Abstract
Purpose
The study is intended to explore the nocturnal sleep determinants for excessive daytime sleepiness (EDS) in patients with obstructive sleep apnea syndrome (OSAS).
Methods
Consecutive patients (n = 182) who had an apnea/hypopnea index (AHI) greater than 5 times per hour were used in this study. EDS (n = 32) was considered present whenever the Epworth sleepiness scale (ESS) score was >10 and the multiple sleep latency test (MSLT) score was <5 min. Absence of EDS (no EDS, n = 48) was determined in patients with an ESS score of <10 and a MSLT score of >10 min.
Results
Compared to no EDS patients, EDS patients exhibited (1) greater AHI and time length of SaO2 <95%, lower nocturnal SaO2 during separate rapid eye movement (REM) and NREM periods, and lower total mean and minimum SaO2 during total recording period; (2) shortened latency to sleep and to REM sleep, and increased total sleep time and sleep efficiency; and (3) increases in the brief arousal index and duration of sleep stage 1. In addition, stepwise logistic regression analysis showed that the arousal index, the time length of SaO2 <95%, and the latency to REM were independent predictors of EDS.
Conclusions
The results suggest that EDS in OSAS patients are characterized by the following aspects of nocturnal sleep: (1) severe sleep apnea/hypopnea and hypoxemia, (2) fragmented sleep, (3) low quality of sleep, and (4) high pressure of sleep drive.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Excessive daytime sleepiness (EDS) is one of the most commonly seen symptoms in patients suffering from obstructive sleep apnea syndrome (OSAS). EDS is known to be a predisposing factor for accidents, psychosocial morbidity, and poor quality of life [1–4]. The reason why some patients with OSAS complain of EDS, whereas others do not, is unclear. Based on the fact that both sleep fragmentation [5, 6] and hypoxemia [7, 8] are statistically related to EDS among patients with OSAS, sleep fragmentation and hypoxemia have been proposed as explanations to EDS associated with OSAS.
With regard to subjective and objective evaluation of daytime sleepiness, the Epworth sleepiness scale (ESS) and the multiple sleep latency test (MSLT), respectively, appear to be the most often used tools in the research of patients with OSAS. Some studies showed that, compared to health control or OSAS patients with less severe sleep apnea/hypopnea, severe OSAS patients had significantly increased ESS scores [9–12]. However, some other works did not find a significant correlation between ESS score and sleep apnea/hypopnea index (AHI) [13–15]. Between ESS and MSLT scores in the measurement of daytime sleepiness in relation to the severity of OSAS, MSLT has been demonstrated to be a more objectively accurate determinant of EDS than ESS [13, 16], including an investigation among patients of Hong Kong, China [17]. However, a few clinical studies have also established the negative finding that ESS and MSLT were not correlated with the severity of OSAS [6, 18]. Moreover, among individuals with OSAS, a significantly negative correlation between ESS and MSLT scores was reported in some studies [6, 15, 18].
Many potential factors, including motivation, adaptation, environment, and methodology, could have contributed to the said variations between subjective and objective evaluation in determining EDS across studies in patients with OSAS. Therefore, determinants of the influences of overnight sleep on daytime sleepiness among OSAS patients may vary depending on the different tools used in the evaluation of daytime sleepiness. For example, Roure et al. [19] found that patients with complaints of EDS as assessed by ESS were characterized by longer sleep durations and an increased slow wave sleep (SWS) compared to those with no EDS. They did not deem respiratory disturbance and sleep fragmentation as the primary determinants of EDS in patients with OSAS. In contrast, according to MSLT scores, Seneviratne et al. [20] demonstrated that severe snoring, higher sleep efficiency, and an increase in total arousals seemed to be the most useful predictors for EDS in patients with OSAS.
The practice that Mediano et al. first established, in which EDS and no EDS were determined with a combination of ESS and MSLT scores, appears to be a useful analysis that can more reliably distinguish between patients with EDS and those with no EDS in the research of OSAS [21]. Analyses of the parameters of overnight recording between these two groups may provide valuable data to elucidate the relationship between overnight sleep problems and EDS in patients with OSAS. In particular, the present study included more patients with mild sleep apnea and led to larger differences between the EDS and no EDS groups, compared to previous work. This may allow us to fine tune determinants used in the comparisons of the two groups.
Methods
Subjects
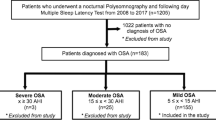
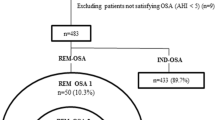
One hundred eighty-two consecutive patients (162 male and 20 female) with a clinical suspicion of OSAS attended the Sleep Medicine Center of West China Hospital (Chengdu, China) and were identified by overnight polysomnography (PSG) to have AHI greater than 5 times per hour. After an overnight PSG recording, ESS and MSLT data were collected. All methodological details are described below.
The presence of EDS was diagnosed by considering the results of both ESS and MSLT scores, as described by Mediano et al. [21]. EDS (n = 32, 17.6%, 32 male) was considered present whenever the ESS score was >10 and the MSLT score <5 min. Conversely, the absence of EDS (no EDS, n = 48, 26.4%, 38 male and 10 female) was determined by an ESS score of <10 and an MSLT score of >10 min. One hundred two subjects were excluded from the data analysis due to the presence of one or more of the following: chronic disease, chronic obstructive pulmonary disease, liver cirrhosis, thyroid dysfunction, rheumatoid arthritis, chronic renal failure, major psychiatric disorder, or the intake of hypnotics or antidepressant medications. In addition, we ensured that patients with EDS caused by other types of illnesses (e.g., narcolepsy) according to their history of illness and examinations were also excluded.
Overnight polysomnography
The diagnosis of OSAS was established by a standard overnight PSG. Overnight PSG consisted of continuous recordings from four electroencephalographic (EEG) leads (F3-A2, F4-C1, C3-A2, C4-A1, O1-A2, O2-A1, international 10–20 system), two electrooculographic leads (ROC-A1, LOC-A2), four electromyographic leads (two submental and bilateral tibialis anterior), thermistors for nasal and oral airflow, strain gauges for thoracic and abdominal excursion, finger pulse oximetry, and electrocardiography. Thirty-second epochs were analyzed and sleep stages were scored according to the international criteria of American Academy of Sleep Medicine [22]. An apnea was defined as more than 90% reduction in airflow for at least 10 s; hypopnea as 50% or more reduction of airflow for at least 10 s associated with 3% or more reduction in oxygen saturation.
EEG arousals [23] were also scored according to the criteria of American Sleep Disorders Association. Arousal index was defined as total number of EEG arousals per hour of total sleep time.
Multiple sleep latency test
According to international guidelines [24], MSLT was carried out during daytime on the day immediately following the overnight PSG and was comprised of four 20-min nap trials at intervals of 2 h. The recording montages were similar to that of the PSG, except that chest and abdominal strain gauges and thermistors were not included. The nap trial was terminated at 20 min if the subject did not achieve sleep, but was continued for 15 min after the onset of sleep if sleep had occurred within 20 min. Sleep latency was defined as the duration in minutes from lights-out to the first epoch of sleep in each nap trial. Mean sleep latency was calculated using MSLT data from all four trials.
Epworth sleepiness scale
All patients completed the validated Chinese version of ESS [9]. ESS is a self-administered questionnaire designed to measure the general level of daytime sleepiness. Patients rate on a scale of 0–3 their likelihood of falling asleep in eight different situations commonly encountered in daily life. Total ESS score ranges from 0 to 24; higher scores indicate more subjective sleepiness. All questionnaires were completed on the morning of the MSLT recording.
The procedure was approved by the research ethics board of West China Hospital of Sichuan University, and informed consent was obtained from each participant.
Statistical analysis
Results were shown as mean ± SD. Comparisons between both groups of patients were performed using independent t tests and Mann–Whitney U tests for normally and abnormally distributed data, respectively. Subsequently, to determine the independent risk factors for sleepiness in OSAS, all variables that were found by the above analysis with p ≤ 0.10 were included in a multivariate forward stepwise logistic regression model. Statistical significance was defined using a p value of 0.05. Statistical analyses were performed with SPSS for Windows software (version 17.0).
Results
Table 1 shows the main demographic characteristics of patients with no EDS and those of patients with EDS. Compared to the no EDS group, the EDS group had a significantly greater body mass index (BMI) and ESS score, but a lower MSLT score and awakening SaO2 percentage. No difference in age was obtained between the two groups.
Table 2 presents polysomnographic data in OSAS patients with and without EDS. EDS patients exhibited a significantly greater AHI, a longer time length of SaO2 <95%, lower nocturnal SaO2 during separate REM and NREM periods, as well as lower total mean and minimum SaO2, compared to those of no EDS patients. EDS patients had a significantly shorter average snore duration (obtained with total snoring time/number of snores), compared to those of no EDS patients.
Statistically significant differences in overnight sleep parameters included shortened latencies to sleep and to REM, an increase in total sleep, and an increase in sleep efficiency in patients with EDS compared to those with no EDS. The comparison between the two groups in absolute time spent in different sleep stages revealed that the increase was only significant in N1, but not in N2, N3, or REM in patients with EDS. Last but not least, patients with EDS showed a significant decrease in wakefulness after sleep onset (WASO) and an increase in the brief arousal index.
In summary, univariate analysis revealed that AHI, five parameters of SaO2 induced by sleep apnea, mean snoring time, and 11 parameters of sleep architecture were variables for which a significant difference between the no EDS and EDS groups could be observed. Additionally, stepwise logistic regression analysis showed that the arousal index, time length of SaO2 <95%, and REM sleep latency were found to be independent predictors of EDS (Table 3).
Discussion
An independent ESS evaluation has been the most often used tool in the determination of EDS in both population- and hospital-based studies for OSAS. In population-based studies, snoring and AHI have both been independently associated with EDS as determined by ESS scores [10, 11]. Hospital-based studies have suggested that nocturnal hypoxemia and autonomic arousal may play a major role in the development of EDS [25, 26]. Patients with OSAS and EDS were also found to have increased total sleep and SWS compared to those with no EDS [19]. A recent investigation among Chinese patients with OSAS showed that ESS score was significantly linked to the oxygen desaturation index, AHI, and BMI; in fact, the oxygen desaturation index was the strongest determinant of ESS score [25]. Therefore, these ESS-score-based works suggest that EDS among OSAS patients may be linked with the following potential nocturnal polysomnographic determinants: (1) severity of OSAS (e.g., increased AHI and oxygen desaturation index), (2) high sleep drive as reflected by increased total sleep and SWS, and (3) fragmented sleep characterized by increased arousals.
Comparisons of the MSLT score between no EDS and EDS patients revealed that severe snoring, high sleep efficiency, and increased total arousals in PSG seemed to predict EDS [20], consistent with the results in some studies using ESS score as a determinant of EDS. However, other studies have suggested that MSLT could be a more objective and accurate determinant of EDS than could ESS [13, 16], potentially due to psychological factors and the subject's lack of awareness of EDS, which can strongly influence ESS scores. As a result, ESS and MSLT scores were not always significantly associated with each other among individuals with OSAS [27], and thus, an assessment using MSLT or ESS alone may not truly reflect sleepiness. Using a combination of both measures, therefore, may offer complementary advantages in the judgment of EDS.
Mediano et al. used ESS and MSLT in conjunction to determine EDS among patients with OSAS, in which the presence of EDS was marked by an ESS score of >10 and a MSLT score of <5 min, while the absence of EDS was defined as an ESS score of <10 and a MSLT score of >10 min [21]. They found that, compared to no EDS patients, EDS patients were characterized by increased sleep efficiency, longer apnea duration, more changes in nocturnal SaO2%, shortened sleep latency, and decreased awakening time. However, no differences were obtained in AHI, arousal index, and total sleep time between the two groups [21], though such differences have been identified in some studies using ESS or MSLT alone as the criterion for EDS. One possible reason for the discrepancy is that the patients in Mediano et al.'s were selected by AHI of greater than 20 times per hour, as opposed to the standard of 5 times per hour that we used.
In the current study, we utilized the joint ESS and MSLT criteria as used by Mediano et al. to identify EDS and no EDS patients [21]. The only difference in methodology is that we set the AHI standard as greater than 5 times per hour rather than 20 times per hour that Mediano et al. used, so that we could include more patients with mild sleep apnea, which we believe would lead to larger differences between the EDS and no EDS groups, thus allowing us to fine tune determinants used in the comparisons of the two groups. Exactly as we anticipated, compared to Mediano et al.'s results, many more variables with significant differences between the two groups were identified in the current work, as discussed below.
First of all, EDS patients had more severe sleep apnea and hypoxemia relative to those with no EDS in the present study. For instance, the mean AHI in no EDS and EDS groups were 33.7 ± 22.71 vs. 60.92 ± 19.24 (p < 0.001), respectively, in the current investigation, whereas the mean AHI were 60 ± 20 vs. 62 ± 18 for the two groups with no significant difference in Mediano et al.'s work. For reduction of mean SaO2%, we found that EDS patients had significantly lower SaO2%, not only during NREM and REM, but also during the awakening period (see Table 1), compared to those of no EDS patients. The latter parameter, however, did not yield a significant difference in Mediano et al.'s work. BMI was also significantly greater in the EDS group than in the no EDS group in the current work, which was not established by Mediano et al.'s work. Nonetheless, the distribution of ESS (5.3 ± 3.2, 16.5 ± 3.8) and MSLT (14.7 ± 3.0, 3.6 ± 1.0) scores between the two groups in the current work (see Table 1) was comparable to that of the study by Mediano et al. (ESS 5 ± 2, 17 ± 3; MSLT 16 ± 3, 4 ± 1). This suggests that similar levels of daytime sleepiness within no EDS and within EDS groups were obtained in our study compared to the work by Mediano et al. even though subjects in our EDS group had more severe sleep apnea events and hypoxemia.
As expected, significant differences between the two groups were found in a wide range of sleep parameters in the current investigation. Firstly, in accordance with previous works [19, 20], a significant increase in the arousal index was observed in EDS patients, and the distribution of mean values for the arousal index (56.3 ± 23.6 vs. 28.9 ± 17.0) was quite similar to that of AHI (60.92 ± 19.24 vs. 33.7 ± 22.71) between the two groups. This suggests that the difference in the arousal index between the two groups could mainly be attributed to the difference in AHI. Though whether microarousal is necessary to terminate apnea is still debatable [28], a high frequency of recurrent arousals appears to disrupt the continuity of sleep. Apnea/hypoxemia and fragmentation of sleep are considered to be the two main pathological problems for OSAS [6–8]. As the number of awakening episodes did not differ significantly, an increase in the arousal index in EDS patients is the only difference that we obtained between the two groups that reflect fragmented sleep. Therefore, current results illustrate that increased arousal appears to play a central role in the connection of sleep apnea/hypoxemia with the fragmentation of sleep. Secondly, with respect to the quality of sleep as reflected by time spent in light (N1) and deep (SWS) sleep, we found that EDS patients had a remarkable increase in N1 amount (both absolute and percentage), compared to no EDS patients. Increases in N1 time spent/percentage suggest that EDS patients exhibited poorer quality of sleep, which appears to be connected with increases in the arousal index and apnea/hypoxemia. In contrast, Mediano et al. did not see differences between the two groups in N1/N2 and N3 (SWS) percentage. Thirdly, in accordance with previous works [19–21], the majority of differences that we obtained suggest that EDS patients have increased pressure of nocturnal sleep drive, which includes shortened latency to sleep and to REM; reduced time of wakefulness after sleep onset; and increased sleep efficiency and total sleep time, compared to those of no EDS patients. These characteristics illustrate that EDS patients were under consistently higher pressure of sleep drive over both nocturnal and diurnal phases, which are underscored by consistently shortened latency to sleep in the measures of nocturnal sleep and daytime MSLT. High pressure of sleep drive in night and daytime may be attributed to the compensatory mechanism under homeostasis regulation of sleep in response to poor sleep quality and fragmented sleep. However, the mechanism of homeostasis regulation of sleep also may not be able to account for the observed differences between the two groups. For example, as a result of sleep deprivation and partial sleep deprivation, increases in REM sleep and SWS have been shown in an overwhelming majority of literatures in both human and animal experiment, though changes in REM in EDS patients were rarely reported for OSAS. For SWS, Mediano et al. did not see a significant difference in SWS percentage between the two groups, but Seveide et al. reported an increase in SWS in the EDS group compared to that of no EDS subjects [19]. In addition, there were indeed large variations in the amount of REM and SWS amount among individual clinical cases of OSAS patients. Therefore, a more specifically designed investigation is required to clarify whether REM amount and SWS amount are reliable determinants of EDS and whether EDS patients of OSAS have similar sleep compensation mechanisms in response to poor quality of sleep as those that occur under normal homeostasis regulation.
In summary, this study utilized clear cutoff criteria to determine EDS by combining subjective and objective evaluations for daytime sleepiness to identify many variables of nocturnal sleep that may be associated with the phylogeny of EDS in patients with OSAS. The difference for each significant variable that we obtained between the two groups may not be entirely novel in the field of research on OSAS patients. Nonetheless, after an extensive review of literature, we did not find any previous studies that simultaneously captured such a large number of nocturnal determinants of EDS in OSAS patients. EDS patients with OSAS are characterized by the following aspects of nocturnal sleep: (1) severe sleep apnea/hypopnea and hypoxemia, (2) fragmented sleep, (3) low quality of sleep, and (4) high pressure of sleep drive. As demonstrated by the animal study, intermittent hypoxia can lead to a large range of abnormal brain biochemistry [29], which might play a role in mediating changes between hypoxemia, nocturnal sleep, and EDS.
Stepwise logistic regression analysis added interesting data to predict nocturnal determinants of sleep for EDS (Table 3). This analysis showed that the arousal index, the time length of SaO2 <95%, and REM sleep latency were found to be independent predictors of EDS (Table 3). As we mentioned above, the arousal index may play a central role in establishing the changes between sleep apnea/hypopnea events and sleep quality. Existing literatures have consistently shown that changes in SaO2 appear to be the most sensitive variable in the determination of sleep apnea/hypopnea [6–8]. Shortened REM latency is possibly associated with increased pressure of sleep drive. Therefore, we believe that these predictors reflect the major pathological issues in the fragmentation of sleep, severity of apnea, and pressure of sleep drive for EDS in OSAS patients.
References
Douglas NJ, Polo O (1994) Pathogenesis of obstructive sleep apnoea/hypopnoea syndrome. Lancet 344:653–655
Sassani A, Findley LJ, Kryger M, Goldlust E, George C, Davidson TM (2004) Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep 27:453–458
Christou K, Markoulis N, Moulas AN, Pastaka C, Gourgoulianis KI (2003) Reactive oxygen metabolites (ROMs) as an index of oxidative stress in obstructive sleep apnea patients. Sleep Breath 7:105–110
Vennelle M, Engleman HM, Douglas NJ (2010) Sleepiness and sleep-related accidents in commercial bus drivers. Sleep Breath 14:39–42
Ciftci TU, Kokturk O, Ozkan S (2004) Apnea-hypopnea indexes calculated using different hypopnea definitions and their relation to major symptoms. Sleep Breath 8:141–146
Guilleminault C, Partinen M, Quera-Salva MA, Hayes B, Dement WC, Nino-Murcia G (1988) Determinants of daytime sleepiness in obstructive sleep apnea. Chest 94:32–37
Colt HG, Haas H, Rich GB (1991) Hypoxemia vs sleep fragmentation as cause of excessive daytime sleepiness in obstructive sleep apnea. Chest 100:1542–1548
Bedard MA, Montplaisir J, Richer F, Malo J (1991) Nocturnal hypoxemia as a determinant of vigilance impairment in sleep apnea syndrome. Chest 100:367–370
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Gottlieb DJ, Yao Q, Redline S, Ali T, Mahowald MW (2000) Does snoring predict sleepiness independently of apnea and hypopnea frequency? Am J Respir Crit Care Med 162:1512–1517
Gottlieb DJ, Whitney CW, Bonekat WH, Iber C, James GD, Lebowitz M, Nieto FJ, Rosenberg CE (1999) Relation of sleepiness to respiratory disturbance index: the Sleep Heart Health Study. Am J Respir Crit Care Med 159:502–507
Johns MW (1993) Daytime sleepiness, snoring, and obstructive sleep apnea. The Epworth sleepiness scale. Chest 103:30–36
Chervin RD, Aldrich MS (1999) The Epworth sleepiness scale may not reflect objective measures of sleepiness or sleep apnea. Neurology 52:125–131
Chervin RD, Aldrich MS, Pickett R, Guilleminault C (1997) Comparison of the results of the Epworth sleepiness scale and the multiple sleep latency test. J Psychosom Res 42:145–155
Chung KF (2000) Use of the Epworth sleepiness scale in Chinese patients with obstructive sleep apnea and normal hospital employees. J Psychosom Res 49:367–372
Furuta H, Kaneda R, Kosaka K, Arai H, Sano J, Koshino Y (1999) Epworth sleepiness scale and sleep studies in patients with obstructive sleep apnea syndrome. Psychiatry Clin Neurosci 53:301–302
Fong SY, Ho CK, Wing YK (2005) Comparing MSLT and ESS in the measurement of excessive daytime sleepiness in obstructive sleep apnoea syndrome. J Psychosom Res 58:55–60
Olson LG, Cole MF, Ambrogetti A (1998) Correlations among Epworth sleepiness scale scores, multiple sleep latency tests and psychological symptoms. J Sleep Res 7:248–253
Roure N, Gomez S, Mediano O, Duran J, Pena Mde L, Capote F, Teran J, Masa JF, Alonso ML, Corral J, Sanchez-Armengod A, Martinez C, Barcelo A, Gozal D, Marin JM, Barbe F (2008) Daytime sleepiness and polysomnography in obstructive sleep apnea patients. Sleep Med 9:727–731
Seneviratne U, Puvanendran K (2004) Excessive daytime sleepiness in obstructive sleep apnea: prevalence, severity, and predictors. Sleep Med 5:339–343
Mediano O, Barcelo A, de la Pena M, Gozal D, Agusti A, Barbe F (2007) Daytime sleepiness and polysomnographic variables in sleep apnoea patients. Eur Respir J 30:110–113
Iber C, Ancoli-Israel S, Chesson AL, Quan SF (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, 1st edn. American Academy of Sleep Medicine, Westchester
ASDA (1992) EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep 15:173–184
Carskadon MA, Dement WC, Mitler MM, Roth T, Westbrook PR, Keenan S (1986) Guidelines for the multiple sleep latency test (MSLT): a standard measure of sleepiness. Sleep 9:519–524
Chen R, Xiong KP, Lian YX, Huang JY, Zhao MY, Li JX, Liu CF (2010) Daytime sleepiness and its determining factors in Chinese obstructive sleep apnea patients. Sleep Breath. doi:10.1007/s11325-010-0337-4
Castiglioni P, Lombardi C, Di Rienzo M, Lugaresi E, Montagna P, Cortelli P, Parati G (2008) What are the causes of excessive daytime sleepiness in patients with sleep-disordered breathing? Eur Respir J 32:526–527
Benbadis SR, Mascha E, Perry MC, Wolgamuth BR, Smolley LA, Dinner DS (1999) Association between the Epworth sleepiness scale and the multiple sleep latency test in a clinical population. Ann Intern Med 130:289–292
Jordan AS, Eckert DJ, Catcheside PG, McEvoy RD (2003) Ventilatory response to brief arousal from non-rapid eye movement sleep is greater in men than in women. Am J Respir Crit Care Med 168:1512–1519
Wang Y, Zhang SX, Gozal D (2010) Reactive oxygen species and the brain in sleep apnea. Respir Physiol Neurobiol 174:307–316
Acknowledgments
This work was supported by Chinese National Science Foundation 30870891 and 30970902.
Conflict of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sun, Y., Ning, Y., Huang, L. et al. Polysomnographic characteristics of daytime sleepiness in obstructive sleep apnea syndrome. Sleep Breath 16, 375–381 (2012). https://doi.org/10.1007/s11325-011-0515-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-011-0515-z