Abstract
Objective
This study aimed to develop and validate nomograms to predict overall survival (OS) and cancer-specific survival (CSS) in patients with prostate cancer.
Methods
Clinical data of patients with mPCa between 2010 and 2014 were retrieved retrospectively, and randomized into training (2/3) and validation sets (1/3). Nomograms were built with potential risk factors based on COX regression analysis. Accuracy was validated using the discrimination and calibration curve for the training and validation groups, respectively.
Results
6659 mPCa patients were collected and enrolled, including 4440 in the training set and 2219 in the validation set. Multivariate analysis showed that age, marital status, PSA, biopsy Gleason score, T stage, and bone metastasis were independent risk factors for both OS and CSS. The concordance index (C-index) of OS was 0.735 (95% CI 0.722–0.748) for the internal validation and 0.735 (95% CI 0.717–0.753) for the external validation. For CSS, it was 0.734 (95% CI 0.721–0.747) and 0.742 (95% CI 0.723–0.761), respectively. The nomograms for predicting OS and CSS displayed better discrimination power in both training and validation sets. Moreover, a favorable consistency between the predicted and actual survival probabilities was demonstrated using calibration curves.
Conclusions
The nomograms showed good performances for predicting OS and CSS in patients with prostate cancer. It might be a convenient individualized predictive tool for prognosis in clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) is the most common non-cutaneous malignancy among men in the United States, with an estimated 164,690 new cases and 29,430 cancer-related deaths in 2018 [1]. The visceral metastases rate of PCa patients is approximately 15% [2]. Due to the widespread use of prostate-specific antigen (PSA) screening and extended prostate biopsy techniques, the detection of PCa has increased substantially. Huggins and Hodges [3] introduced the efficacy of androgen deprivation therapy (ADT) in the treatment of advanced PCa in 1941. Although 80–90% of metastatic prostate cancers (mPCa) respond to initial androgen ablation, most patients eventually develop progressive disease. Unlike patients with localized PCa, for whom the 5-year survival rate approaches 100%, the 5-year survival rate for patients with mPCa is 20–30% [4]. In the US and Europe, some new and more effective agents are now available, such as enzalutamide, abiraterone, sipuleucel-T, and radium-223 [5]. However, treatment for CRPC is at a standstill [6]. Therefore, more accurate information on patient characteristics related to survival is needed.
Previously, the tumor-node-metastasis (TNM) cancer staging system of American Joint Committee on Cancer (AJCC) has been periodically updated for effective cancer management [7]. It is effective for patient populations. Nevertheless, increasing studies indicated that other factors, including age, marital status, PSA, Gleason score (GS), and surgical margins have also been in association with prognosis of patients with PCa [8,9,10,11]. Therefore, it is needed to establish a prognostic indicator system specified for PCa patients.
The nomogram is a simple statistical tool used for predicting cancer prognosis in clinical practices [12, 13]. Nomograms enable specifically individual survival scores by dynamically incorporating clinical variables with technical feasibility and reproducibility. They were created by regression analysis and extended beyond the standard TNM anatomical criteria [14]. It has been proved to be accurate with the advantage of visualization and quantification with a friendly interface for doctors and patients [15,16,17,18]. Several prognostic nomograms have been reported for patients with PCa [19, 20]. Nevertheless, there is still no report on a model for PCa patients based on a large cohort. Because of this need, a nomogram was constructed to predict OS and CSS based on data from the Surveillance, Epidemiology and End Results (SEER) database.
Materials and methods
Patients
The SEER database is free to the public and is updated annually, with routinely collected general messages from patients, primary tumor characteristics, treatments, survival, and follow-up, etc. It is made up of 18 population-based cancer registries, which nearly account for 25% of the total population in the United States [21]. In this study, the data were updated in November 2016, and released on April 16, 2018. The target population downloaded from the database was between 2010 and 2014. The time period of the study was between January 2010 and December of the year 2014. The inclusion criteria included the following: age at diagnosis > 18 years; adenocarcinoma of the prostate pathologically confirmed based on histology (site code: C61.9, and histological code: 8140). Primary prostate adenocarcinoma at all stages, including M1a-c [AJCC cancer staging manual, 7th edition [22]. Patients were excluded if they had a history of previous malignancy. Further patient exclusion criteria were unknown AJCC stage, unknown biopsy GS, unknown PSA values, and unknown survival month. All the finally included patients were randomly divided into the training set and validation set with a ratio of 2:1. Patients have been de-identified in the database, approval for this study was waived by the local ethics committee, and no informed consents were needed.
Variables
The data of patients and tumor characteristics, such as the age, race, marital status, PSA, biopsy GS, T stage, and bone metastasis, and follow-up information. Age was categorized subjectively as ≤ 49 years, 50–59 years, 60–69 years, 70–79 years, and ≥ 80 years. PSA was classified as < 20 ng/mL, 20–50 ng/mL, and > 50 ng/mL. Biopsy GS was classified as ≤ 6%, 7%, 8%, 9%, and 10%. The AJCC TNM staging system 7th edition was used, with the study being limited to the time period of 2010 and 2014, since it had been published in 2010. Overall survival (OS) and cancer-specific survival (CSS) were used as primary end point. OS was defined as the interval from the time of diagnosis to death or last follow-up regardless of death cause. CSS was measured from the date of first diagnosis to the date of death due to mPCa. There was a predetermined cutoff date based on the SEER 2016 submission database, containing information on the date of death until 2014. Therefore, the study used a cutoff date of December 31, 2014.
Statistical analyses
All the categorical variables were described as frequencies and percentages, and were compared between both groups through a Chi-squared test. The Kaplan–Meier method and log-rank test were used to analyze each potential prognostic variable. Cox proportional hazard regression was applied to identify significant prognostic factors with hazard ratios (HRs) and 95% confidence intervals (95% CIs). Variables in the univariate analysis with P values < 0.05 were selected for multivariate analysis. The nomogram was built with potential risk factors based on the multivariate Cox regression analysis in the training set. A final model selection was performed by a backward step-down selection process with the Akaike information criterion [23, 24]. The validation set was used for the validation of the nomogram. C-index (concordance index) was used to estimate predictive performance of the nomogram. The larger the C-index is, the more accurate the model’s predictive ability is [25]. The calibration curves were based on 1000 times bootstrap resampling. The 45-degree line in a calibration plot was used as a perfect model to compare the actual outcomes. SPSS version 23 software (supplied by Chicago, IL, the United States) and R version 3.5.1 (http://www.r-project.org) were used in all above statistical analyses, where all P values were two sided, and statistical significance would be indicated when P value was below 0.05.
Results
Patient characteristics
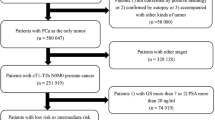
A total of 6659 eligible patients were involved. Out of the patients, 4440 patients were placed within the training set, while 2219 were placed within a validation set. Figure 1 shows the specific screening process. Most patients (34.7%) were between 60 and 69 years old, 28.2% were between 70 and 79 years old, and 17.3% were older than 80; only 2.4% patients were younger than 49 years old. Most of the patients of both sets were white (73.7%), married (57.2%), and have stage T1–T3 disease (87.5%), and PSA more than 50 ng/ml (59.4%). For GS, most patients (46.7%) have a higher proportion of GS 9. The two sets did not show any other major statistical differences for the remaining variables. Table 1 shows demographic and pathological characteristics of patients.
Nomogram construction
To analyze prognostic factors of OS, we used the univariate analysis and multivariate analysis on the training set. As shown in Table 2, univariate analysis showed that age, race, marital status, PSA, biopsy GS, T stage, and bone metastasis were associated with OS. Meanwhile, adjustments were made for the major risk factors, indicating six variables from the multivariate analysis that were independent OS predictive factors: age, marital status, PSA, biopsy GS, T stage, and bone metastasis. Therefore, a nomogram of 1-, 3- and 5-year OS was established with the independent variables (Fig. 2a). Similarly, those six variables were also used to establish CSS nomogram (Table 3, Fig. 2b).
Nomogram validation
The nomograms were both internally and externally validated. In the training set, the C-index was 0.735 (95% CI 0.722–0.748) in OS and 0.734 (95% CI 0.721–0.747) in CSS, respectively. In the validation set, the C-index was 0.735 (95% CI 0.717–0.753) in OS and 0.742 (95% CI 0.723–0.761) in CSS, respectively. The calibration plots for the probability of OS and CSS indicated that no apparent departure forms ideal line with optimal agreement between prediction by nomogram and observation in both training cohort and validation set (Figs. 3 and 4).
Discussion
In the current study, we made use of the population-based SEER database, and established clinical nomograms to predict conditional survival in patients with mPCa. A total of 6659 patients were included in this study. We successfully developed nomograms that were able to predict the 1-year, 3-year, and 5-year OS and CS for mPCa, whereas both external and internal nomogram validation indicated favorable calibration and discrimination. Nomograms highlighted the clinical significance of age, marital status, PSA, biopsy GS, T stage, and bone metastasis in mPCa patients. Therefore, the proposed nomograms are easy-to-use clinical tools for facilitating popularization of personalized treatment and patient counseling.
Nomograms have been widely used to predict survival outcomes in individual patients. They can be used to predict cancer risk and treatment outcomes [12, 14]. They address the complexity of balancing different variables through statistical modeling and risk quantification. The systematic approach of nomograms also avoids individual physician bias or individual abnormal clinical variables. A growing body of study has shown that nomograms outperform traditional staging scoring systems in various types of cancer, highlighting their use as new standards or alternatives [26,27,28]. Additionally, nomograms are suitable for assisting clinicians in handling complex situations without standard guidelines [29, 30]. They enable individualized risk stratification and enable clinicians to identify and stratify suitable patients for optimal management strategies.
Gleason scores (GSs) were the most powerful factors for predicting mPCa. Previous studies also indicated that GSs play important roles in the prognosis of localized and mPCa [31,32,33]. Rusthoven et al. [34] performed a retrospective analysis including 4654 mPCa patients, and indicated that survival differences for GS 7 vs. 8, 8 vs. 9, and 9 vs.10 were highly significant in both univariate and multivariate analyses. Age was identified as a predictor of survival for patients with solid tumors [35, 36]. It has been reported by several studies to play paradoxical roles in prognosis of PCa [37, 38]. Guo et al. [38] evaluated the effects of age on prognosis of thymomas based on SEER data. They divided age into the younger-aged group (≤ 70 years old), middle-aged group (30.9%, 70–82 years old), and elderly aged group (> 82 years old). They found that patients in the younger group had better prognosis than patients in the middle-aged and elderly groups. In present study, 6659 patients were divided into 5 groups. The results showed that as the patient ages, the prognosis of the patient is getting worse. It was consistent with previous findings. Marital status has been found to be an independent prognostic factor in multiple cancers [39, 40]. Married patients were featured by reduced cancer-specific deaths and more likely to receive definitive therapy [41]. Married patients were more likely to be diagnosed at earlier stage and to receive surgical treatment. Moreover, married patients had significantly lower risk in OS [42]. Our study also indicated the consistent results. This may be due to the fact that married patients tend to get more social support and heart comfort. Pretreatment PSA level is widely considered to be powerful prognostic factor for PCa. This was not surprising because PSA level is a well-known factor in determining the aggressiveness of PCa [43]. Our study also indicated the consistent results. In addition to the above factors, bone metastases have also been identified as important prognostic factors.
There were several limitations of the present study. The first limitation of this study was that the nomograms were constructed from retrospective data. Therefore, the potential risk of selection bias cannot be ruled out. The second limitation was that several critical prognostic factors, such as performance status, serum hemoglobin, and lactate dehydrogenase, were unavailable in the SEER database. These factors have been reported as predictive factors for PCa patients. The third limitation was the lack of external clinical data from independent sources, which is required to improve the utilization of this nomogram. Therefore, these areas will be key areas for future studies.
In conclusion, we were successful in establishing and validating nomograms to predict 1-year, 3-year, and 5-year OS and CSS in individual patients with mPCa based on a large study cohort. The prediction nomograms might be a useful tool for predicting prognosis for patients with mPCa.
References
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics. CA Cancer J Clin 68(1):7–30. https://doi.org/10.3322/caac.21442
Gandaglia G, Abdollah F, Schiffmann J, Trudeau V, Shariat SF, Kim SP, Perrotte P, Montorsi F, Briganti A, Trinh QD, Karakiewicz PI, Sun M (2014) Distribution of metastatic sites in patients with prostate cancer: a population-based analysis. Prostate 74(2):210–216. https://doi.org/10.1002/pros.22742
Huggins C, Hodges CV (1941) Studies on prostatic cancer I: the effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostate. Cancer Res 168(1):293–297
Gillessen S, Attard G, Beer TM, Beltran H, Bossi A, Bristow R, Carver B, Castellano D, Chung BH, Clarke N, Daugaard G, Davis ID, de Bono J, Borges Dos Reis R, Drake CG, Eeles R, Efstathiou E, Evans CP, Fanti S, Feng F, Fizazi K, Frydenberg M, Gleave M, Halabi S, Heidenreich A, Higano CS, James N, Kantoff P, Kellokumpu-Lehtinen PL, Khauli RB, Kramer G, Logothetis C, Maluf F, Morgans AK, Morris MJ, Mottet N, Murthy V, Oh W, Ost P, Padhani AR, Parker C, Pritchard CC, Roach M, Rubin MA, Ryan C, Saad F, Sartor O, Scher H, Sella A, Shore N, Smith M, Soule H, Sternberg CN, Suzuki H, Sweeney C, Sydes MR, Tannock I, Tombal B, Valdagni R, Wiegel T, Omlin A (2018) Management of patients with advanced prostate cancer: the report of the advanced prostate cancer consensus conference APCCC 2017. Eur Urol 73(2):178–211. https://doi.org/10.1016/j.eururo.2017.06.002
Cornford P, Bellmunt J, Bolla M, Briers E, De Santis M, Gross T, Henry AM, Joniau S, Lam TB, Mason MD, van der Poel HG, van der Kwast TH, Rouviere O, Wiegel T, Mottet N (2017) EAU-ESTRO-SIOG guidelines on prostate cancer. Part II: treatment of relapsing, metastatic, and castration-resistant prostate cancer. Eur Urol 71(4):630–642. https://doi.org/10.1016/j.eururo.2016.08.002
Wu JN, Fish KM, Evans CP, Devere White RW, Dall’Era MA (2014) No improvement noted in overall or cause-specific survival for men presenting with metastatic prostate cancer over a 20-year period. Cancer 120(6):818–823. https://doi.org/10.1002/cncr.28485
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, Meyer L, Gress DM, Byrd DR, Winchester DP (2017) The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin 67(2):93–99. https://doi.org/10.3322/caac.21388
Liu Y, Xia Q, Xia J, Zhu H, Jiang H, Chen X, Zheng Y, Zhang F, Li S (2018) The impact of marriage on the overall survival of prostate cancer patients: a surveillance, epidemiology, and end results (SEER) analysis. Can Urol Assoc J. https://doi.org/10.5489/cuaj.5413
Guo Y, Mao S, Zhang A, Wang R, Zhang Z, Zhang J, Wang L, Zhang W, Wu Y, Ye L, Yang B, Yao X (2019) Prognostic significance of young age and non-bone metastasis at diagnosis in patients with metastatic prostate cancer: a SEER population-based data analysis. J Cancer 10(3):556–567. https://doi.org/10.7150/jca.29481
Preisser F, Mazzone E, Knipper S, Nazzani S, Bandini M, Shariat SF, Tian Z, Saad F, Montorsi F, Zorn KC, Graefen M, Tilki D, Karakiewicz PI (2019) Rates of positive surgical margins and their effect on cancer-specific mortality at radical prostatectomy for patients with clinically localized prostate cancer. Clin Genitourin Cancer 17(1):e130–e139. https://doi.org/10.1016/j.clgc.2018.09.024
Gu X, Gao X, Cui M, Xie M, Ma M, Qin S, Li X, Qi X, Bai Y, Wang D (2018) Survival outcomes of radical prostatectomy and external beam radiotherapy in clinically localized high-risk prostate cancer: a population-based, propensity score matched study. Cancer Manag Res 10:1061–1067. https://doi.org/10.2147/CMAR.S157442
Balachandran VP, Gonen M, Smith JJ, DeMatteo RP (2015) Nomograms in oncology: more than meets the eye. Lancet Oncol 16(4):e173–e180. https://doi.org/10.1016/S1470-2045(14)71116-7
Song W, Lv CG, Miao DL, Zhu ZG, Wu Q, Wang YG, Chen L (2018) Development and validation of a nomogram for predicting survival in patients with gastrointestinal stromal tumours. Eur J Surg Oncol 44(10):1657–1665. https://doi.org/10.1016/j.ejso.2018.07.004
Iasonos A, Schrag D, Raj GV, Panageas KS (2008) How to build and interpret a nomogram for cancer prognosis. J Clin Oncol 26(8):1364–1370. https://doi.org/10.1200/jco.2007.12.9791
Attiyeh MA, Fernandez-Del Castillo C, Al Efishat M, Eaton AA, Gonen M, Batts R, Pergolini I, Rezaee N, Lillemoe KD, Ferrone CR, Mino-Kenudson M, Weiss MJ, Cameron JL, Hruban RH, D’Angelica MI, DeMatteo RP, Kingham TP, Jarnagin WR, Wolfgang CL, Allen PJ (2018) Development and validation of a multi-institutional preoperative nomogram for predicting grade of dysplasia in intraductal papillary mucinous neoplasms (IPMNs) of the pancreas: a report from the pancreatic surgery consortium. Ann Surg 267(1):157–163. https://doi.org/10.1097/SLA.0000000000002015
Huang Z, Sun B, Wu S, Meng X, Cong Y, Shen G, Song S (2018) A nomogram for predicting survival in patients with breast cancer brain metastasis. Oncol Lett. https://doi.org/10.3892/ol.2018.8259
Sonpavde G, Pond GR, Rosenberg JE, Choueiri TK, Bellmunt J, Regazzi AM, Mullane SA, Necchi A, Raggi D, Lee JL, Lee S, Simpson J, Derleth CL, Lin SW, Bajorin DF (2018) Nomogram to assess the survival benefit of new salvage agents for metastatic urothelial carcinoma in the era of immunotherapy. Clin Genitourin Cancer. https://doi.org/10.1016/j.clgc.2018.03.016
Song W, Zhu ZG, Wu Q, Lv CG, Wang YG, Chen L, Miao DL (2018) A nomogram to predict overall survival for biliary tract cancer. Cancer Manag Res 10:1535–1541. https://doi.org/10.2147/cmar.s163291
Zhao J, Sun G, Liao B, Zhang X, Armstrong CM, Yin X, Liu J, Chen J, Yang Y, Zhao P, Tang Q, Wang Z, Chen Z, Li X, Wei Q, Li X, Chen N, Gao AC, Shen P, Zeng H (2018) Novel nomograms for castration-resistant prostate cancer and survival outcome in patients with de novo bone metastatic prostate cancer. 122(6):994–1002. https://doi.org/10.1111/bju.14398
Yang YJ, Lin GW, Li GX, Dai B, Ye DW, Wu JL, Xie HY, Zhu Y (2018) External validation and newly development of a nomogram to predict overall survival of abiraterone-treated, castration-resistant patients with metastatic prostate cancer. Asian J Androl 20(2):184–188. https://doi.org/10.4103/aja.aja_39_17
Cronin KA, Ries LA, Edwards BK (2014) The surveillance, epidemiology, and end results (SEER) program of the national cancer institute. Cancer 120(Suppl 23):3755–3757. https://doi.org/10.1002/cncr.29049
Edge SB, Compton CC (2010) The American joint committee on cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–1474. https://doi.org/10.1245/s10434-010-0985-4
Harrell FE Jr, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15(4):361–387. https://doi.org/10.1002/(sici)1097-0258(19960229)15:4%3c361:aid-sim168%3e3.0.co;2-4
Chen S, Lai Y, He Z, Li J, He X, Shen R, Ding Q, Chen H, Peng S, Liu W (2018) Establishment and validation of a predictive nomogram model for non-small cell lung cancer patients with chronic hepatitis B viral infection. J Transl Med 16(1):116. https://doi.org/10.1186/s12967-018-1496-5
Wolbers M, Koller MT, Witteman JC, Steyerberg EW (2009) Prognostic models with competing risks: methods and application to coronary risk prediction. Epidemiology 20(4):555–561. https://doi.org/10.1097/EDE.0b013e3181a39056
Fang C, Wang W, Feng X, Sun J, Zhang Y, Zeng Y, Wang J, Chen H, Cai M, Lin J, Chen M, Chen Y, Li Y, Li S, Chen J, Zhou Z (2017) Nomogram individually predicts the overall survival of patients with gastroenteropancreatic neuroendocrine neoplasms. Br J Cancer 117(10):1544–1550. https://doi.org/10.1038/bjc.2017.315
Roberto M, Botticelli A, Strigari L, Ghidini M, Onesti CE, Ratti M, Benzoni I, Pizzo C, Falcone R, Lomiento D, Donida BM, Totaro L, Mazzuca F, Marchetti P (2018) Prognosis of elderly gastric cancer patients after surgery: a nomogram to predict survival. Med Oncol 35(7):111. https://doi.org/10.1007/s12032-018-1166-8
Cao J, Yuan P, Wang L, Wang Y, Ma H, Yuan X, Lv W, Hu J (2016) Clinical nomogram for predicting survival of esophageal cancer patients after esophagectomy. Sci Rep 6:26684. https://doi.org/10.1038/srep26684
Rudloff U, Jacks LM, Goldberg JI, Wynveen CA, Brogi E, Patil S, Van Zee KJ (2010) Nomogram for predicting the risk of local recurrence after breast-conserving surgery for ductal carcinoma in situ. J Clin Oncol 28(23):3762–3769. https://doi.org/10.1200/jco.2009.26.8847
Weiser MR, Landmann RG, Kattan MW, Gonen M, Shia J, Chou J, Paty PB, Guillem JG, Temple LK, Schrag D, Saltz LB, Wong WD (2008) Individualized prediction of colon cancer recurrence using a nomogram. J Clin Oncol 26(3):380–385. https://doi.org/10.1200/jco.2007.14.1291
Pierorazio PM, Walsh PC, Partin AW, Epstein JI (2013) Prognostic Gleason grade grouping: data based on the modified Gleason scoring system. BJU Int 111(5):753–760. https://doi.org/10.1111/j.1464-410X.2012.11611.x
Kim TH, Jeon HG, Jeong BC, Seo SI, Jeon SS, Choi HY, Lee HM (2017) Development of a new nomogram to predict insignificant prostate cancer in patients undergoing radical prostatectomy. Scand J Urol 51(1):27–32. https://doi.org/10.1080/21681805.2016.1266384
Halabi S, Small EJ, Kantoff PW, Kattan MW, Kaplan EB, Dawson NA, Levine EG, Blumenstein BA, Vogelzang NJ (2003) Prognostic model for predicting survival in men with hormone-refractory metastatic prostate cancer. J Clin Oncol 21(7):1232–1237. https://doi.org/10.1200/jco.2003.06.100
Rusthoven CG, Carlson JA, Waxweiler TV, Yeh N, Raben D, Flaig TW, Kavanagh BD (2014) The prognostic significance of Gleason scores in metastatic prostate cancer. Urol Oncol 32(5):707–713. https://doi.org/10.1016/j.urolonc.2014.01.004
Shah S, Boucai L (2018) Effect of Age on Response to Therapy and Mortality in Patients With Thyroid Cancer at High Risk of Recurrence. J Clin Endocrinol Metabol 103(2):689–697. https://doi.org/10.1210/jc.2017-02255
Chen CH, Chang TT, Cheng KS, Su WW, Yang SS, Lin HH, Wu SS, Lee CM, Changchien CS, Chen CJ, Sheu JC, Chen DS, Lu SN (2006) Do young hepatocellular carcinoma patients have worse prognosis? The paradox of age as a prognostic factor in the survival of hepatocellular carcinoma patients. Liver Int 26(7):766–773. https://doi.org/10.1111/j.1478-3231.2006.01309.x
Pettersson A, Robinson D, Garmo H, Holmberg L, Stattin P (2018) Age at diagnosis and prostate cancer treatment and prognosis: a population-based cohort study. Ann Oncol 29(2):377–385. https://doi.org/10.1093/annonc/mdx742
Guo X, Zhang C, Guo Q, Xu Y, Feng G, Li L, Han X, Lu F, Ma Y, Wang X, Wang G (2018) The homogeneous and heterogeneous risk factors for the morbidity and prognosis of bone metastasis in patients with prostate cancer. Cancer Manag Res 10:1639–1646. https://doi.org/10.2147/CMAR.S168579
Bai DS, Chen P, Qian JJ, Jin SJ, Jiang GQ (2017) Effect of marital status on the survival of patients with gallbladder cancer treated with surgical resection: a population-based study. Oncotarget 8(16):26404–26413. https://doi.org/10.18632/oncotarget.15476
Zhou H, Zhang Y, Song Y, Tan W, Qiu Z, Li S, Chen Q, Gao S (2017) Marital status is an independent prognostic factor for pancreatic neuroendocrine tumors patients: an analysis of the surveillance, epidemiology, and end results (SEER) database. Clin Res Hepatol Gastroenterol. https://doi.org/10.1016/j.clinre.2017.02.008
Aizer AA, Chen MH, McCarthy EP, Mendu ML, Koo S, Wilhite TJ, Graham PL, Choueiri TK, Hoffman KE, Martin NE, Hu JC, Nguyen PL (2013) Marital status and survival in patients with cancer. J Clin Oncol 31(31):3869–3876. https://doi.org/10.1200/jco.2013.49.6489
Zhou R, Yan S, Li J (2016) Influence of marital status on the survival of patients with gastric cancer. J Gastroenterol Hepatol 31(4):768–775. https://doi.org/10.1111/jgh.13217
Kundu SD, Roehl KA, Yu X, Antenor JA, Suarez BK, Catalona WJ (2007) Prostate specific antigen density correlates with features of prostate cancer aggressiveness. J Urol 177(2):505–509. https://doi.org/10.1016/j.juro.2006.09.039
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
WDJ and PCY collected, analyzed, interpreted the data, and wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jiang, Wd., Yuan, Pc. Development and validation of prognostic nomograms for patients with metastatic prostate cancer. Int Urol Nephrol 51, 1743–1753 (2019). https://doi.org/10.1007/s11255-019-02224-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-019-02224-z