Abstract
Study objectives
Obstructive sleep apnea (OSA) is common, yet the relationship between mild OSA and excessive daytime sleepiness (EDS) is unclear. Our objective was to determine the prevalence of objective EDS in a population with mild OSA using the mean sleep latency (MSL) from the multiple sleep latency test (MSLT).
Methods
We retrospectively analyzed 1205 consecutive patients who underwent a polysomnography and a following day MSLT at a single sleep center. Adult patients who met criteria for mild OSA with an apnea–hypopnea index of 5 to <15 events/h were identified, and the percentage of patients with a MSL ≤ 8 min was determined. Sleep study and demographic variables were examined to evaluate predictors of objective EDS.
Results
Of 155 patients with mild OSA, objective EDS was found in 36% (56/155) with an average MSL of 5.6 ± 2.1 min in the objectively sleepy patients. Objectively sleepy patients with mild OSA had greater total sleep time (411.6 ± 48.9 vs. 384.5 ± 61.7 min, p = 0.004), increased sleep efficiency (84.9 ± 9.7 vs. 79.7 ± 12.7%, p = 0.01), and decreased wake after sleep onset time (53.0 ± 36.9 vs. 67.4 ± 46.1 min, p = 0.04) compared to patients with mild OSA but without objective EDS, with total sleep time being an independent predictor of MSL (p = 0.006). The Epworth Sleepiness Scale (ESS) weakly correlated with objective EDS (ρ = − 0.169, p = 0.03).
Conclusions
There is a large subgroup of patients with mild OSA patients who have objective sleepiness. This may represent an ideal subgroup to target for future studies examining the effect of treatment in mild OSA. Additionally, the ESS was a poor predictor of this subgroup with mild OSA and objective EDS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is a sleep-related breathing disorder that is characterized by prolonged partial or complete blockages of the upper airway that disrupts sleep and has been associated with sleepiness and other adverse effects including cardiovascular and cerebrovascular disease. [1,2,3] The severity of OSA is classified into mild, moderate, and severe based on the number of apneas and hypopneas per hour of sleep. Mild OSA is defined as an apnea–hypopnea index (AHI) of 5 to less than 15 respiratory events per hour and is thought to affect approximately 20% of the middle-aged population. [4, 5] Despite this high prevalence, the decision to treat mild OSA remains highly controversial [6,7,8,9].
The decision to treat moderate and severe OSA is less controversial and the American Academy of Sleep Medicine (AASM) considers treatment with continuous positive airway pressure (CPAP) the standard of practice. [8] This recommendation derives from strong evidence demonstrating that both moderate and severe OSA are closely associated with sleepiness. [8, 10] In similar studies examining excessive daytime sleepiness (EDS) in mild OSA, this relationship has been less clear and the AASM considers it optional to treat mild OSA with CPAP [8, 11,12,13,14,15,16].
To date, the studies that have investigated the prevalence of EDS in patients with mild OSA have mainly used subjective measures of sleepiness such as the Epworth Sleepiness Scale (ESS). [12,13,14,15,16] While the ESS is easy to conduct and has a minimal financial cost, it has been shown to be a poor predictor of the severity of OSA and is considered unreliable. [17,18,19,20] Objective measures of EDS, such as the mean sleep latency (MSL) on the multiple sleep latency test (MSLT), have been shown to correlate better with the severity of OSA and may be more suitable to investigate this relationship between EDS and mild OSA. [21, 22]
Therefore, our primary goal was to investigate the prevalence of objective EDS in a population with mild OSA using the MSL from the MSLT. Additionally, we examined for demographic and sleep study predictors of objective EDS and investigated the correlation between the ESS and MSL.
Methods
Study population and study design
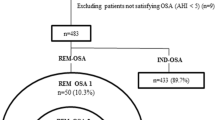
We retrospectively examined 1205 consecutive patients who underwent both a polysomnography (PSG) and following daytime MSLT at a single comprehensive sleep center between the years 2008 and 2017. Patients were reclassified using the International Classification of Sleep Disorders 3rd edition (ICSD-3) criteria and adult patients (age ≥ 18 years) with mild OSA were identified. Mild OSA was defined as an AHI of ≥ 5 and < 15 events/h. Patients were excluded if they met ICSD-3 criteria for narcolepsy, had a previous sleep disorder diagnosis including idiopathic hypersomnia, or had previously been treated with CPAP. [1] Demographic, PSG, and MSLT variables were collected through a retrospective electronic medical record review. The study design is summarized in Fig. 1.
Laboratory polysomnography protocol
All overnight PSGs were performed at an AASM accredited sleep center and were recorded digitally using Nihon-Kohden Diagnostic Systems (Neurofax EEG-1100, Polysmith 6.0, Nihon-Kohden Corporation, Tokyo). PSGs were conducted according to technical specifications from the AASM. [23] The PSG consisted of six electroencephalography (EEG) channels (F3, F4, C3, C4, 01, 02) with use of the International 10–20 system, three chin and bilateral leg (over anterior tibialis muscle) surface electromyogram leads, two electrooculogram leads, two electrocardiogram leads, snore microphone, respiratory effort belt over the chest and abdomen, pulse oximetry, thermocouples, and nasal pressure cannulas.
Scoring and sleep staging were in accordance with the AASM Scoring Manual and performed by a trained sleep technologist. [23, 24] PSG parameters included nocturnal sleep onset REM period (nSOREMP) (REM sleep recorded within 15 min of sleep onset); apneas (greater than 90% decrement in the thermistor for at least 10 s); hypopneas (50–90% decrement in the nasal pressure transducer for at least 10 s with a concurrent 3% or greater oxyhemoglobin desaturation or an EEG arousal); AHI; sleep efficiency; sleep onset latency; REM latency; quantity of time spent in N1, N2, N3, and REM sleep stages; periodic leg movement index; and arousal index.
Multiple sleep latency test protocol
All patients underwent an MSLT at an AASM accredited sleep center. The MSLT was performed the subsequent morning following the PSG and performed according to established AASM guidelines. [24] MSLT parameters included MSL, number of nap sessions with sleep, and sleep onset REM periods (SOREMPs) (if REM sleep occurred within 15 min of sleep onset). Objective excessive daytime sleepiness was defined as an MSL ≤ 8 min.
Epworth Sleepiness Scale
The ESS is a widely used measure to grade subjective sleepiness. [25] The ESS consists of 8 questions that ask the subjects to rate their likelihood of sleeping (on a scale of 0–3) in common daily life situations. All patients completed the ESS prior to the start of the PSG. Subjective excessive daytime sleepiness was defined as an ESS score > 10.
Statistical analysis
Data analysis was performed using IBM SPSS Statistics 24.0 (IBM-Armonk, NY, USA). The percentage of patients with mild OSA who met criteria for objective EDS from the MSL was calculated, and patients were then separated into a mild OSA with objective EDS and a mild OSA without objective EDS group. Univariable analysis was performed to examine for predictors of objective EDS. The Shapiro–Wilk test was used to test for normality. Categorical variables were compared by χ2 test and continuous variables were compared by independent t-test or Mann–Whitney U test, as appropriate. Additionally, ordinal variables were compared by Mann–Whitney U test. Statistical significance was set at p < 0.05. To determine predictors independently associated with objective EDS, multivariable linear regression analysis was performed on variables that were statistically significant during univariable analysis with MSL as the dependent variable. Collinearity was tested by the variance inflation factor (VIF), and variables with VIF > 10 were excluded.
To examine correlations between subjective and objective EDS, Spearman’s rank coefficient correlation was performed between the ESS and MSL. The predictive power of subjective sleepiness towards objective sleepiness was calculated through the positive predictive value. In addition, correlations between both the ESS and MSL to the AASM AHI were performed using Spearman’s rank correlation coefficient.
Results
Mild OSA population
Baseline and PSG characteristics
There were a total of 1205 untreated patients during this time period that had both a PSG and following day MSLT. Of these patients, 155 (13%) had mild OSA. Table 1 summarizes the demographic, PSG, and MSLT characteristics of the mild OSA patients. Patient ages ranged from 18 to 74 years (40.1 ± 12.9) and 37% were male. The mean body mass index (BMI) was 29.8 ± 6.9. The mean AASM AHI was 8.5 ± 2.7 events/h with a mean NREM AHI of 7.0 ± 3.4 events/h and a mean REM AHI of 15.3 ± 11.5 events/h.
Subjective and objective sleepiness
The average ESS for the patients with mild OSA was 13.9 ± 5.0. The percentage of patients with mild OSA who met criteria for subjective excessive daytime sleepiness was 82% (117/143). There were 12 patients with unreported ESS scores. The average MSL for patients with mild OSA was 10.6 ± 4.7 min. The percentage of patients with mild OSA who met criteria for objective excessive daytime sleepiness was 36% (56/155) with an average mean sleep latency of 5.6 ± 2.1 min amongst the objectively sleepy patients with mild OSA. Figure 2 illustrates the MSL distribution for the mild OSA group. There were no episodes of SOREMPs on MSLT experienced in this population.
Distribution and frequency of objective EDS in the population with mild OSA. Objective EDS was identified in 56 patients, which was 36% of our studied population. EDS, excessive daytime sleepiness; OSA, obstructive sleep apnea. An asterisk denotes that cutoff for objective EDS was defined as a mean sleep latency ≤ 8 min
Predictors of objective EDS in patients with mild OSA
Group analysis was performed between the 56 patients with mild OSA accompanied by objective EDS and the 99 patient with mild OSA but no objective EDS. Table 2 summarizes the clinical and PSG characteristics of these two groups. The patients with mild OSA and objective EDS had similar age (41.6 ± 12.2 vs. 39.3 ± 13.3 years, p = 0.19), percentage of men (39 vs. 36%, p = 0.72), BMI (29.4 ± 6.4 vs. 30.0 ± 7.2, p = 0.67), and ESS (14.7 ± 4.5 vs. 13.5 ± 5.3, p = 0.22) compared to those with mild OSA but no objective EDS. The patients with mild OSA and objective EDS had greater total sleep time (411.6 ± 48.9 vs. 384.5 ± 61.7 min, p = 0.004), decreased wake after sleep onset time (53.0 ± 36.9 vs. 67.4 ± 46.1 min, p = 0.04), and increased sleep efficiency (84.9 ± 9.7 vs. 79.7 ± 12.7%, p = 0.01), compared to patients with mild OSA but no objective EDS.
Multivariable analysis
The multivariable analysis is summarized in Table 3. Sleep efficiency was excluded from the multivariate analysis due to high collinearity (VIF = 11.8). Using multivariate linear regression, total sleep time was found to be an independent predictor of MSL (p = 0.006).
Correlations with severity of disease
The ESS significantly correlated with MSL; however, this correlation was weak (ρ = − 0.169, p = 0.03). The linear relationship between the ESS and MSL is shown in Fig. 3. Additionally, subjective EDS with the ESS was a poor predictor of objective EDS with a positive predictive value of 38.5% (45/117) and a negative predictive value of 73.1% (19/26). The ESS and MSL weakly correlated with the severity of mild OSA based on AASM AHI but were not statistically significant (ρ = 0.008, p = 0.92 and ρ = 0.061, p = 0.46 respectively).
Discussion
While moderate and severe OSA have been shown to be associated with EDS, the relationship between mild OSA and EDS is unclear. We sought to investigate this relationship by examining the MSL, an objective measure of EDS, in patients with mild OSA. We found that in our large population with mild OSA, 36% of the patients met criteria for objective excessive daytime sleepiness with an MSL ≤ 8 min on MSLT.
There have been multiple studies that have examined EDS in moderate and severe OSA, with these studies showing a subjective EDS prevalence of 46–57%. [26,27,28,29] While moderate and severe OSA classically are thought to have more of an effect on patients, our sample group with mild OSA had a similar high rate of sleepiness with using either ESS or MSL. In our patients with mild OSA, there were 81% who had subjective sleepiness using the ESS and 36% who had objective sleepiness using MSL, indicating a significant prevalence of sleepiness in mild OSA.
Patients with mild OSA who are experiencing objective EDS appear to have a significant burden of disease. The mean MSL in the objectively sleepy patients with mild OSA was 5.6 ± 2.1 min. This is similar to the disease burden of patients with idiopathic hypersomnia who have a reported average MSL of 6.2 ± 3.0 min. [24] Additionally, these objectively sleepy patients with mild OSA appear to have a compensatory response of increased restorative nocturnal sleep with significantly longer total sleep time, greater sleep efficiency, and a shorter WASO on PSG compared to the not objectively sleepy patients with mild OSA. These objectively sleepy patients with mild OSA may represent a specific subtype of patients, with an undefined mechanism driving sleepiness. One potential mechanism of sleepiness is an increase in systemic inflammation as inflammatory markers such as IL-6 and TNF-α have been shown to be elevated in patients with severe OSA. [30] These inflammatory markers may be better markers of sleep apnea severity than the traditional AHI. Further studies are needed to compare inflammatory levels between patients with mild OSA with and without objective EDS. Another important consideration is that these objectively sleepy patients with mild OSA may represent a group that has a second sleep disorder such as idiopathic hypersomnia.
Subjective sleepiness scores appear to be a poor predictor of objective EDS in patients with mild OSA. In our sample population, the ESS only weakly correlated with the MSL (ρ = − 0.169). An ESS > 10 predicted objective EDS in only 39% of the patients, while the negative predictive value was 73%. Total sleep time on PSG was the only variable we found to be an independent predictor of MSL; however, its predictive power is too small to be clinically useful. While the ESS test is more economically favorable, the MSLT appears to be the only way to accurately identify objectively sleepy patients with mild OSA.
Daytime sleepiness is a serious condition that adversely affects daytime functioning and quality of life. [3] While treating all cases of mild OSA with CPAP has previously been shown to have only minor effects on subjective sleepiness, there have been no studies that have assessed improvements specifically in objectively sleepy patients with mild OSA. [31,32,33,34] Future treatment studies are needed to investigate responses in objectively sleepy patients with mild OSA as these objectively sleepy patients potentially represent a subpopulation that may respond better to treatment.
The presence of subjective sleepiness has been shown in patients with OSA to be associated with cardiovascular consequences. [35,36,37] This association is thought to reflect subjective sleepiness being a surrogate marker of underlying cardiovascular risk pathways influenced by OSA mechanisms. [37] Given that objectively sleepy patients with mild OSA have evidence of a physiologic compensatory response, this subgroup may also be at risk for cardiovascular consequences.
A limitation of our study was that our sample population of patients consisted of sleep clinic patients as opposed to a general population of patients with mild OSA. These patients may be more likely to have subjective EDS compared to those who do not seek medical evaluation. Another limitation is that we examined patients who had undergone both a PSG and following day MSLT, which could introduce relevant bias as MSLTs are usually reserved for patients with subjective sleepiness. However, the ESS and other measures of subjective sleepiness are poor predictors of objective sleepiness and while this may have led to a larger percentage of subjectively sleepy patients in our sample population, it should not have resulted in significant selection bias of objectively sleepy patients. Additionally, the mean ESS for our group of patients with mild OSA was only mildly elevated at 13.9.
In conclusion, we show that in our cohort of patients with mild OSA, there is a large percentage of patients with objective EDS. These patients appear to have a compensatory response of increased restorative nocturnal sleep with increased total sleep time, shorter WASO, and greater sleep efficiency on PSG. The MSLT appears to be the best way to accurately identify objectively sleepy patients with mild OSA, as the traditional subjective sleep measure ESS is a poor predictor of MSL. Further studies are needed to determine whether or not objectively sleepy patients with mild OSA represent a unique subgroup in which treatment of these patients would be beneficial.
References
International classification of sleep disorders (2014) 3rd ed. Darien, IL: American Academy of Sleep Medicine
Foldvary-Schaefer NR, Waters TE (2017) Sleep-disordered breathing. (Continuum Minneap Minn). Sleep Neurol 23(4):1093–1116
Berry RB (2017) Sleep related breathing disorders: classification. In: Principles and Practice of Sleep Medicine. 6th ed. Philadelphia: Elsevier 1030–1040
Arnardottir ES, Bjornsdottir E, Olafsdottir KA, Benediktsdottir B, Gislason T (2016) Obstructive sleep apnoea in the general population: highly prevalent but minimal symptoms. Eur Respir J 47(1):194–202
Fietze I, Laharnar N, Obst A, et al (2019) Prevalence and association analysis of obstructive sleep apnea with gender and age differences - results of SHIP-Trend. J Sleep Res 28(5):e12770
Littner MR (2007) Mild obstructive sleep apnea syndrome should not be treated. Con J Clin Sleep Med 3(3):263–264
Brown LK (2007) Mild obstructive sleep apnea syndrome should be treated. Pro J Clin Sleep Med 3(3):259–262
Kushida CA, Littner MR, Hirshkowitz M et al (2006) Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep 29(3):375–380
Gay P, Weaver T, Loube D et al (2006) Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep 29(3):381–401
Chowdhuri S, Quan SF, Almeida F et al (2016) An official American Thoracic Society research statement: impact of mild obstructive sleep apnea in adults. Am J Respir Crit Care Med 193(9):e37-54
Weaver TE, Mancini C, Maislin G et al (2012) Continuous positive airway pressure treatment of sleepy patients with milder obstructive sleep apnea: results of the CPAP Apnea Trial North American Program (CATNAP) randomized clinical trial. Am J Respir Crit Care Med 186(7):677–683
Balsevicius T, Uloza V, Sakalauskas R, Miliauskas S (2012) Peculiarities of clinical profile of snoring and mild to moderate obstructive sleep apnea-hypopnea syndrome patients. Sleep Breath 16(3):835–843
Sharkey KM, Orff HJ, Tosi C, Harrington D, Roye GD, Millman RP (2013) Subjective sleepiness and daytime functioning in bariatric patients with obstructive sleep apnea. Sleep Breath 17(1):267–274
Svensson M, Franklin KA, Theorell-Haglow J, Lindberg E (2008) Daytime sleepiness relates to snoring independent of the apnea-hypopnea index in women from the general population. Chest 134(5):919–924
Ishman SL, Cavey RM, Mettel TL, Gourin CG (2010) Depression, sleepiness, and disease severity in patients with obstructive sleep apnea. Laryngoscope 120(11):2331–2335
Quan SF, Chan CS, Dement WC et al (2011) The association between obstructive sleep apnea and neurocognitive performance–the Apnea Positive Pressure Long-term Efficacy Study (APPLES). Sleep 34(3):303-314B
Chen R, Xiong KP, Lian YX et al (2011) Daytime sleepiness and its determining factors in Chinese obstructive sleep apnea patients. Sleep Breath 15(1):129–135
Cai SJ, Chen R, Zhang YL et al (2013) Correlation of Epworth Sleepiness Scale with multiple sleep latency test and its diagnostic accuracy in assessing excessive daytime sleepiness in patients with obstructive sleep apnea hypopnea syndrome. Chin Med J (Engl) 126(17):3245–3250
Aurora RN, Caffo B, Crainiceanu C, Punjabi NM (2011) Correlating subjective and objective sleepiness: revisiting the association using survival analysis. Sleep 34(12):1707–1714
Benbadis SR, Mascha E, Perry MC, Wolgamuth BR, Smolley LA, Dinner DS (1999) Association between the Epworth sleepiness scale and the multiple sleep latency test in a clinical population. Ann Intern Med 130(4 Pt 1):289–292
Fong SY, Ho CK, Wing YK (2005) Comparing MSLT and ESS in the measurement of excessive daytime sleepiness in obstructive sleep apnoea syndrome. J Psychosom Res 58(1):55–60
Chervin RD, Aldrich MS, Pickett R, Guilleminault C (1997) Comparison of the results of the Epworth Sleepiness Scale and the Multiple Sleep Latency Test. J Psychosom Res 42(2):145–155
Iber C, Ancoli-Israel S, Quan S (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specifications. 1 ed. Westchester, Ill: American Academy of Sleep Medicine
Littner MR, Kushida C, Wise M et al (2005) Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep 28(1):113–121
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545
Kapur VK, Baldwin CM, Resnick HE, Gottlieb DJ, Nieto FJ (2005) Sleepiness in patients with moderate to severe sleep-disordered breathing. Sleep 28(4):472–477
Mediano O, Barcelo A, de la Pena M, Gozal D, Agusti A, Barbe F (2007) Daytime sleepiness and polysomnographic variables in sleep apnoea patients. Eur Respir J 30(1):110–113
Roure N, Gomez S, Mediano O et al (2008) Daytime sleepiness and polysomnography in obstructive sleep apnea patients. Sleep Med 9(7):727–731
Oksenberg A, Arons E, Nasser K, Shneor O, Radwan H, Silverberg DS (2010) Severe obstructive sleep apnea: sleepy versus nonsleepy patients. Laryngoscope 120(3):643–648
Nadeem R, Molnar J, Madbouly EM et al (2013) Serum inflammatory markers in obstructive sleep apnea: a meta-analysis. J Clin Sleep Med 9(10):1003–1012
Avlonitou E, Kapsimalis F, Varouchakis G, Vardavas CI, Behrakis P (2012) Adherence to CPAP therapy improves quality of life and reduces symptoms among obstructive sleep apnea syndrome patients. Sleep Breath 16(2):563–569
Engleman HM, Kingshott RN, Wraith PK, Mackay TW, Deary IJ, Douglas NJ (1999) Randomized placebo-controlled crossover trial of continuous positive airway pressure for mild sleep apnea/hypopnea syndrome. Am J Respir Crit Care Med 159(2):461–467
Kushida CA, Nichols DA, Holmes TH et al (2012) Effects of continuous positive airway pressure on neurocognitive function in obstructive sleep apnea patients: the Apnea Positive Pressure Long-term Efficacy Study (APPLES). Sleep 35(12):1593–1602
Barnes M, McEvoy RD, Banks S et al (2004) Efficacy of positive airway pressure and oral appliance in mild to moderate obstructive sleep apnea. Am J Respir Crit Care Med 170(6):656–664
Ogilvie RP, Lakshminarayan K, Iber C, Patel SR, Lutsey PL (2018) Joint effects of OSA and self-reported sleepiness on incident CHD and stroke. Sleep Med 44:32–37
Tung P, Levitzky YS, Wang R, et al (2017) Obstructive and central sleep apnea and the risk of incident atrial fibrillation in a community cohort of men and women. J Am Heart Assoc 6(7)
Mazzotti DR, Keenan BT, Lim DC, Gottlieb DJ, Kim J, Pack AI (2019) Symptom subtypes of obstructive sleep apnea predict incidence of cardiovascular outcomes. Am J Respir Crit Care Med 200(4):493–506
Acknowledgements
The authors wish to thank Clinton Colaco, MD, and James Andry, MD, for their advice and support of this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Ethics committee approval was received for this study from the ethics committee of Vanderbilt University (2017) (IRB#170589).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Research was performed at Vanderbilt Medical Center.
All authors stated above have viewed and approved this manuscript.
Rights and permissions
About this article
Cite this article
Landzberg, D., Bagai, K. Prevalence of objective excessive daytime sleepiness in a cohort of patients with mild obstructive sleep apnea. Sleep Breath 26, 1471–1477 (2022). https://doi.org/10.1007/s11325-021-02473-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-021-02473-2