unamenable to curative therapies (e.g. surgery, transplant, radiofrequency ablation) who had previously been treated with sorafenib (tolerance to sorafenib was not specified) [16]. Patients must have had disease progression despite one or more systemic therapies for HCC, were permitted to have received up to two systemic treatment regimens for advanced disease and had an ECOG performance status (PS) of 0 or 1 and Child-Pugh class A liver function. Eligible patients were randomized to receive cabozantinib or placebo, with randomization stratified by etiologic factor [the most common of which was HBV infection (38% of patients)], geographic region [the most common of which was Europe (48%)] and evidence of extrahepatic disease and/or macrovascular invasion (85% of patients affected). Therapy was continued for as long as clinical benefit was evident or until unacceptable toxicity; treatment could be continued beyond radiographic progression provided clinical benefit was sustained. The data discussed here are from the second planned interim analysis (data cut-off 1 June 2017) in which patients had received cabozantinib or placebo for a median duration of 3.8 and 2.0 months. At baseline, 79 and 77% of patients in the cabozantinib and placebo groups had extrahepatic disease, 27 and 34% had macrovascular invasion, and 27% of patients across the two groups had previously received two systemic anticancer regimens for advanced HCC [16].
Treatment with cabozantinib significantly prolonged overall survival (OS; primary endpoint) relative to placebo, with the corresponding hazard ratio (HR) indicating a 24% reduction in the risk of death (Table 1) [16]. Kaplan–Meier estimates of the proportion of patients alive at 6, 12, 18 and 24 months in the cabozantinib (72, 46, 32 and 18%, respectively) and placebo (61, 34, 18 and 13%) group supported these findings. Progression-free survival (PFS) was also significantly prolonged with cabozantinib versus placebo (Table 1) [16].
When stratification factors [16, 20, 21] and other patient/disease characteristics (e.g. age [16, 22], sex [16], race [16], ECOG PS [16], AFP level [16, 23], sum of target lesion diameters (SOD) [21], prior TACE status [24] and number of previous systemic therapies [16] (including sorafenib only [16, 25]) were assessed to determine their impact on these survival endpoints, findings were generally consistent with those of the overall trial population. The HR for death indicated that OS favored cabozantinib versus placebo (i.e. was <1.0) in most subgroups, with the exceptions being patients enrolled in Asia (1.01; 95% CI 0.68–1.48) and patients with HCV (without HBV) infection (1.11; 95% CI 0.72–1.71); however, the difference was not always statistically significant (based on 95% CIs) [16]. By contrast, significant PFS benefit was seen with cabozantinib over placebo in all subgroups, as indicated by HRs (and 95% CIs) for progression or death [16, 20,21,22,23,24,25].
The rate of objective tumor response with cabozantinib was significantly greater than with placebo, albeit <4.0% (Table 1), with all of the responses being partial in nature [16]. The remaining cabozantinib and placebo recipients had stable disease (60 vs. 33%), progressive disease (21 vs. 55%) or were missing/not evaluable (15 vs. 11%) [16]. Almost half of cabozantinib recipients had a reduction from baseline in the SOD as a best response (47 vs. 11% of placebo recipients) [19]. Moreover, cabozantinib was associated with a rate of disease control almost twice as high [16], and a time to progression almost three-times as long [19], as with placebo (Table 1). In the respective groups, 26 and 33% of patients were subsequently treated with systemic or local liver-directed anticancer therapy other than radiation [16].
5 Tolerability of Cabozantinib
Oral cabozantinib had an acceptable tolerability profile in adults with advanced HCC in CELESTIAL, with the adverse events (AEs) being manageable through dose modification and supportive care [16].
Treatment-emergent AEs (TEAEs) occurred in most cabozantinib and placebo recipients (99 vs. 92%), with those that occurred most commonly (i.e. incidence ≥20%) and with at least a 10% greater incidence with cabozantinib including diarrhea, decreased appetite, palmar-plantar erythrodysesthesia (PPE), fatigue, nausea, hypertension, vomiting, increased AST level and asthenia (Fig. 1) [16]. Five-fold more cabozantinib than placebo recipients (16 vs. 3%) discontinued treatment because of AEs that were considered to be treatment related (TRAEs), among which were PPE, fatigue, decreased appetite, diarrhea and nausea in the cabozantinib group (1–2% of recipients discontinued for each) [8, 16]. Dose reductions occurred in 62 and 13% of patients in the cabozantinib and placebo groups (median 38 days to first cabozantinib reduction) [16] and treatment was interrupted in 84% of cabozantinib recipients (median 28 days to first interruption) [9].
Most common (incidence ≥20%) treatment-emergent adverse events with ≥10% greater incidence with oral cabozantinib than with placebo in adults with advanced hepatocellular carcinoma in the CELESTIAL trial [16]. AST aspartate aminotransferase, PPE palmar-plantar erythrodysesthesia
Grade 3 or 4 TEAEs occurred in almost twofold more cabozantinib than placebo recipients (68 vs. 36%), with the most frequent with cabozantinib being PPE (17 vs. 0% of placebo recipients), hypertension (16 vs. 2%), increased AST (12 vs. 7%), diarrhea (10 vs. 2%) and fatigue (10 vs. 4%) [16]. Some patients experienced grade 5 AEs within 30 days of the last cabozantinib or placebo dose (12% of each group), although these were often related to progression of disease; 1.3% of cabozantinib recipients had grade 5 AEs that were considered to be treatment related, among which were bronchoesophageal fistula, upper gastrointestinal (GI) hemorrhage, hepatic failure, portal-vein thrombosis, pulmonary embolism and hepatorenal syndrome (one patient each). Half of cabozantinib recipients experienced serious TEAEs (50 vs. 37% of placebo recipients) [16]. Of note, among the exclusion criteria of CELESTIAL were concomitant anticoagulant/antiplatelet therapy (low doses of aspirin, warfarin or low molecular-weight heparin were permitted), untreated/incompletely treated varices with bleeding/high bleeding risk and various other clinically significant illnesses, including certain cardiovascular disorders, and GI disorders with high fistula/perforation risk [16].
Liver function should be monitored before initiating cabozantinib and closely during treatment [9]. As many of the AEs associated with the drug (including GI AEs, hypertension, and PPE) occur early in the course of therapy, close patient monitoring is recommended during the first 8 weeks to determine whether dose modifications may be necessary [9]. As highlighted in CELESTIAL, cabozantinib therapy may need to be interrupted and/or reduced in dosage in order to manage suspected adverse drug reactions (depending on their severity), although may need to be permanently discontinued if adverse reactions cannot be adequately managed; supportive/medical care may also be required [9].
On the basis of the tolerability profile of cabozantinib across trials and indications, there are specific warnings and precautions relating to the potential for PPE, hepatic function abnormalities, GI disorders/fistulas/perforations, hypertension and thromboembolic events, as well as a number of other AEs, including hepatic encephalopathy, hemorrhage, thrombocytopenia, wound complications, reversible posterior leukoencephalopathy syndrome, proteinuria, QT interval prolongation and electrolyte abnormalities [9].
6 Dosage and Administration of Cabozantinib
For the treatment of HCC in patients (specifically adults [9]) previously treated with sorafenib, the recommended dosage of cabozantinib in the EU [9] and USA [8] is 60 mg taken once daily on an empty stomach (i.e. no food should be eaten for at least 2 h before and for 1 h after taking the drug). Treatment should be continued until there is no longer clinical benefit [9], there is disease progression [8] or toxicity is unacceptable [8, 9]. Consult local prescribing information for details regarding potential drug interactions, use in special patient populations, dosage modifications, contraindications, warnings and other precautions.
7 Place of Cabozantinib in Managing Advanced Hepatocellular Carcinoma
Over the years, a variety of targeted systemic treatments have been investigated as treatments for HCC. The multi-RTK inhibitor sorafenib was the first such agent to improve survival in those with advanced disease and remains the standard of care in this setting today [3, 4, 6]. However, sorafenib is no longer the only systemic treatment option available for HCC, with second-line (regorafenib, cabozantinib, nivolumab, pembrolizumab) and further first-line (lenvatinib) targeted systemic options now also approved for use in various markets, and some novel agents also showing promise in development. Like sorafenib, most of the newer approved agents inhibit multiple RTKs with roles in HCC pathogenesis, although differences in their RTK inhibition profiles [5] allow for sequential use.
Of these agents, cabozantinib is the most recently approved for HCC. The drug inhibits various RTKs (Sect. 2), some of which (MET and AXL) are implicated in antiangiogenic agent resistance [26, 27] and are poor prognostic factors in HCC [28,29,30] (although MET expression is not currently used for patient selection). Cabozantinib is indicated in the EU and USA for the treatment of HCC in patients previously treated with sorafenib, with the approval being largely based on the findings of the large CELESTIAL trial (Sect. 4). Compared with placebo in this study, cabozantinib prolonged both the OS and PFS of adults with advanced HCC who had previously received sorafenib (regardless of their tolerance of the drug), had progressive disease after at least one systemic therapy and had received up to two systemic treatments for advanced disease, with these findings largely unaffected by patient/disease characteristics (Sect. 4). Cabozantinib had an acceptable tolerability profile in this study, consistent with that of other multi-RTK inhibitors, with AEs that were manageable through dose modification and supportive care (Sect. 5).
On the basis of these findings, some [3, 4] of the most recent guidelines [3, 4, 6] for HCC management strongly recommend cabozantinib as a second-line targeted treatment option for advanced disease, although the patient population specifics differ slightly between guidelines (i.e. patients with well-preserved hepatic function with progressive HCC on one or two systemic therapies and ECOG PS 0–1 [3] or those with good hepatic function whose HCC is unresectable (and unsuitable for transplant) or inoperable/metastatic/of high tumour burden and has progressed on/after sorafenib [4]). The only other agent strongly recommended for use in this setting is regorafenib [3, 4, 6], which was the first systemic agent approved for use after sorafenib progression [7] and is considered in some guidelines as the standard option for those who have progressed on, but tolerate, sorafenib [3, 6].
Further robust clinical and real-world studies would be beneficial to confirm the efficacy and safety of cabozantinib in patients with poorer performance status or more impaired hepatic function than those enrolled in CELESTIAL (Sect. 4) and to determine the drug’s efficacy relative to that of other agents such as regorafenib (as only indirect comparisons of second-line treatments for HCC are available to date [31, 32]). Cost-effectiveness data for cabozantinib would also be of interest. In the meantime, current data indicate that cabozantinib prolongs survival and has acceptable tolerability in patients with HCC previously treated with sorafenib, making it a welcome additional treatment option for use in this setting.
Data Selection Cabozantinib: 189 records identified
Duplicates removed | 49 |
Excluded during initial screening (e.g. press releases; news reports; not relevant drug/indication; preclinical study; reviews; case reports; not randomized trial) | 102 |
Excluded during writing (e.g. reviews; duplicate data; small patient number; nonrandomized/phase 1/2 trials) | 4 |
Cited efficacy/tolerability articles | 12 |
Cited articles not efficacy/tolerability | 22 |
Search Strategy: EMBASE, MEDLINE and PubMed from 1946 to present. Clinical trial registries/databases and websites were also searched for relevant data. Key words were cabozantinib, XL184, Cabometyx, hepatocellular carcinoma, HCC. Records were limited to those in English language. Searches last updated 25 January 2019. | |
References
Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Ghouri YA, Mian I, Rowe JH. Review of hepatocellular carcinoma: epidemiology, etiology, and carcinogenesis. J Carcinog. 2017;16:1.
Vogel A, Cervantes A, Chau I, et al. Hepatocellular carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018; 29(Suppl 4):iv238–55.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN Guidelines)—hepatobiliary cancers [version 3.2018]. 2018. https://www.nccn.org/professionals/physician_gls/pdf/hepatobiliary.pdf Accessed 1 Feb 2019.
Desai JR, Ochoa S, Prins PA, et al. Systemic therapy for advanced hepatocellular carcinoma: an update. J Gastrointest Oncol. 2017;8(2):243–55.
European Association for the Study of the Liver. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236.
Raoul JL, Kudo M, Finn RS, et al. Systemic therapy for intermediate and advanced hepatocellular carcinoma: sorafenib and beyond. Cancer Treat Rev. 2018;68:16–24.
Exelixis Inc. Cabometyx® (cabozantinib) tablets for oral use: US prescribing information. 2019. https://cabometyx.com/resources. Accessed 15 Jan 2019.
Ipsen Pharma. Cabometyx film-coated tablets: EU summary of product characteristics. 2019. https://www.ema.europa.eu. Accessed 4 Feb 2019.
Yakes FM, Chen J, Tan J, et al. Cabozantinib (XL184), a novel MET and VEGFR2 inhibitor, simultaneously suppresses metastasis, angiogenesis, and tumor growth. Mol Cancer Ther. 2011;10(12):2298–308.
Xiang Q, Chen W, Ren M, et al. Cabozantinib suppresses tumor growth and metastasis in hepatocellular carcinoma by a dual blockade of VEGFR2 and MET. Clin Cancer Res. 2014;20(11):2959–70.
Nguyen L, Benrimoh N, Xie Y, et al. Pharmacokinetics of cabozantinib tablet and capsule formulations in healthy adults. Anticancer Drugs. 2016;27(7):669–78.
Nguyen L, Holland J, Mamelok R, et al. Evaluation of the effect of food and gastric pH on the single-dose pharmacokinetics of cabozantinib in healthy adult subjects. J Clin Pharmacol. 2015;55(11):1293–302.
Nguyen L, Holland J, Ramies DA, et al. Effect of renal and hepatic impairment on the pharmacokinetics of cabozantinib. J Clin Pharmacol. 2016;56(9):1130–40.
Nguyen L, Holland J, Miles D, et al. Pharmacokinetic (PK) drug interaction studies of cabozantinib: effect of CYP3A inducer rifampin and inhibitor ketoconazole on cabozantinib plasma PK and effect of cabozantinib on CYP2C8 probe substrate rosiglitazone plasma PK. J Clin Pharmacol. 2015;55(9):1012–23.
Abou-Alfa GK, Meyer T, Cheng AL, et al. Cabozantinib in patients with advanced and progressing hepatocellular carcinoma. N Engl J Med. 2018;379(1):54–63.
Schoffski P, Gordon M, Smith DC, et al. Phase II randomised discontinuation trial of cabozantinib in patients with advanced solid tumours. Eur J Cancer. 2017;86:296–304.
Kelley RK, Verslype C, Cohn AL, et al. Cabozantinib in hepatocellular carcinoma: results of a phase 2 placebo-controlled randomized discontinuation study. Ann Oncol. 2017;28(3):528–34.
Merle P, Rimassa L, Ryoo B, et al. Assessment of tumor response, AFP response, and time to progression in the phase 3 CELESTIAL trial of cabozantinib versus placebo in advanced hepatocellular carcinoma (HCC) [abstract no. O-011]. Ann Oncol. 2018;29(Suppl 5).
Meyer T, Baron A, Gordan J, et al. Outcomes in patients (pts) with hepatitis B virus (HBV) in the phase 3 CELESTIAL trial of cabozantinib (C) versus placebo (P) in advanced hepatocellular carcinoma (HCC). [abstract no. 0-012]. In: International Liver Cancer Association Annual Meeting. 2018.
Blanc JF, Meyer T, Cheng AL, et al. Assessment of disease burden in the phase III CELESTIAL trial of cabozantinib (C) versus placebo (P) in advanced hepatocellular carcinoma (HCC) [abstract no. 703P plus poster]. Ann Oncol. 2018;29(Suppl 8).
Rimassa L, Cicin I, Blanc JF, et al. Outcomes based on age in the phase 3 CELESTIAL trial of cabozantinib (C) versus placebo (P) in patients (pts) with advanced hepatocellular carcinoma (HCC) [abstract no. 4090]. J Clin Oncol. 2018;36(Suppl).
Kelley R, El-Khoueiry A, Meyer T, et al. Outcomes by baseline alpha-fetoprotein (AFP) levels in the phase III CELESTIAL trial of cabozantinib (C) versus placebo (P) in previously treated advanced hepatocellular carcinoma (HCC). [abstract no. 702P plus poster]. Ann Oncol. 2018;29(Suppl 8).
Yau T, Cheng AL, Meyer T, et al. Outcomes by prior transarterial chemoembolization (TACE) in the phase III CELESTIAL trial of cabozantinib (C) versus placebo (P) in patients (pts) with advanced hepatocellular carcinoma (HCC) [abstract no. 704P plus poster]. Ann Oncol. 2018;29(Suppl 8).
Kelley RK, Ryoo BY, Merle P, et al. Outcomes in patients (pts) who had received sorafenib (S) as the only prior systemic therapy in the phase 3 CELESTIAL trial of cabozantinib (C) versus placebo (P) in advanced hepatocellular carcinoma (HCC). [abstract no. 4088]. J Clin Oncol. 2018;36(Suppl).
Zhou L, Liu XD, Sun M, et al. Targeting MET and AXL overcomes resistance to sunitinib therapy in renal cell carcinoma. Oncogene. 2016;35(21):2687–97.
Shojaei F, Lee JH, Simmons BH, et al. HGF/c-Met acts as an alternative angiogenic pathway in sunitinib-resistant tumors. Cancer Res. 2010;70(24):10090–100.
Kudo M. Cabozantinib as a second-line agent in advanced hepatocellular carcinoma. Liver Cancer. 2018;7(2):123–33.
Ueki T, Fujimoto J, Suzuki T, et al. Expression of hepatocyte growth factor and its receptor, the c-met proto-oncogene, in hepatocellular carcinoma. Hepatology. 1997;25(3):619–23.
Liu J, Wang K, Yan Z, et al. Axl expression stratifies patients with poor prognosis after hepatectomy for hepatocellular carcinoma. PLoS ONE. 2016;11(5):e0154767.
Bakouny Z, Assi T, El Rassy E, et al. Second-line treatments of advanced hepatocellular carcinoma: systematic review and network meta-analysis of randomized controlled trials. J Clin Gastroenterol. 2018. https://doi.org/10.1097/mcg.0000000000001160.
Roskell N, Gregory J, Wisniewski T, et al. Indirect treatment comparisons of nivolumab versus regorafenib, cabozantinib and best supportive care after treatment with sorafenib for hepatocellular carcinoma [poster no. PCN17]. In: ISPOR Europe conference. 2018.
Acknowledgements
During the peer review process, the marketing authorization holders of cabozantinib (Exelixis and Ipsen) were also offered the opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflict of interest
Emma Deeks is a salaried employee of Adis/Springer, is responsible for the article content and declares no relevant conflicts of interest.
Additional information
The manuscript was reviewed by:J. Edeline, Medical Oncology Department, Centre Eugène Marquis, Rennes, France; M. Peck-Radosavljevic, Department of Internal Medicine and Gastroenterology, Hepatology, Endocrinology, Rheumatology and Nephrology, Central Emergency Medicine, Klinikum Klagenfurt am Wörthersee, Klagenfurt, Austria; L. Rimassa, Medical Oncology and Hematology Unit, Humanitas Clinical and Research Center, Milan, Italy.
Rights and permissions
About this article
Cite this article
Deeks, E.D. Cabozantinib: A Review in Advanced Hepatocellular Carcinoma. Targ Oncol 14, 107–113 (2019). https://doi.org/10.1007/s11523-019-00622-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-019-00622-y