Abstract
Cerebral autoregulation (CA) was assessed by chaotic analysis based on mean arterial blood pressure (MABP) and mean cerebral blood flow velocity (MCBFV) in 19 diabetics with autonomic neuropathy (AN) and 11 age-matched normal subjects. MABP in diabetics dropped significantly in response to tilting (91.6 ± 14.9 vs. 74.1 ± 13.4 mmHg, P < 0.05). Valsalva ratio of heart rate was reduced in diabetics compared to normal (1.1 ± 0.1 vs. 1.5 ± 0.2, P < 0.05). It indicated AN affects the vasomotor tone of peripheral vessels and baroreflex. Nonlinear results showed higher correlation dimension values of MABP and MCBFV in diabetics compared to normal, especially MABP (3.7 ± 2.3 vs. 2.0 ± 0.8, P < 0.05). It indicated CA is more complicated in diabetics. The lower Lyapunov exponent and the higher Kolmogorov entropy values in diabetics indicated less predictable behavior and higher chaotic degree. This study suggests impaired autoregulation would be more chaotic and less predictable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
According to literature, diabetes mellitus is a chronic disease that occurs when the body does not produce enough insulin (type 1) or cannot effectively use the insulin (type 2). Most diabetics are type 2 that have no symptoms and are diagnosed after many years of onset leading to serious condition with high long-term morbidity and mortality rates in the world (website:http://www.who.int/en/). Diabetic autonomic neuropathy is probably the most common complication of diabetes that can cause vasomotor and cardiovagal dysfunction, the major risk factors for mortality of diabetics. Disturbance of cerebral autoregulation (CA) due to diabetic autonomic dysfunction is one of the important factors to cause cerebral diseases and it has been indicated that the diabetic autonomic failure would result in the impairment of CA [12, 28]. CA is a feedback mechanism, which maintains cerebral blood flow in a constant level despite change of blood pressure [1]. Regular CA shows the property of flow autoregulation, whereby CBF tends to remain relatively constant despite changes in cerebral perfusion pressure (CPP) within the limits of 50–150 mmHg [4, 18, 26, 35]. The limits of autoregulation reflect the points at which vasomotor adjustments are exhausted and cerebral vascular resistance cannot either increase or decrease further to regulate cerebral blood flow. Cerebral blood flow tends to follow changes in CPP outside these limits and the homeostatic protection of CA is therefore lost [31]. Although CA has been investigated by using time and frequency domain analysis methods [10, 11, 20, 37, 42] based on arterial blood pressure (ABP) and cerebral blood flow velocity (CBFV), CA is more a concept rather than a physically measurable entity [31]. Autoregulatory index (ARI) is one of the methods generated by CBFV and ABP values to evaluate CA and it revealed aging does not affect CA [5, 15, 31, 34]. Phase analysis using time-domain cross-correlation function (CCF) to assess the CA showed the relationship between ABP and CBFV [7, 10, 11, 30, 33, 36]. Spectral and transfer function analyses of ABP and CBFV performed by fast Fourier transform (FFT) in normal subjects [14, 49] and autonomic failure patients [3] to observe the fluctuation of CA system. However, these methods are to analyze the dynamic relationship between ABP and CBFV linearly and it might ignore the nonlinear properties of CA.
Because CBF remains constant despite CPP changes, the region in this constant level is nonlinear. Some useful nonlinear information maybe missed and cannot be characterized by using linear analysis. Therefore, it might be beneficial to analyze CA using nonlinear methods. Panerai et al. used a second-order mathematical linear model and nonlinear Volterra-Wiener moving-average approach to model human dynamic CA [32]. Mitsis et al. applied the Laguerre-Volterra network methodology to model nonlinear systems for analyzing dynamic CA in human under orthostatic stress [29]. In addition, chaos theorem, the nonlinear approach, has been applied to many physiological studies, such as heart rate variability (HRV) [6, 13, 23, 48], electroencephalograph (EEG), respiratory rhythm, speech recognition, blood pressure, and cardiovascular system [17, 22, 43, 45, 46]. They provided the chaotic nature in physiological systems. Nevertheless, nonlinear dynamic CA in diabetics dealt with chaotic analysis was still rarely discussed.
In this study, the chaotic analysis will be implemented to assess dynamic CA in diabetics by three nonlinear measures, correlation dimension (CD), Lyapunov exponent (LE), and Kolmogorov entropy (K2). CD focuses on the system’s complexity. LE quantifies the sensitivity of the system to initial conditions, while the K2 metric evaluates the degree of chaos in the system. The main purpose of this study is to investigate and compare the nonlinear components of CA from chaotic analysis of mean arterial blood pressure (MABP) and mean cerebral blood flow velocity (MCBFV) in normal subjects and diabetics with autonomic neuropathy. It is expected to be a tool to predict the CA in diabetes and possible cardiovascular outcome in clinical practice. Because autonomic nervous system was impaired in our diabetics, it affected vasomotor control of peripheral and brain vessels and reduced baroreflex sensitivity. By using the parameters of chaotic analysis to quantify CA, we expect that normal autoregulation system would tend to lower chaos and higher regular, predictable behavior of the system to initial conditions, but impaired autoregulation would be more chaotic and less predictable in terms of chaotic analysis.
2 Methods
2.1 Subjects and measurements
There were two groups of subjects recruited in this study, i.e., 19 diabetic autonomic neuropathy (63.7 ± 11.0 years, 12 males) and 11 age-matched healthy subjects (57.4 ± 8.4 years, 8 males). All subjects gave their informed consent prior to entry to the study and it had been approved by the Research Ethics Committee of Cheng-Ching General Hospital. The diabetics took one or two oral hypoglycemic drugs such as Sulfonylureas and Metformin. Proceeding from a consensus conference in 1992 recommended that three tests (R-R variation, Valsalva maneuver, and postural blood pressure testing) could be used for longitudinal testing of the cardiovascular autonomic system. The determination of the presence of prominent autonomic neuropathy was based on a battery of autonomic reflex tests (more than two abnormal response in the following tests: deep breathing HRV, Valsalva maneuver, skin sympathetic response, and postural blood pressure test). The healthy subjects were included only if they had no history of cardiovascular disease, heart problems, hypertension, migraine, epilepsy, cerebral aneurysm, intracerebral bleeding or other pre-existing neurological conditions. None of the subjects were receiving any medication during the period of the study. The diabetics have no stroke history and their blood pressure is similar to that in controls in supine position. Subjects were investigated on a tilt-table that enabled a motor-driven change from a supine to an upright position 75° within 4 s. Data acquisition was started after a 10-min relaxation in supine position. Spontaneous ABP and CBFV were recorded simultaneously to PC for off-line analysis. CBFV was measured in the middle cerebral artery using transcranial Doppler ultrasound (TCD, EME TC2020, Nicolet Instruments, Warwick, UK) in conjunction with a 5-MHz transducer fixed over the temporal bones by an elastic headband. Continuous ABP recordings were obtained through the Finapres (Model 2300, Ohmeda, Englewood, CO) device with the cuff attached to the middle finger of the right hand. The acquisition periods were approximately 5 min in both the supine and 75° head-up tilt positions by a self-developed data acquisition system. During the period of data acquiring, the middle finger of the right hand was on the arm-table, which always keeps the same amplitude and position with that of the heart. The personal computer combined with a general-purpose data acquisition board and LabVIEW environment for acquiring signals correctly was developed in our previous study [9]. The sampling rate to acquire the analog data from TCD and Finapres was adjustable in this system. In our experiments, the sampling rate is set to 60 Hz.
The Finapres device was fully automated. It consists of a finger cuff with an infrared transmission plethysmograph, a servo control box, and a monitor unit. The blood volume under an inflatable finger cuff was measured using an infrared plethysmograph, and kept constant to a set point value by controlling the cuff pressure in response to the volume changes in the finger artery. A proper volume-clamped set point was established and adjusted at regular intervals using a built-in servo adjustment mechanism. However, it displays too great a variability [24] and this procedure interrupted the blood pressure recording (usually for 2–3 beats every 70 beats). We called the artifacts caused by the regular servo adjustment in the continuously acquired pulse signal “servo components”. In our previous study [8], we used a personal computer combined with a general-purpose data acquisition board and LabVIEW environment to develop techniques for acquiring signals correctly from a Finapres monitor.
2.2 Nonlinear analysis
Three nonlinear parameters, correlation dimension (CD), Lyapunov exponent (LE), and Kolmogorov entropy (K2) [16, 19], were calculated from the MABP and MCBFV segments to quantify chaos in blood pressure and cerebral blood flow velocity signals. The signals should be reconstructed from the time series before measuring the chaotic properties to determine the signal complexity and regularity. A new coordinate system called the phase space was used to reconstruct an attractor. The phase space is a coordinate system that expresses the behavior of a dynamic system, which is blood pressure or cerebral blood flow in this study. In the phase space, the dynamic system behavior (trajectory or orbit) converges into the stationary state, called the attractor. Because the number of phase space coordinates cannot be calculated directly from the time series data, it is necessary to reconstruct the n-dimensional phase space from a single time series measurement record. The n-dimensional attractor can be reconstructed from one-dimension time series projected data using the delay embedding method. The n-dimensional vector is constructed as follows.
where X(t) is the newly reconstructed n-dimensional vector. x(t) can be MABP or MCBFV signals in this study. τ is the delay time, dm is an embedded reconstructed phase space dimension. An example of MABP that reconstructs a two-dimensional attractor is illustrated in Fig. 1. A typical sample of MABP in normal subjects to reconstruct a two-dimensional attractors are illustrated in Fig. 2.
2.2.1 Correlation dimension
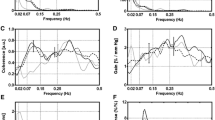
Correlation dimension focuses on the system’s complexity. The correlation function can be calculated using the distances between each pair of points in the set of N points. An MABP example is shown in Fig. 3.
The correlation function is calculated from the reconstructed vectors using the embedding algorithm as follows.
where C d (R) is correlation function, N the total number of time series in MABP in this study, H E Heaviside step function, H E = 1, if R−| MABP i − MABP j | ≥ 0, H E = 0, otherwise, and R radius. Where the distance between MABP i and MABP j is calculated using the Euclidean distance measure, \( \left| {{\text{MABP}}_i - {\text{MABP}}_j } \right| = \left[ {\left( {x_{i,1} - x_{j,1} } \right)^2 + \left( {x_{i,2} - x_{j,2} } \right)^2 +\cdots+\left( {x_{i,dm} - x_{j,dm} } \right)^2 } \right]^{\frac{1} {2}} . \) Because CD is not known initially, a series of computations that gradually increase the embedding dimension must be performed until the slope becomes stable. Figure 4 illustrates the CD that is estimated from the slope by plotting C d (R) versus R. A typical sample, C d (R) versus R plotting, for each of MABP is illustrated in Fig. 5.
2.2.2 Lyapunov exponent
Lyapunov exponent quantifies the sensitivity of the system to initial conditions. It is an important feature of chaotic systems and describes how small changes in the state of a system grow at an exponential rate and eventually dominate the behavior. LE is defined as the long time average exponential rates of divergence of nearby states. An example of MABP showing how the LE is calculated is illustrated in Fig. 6. Assume that the initial time is t and t = 0, which the distance between the two points on a trajectory and nearby trajectory are d(0). After a time interval t, the initial length will evolve into length d(t). The sequence of differences between d(t) and d(0) is assumed to increases exponentially. Thus, we can write
where λ is LE. A system is chaotic if the system has a positive value of LE. The larger value of positive LE, the more chaotic the system becomes. A system is regular if that LE value of the system is zero or negative. A system has n LE values for an n-dimensional attractor.
2.2.3 Kolmogorov entropy
Kolmogorov entropy metric evaluates the degree of chaos in the system, or the average rate at which information is generated by the system, or equivalently, the rate at which current information about the system is lost. Assume that the starting information, entropy, is S(t 1), after a time interval t 2 − t 1, the information becomes S(t 2). The change in information is K(t 2 − t 1). Thus, we can write: S(t 2) = S(t 1) + K(t 2 − t 1). Certainly, S(t 1) > S(t 2), so K(t 2 − t 1) = S(t 1) − S(t 2). Assume S(t 1) = lnC d (R), S(t 2) = lnC d+1(R). C d (R) is the correlation function of MABP or MCBFV. The equation for K2 is calculated as follows.
when K2 = 0, the system is regular; K2 = ∞, the system is random; K2 > 0, and finite, the system has chaotic behavior.
3 Results
3.1 Linear analysis results [21]
The MABP signal in the finger was acquired by using Finapres. The MCBFV signal of the middle cerebral artery was acquired by using TCD ultrasound. Both values were measured continuously during supine and head-up tilt positions for 5 min in diabetics and normal subjects. Two hundred and fifty six points were acquired for each position. Typical MABP and MCBFV signals for a normotensive subject during supine and head-up tilt positions are represented in Fig. 7a, b. Typical results shown in Fig. 7c, d indicate that both MABP and MCBFV for patients with diabetic autonomic neuropathy decrease in response to head-up tilt. However, MABP and MCBFV for normal subjects revealed no obvious difference in both the supine and upright positions. Valsalva ratio of heart rate was reduced significantly in diabetics as compared to normal subjects (1.1 ± 0.1 vs. 1.5 ± 0.2, P < 0.05). The results showed in Table 1 stand for mean value of each group and it could be a tendency in each group. However, it probably would not be each individual’s actual condition because some standard deviations in diabetics are larger.
Typical MABP and MCBFV signal samples in normal subjects and diabetics during supine and upright positions were shown in Fig. 7. The scatter plots shown in Fig. 8a, b represent the relative location change of (MABP, MCBFV) pair during the recording period in normal subjects and diabetics, respectively. (MABP, MCBFV) pairs in upright position are with cross symbols and in supine position are with square symbols. Figure 8a shows the cross and square symbols are not separated. It indicated the change of positions would not alter the locations of symbols for the typical normal subject. On the other hand, Fig. 8b shows the cross and square symbols are well separated for the typical diabetic while the positions changed which is different from that in normal persons.
a The scatter plot shows the (MABP, MCBFV) pair in the typical normal subject. b The scatter plot shows the (MABP, MCBFV) pair in the typical diabetic. The square stands for data in supine position and the cross stands for data in upright position. The solid line is connected the centers of data in supine and tilting groups
3.2 Nonlinear chaotic analysis results
The results revealed that the MABP CD values in diabetics decreased significantly in response to head-up tilt (3.7 ± 2.3 vs. 2.1 ± 1.2, P < 0.05). The MABP CD values of diabetics in supine position were significantly higher as compared to normal subjects (3.7 ± 2.3 vs. 2.0 ± 0.8, P < 0.05). In addition, the MABP correlation function characteristics are similar to that for MCBFV. However, the MCBFV CD showed no obvious change. MABP LE values in diabetics were significantly lower than that in normal subjects during supine position (1.0 ± 0.4 vs. 1.7 ± 1.0, P < 0.05) and MCBFV LE values in diabetics decreased significantly during supine to head-up tilt positions (1.1 ± 0.3 vs. 0.8 ± 0.4, P < 0.05). The MCBFV K2 values for diabetic were significantly higher during upright position as compared to normal subjects (3.3 ± 0.6 vs. 2.8 ± 0.5, P < 0.05).
4 Discussion
The linear analysis results indicated that the values of MABP and MCBFV in diabetics decreased more than that in normal subjects in response to head-up tilt. It might be speculated that due to the effect of diabetic autonomic neuropathy that cannot maintain blood pressure and cerebral blood flow velocity stable within a period of short time. Based on the results of (MABP, MCBFV) pairs in response to head-up tilt, the scatter plot revealed that the (MABP, MCBFV) pairs in diabetics were separated into two groups distinctly but not in normal subjects. It could be another evidence to reveal that diabetics cannot maintain the relationship between MABP and MCBFV constant because of the influence of diabetic autonomic neuropathy on CA. In contrast, normal subjects could keep the relationship stable due to regular CA function can maintain blood flow constant in the brain. The difference between diabetics and normal subjects might be due to the effect of CA function that CA works more well in normal subjects than that in diabetics. On the other hand, Valsalva ratio of heart rate was lower in diabetics as compared to normal. It might indicate that autonomic neuropathy would affect the vasomotor tone of peripheral vessels and baroreflex. As mentioned in the section of methods, the distance between MABP i and MABP j is calculated using the Euclidean distance measure, \( \left| {{\text{MABP}}_i - {\text{MABP}}_j } \right| = \left[ {\left( {x_{i,1} - x_{j,1} } \right)^2 + \left( {x_{i,2} - x_{j,2} } \right)^2 +\cdots+\left( {x_{i,dm} - x_{j,dm} } \right)^2 } \right]^{1/2}. \) Due to the minus in MABP, the brain-level blood pressure and the heart-level blood pressure will have the similar outcome in the estimation of Euclidean distances. Although the values are not hydrostatically corrected for brain level, the difference would be eliminated from the process of the chaotic analysis and it would not affect the results. Therefore, the blood pressure is heart-level but it still makes sense to brain-level for upright position in all subjects.
Correlation dimension describes the complexity of the time series. The higher the CD value, the more complex the system. Because CD values of MABP and MCBFV in diabetics were higher than that in normal subjects, it could reveal CA system in diabetics was more chaotic. Due to LE values in diabetics were lower than that in normal subjects and LE quantified the sensitivity of the system to the initial condition; it might be the reason that baroreflex control in diabetics is less active than that in normal subjects. The results agreed with published data [23] based on the values of CD and LE decreased in response to head-up tilt in present study. Comparing the change of CD and LE values in diabetics during supine to tilting positions, it could be speculated that tilting in diabetic autonomic neuropathy can alter the sensitivity effect of the initial condition in MCBFV but it cannot affect the complexity. In contrast, the effect of tilting on MABP could not alter the sensitivity of the initial condition, although the CD values changed significantly in diabetic autonomic neuropathy. On the other hand, posture change in normal subjects did not influence complexity and initial condition in both MABP and MCBFV obviously since the values of CD and LE values did not change significantly. K2 metric evaluates the degree of chaos in the system. The MCBFV K2 values in diabetics were significantly higher during upright position. It might indicate that the degree of chaos in diabetics was more than that in normal subjects during upright posture.
Due to diabetic autonomic neuropathy, the ability in diabetics to control blood pressure might not be as well as that in normal subjects. In this study, the CD and K2 values in diabetics are higher than that in normal subjects and it is significantly different between diabetics and normal subjects (P < 0.05). It might reveal the complexity and chaotic degree of MABP and MCBFV are higher in diabetics. The results are satisfied with the hypothesis in the section of introduction. Because LE values in all groups are positive, it indicates CA system is chaotic and nonlinear. Therefore, chaotic analysis can be suitable to analyze CA. In addition, previous study indicated chaotic nature existed in blood pressure [45]. The results in present study indicated both blood pressure and cerebral blood flow velocity were chaotic. Previous study showed that the complexity of blood pressure, correlation dimension, was reduced with aging and normative physiology has greater CD values (higher complexity) [25]. In our study, the CD values are higher in diabetics than that in normal subjects. The reason of the difference might be that age was the variable and the subjects are all healthy ones in previous study. In present study, autonomic failure is the variable and the age is matched between diabetics and normal subjects. Aging indeed is a factor might affect some physiological conditions. However, previous studies indicated that aging does not affect dynamic CA [5, 15, 47]. In our study, the age between two groups is matched (P > 0.05) so the age effect is considered and it would not affect the results.
There are several reasons that we recruited only 19 diabetics and 11 age-matched normal subjects in this study. As a matter of fact, it took almost 2 years to recruit about 100 diabetics. However, it was not easy to acquire the cerebral blood flow velocity signal from about 30–40% of the diabetics subjects due to the poor temporal window for TCD study. Moreover, only 10–20% of the diabetics suffered from prominent or severe autonomic failure. In addition, the daily outpatient number is limited due to health insurance policy. The source of subjects was restricted. Another limit was that the experiments were time-consuming. It needed 2 h to complete the experiment on one subject from the very beginning to the end. The other reason we had to take into consideration was age. Some of the subjects were too old to accomplish this study and it might affect the results. Therefore, only 19 diabetic autonomic neuropathy and 11 age-matched normal subjects were recruited in this study. Although the samples of diabetics and healthy subjects were not large, the statistical results may stand for some kind of tendency and prediction.
Most previous studies induced rapid changes in ABP pharmacologically by intravenous injection of pressor or antihypertensive agents or by physiological manipulations such as Valsalva maneuver that needs patient’s cooperation. In this study, Finapres and TCD were adopted to measure ABP and CBFV fluctuation non-invasively by tilt-table test that enabled a motor-driven change from supine to upright position. Studies on accuracy of Finapres system suggested little systematic bias versus intra-arterial pressure but substantial variability. The average Finapres mean arterial pressure bias was 2.1 mmHg (SD ± 8.6) with precision of 7.6 mmHg (SD ± 5.3) as depicted in [39]. Changes in the heart rate or in the arterial compliance may result in a disproportionate amplification of the arterial waveform during exercise [40]. Therefore, the subjects’ relaxing for 5–10 min in supine position to reduce the error measurement is necessary. Calibration against a reliable reference arterial pressure is desirable to obviate. In our previous study [8], we used a personal computer combined with a general-purpose data acquisition board and LabVIEW environment to develop techniques for acquiring signals correctly from a Finapres monitor. Consequentially, the Finapres device can provide an accurate estimate of blood pressure. TCD is based on the same physics and principles as those that apply to any sound-producing device. Ultrasound is a traveling wave of energy that has a frequency of more than 20,000 Hz. The variability of TCD flow velocity had been studied by several investigators. Sorteberg et al. [41] studied side-by-side and day-to-day variations in 35 normal adults in measurements taken 1 week apart. The standard deviation of the side-by-side variations was 7% for the middle cerebral artery. The standard deviation of the day-to-day variations was 12% for the middle cerebral artery. Maeda et al. [27] performed a validation study of TCD reproducibility in 15 patients evaluated twice by a single examiner and later by a second examiner on separate days. The overall intraobserver correlation for the middle cerebral artery was between 0.71–0.95. Vriens et al. [44] found the maximum interobserver difference in TCD-measured mean velocity to be 23 cm/s. The difference was less than 10 cm/s in 95% of cases. From these studies, it can be concluded that the relatively high consistency exists across TCD examinations [2]. However, lack of regular practice with the system would reduce the accuracy of measurements [38]. In our study, the examiner has the experience of operating the system for almost 10 years. Therefore, the measurement of transient change in ABP and CBFV results can be achieved by noninvasive, rapid, passive, and simple approaches and it can make the result more reliable and accurate. The results might be helpful for clinical practice in assessing the dynamic CA conditions and can provide critical information for physicians.
5 Conclusion
The study demonstrated the results of assessing CA by chaotic analysis. The significant difference of nonlinear parameters might stand for autonomic dysfunction in diabetics in response to head-up tilt. The results from this study revealed the nonlinear measures, CD, LE, and K2, are suitable parameters to explore the nonlinear components of dynamic CA in diabetic autonomic neuropathy. We speculate that regular autoregulation system would tend to lower chaos and predictable behavior to initial conditions but impaired autoregulation would be more chaotic and less predictable in terms of chaotic analysis.
References
Aaslid R, Lindegaard KF, Sorteberg W, Nornes H (1989) Cerebral autoregulation dynamics in humans. Stroke 20:45–52
Babikian VL, Wechsler LR (1999) Transcranial doppler ultrasonography, 2nd edn. Butterworth-Heinemann, Boston, pp 13–31
Blaber AP, Bondar RL, Stein F, Dunphy PT, Moradshahi P, Kassam MS, Freeman R (1997) Transfer function analysis of cerebral autoregulation dynamics in autonomic failure patients. Stroke 28:1686–1692
Busija DW (1993) Cerebral autoregulation. The regulation of cerebral blood flow. Chemical Rubber Company, Boca Raton, pp 45–64
Carey BJ, Eames PJ, Blake MJ, Panerai RB, Potter JF (2000) Dynamic cerebral autoregulation is unaffected by aging. Stroke 31:2895–2900
Carvajal R, Vallverdu M, Baranowski R, Chojnowski L, Rydlewska-Sadowska W, Jane R, Caminal P (1996) Non-linear analysis of heart rate variability in patients with hypertrophic cardiomyopathy. Annual international conference of the IEEE Engineering in Medicine and Biology Society, pp 1616–1617
Carvajal R, Zebrowski JJ, Vallverdu M, Baranowski R, Chojnowska L, Poplawska W, Caminal P (2002) Dimensional analysis of HRV in hypertrophic cardiomyopathy patients. IEEE Eng Med Biol Mag 21:71–78
Chiu CC, Yeh SJ, Lin RC (1996) Data acquisition and validation analysis for Finapres signals. J Med Biol Eng 15:47–58
Chiu CC, Yeh SJ, Chen CH (2000) Self-organizing arterial pressure pulse classification using neural network: theoretical considerations and clinical applicability. Comput Biol Med 30:71–88
Chiu CC, Yeh SJ (2001) Assessment of cerebral autoregulation using time-domain cross-correlation analysis. Comput Biol Med 30:471–480
Chiu CC, Yeh SJ, Liau BY (2005) Assessment of cerebral autoregulation dynamics in diabetics using time-domain cross-correlation analysis. J Med Biol Eng 25(2):53–59
Croughwell N, Lyth M, Quill TJ, Newman M, Greeley WJ, Smith LR, Reves JG (1990) Diabetic patients have abnormal cerebral autoregulation during cardiopulmonary bypass. Circulation 82(5 suppl):407–412
Czosnyka M, Smielewski P, Kirkpatrick P, Menon DK, Pickard JD (1996) Monitoring of cerebral autoregulation in head-injured patients. Stroke 27:1829–1834
Diehl RR, Linden D, Lücke D, Berlit P (1998) Spontaneous blood pressure oscillations and cerebral autoregulation. Clin Auton Res 8:7–12
Eames PJ, Blake MJ, Panerai RB, Potter JF (2003) Cerebral autoregulation indices are unimpaired by hypertension in middle aged and older people. Am J Hypertens 16:746–753
Grassberger P, Procaccia I (1983) Measuring the strangeness of strange attractors. Physica D 9:189–208
He TG, Zheng CX, Jiang DZ (1997) Detecting nonlinearity in multichannel epileptic EEG. IEEE Eng Med Biol Mag 3:1202–1204
Heistad DD, Kontos HA (1983) Cerebral circulation handbook of physiology 3. American Physiological Society, Bethesda, pp 137–82
Hilborn RC (2000) Chaos and nonlinear dynamics. 2nd edn. Oxford Press, New York
Jiang ZX, Chiu CC, Yeh SJ (2001) Using clustering analysis to the study of cerebral autoregulation. In: proceedings of the biomedical engineering society 2001 Annual Symposium, pp 639–641
Jiang ZX (2002) The assessment of dynamic cerebral autoregulation in diabetes using linear analysis. Master thesis, Institute of Automatic Control Engineering, Feng Chia University
Jiang JJ, Zhang Y (2002) Nonlinear dynamic analysis of speech from pathological subjects. Electron Lett 38(6):294–295
Kagiyama S, Tsukashima A, Abe I, Fujishima S, Ohmori S, Onaka U, Ohya Y, Fujii K, Tsuchihashi T, Fujishima M (1999) Chaos and spectral analysis of heart rate variability during head-up tilting in essential hypertension. J Auton Nerv Syst 76:153–158
Kermode JL, Davis NJ, Thompson WR (1989) Comparison of the Finapres blood pressure monitor with intra-arterial manometry during induction of anaesthesia. Anaesth Intensive Care 17(4):470–475
Kplan DK, Furman MI, Pincus SM, Ryan SM, Lipsitz LA, Goldberger AL (1991) Aging and the complexity of cardiovascular dynamics. Biophys J 59(4):945–949
Lassen NA (1959) Cerebral blood flow and oxygen consumption in man. Physiol Rev 39:183–238
Maeda H, Matsumoto M, Handa N, Hougaku H, Ogawa S, Itoh T, Tsukamoto Y, Kamada T (1993) Reactivity of cerebral blood flow to carbon dioxide in various types of ischemic cerebrovascular disease: evaluation by the transcranial Doppler method. Stroke 24:670–675
Mankovsky BN, Piolot R, Mankovsky OL, Ziegler D (2003) Impairment of cerebral autoregulation in diabetic patients with cardiovascular autonomic neuropathy and orthostatic hypotension. Diabet Med 20(2):119–126
Mitsis GD, Mahalingam A, Zhang R, Levine BD, Marmarelis VZ (2003) Nonlinear analysis of dynamic cerebral autoregulation in humans under orthostatic stress. In: proceedings of the 25th annual intenational conference of the IEEE EMBS, pp 398–401
Panerai RB, Kelsall AWR, Rennie JM, Evans DH (1996) Analysis of cerebral blood flow autoregulation in neonates. IEEE Trans Biomed Eng 43:779–788
Panerai RB (1998) Assessment of cerebral pressure autoregulation in humans—a review of measurement methods. Physiol Meas 19:305–338
Panerai RB, Dawson SL, Potter JF (1999) Linear and nonlinear analysis of human dynamic cerebral autoregulation. Am J Physiol 277:H1089–H1099
Panerai RB, Simpson DM, Deverson ST, Mathony P, Hayes P, Evans DH (2000) Multivariate dynamic analysis of cerebral blood flow regulation in humans. IEEE Trans Biomed Eng 47:419–423
Panerai RB, Eames PJ, Potter JF (2003) Variability of time-domain indices cerebral autoregulation. Physiol Meas 24:367–381
Paulson OB, Strandgaard S, Edvinson L (1990) Cerebral autoregulation. Cerebrovasc Brain Metab Rev 2:161–192
Steinmeier R, Bauhuf C, Subner UH, Bauer RD, Fahlbusch R, Laumer R, Bondar I (1996) Slow rhythmic oscillations of blood pressure, intracranial pressure, microcirculation and cerebral oxygenation. Stroke 27:2236–2243
Shen CL, Chiu CC, Yeh SJ (1998) The study of cerebral flow autoregulation based on the arterial blood pressure and cerebral blood flow velocity. In: proceedings of the biomedical engineering society, 1998 Annual Symposium, pp 293–294
Shen Q, Stuart J, Venkatesh B, Wallace J, Lipman J (1999) Inter observer variability of the transcranial Doppler ultrasound technique: impact of lack of practice on the accuracy of measurement. J Clin Monit Comput 15:179–184
Silke B, McAuley D (1998) Accuracy and precision of blood pressure determination with the Finapres: an overview using re-sampling statistics. J Hum Hypertens 12:403–409
Silke B, Spiers JP, Boyd S, Graham E, McParland G, Scott ME (1994) Evaluation of non-invasive blood pressure measurement by the Finapres method at rest and during dynamic exercise in subjects with cardiovascular insufficiency. Clin Auton Res 4(1–2):49–56
Sorteberg W, Langmoen IA, Lindegarrd KF, Nornes H (1990) Side-to-side differences and day-to-day variations of transcranial Doppler parameter in normal subjects. J Ultrasound Med 9:403–409
Tiecks FP, Lam AM, Aaslid DW, Newell DW (1995) Comparison of static and dynamic cerebral autoregulation measurements. Stroke 26:1014–1019
Tranquillo J, Ning T (1997) Chaotic behavior of respiration signals. In: proceedings of the IEEE 23rd northeast bioengineering conference, pp 50–51
Vriens EM, Kraaier V, Musbach M, Wieneke GH, van Huffelen AC (1989) Transcranial pulsed Doppler measurements of blood velocity in the middle cerebral artery: reference values at rest and during hyperventilation in healthy volunteers in relation to age and sex. Ultrasound Med Biol 15(1):1–8
Wagner CD, Persson PB (1998) Chaos in blood pressure control. Cardiovasc Res 31:380–387
Wagner CD, Persson PB (1998) Chaos in the cardiovascular system: an update. Cardiovasc Res 40:257–264
Yam AT, Lang EW, Lagopoulos J, Yip K, Griffith J, Mudaliar Y, Dorsch NWC (2005) Cerebral autoregulation and ageing. J Clin Neurosci 12(6):643–646
Zhang S, Reisman SS, Tapp WN, Zhang PZ (1993) Correlation dimension in heart rate variability. In: proceedings of the 1993 IEEE nineteenth annual northeast bioengineering conference, pp 11–12
Zhang R, Zuckerman JH, Giller CA, Levine BD (1998) Transfer function analysis of dynamic cerebral autoregulation in humans. Am J Physiol 274:H233–241
Acknowledgments
The authors would like to thank the National Science Council, Taiwan, ROC., for supporting this research under Contract No. NSC94-2213-E-035-045.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liau, BY., Yeh, SJ., Chiu, CC. et al. Dynamic cerebral autoregulation assessment using chaotic analysis in diabetic autonomic neuropathy. Med Bio Eng Comput 46, 1–9 (2008). https://doi.org/10.1007/s11517-007-0243-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-007-0243-5