Abstract
Purpose
Chronic intermittent hypoxia (CIH) is key pathological mechanism of obstructive sleep apnea (OSA), which induced cardiac dysfunction. Filamin c (FLNC) is a muscle-restricted isoform and predominantly expressed in muscle tissue. In this study, we utilized a recently developed CIH rat model to mimic OSA, investigated the expression of FLNC in cardiomyocytes, and examined the correlations of FLNC with active caspase-3 to ascertain whether FLNC regulates the survival of cardiomyocytes.
Methods
Forty Sprague-Dawley rats were randomly divided into normoxia and CIH groups. All rats were exposed either to normoxia or CIH 8 h daily for 6 weeks. Echocardiogram and HE staining were used to examine cardiac pathology, structure, and function. Body weight, heart weight, and blood gas values were recorded, respectively. The FLNC, Bax, Bcl-2, BNIP 3, and active caspase-3 proteins were detected by western blot; FLNC was examined by immunohistochemistry and immunofluorescence. Association of FLNC with cardiomyocyte apoptosis was detected by immunofluorescence.
Results
CIH induced cardiac injuries and caused arterial blood gas disorder. FLNC significantly increased in CIH-induced cardiomyocytes than that in normoxia tissues. Pro-apoptotic BNIP 3 and Bax proteins were significantly increased in CIH, whereas anti-apoptotic member Bcl-2 was decreased. Active caspase-3, a universal marker of apoptosis, was significantly increased in CIH group. Co-localizations of FLNC and active caspase-3 were observed in CIH group.
Conclusions
These results suggested FLNC is implicated in the pathogenesis of CIH-induced cardiomyocyte apoptosis, and FLNC may serve as a novel cardioprotective target for OSA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
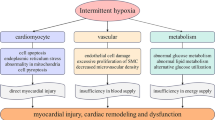
Obstructive sleep apnea (OSA), a common sleep and breath disease, is characterized by repetitive partial (hypopnea) or complete (apnea) upper airway collapse during sleep, leading to daytime sleepiness, sleep fragmentation, oxygen desaturation, arousal, and chronic intermittent hypoxia (CIH) [1]. CIH is a distinct pathological mechanism of OSA, which is recognized as an independent risk factor in cardiovascular pathogenesis during the development of OSA [2]. CIH had been reported to induce cardiac protection or cardiac damage in different studies with various conditions. During hypoxia, different cell types have been shown to induce apoptosis and cardiomyocytes produce large amounts of reactive oxygen species that contributed to cardiac injury, resulting in apoptotic cell death [3, 4]. Since the first CIH animal model was described by Fletcher in the early 1990s [5], it has been widely used to the study of OSA [6, 7]. In this study, we utilized a recently developed CIH rat model to mimic OSA, which summarizes the characteristics of OSA.
Apoptosis, known as programmed cell death, has been recognized as an important pathophysiological process in many disease states, and is implicated in the pathogenesis of different heart diseases [8, 9]. It has been revealed that cardiomyocyte apoptosis occurs in adult mammalian hearts of patients with cardiac disorders, including end-stage heart failure, dilated cardiomyopathy, myocardial infarction, and is recognized as a predictor of adverse outcomes in patients with cardiac diseases [10]. Cells undergoing apoptosis are induced by a variety of signaling pathways and release a series of apoptosis-associated proteins such as P53, Bax, Bcl-2, BNIP3, Slug, Msx1, and Bmp4, which may be responsible for cardiomyocyte apoptosis [11]. Improved myocardial cell survival and cardiac function after exposing to CIH are crucial to identify potential cardioprotective targets and develop effective therapies for OSA patients.
Filamins (FLNs) are mainly structural proteins that belong to an extended family of homodimeric actin-binding and actin-crosslinking proteins [12, 13]. The main function of FLNs is to cross-link actin filaments. It has also been shown that FLNs exert a significant part in cell signaling through the introduction of novel interactions or else by disrupting existing interactions [14, 15]. Over 90 proteins have been shown to bind to FLNs, including actin, receptors, cytoskeletal and cell adhesion proteins, transcription factors, ion channels, and intracellular signaling molecules [16, 17]. Acting as scaffolding proteins, FLNs are associated with many cellular stress responses, including hypoxia-related effects [18].
FLNs consist of three isoforms: the filamin A (FLNA), the filamin B (FLNB), and the filamin C (FLNC), which are differentially expressed in different cell types [13, 16]. Unlike FLNA and FLNB which are ubiquitously expressed, FLNC is a muscle-restricted isoform, which is predominantly expressed in muscle tissue [19]. FLNC acts many significant parts in a variety of pathophysiological conditions. FLNC plays a crucial role in cancer metastasis, downregulation impaired cancer cell proliferation, inhibits cell migration, and promotes apoptosis [20], and opposite consequence in other study was observed [21]. In addition, high FLNC is associated with better prognosis of prostate cancer, leukemia, and breast cancer patients [22]. In cardiac disease studies, FLNC as a candidate gene is involved in chronic heart failure, arrhythmias, conduction blocks, and cardiomyopathy, frequently resulting in sudden cardiac death [23,24,25].
However, the biological function of FLNC in cardiomyocyte apoptosis after CIH is unknown. Therefore, understanding the mechanisms of FLNC in CIH-induced cardiomyocyte apoptosis has a critical effect on the development of effective therapeutics for OSA patients.
Materials and methods
Rat model
Forty Sprague-Dawley (SD) rats (initial BW, (200 ± 10) g; age, 8 weeks) from the Laboratory Animal Center of Nanjing Medical University were randomly divided into the following two groups: the normoxia group and the CIH group. Water and food were available ad libitum. All rats were exposed either to normoxia or CIH 8 h daily for 6 weeks. CIH rats were exposed to intermittent hypoxia chamber with cycling changes of the hypoxic conditions (2 min) 8 h a day (from 8 a.m. to 4 p.m.). The protocol of this study was approved by the Jiangsu Province Animal Care ethics committee and performed in accordance with the Animal Management Rule of the People’s Republic of China and the Care and Use of the Laboratory Animals Guide of the Nanjing Medical University.
Tissue preparation
At the end of study, all rat cardiac functions were assessed by VisualSonics Vevo 2100 ultrasound system (VisualSonics, Canada). To analyze the arterial blood gas value, a blood gas analyzer was performed on two groups. The heart weight (HW) and body weight (BW) were evaluated for each rat. Ten hearts from each group were quickly stored in a − 80 °C refrigerator, and the other ten hearts were immersed in 4% paraformaldehyde for histological detection.
Histology evaluation of tissue sections
The hearts were harvested after CIH 6 weeks. The cardiac tissues were immersed in 10% formalin, fastened in paraffin, and sectioned at 7 μm. Then, the tissues were stained with hematoxylin and eosin (HE), and all photographs were assessed blindly and collected directly by a certified histocytopathologist.
Western blot analysis
Western blotting was performed as described previously [26]. Briefly, total heart tissue protein was then homogenized in lysis buffer containing 1% NP-40, pH 7.5, 5 mmol/l EDTA, 50 mmol/l Tris, 1% SDS, 1% Triton X-100, 1% sodium deoxycholate, 10 mg/ml aprotinin, 1 mmol/l PMSF, and 1 mg/ml leupeptin, then micro centrifuge at 10,000 rpm and 4 °C for 20 min to collect the supernatant. After protein concentrations were determined with a Bio-Rad protein assay (Bio-Rad, Hercules, CA, USA), the resulting supernatant was subjected to with SDS-polyacrylamide gel electrophoresis (PAGE). Proteins were transferred to polyvinylidene difluoride filter (PVDF) membranes (Millipore) by a transfer apparatus at 350 mA for 2.5 h. The membranes were blocked with 5% nonfat milk in Tris-buffered saline with Tween (TBST) at room temperature for 2 h. The filters were immediately rinsed three times in TBST and then incubated overnight with primary antibodies against filamin C (FLNC) (anti-mouse, 1:600; Santa Cruz), BNIP 3 (anti-rabbit, 1:800; Sigma), Bcl-2 (anti-mouse, 1:800; Santa Cruz), Bax (anti-mouse, 1:800; Santa Cruz), or GAPDH (glyceraldehyde-3-phosphate dehydrogenase, anti-rabbit, 1:1000; Sigma) at 4 °C. Finally, the horseradish peroxidase-conjugated secondary antibody was added to filters for an additional 2 h, and the proteins were examined with an enhanced chemiluminescence detection system (ECL, Pierce Company, USA).
TUNEL assay
The sections were deparaffinized by immersion in xylene, rehydrated, and incubated in phosphate-buffered saline with 3% H2O2 to inactivate endogenous peroxidases. They were incubated with proteinase K (20 mg/ml) for 10 min, then washed in phosphate-buffered saline, and incubated with terminal deoxynucleotidyl transferase and fluorescein isothiocyanate-dUTP for 60 min at 37 °C using an apoptosis detection kit. The mean number of TUNEL-positive cells was counted in at least five randomly chosen fields in each group. All counts were performed by two independent individuals.
Immunohistochemistry
Immunohistochemistry was performed as our previous studies [27]. In short, all of the sections were blocked with 10% goat serum with 1% (w/v) bovine serum albumin (BSA) and 0.3% Triton X-100 at room temperature (RT) for 2 h and was incubated overnight at 4 °C with anti-FLNC antibody (anti-mouse, 1:100; Santa Cruz), then by incubation in a biotinylated secondary antibody. Immunostaining was visualized with DAB (Vector Laboratories). The stained sections were examined with Leica confocal microscope or Leica fluorescence microscope (Germany). Same exposure time and light intensity were applied to all photographs.
Double immunofluorescent staining
According to our previous studies [28], double immunofluorescent staining was used to investigate the heart tissues. Briefly, the slides were incubated with polyclonal antibody specific for FLNC (Santa Cruz, 1:50) and different markers as follows: active caspase-3 (Santa Cruz, 1:100) and α-actinin (a marker of heart, Sigma, 1:100) overnight at 4 °C. After three washes of 15 min each in PBS, a mixture of DAPI and FITC- and Cy3-conjugated secondary antibodies was added in a dark room and incubated for 2 h at 4 °C. Images were collected by Leica fluorescence microscope (Germany). Same exposure time and light intensity were applied to all photographs.
Statistical analysis
Throughout the paper, all data were analyzed with SPSS 16.0 (SPSS Inc., USA). All values were expressed as the mean ± (SD). F test was used to compare variances. P value > 0.1 was considered to be variance equal, thus the T test is used accordingly. If not, the T test or the variable transformation or the rank sum test should be chosen. P value of less than 0.05 was considered to be statistically significant. Each experiment consisted of at least three replicates per condition.
Results
Cardiac changes of rats exposed to chronic intermittent hypoxia
Initial body weight (BW) of rats was about (200 ± 10) g in two groups. No difference in BW growth following 1 week, but difference was significant following 2 weeks. At the end of the study, BW of CIH was significantly reduced compared with the normoxia group (P < 0.0001, Fig. 1b). The heart weight (HW) was markedly increased following 6 weeks (P = 0.0159, Fig. 1c), significant cardiac hypertrophy was observed based on increased HW to BW (HW/BW) ratio (Fig. 1d).
Normoxia, normoxia group; CIH, chronic intermittent hypoxia group. a Body weight was significantly increased in two groups after 6 weeks. b Average body weight was a significant difference between normoxia and CIH groups after 2 weeks. c HW was markedly increased in two CIH group following 6 weeks. d HW/BW ratio was significantly increased in CIH group
Cardiopathic changes of rats after chronic intermittent hypoxia
To examine the possible cardiomyopathic alteration after CIH, we did a histopathological analysis of cardiomyocytes by hematoxylin and eosin (HE) staining (Fig. 2a). Cardiomyocytes were arranged regularly in normoxia control group, and ventricular myocardium was normal architecture with normal interstitial space (Fig. 2a). However, cardiomyocytes in CIH 6-week rats were disarrayed with some necrosis and edema. In addition, increased interstitial space and abnormal architecture were observed in rat hearts under CIH 6 weeks (Fig. 2a). These results indicated that CIH induced cardiac injuries (original magnification × 20).
a Representative examples of heart slice by HE staining (original magnification ×20). Compared with normal heart, cardiomyocytes in CIH rats were disarrayed with some edema and necrosis, and ventricular myocardium was abnormal architecture with increased interstitial space. b Echocardiographic alterations in two groups after CIH 6 weeks. Compared with the normoxia group, CIH caused left ventricle (LV) hypertrophy and remodeling, and decreased ejection fraction (EF) and fractional shortening (FS), resulting in cardiac dysfunction
Echocardiographic alterations of rats after chronic intermittent hypoxia
To examine the possible echocardiographic alteration after CIH 6 weeks, we performed echocardiography to study dynamic changes. The echocardiographic parameters of two groups are shown in Table 1. Echocardiography showed significant increase in left ventricular internal diameter in diastole (LVIDd), left ventricular internal diameter in systole (LVIDs), left ventricular posterior wall in systole (LVPWs), left ventricular posterior wall in diastole (LVPWd), and left ventricular (LV) mass, indicating LV hypertrophy, in CIH-exposed rats. Compared with the normoxia group, the fractional shortening (FS) and ejection fraction (EF) were significantly decreased in CIH group (Fig. 2b, Table 1). Taken together these results clearly demonstrated CIH caused cardiac dysfunction.
Arterial blood gas values under chronic intermittent hypoxia
Arterial blood was gathered at baseline (date not show) and under CIH. Arterial blood gases identified significant oxygen desaturation and hypoventilation in CIH 6-week rats (Table 2). The blood pO2 of rats was maintained between 95 and 100 mmHg in normoxia group (21% O2). In CIH group (6% O2), the lowest blood oxygen pO2 of rats was maintained between 51 and 60 mmHg. PH was significantly reduced in CIH, compared to the normoxia group. There was no significant difference in BE, Ca2+, Na+, and K+ between normoxia and CIH groups.
FLNC is upregulated in chronic intermittent hypoxia-induced cardiomyocytes
Western blot analysis was performed to examine the expression of FLNC at protein level in CIH-induced cardiomyocytes. As shown in Fig. 3a, compared to the normoxia group, the FLNC protein level was significantly higher in CIH group. Each experiment consisted of at least three replicates per condition. To identify the distribution of FLNC in CIH-induced cardiomyocytes, we performed immunohistochemistry experiments with anti-FLNC mouse monoclonal antibody. Representative examples of reactivity for FLNC were shown in Fig. 3b. In CIH rats, the staining of FLNC-positive cells was increased around the cardiomyocytes. In addition, the number of FLNC-positive cells measured between normoxia and CIH was consistent with our western blot results. These data indicated that FLNC had higher expression in CIH-induced cardiomyocytes than that in normoxia tissues.
a Western blot analysis shows the protein expression of FLNC in two groups. N or Normoxia, normoxia group; CIH, chronic intermittent hypoxia group. The expression of FLNC protein level was significantly higher in CIH group (P < 0.0001). b Representative immunohistochemical staining of FLNC in two groups (original magnification × 20). Black arrows mean FLNC-positive cells. Compared with little expression in normoxia group, FLNC expression was significantly increased in CIH groups (P < 0.0001)
Co-localizations of FLNC and α-actinin by double immunofluorescent staining
To further confirm the cell types expressing FLNC after CIH, double-labeling immunofluorescent staining was performed with the following cell-specific markers: α-actinin (a marker of cardiomyocytes; green) and DAPI (a marker of nucleus; blue). In the normoxia group, the expression of FLNC was low in cytoplasm of cardiomyocytes (date not shown). However, in the CIH group, the expression of FLNC was higher in cytoplasm of cardiomyocytes (Fig. 4a). To identify the proportion of myocardium-positive cells expressing FLNC, a minimum of 200 phenotype-specific marker-positive cells was counted between the normoxia and CIH groups (Fig. 4b).
Apoptotic response to chronic intermittent hypoxia
Cardiomyocytes of heart were stained using the TUNEL assay and observed by light microscopy. TUNEL assay showed the number of TUNEL-positive cells from the CIH group was significantly increased than that in the normoxia group (Fig. 5a). The test of several independent samples revealed that there were significant differences between normoxia and CIH groups (Fig. 5a). To further understand the occurrence of cardiac apoptosis induced by CIH, the protein levels of BNIP 3, BCL-2, and Bax were examined. Pro-apoptotic BNIP 3 and Bax proteins were significantly increased in CIH group (Fig. 5b), whereas anti-apoptotic member Bcl-2 was decreased (Fig. 5b). These results clearly indicated that CIH caused cardiomyocyte apoptosis.
a Representative TUNEL staining of cardiac sections from left ventricles in two groups (original magnification × 40). Compared with normoxia group, positive TUNEL reactivity was observed in CIH groups. Quantitative analysis of brown apoptotic cells between normoxia and CIH groups (P < 0.001). b The Bcl-2 family protein expression by western blot analysis. N or Normoxia, normoxia group; CIH, chronic intermittent hypoxia group. The expression of BNIP 3 and Bax proteins was significantly higher in CIH group, whereas Bcl-2 protein was significantly decreased. The data are represented as the mean ± SEM (*P < 0.0001, significantly different from the normoxia group)
FLNC was relevant to cardiomyocyte apoptosis
To further confirm the cardiomyocyte apoptosis, we did a protein analysis of active caspase-3 (a universal maker of apoptosis) by western blot. Compared with the normoxia group, the active caspase-3 protein level was significantly increased in CIH group (Fig. 6a, b). In addition, we performed double-labeling immunofluorescent staining of FLNC and active caspase-3 in rat cardiomyocytes after CIH to assess whether FLNC is associated with the cardiomyocyte apoptosis. Double-labeling immunofluorescent staining revealed that the co-localization of FLNC and active caspase-3 was observed after CIH (Fig. 6c). Therefore, we speculated that the increased expression of FLNC could regulate cell apoptosis in CIH-induced cardiomyocytes.
Association of FLNC with cardiomyocyte apoptosis after CIH. N or Normoxia, normoxia group; CIH, chronic intermittent hypoxia group. a The expression of active caspase-3 protein was significantly higher in CIH group. GAPDH was used as an internal control. b Tendency of active caspase-3 protein expression in two groups (P < 0.001). c The co-localization of FLNC with activate caspase-3 was observed in CIH-induced cardiomyocytes (original magnification × 40)
Discussion
In this study, we utilized a recently developed CIH rat model to mimic OSA, which summarizes the characteristics of OSA, convenient to investigate the pathophysiology of OSA, and found appropriate treatments. OSA is a common sleep and breathing disease, which affects 17% of women and 34% of men and is largely undiagnosed [29]. OSA is strongly linked to increased mortality cardiovascular diseases [2]. There exist many pathologic changes in cardiomyocytes of OSA patients. CIH is recognized as an independent risk factor in cardiovascular pathogenesis during the development of OSA [2]. CIH during sleeping hours has been proposed to contribute to the cardiac dysfunction, with multiple complex mechanisms, including induced cardiac inflammation [7], increased oxidative stress [30], and aggravated cardiomyocyte apoptosis [31]. In addition, CIH has been also shown to be implicated in sympathetic activation and hypertension in animal models, both of which could influence cardiac function [32]. CIH models are convenient to explore the chronic results of human disease development because of allowing animals to be exposed to hypoxia for a long period of time.
CIH has been shown to be aggravated cardiomyocyte apoptosis, which resulting in cardiac dysfunction. In this study, we observed significant apoptosis in the myocardium in the CIH group, as indicated by increased TUNEL-positive myocytes (Fig. 5). We also found CIH caused cellular death and structural changes by HE staining (Fig. 2), and caused cardiac dysfunction by echocardiography (Fig. 3). Apoptosis, also termed programmed cell death, is associated with the Bcl-2 family of proteins [33]. The Bcl-2 family is a kind of apoptosis-related genes; moreover, its expression and regulation are the key factors influencing apoptosis [34]. Bcl-2 and Bax proteins, members of the Bcl-2 family, have been reported to play an important role in response to apoptosis [35]. Bcl-2 is the anti-apoptotic member, but Bax is the pro-apoptotic member. Because of this, we examined the expression of Bcl-2 and Bax in cardiomyocytes after exposing to CIH. We observed pro-apoptotic Bax protein was significantly increased following CIH 6 weeks (Fig. 5), whereas anti-apoptotic member Bcl-2 was decreased after CIH 6 weeks (Fig. 5). BNIP3 is also a member of the Bcl-2 protein family [36]. Hypoxia-induced BNIP3 expressions are directly involved in cardiomyocyte apoptosis and cardiac remodeling [36, 37]. In our study, we demonstrated that pro-apoptotic BNIP 3 is upregulated during CIH (Fig. 5). In other words, increased expression of pro-apoptotic BNIP3 and Bax or deceased expression of anti-apoptotic Bcl-2 during hypoxic conditions indicated that CIH caused cardiomyocyte apoptosis. So we inferred that apoptosis plays a crucial role in cardiac dysfunction in CIH; however, its molecular mechanisms are still unclear.
FLNs are classically recognized as large cytoplasmic proteins that belong to an extended family of homodimeric actin-binding and actin-crosslinking proteins [12, 13]. FLNs are associated with many cellular stress responses, including hypoxia-related effects [18]. There are three members in the FLNs: FLNA and FLNB, which are ubiquitously expressed, and FLNC, a muscle-restricted isoform, which is predominantly expressed in muscle tissue [19].
FLNC plays a role in cancer metastasis; the expression of FLNC is directly involved in cancer cell apoptosis [20, 21]. In cardiac disease studies, FLNC as a candidate gene is involved in chronic heart failure, arrhythmias, conduction blocks, and cardiomyopathy, frequently resulting in sudden cardiac death [23,24,25]. However, the expression and function of FLNC in cardiomyocyte apoptosis after CIH are unknown. In the present study, we examined the expression of FLNC in cardiomyocytes after exposing to CIH. We demonstrated that FLNC had higher expression in CIH-induced cardiomyocytes than that in normoxia tissues (Figs. 4, 5, and 6). To understand whether high expression of FLNC could regulate apoptosis in CIH-induced cardiomyocytes, we examined the expression of active caspase-3 and the relationship between active caspase-3 and FLNC. Compared with the normoxia group, the active caspase-3 protein level was significantly increased in CIH group (Fig. 6a). Double-labeling immunofluorescent staining revealed that the co-localizations of FLNC and active caspase-3 were observed after CIH (Fig. 6b). Therefore, we speculated that the increased expression of FLNC could regulate cell apoptosis in CIH-induced cardiomyocytes.
In conclusion, our study demonstrated that in CIH model of OSA rat, CIH induced cardiomyocyte apoptosis, resulting in cardiac dysfunction. We also observed that FLNC expression is upregulated in CIH-induced cardiomyocytes, and this phenomenon is related to high expression of active caspase-3. These suggest that FLNC is implicated in the pathogenesis of CIH-induced cardiomyocyte apoptosis, and FLNC may serve as a novel cardioprotective target for OSA patients.
Limitations
Despite our compelling and novel findings, the study had limitations. This study was done in rat models and has some limitations, like all animal models of human disease. However, CIH is a distinct pathological mechanism of OSA, which is recognized as an independent risk factor in cardiovascular pathogenesis during the development of OSA. Therefore, establishing a reliable animal model of OSA is an important prerequisite for in-depth experimental studies. In our study, although there were no obvious evidences on “regulation” of cell survival or death, we examined the expression of BNIP 3, BCL-2, Bax, and active caspase-3 in normoxia group and CIH group, and the relationship between FLNC and active caspase-3 after CIH. In cardiac disease studies, FLNC as a candidate gene is involved in chronic heart failure, arrhythmias, conduction blocks, and cardiomyopathy, frequently resulting in sudden cardiac death [23,24,25]. These results directly or indirectly demonstrated that FLNC expression correlated with survival of cardiomyocytes in CIH.
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328(17):1230–1235. https://doi.org/10.1056/NEJM199304293281704
Javaheri S, Barbe F, Campos-Rodriguez F, Dempsey JA, Khayat R, Javaheri S, Malhotra A, Martinez-Garcia MA, Mehra R, Pack AI, Polotsky VY, Redline S, Somers VK (2017) Sleep apnea: types, mechanisms, and clinical cardiovascular consequences. J Am Coll Cardiol 69(7):841–858. https://doi.org/10.1016/j.jacc.2016.11.069
Oktay B, Akbal E, Firat H, Ardic S, Akdemir R, Kizilgun M (2008) Evaluation of the relationship between heart type fatty acid binding protein levels and the risk of cardiac damage in patients with obstructive sleep apnea syndrome. Sleep Breath 12(3):223–228. https://doi.org/10.1007/s11325-007-0167-1
Lee SD, Kuo WW, Wu CH, Lin YM, Lin JA, Lu MC, Yang AL, Liu JY, Wang SG, Liu CJ, Chen LM, Huang CY (2006) Effects of short- and long-term hypobaric hypoxia on Bcl2 family in rat heart. Int J Cardiol 108(3):376–384. https://doi.org/10.1016/j.ijcard.2005.05.046
Fletcher EC, Lesske J, Behm R, Miller CC 3rd, Stauss H, Unger T (1992) Carotid chemoreceptors, systemic blood pressure, and chronic episodic hypoxia mimicking sleep apnea. J Appl Physiol 72(5):1978–1984. https://doi.org/10.1152/jappl.1992.72.5.1978
Gozal D, Daniel JM, Dohanich GP (2001) Behavioral and anatomical correlates of chronic episodic hypoxia during sleep in the rat. J Neurosci 21(7):2442–2450
Wei Q, Bian Y, Yu F, Zhang Q, Zhang G, Li Y, Song S, Ren X, Tong J (2016) Chronic intermittent hypoxia induces cardiac inflammation and dysfunction in a rat obstructive sleep apnea model. J Biomed Res 30(6):490–495. https://doi.org/10.7555/JBR.30.20160110
Haunstetter A, Izumo S (1998) Apoptosis: basic mechanisms and implications for cardiovascular disease. Circ Res 82(11):1111–1129
Konstantinidis K, Whelan RS, Kitsis RN (2012) Mechanisms of cell death in heart disease. Arterioscler Thromb Vasc Biol 32(7):1552–1562. https://doi.org/10.1161/ATVBAHA.111.224915
Narula J, Pandey P, Arbustini E, Haider N, Narula N, Kolodgie FD, Dal Bello B, Semigran MJ, Bielsa-Masdeu A, Dec GW, Israels S, Ballester M, Virmani R, Saxena S, Kharbanda S (1999) Apoptosis in heart failure: release of cytochrome c from mitochondria and activation of caspase-3 in human cardiomyopathy. Proc Natl Acad Sci U S A 96(14):8144–8149
Cosentino K, Garcia-Saez AJ (2014) Mitochondrial alterations in apoptosis. Chem Phys Lipids 181:62–75. https://doi.org/10.1016/j.chemphyslip.2014.04.001
Razinia Z, Makela T, Ylanne J, Calderwood DA (2012) Filamins in mechanosensing and signaling. Annu Rev Biophys 41:227–246. https://doi.org/10.1146/annurev-biophys-050511-102252
Weihing RR (1985) The filamins: properties and functions. Can J Biochem Cell Biol 63(6):397–413. https://doi.org/10.1139/o85-059
van der Ven PF, Obermann WM, Lemke B, Gautel M, Weber K, Furst DO (2000) Characterization of muscle filamin isoforms suggests a possible role of gamma-filamin/ABP-L in sarcomeric Z-disc formation. Cell Motil Cytoskeleton 45(2):149–162. https://doi.org/10.1002/(SICI)1097-0169(200002)45:2<149::AID-CM6>3.0.CO;2-G
Feng Y, Walsh CA (2004) The many faces of filamin: a versatile molecular scaffold for cell motility and signalling. Nat Cell Biol 6(11):1034–1038. https://doi.org/10.1038/ncb1104-1034
van der Flier A, Sonnenberg A (2001) Structural and functional aspects of filamins. Biochim Biophys Acta 1538(2–3):99–117
Nakamura F, Stossel TP, Hartwig JH (2011) The filamins: organizers of cell structure and function. Cell Adhes Migr 5(2):160–169
Hastie LE, Patton WF, Hechtman HB, Shepro D (1997) H2O2-induced filamin redistribution in endothelial cells is modulated by the cyclic AMP-dependent protein kinase pathway. J Cell Physiol 172(3):373–381. https://doi.org/10.1002/(SICI)1097-4652(199709)172:3<373::AID-JCP11>3.0.CO;2-7
Zhou X, Boren J, Akyurek LM (2007) Filamins in cardiovascular development. Trends Cardiovasc Med 17(7):222–229. https://doi.org/10.1016/j.tcm.2007.08.001
Qiao J, Cui SJ, Xu LL, Chen SJ, Yao J, Jiang YH, Peng G, Fang CY, Yang PY, Liu F (2015) Filamin C, a dysregulated protein in cancer revealed by label-free quantitative proteomic analyses of human gastric cancer cells. Oncotarget 6(2):1171–1189. https://doi.org/10.18632/oncotarget.2645
Yang B, Liu Y, Zhao J, Hei K, Zhuang H, Li Q, Wei W, Chen R, Zhang N, Li Y (2017) Ectopic overexpression of filamin C scaffolds MEK1/2 and ERK1/2 to promote the progression of human hepatocellular carcinoma. Cancer Lett 388:167–176. https://doi.org/10.1016/j.canlet.2016.11.037
Ai J, Jin T, Yang L, Wei Q, Yang Y, Li H, Zhu Y (2017) Vinculin and filamin-C are two potential prognostic biomarkers and therapeutic targets for prostate cancer cell migration. Oncotarget 8(47):82430–82436. https://doi.org/10.18632/oncotarget.19397
Neethling A, Mouton J, Loos B, Corfield V, de Villiers C, Kinnear C (2016) Filamin C: a novel component of the KCNE2 interactome during hypoxia. Cardiovasc J Afr 27(1):4–11. https://doi.org/10.5830/CVJA-2015-049
Kong SW, Hu YW, Ho JW, Ikeda S, Polster S, John R, Hall JL, Bisping E, Pieske B, dos Remedios CG, Pu WT (2010) Heart failure-associated changes in RNA splicing of sarcomere genes. Circ Cardiovasc Genet 3(2):138–146. https://doi.org/10.1161/CIRCGENETICS.109.904698
Karmouch J, Protonotarios A, Syrris P (2018) Genetic basis of arrhythmogenic cardiomyopathy. Curr Opin Cardiol 33(3):276–281. https://doi.org/10.1097/HCO.0000000000000509
Yang X, Wu X, Wu K, Yang D, Li Y, Shi J, Liu Y (2015) Correlation of serum- and glucocorticoid-regulated kinase 1 expression with ischemia-reperfusion injury after heart transplantation. Pediatr Transplant 19(2):196–205. https://doi.org/10.1111/petr.12417
Qian S, Yang X, Wu K, Lv Q, Zhang Y, Dai J, Chen C, Shi J (2014) The changes of vaccinia related kinase 1 in grafted heart after rat heart transplantation. J Thorac Dis 6(12):1742–1750. https://doi.org/10.3978/j.issn.2072-1439.2014.11.17
Shi J, Yang X, Yang D, Li Y, Liu Y (2015) Pyruvate kinase isoenzyme M2 expression correlates with survival of cardiomyocytes after allogeneic rat heterotopic heart transplantation. Pathol Res Pract 211(1):12–19. https://doi.org/10.1016/j.prp.2014.10.003
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM (2013) Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177(9):1006–1014. https://doi.org/10.1093/aje/kws342
Liu JN, Zhang JX, Lu G, Qiu Y, Yang D, Yin GY, Zhang XL (2010) The effect of oxidative stress in myocardial cell injury in mice exposed to chronic intermittent hypoxia. Chin Med J 123(1):74–78
Gao YH, Chen L, Ma YL, He QY (2012) Chronic intermittent hypoxia aggravates cardiomyocyte apoptosis in rat ovariectomized model. Chin Med J 125(17):3087–3092
Kasai T, Bradley TD (2011) Obstructive sleep apnea and heart failure: pathophysiologic and therapeutic implications. J Am Coll Cardiol 57(2):119–127. https://doi.org/10.1016/j.jacc.2010.08.627
McDonnell TJ, Beham A, Sarkiss M, Andersen MM, Lo P (1996) Importance of the Bcl-2 family in cell death regulation. Experientia 52(10–11):1008–1017
Zhang T, Saghatelian A (2013) Emerging roles of lipids in BCL-2 family-regulated apoptosis. Biochim Biophys Acta 1831(10):1542–1554. https://doi.org/10.1016/j.bbalip.2013.03.001
Beumer TL, Roepers-Gajadien HL, Gademan IS, Lock TM, Kal HB, De Rooij DG (2000) Apoptosis regulation in the testis: involvement of Bcl-2 family members. Mol Reprod Dev 56(3):353–359. https://doi.org/10.1002/1098-2795(200007)56:3<353::AID-MRD4>3.0.CO;2-3
Kubasiak LA, Hernandez OM, Bishopric NH, Webster KA (2002) Hypoxia and acidosis activate cardiac myocyte death through the Bcl-2 family protein BNIP3. Proc Natl Acad Sci U S A 99(20):12825–12830. https://doi.org/10.1073/pnas.202474099
Dorn GW 2nd, Kirshenbaum LA (2008) Cardiac reanimation: targeting cardiomyocyte death by BNIP3 and NIX/BNIP3L. Oncogene 27(Suppl 1):S158–S167. https://doi.org/10.1038/onc.2009.53
Acknowledgements
The authors would like to thank Shi Jiahai and Yang Dunpeng for their pathological diagnosis of HE staining results on this manuscript.
Author information
Authors and Affiliations
Contributions
Y XC, S Y, and Z SJ contributed to conception and design; Y XC, S Y, Z LF, L H, S YF, and Z SJ contributed to acquisition, analysis, and interpretation; Y XC and Z SJ wrote the manuscript, with significant contributions from all of the authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The protocol of this study was approved by the Jiangsu Province Animal Care ethics committee and performed in accordance with the Animal Management Rule of the People’s Republic of China and the Care and Use of the Laboratory Animals Guide of the Nanjing Medical University.
Rights and permissions
About this article
Cite this article
Yang, X., Shi, Y., Zhang, L. et al. Overexpression of filamin c in chronic intermittent hypoxia-induced cardiomyocyte apoptosis is a potential cardioprotective target for obstructive sleep apnea. Sleep Breath 23, 493–502 (2019). https://doi.org/10.1007/s11325-018-1712-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-018-1712-9