Abstract
Purpose
Slow graft function (SGF) can influence overall prognosis in patients receiving deceased donor kidney transplantation (DKT). However, the impact of SGF on renal function remains uncertain. We investigated retrospectively renal function in cases with SGF compared with early graft function (EGF) and delayed graft function (DGF).
Methods
Renal function after transplantation was analyzed in 199 patients who underwent DKT. Patients were classified into 130 (65.3 %) cases with EGF, 27 (13.6 %) cases with SGF, 6 (3.0 %) cases with DGF and one dialysis (DGF1), and 36 (18.1 %) cases with DGF and two or more dialyses (DGF2).
Results
The 1-year estimated glomerular filtration rate (eGFR) in the SGF group was lower than that in the EGF group (P = 0.027), but the rate of eGFR decline did not differ between the groups. The risk factors for renal function were evaluated using the area under the eGFR curve over 3 years (AUCeGFR). Donor age was negatively, and recipient age and the number of HLA matches were positively correlated with the AUCeGFR (all P < 0.05). A multivariate analysis revealed that the AUCeGFR was lower in cases of younger recipient age, older donor age, and acute rejection (all P < 0.05). The AUCeGFR was significantly lower in the SGF and DGF2 groups compared with the EGF group (P = 0.031 and 0.006, respectively).
Conclusions
SGF may be an independent risk factor for poor renal function after DKT. Moreover, it was comparable to DGF. Efforts should be dedicated to minimizing the development of SGF and DGF.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischemia–reperfusion injury after kidney transplantation retards restoration of graft function and, in severe cases, can result in the need for hemodialysis [1]. Delayed graft function (DGF) caused by ischemia–reperfusion injury is generally defined as the need for hemodialysis within the first posttransplantation week. However, some recipients do not need dialysis but exhibit delayed restoration of graft function and are classified as having slow graft function (SGF) in contrast to early graft function (EGF) [2]. The reported incidence of SGF after deceased donor kidney transplantation (DKT) is 20–30 % [2–4]; however, this incidence may be higher when using more marginal kidneys, such as those received from expanded criteria donors or from donation after cardiac death (DCD) [5].
It is well known that recipients with DGF have inferior graft survival and increased risk of acute rejection compared with recipients with EGF [6–8]. In contrast to DGF, a few inconsistent reports have analyzed the long-term outcomes of SGF. Some studies have shown that SGF is associated with an intermediate risk of graft failure and has an acute rejection rate between those of EGF and DGF [2, 9]. In other reports, SGF had the same risk as DGF [4, 10]. It is uncertain whether those results are caused by worse confounding factors, such as acute rejection, or by SGF itself.
It is important to determine whether SGF should be considered as an independent risk factor for graft failure. To evaluate the effect of SGF on renal function, we analyzed the renal function of DKT recipients with SGF and compared it with that of DKT recipients with EGF or DGF.
Methods
Study design and participants
We performed a retrospective cohort study of the effect of SGF on renal function among patients who had undergone DKT. We analyzed renal function according to the grade of graft restoration after transplantation and adjusted for confounding variables that could affect renal function.
A total of 224 patients received DKT between January 2000 and August 2011 at the Samsung Medical Center, which is a 2000-bed tertiary hospital located in Seoul, Korea. We excluded 25 patients according to the following criteria: multi-organ transplants, primary nonfunction, an ABO-incompatible donor, a positive cross-matching test result, or age <18 years. Primary nonfunction was defined as a graft without function up to 3 months after transplantation. Ultimately, we analyzed data from 199 patients. This study was approved by the institutional review board of the Samsung Medical Center.
Data collection
We collected the data from medical records. Several variables related to the recipient, donor, and transplantation were recorded. The recipient variables included age, sex, body mass index (BMI), cause of end-stage renal disease, type and duration of renal replacement therapy, and history of previous kidney transplantation. The donor variables included age, sex, BMI, serum creatinine level, and donor type, such as non-DCD or DCD. The transplantation-related variables included peak panel-reactive antibody (PRA) levels, number of human lymphocyte antigen (HLA) matches, cold ischemia time (CIT), and the use of induction and maintenance immunosuppressive medications. The serum creatinine levels within the first week and the number of hemodialysis sessions after transplantation were identified to classify the grade of graft restoration. The duration of hospitalization was also recorded. The level of proteinuria was assessed using 24-h urine protein measurements at 1 year after transplantation.
We followed the patients after transplantation, and serum creatinine levels were measured at 3, 6, and 12 months posttransplantation, and every 6 months thereafter. These values were used to calculate the estimated glomerular filtration rate (eGFR) using the abbreviated Modification of Diet in Renal Disease study equation [11]. Acute rejection was confirmed by biopsy, and the trough levels of calcineurin inhibitors, such as cyclosporine and tacrolimus, were recorded.
Immunosuppressive regimen
Patients received 500 mg of intravenous methylprednisolone during the kidney transplantation operation. Subsequently, methylprednisolone was tapered to a minimal dose. All patients also received induction and maintenance immunosuppression. Induction immunosuppressive agents included alemtuzumab, basiliximab, and antithymoglobulin. Antithymoglobulin has been used for immunologically high-risk patients, such as those with an increased number of HLA mismatches, older donor age, PRA >0 %, or CIT >24 h [12]. Maintenance immunosuppression comprised a calcineurin inhibitor, an antimetabolite (such as mycophenolate mofetil or azathioprine), and a low-dose corticosteroid. Sirolimus, which is an mTOR inhibitor, can be substituted by a calcineurin inhibitor or an antimetabolite. The doses of maintenance immunosuppression, especially of calcineurin inhibitors, were monitored and adjusted based on the trough levels. The target trough levels of cyclosporine were between 150 and 300 ng/mL for the first 3 months, followed by tapering doses to maintain the trough levels between 100 and 200 ng/mL [13]. The doses of tacrolimus were adjusted to attain a target trough level of 8–10 ng/mL for the first 3 months and 3–7 ng/mL after this period [14].
Definitions
Patients were divided into four groups based on their serum creatinine levels within the first week and the number of hemodialysis sessions after transplantation. DGF was defined as the need for dialysis in the first 7 days after transplantation. The DGF group was divided into two subgroups: DGF1, which required only one dialysis session, and DGF2, which required two or more dialysis sessions, because DGF1 has unique features that distinguish it from DGF2 [15]. SGF was defined as an absence of the need for dialysis after transplantation and a serum creatinine level ≥2.5 mg/dL 5 days after transplantation [16]. EGF was defined as an immediate functioning graft with no need for dialysis and a serum creatinine level <2.5 mg/dL 5 days after transplantation.
Outcomes
Renal function after DKT was evaluated according to the grade of graft restoration after transplantation. The eGFR at each time point was compared between the groups. In addition, the rate of renal function decline 1 year after transplantation was assessed.
In visual data exploration, we found that the patterns of renal function change in individuals showed high variability, even within the same group, and that they were not linear using either eGFR or log(eGFR). Accordingly, we selected 188 patients who had been followed until the third year after transplantation to investigate the predicting factors of renal function. Final analyses excluded 11 patients with missing data for the following reasons: death (5) or loss to follow-up (6) within 3 years after kidney transplantation. For linear regression analysis to evaluate the risk factors for renal function, we calculated the “area under the eGFR versus time curve” (AUCeGFR) values as an index of individual cumulative renal function. The AUCeGFR was calculated using the eGFR at 3, 6, 12, 18, 24, 30, and 36 months after transplantation. For AUCeGFR calculation, we assumed that the eGFR after graft failure was 0 mL/min/1.73 m2.
Statistical analysis
The baseline differences between patients were analyzed. Continuous variables are expressed as the mean value ± standard deviation or median [interquartile range] and were compared using ANOVA followed by Scheffé’s method for multiple comparisons because of unequal sample sizes between groups. Categorical variables are expressed as numbers (percentages) and were analyzed using the χ 2 test. The linear mixed effect model was used to compare the pattern of eGFR change in each group 1 year after DKT. The effects of variables on the AUCeGFR were analyzed by linear regression analysis. The association between the AUCeGFR and variables was confirmed by univariate analysis followed by a multivariate analysis that included variables with P < 0.20 to adjust for the effects of potential confounders. We performed all analyses using SPSS Statistics version 22 (IBM Corp., Armonk, NY, USA). A P value <0.50 was considered significant.
Results
Baseline characteristics in the four groups
Among the 199 patients included in the study, 28 (14.1 %) patients underwent DKT from DCD donors and 42 (21.1 %) patients underwent hemodialysis within 7 days after transplantation. Acute rejection and graft failure occurred in 50 (25.1 %) and 13 (6.5 %) patients, respectively. One hundred and thirty (65.3 %) patients were classified into the EGF group, 27 (13.6 %) were classified into the SGF group, 6 (3.0 %) were classified into the DGF1 group, and 36 (18.1 %) were classified into the DGF2 group.
The baseline characteristics of the groups were analyzed (Table 1). Sex, age, donor age, donor creatinine level, and prevalence of DCD donors differed between groups (all P < 0.05). In contrast, the differences in BMI and CIT were not statistically significant (P = 0.062 and 0.060, respectively). Moreover, the number of HLA matches did not differ between the groups (P = 0.820). The length of hospitalization differed between the groups (P < 0.001). The amount of 24-h urine protein at 1 year, episodes of acute rejection, and occurrence of graft failure did not differ between the groups (P = 0.415, 0.336, and 0.773, respectively).
Multiple comparisons were made. Donor age and donor creatinine levels were higher in the SGF group than in the EGF group (P = 0.013 and 0.002, respectively). Age and donor creatinine level were higher in the DGF2 group than in the EGF group (P = 0.049 and P < 0.001, respectively). CIT was longest in the DGF2 group, but the difference was not significant (P = 0.081). The length of hospitalization was significantly longer in the DGF2 group compared with the EGF group (P < 0.001), whereas it was not significantly different in the SGF group (P = 0.187).
Levels of immunosuppression
After DKT, calcineurin inhibitors were used in 197 (99.0 %) patients, whereas two patients received sirolimus. Forty-four (22.3 %) patients received cyclosporine and 153 (77.7 %) received tacrolimus. To explore the impact of calcineurin inhibitors on renal function, the trough levels of those drugs were compared according to the grade of graft restoration (Fig. 1). The trough levels of cyclosporine at all time points did not differ between groups (Fig. 1a). Conversely, the trough levels of tacrolimus differed at 6 and 30 months after transplantation (P = 0.026 and 0.004, respectively; Fig. 1b). Multiple comparisons revealed that the level of this drug was somewhat higher in the DGF1 group than in the EGF group at 6 months (P = 0.078). At 30 months after DKT, the trough level of tacrolimus in the DGF1 group was highest among all groups (P = 0.016 compared with the EGF group). The trough levels of tacrolimus did not differ between the EGF, SGF, and DGF2 groups at all time points.
Levels of immunosuppression in the four groups. The trough levels of cyclosporine and tacrolimus until the third year after DKT were compared between groups. a The trough levels of cyclosporine did not differ in the four groups at all time points. b At 6 and 30 months after DKT, the trough levels of tacrolimus differed between the groups (P = 0.026 and 0.004, respectively). In multiple comparisons, its level in the DGF1 group was not significantly different at 6 months after transplantation (P = 0.078, compared with the EGF group), but was highest among the groups at 30 months (P = 0.016, compared with the EGF group). There were no differences in the trough levels of tacrolimus among the EGF, SGF, and DGF2 groups at all time points. DGF delayed graft function, DKT deceased donor kidney transplantation, EGF early graft function, SGF slow graft function
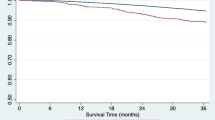
Patterns of renal function change in the four groups
The patterns of mean eGFR change in the four groups are shown in Fig. 2. The mean eGFR exhibited peak levels at 1 year after transplantation and decreased over time in all groups. However, individual eGFR values showed substantial variability, even in patients in the EGF group. The mean eGFR at 1 year after transplantation was 64.8 ± 18.1 mL/min/1.73 m2 in the EGF group, 55.9 ± 21.8 mL/min/1.73 m2 in the SGF group, 69.2 ± 19.1 mL/min/1.73 m2 in the DGF1 group, and 57.7 ± 17.1 mL/min/1.73 m2 in the DGF2 group (P = 0.042). These values decreased to 57.5 ± 21.4 mL/min/1.73 m2 in the EGF group, 49.4 ± 23.1 mL/min/1.73 m2 in the SGF group, 59.9 ± 19.5 mL/min/1.73 m2 in the DGF1 group, and 51.8 ± 17.2 mL/min/1.73 m2 in the DGF2 group at 3 years after transplantation (P = 0.122).
Trends in mean eGFR over 3 years in the four groups. The mean eGFR exhibited peak levels at 1 year after transplantation and decreased over time. As shown, there was substantial variability in renal function. The mean eGFR levels at 1 year after transplantation were 64.8 ± 18.1 mL/min/1.73 m2 in the EGF group, 55.9 ± 21.8 mL/min/1.73 m2 in the SGF group, 69.2 ± 19.1 mL/min/1.73 m2 in the DGF1 group, and 57.7 ± 17.1 mL/min/1.73 m2 in the DGF2 group. The mean eGFR was consistently lower in the SGF and DGF2 groups compared with the EGF and DGF1 groups. The mean eGFR differed between groups from 3 to 30 months (all P < 0.05), but did not differ at 36 months (P = 0.122). Compared with the EGF group, the eGFR in the SGF group was significantly lower at 3 and 6 months (P = 0.001 and 0.007, respectively), and that in the DGF2 group was lower at 3 months (P = 0.030). Data are expressed as mean ± standard deviation. DGF delayed graft function, EGF early graft function, eGFR estimated glomerular filtration rate, SGF slow graft function. *P < 0.05, compared with the EGF group
The linear mixed model yielded a 1-year eGFR in the EGF group of 65.5 mL/min/1.73 m2 [95 % confidence interval (CI), 61.9–69.1 mL/min/1.73 m2], which was lower by −10.1 and −6.5 mL/min/1.73 m2 in the SGF and DGF2 groups, respectively, albeit with no statistically significant difference between the EGF and DGF2 groups (95 % CI −18.9 to −1.2 and −14.4 to 1.4 mL/min/1.73 m2; P = 0.027 and 0.105, respectively). The rate of eGFR change in the EGF group was −2.5 mL/min/1.73 m2 per year (95 % CI −3.1 to −1.9 mL/min/1.73 m2 per year, P < 0.001), whereas the eGFR slope did not differ between the groups (P = 0.310, 0.142, and 0.620, respectively).
Risk factors for renal function
Among the 199 patients included in the study, the 188 patients who had been followed up until the third year after DKT were evaluated regarding predictors of individual renal function, the AUCeGFR, using linear regression analysis (Table 2). Donor age was correlated negatively (β −1.4 mL/min/1.73 m2 year, P < 0.001), and recipient age and the number of HLA matches were correlated positively (β 0.7 and 5.3 mL/min/1.73 m2 year, P = 0.033 and 0.032, respectively) with the AUCeGFR. BMI, donor BMI, and CIT were not associated with the AUCeGFR. There was no relationship between DCD and the AUCeGFR. Moreover, the use of tacrolimus was not associated with a lower AUCeGFR compared with the use of cyclosporine. Proteinuria >500 mg/day at 1 year after transplantation and episodes of acute rejection were significantly associated with the AUCeGFR (P = 0.002 and P < 0.001, respectively). To compare values according to the grade of graft restoration, the AUCeGFR in the EGF group was used as the reference. SGF was a predicting factor for a low AUCeGFR (P = 0.039), whereas DGF2 was not, as assessed using univariate analysis (P = 0.158). DGF1 was not related to AUCeGFR (P = 0.585).
A multivariate regression analysis with adjustments for variables that had a P value <0.20 in the univariate analysis, including age, donor age, the number of HLA matches, proteinuria, episodes of acute rejection, SGF, and DGF2, was performed to assess relationships with the AUCeGFR (Table 2). Older age was associated with a high AUCeGFR (P = 0.003). Donor age was correlated negatively with the AUCeGFR (P < 0.001), but the number of HLA matches was not correlated with the AUCeGFR in the multivariate analysis (P = 0.253). Proteinuria of 500 mg/day or more at 1 year after transplantation was not a significant predictor in multivariate analysis (P = 0.092). Patients with an episode of acute rejection had a significantly lower AUCeGFR (β −29.2 mL/min/1.73 m2 year, P < 0.001). Regarding the grade of graft restoration, the AUCeGFR was significantly lower in the SGF and DGF2 groups compared with the EGF group (β −19.3 and −22.0 mL/min/1.73 m2 year, P = 0.031 and 0.006, respectively).
Discussion
In this retrospective cohort study, we investigated renal function according to the grade of graft restoration after DKT. Patients with SGF had decreased renal function compared with those with EGF. This decreased renal function associated with SGF was significant even after adjusting for multiple variables, including acute rejection and proteinuria. In addition, we found that renal function in the SGF group was not superior to that observed in the DGF2 group.
Renal function is an important prognostic marker in transplantation and can be used to predict long-term outcomes [17, 18]. Several reports have described renal function in cases of SGF compared with EGF and DGF. One of those studies found that renal function in cases of SGF was intermediate between that in cases of EGF and DGF [9], while other studies reported that renal function was lower in cases of SGF compared with EGF, but did not differ between cases of SGF and DGF, as in our results [4, 19–21]. However, most of those studies did not rule out the effects of other variables, such as acute rejection; therefore, it remains uncertain whether the worse outcomes of SGF are related to the effects of SGF itself or to confounding variables. It is noteworthy that the poor renal function observed in patients with SGF was persistent, independent of episodes of acute rejection and amount of proteinuria.
According to our results, patients with SGF might have worse renal function than those with DGF. Thus, we also performed comparisons between the SGF and DGF2 groups, but found no statistically significant differences. The low eGFR detected in the SGF group may have been the result of various confounding factors, such as donor age or episodes of acute rejection, which were higher in the SGF group. Previous studies that reported a similar impact of SGF and DGF also found that serum creatinine level or eGFR at 1 year after transplantation was somewhat worse in patients with SGF than they were in those with DGF [4, 19–21]. Conversely, those results might have stemmed from a discrepancy between the definitions of SGF and DGF; i.e., the characteristics of patients with DGF, which is defined by the presence of dialysis treatment, may vary between centers or physicians. Akkina et al. [22] demonstrated that two centers that had different incidences of SGF and DGF had similar levels of graft survival, and that SGF, but not DGF, was a predictor of worse outcomes in one center. Therefore, a better definition that integrates SGF and DGF is needed to identify the degree of ischemia–reperfusion injury.
Here, we applied the definition of SGF (serum creatinine level of ≥2.5 mg/dL at 5 days after kidney transplantation) of Schroppel and Legendre [16]. Similar to that of DGF, there is no consensus regarding the definition of SGF and various definitions have been used in several reports. Most previous studies used a serum creatinine level of ≥3.0 mg/dL at 5 days posttransplantation; thus, there could be differences between previous results and our findings. In a pilot analysis, we also evaluated renal function in patients who had serum creatinine levels of ≥3.0 mg/dL at 5 days posttransplantation and obtained similar results. Because a higher cutoff point for SGF might decrease analytic power, we chose to define SGF as serum creatinine level of ≥2.5 mg/dL at 5 days after kidney transplantation. Nevertheless, we obtained consistent and significant results regarding the impact of SGF on renal function after DKT.
To compare the rate of eGFR change according to group, we used the linear mixed effect model. Although this model is the most appropriate statistical method to evaluate the impact of predictors on the rate of eGFR change, it requires the assumption that the eGFR trajectories are linear [23]. We found that the eGFR after DKT exhibited peak levels at 1 year after transplantation and decreased over time. Thus, we selected 1-year eGFR as the intercept in the model. Moreover, renal function at 1 year after transplantation was reported as a strong predictor of patient and graft outcomes [24]. Our results revealed significant differences in 1-year eGFR, but did not show differences in the rate of eGFR change. These negative findings regarding the rate of eGFR change were also reported in a previous study [25].
Visual exploration of our data showed that the eGFR after transplantation was highly changeable and did not exhibit linear patterns. Up to 40 % of patients with chronic kidney disease may have a nonlinear renal function trajectory [26, 27]. We thought that it would be more prevalent in cases of kidney transplantation, because of frequent episodes of acute kidney injury [28, 29]. Patients who undergo renal transplantation have a vulnerable kidney for multiple reasons, including having a single kidney, taking calcineurin inhibitors, the presence of episodes of rejection, and surgical complication, which lead to variable changes in renal function. For that reason, we compared the cumulative renal function estimated by the AUCeGFR to investigate the risk factors that affect renal function after transplantation. Several studies have shown that renal function assessed by the AUC predicts prognosis in the context of variability in graft function [30–32].
We divided the DGF group into two subgroups: DGF1 and DGF2. The definition of DGF based on the need for dialysis presents several problems, including clinical-dependent decision, dialysis required for postoperative potassium or transient fluid overload, residual renal function, or preemptive transplantation, which may lead to misclassification [16, 22, 33]. In this study, the DGF1 subgroup exhibited similar baseline characteristics, including serum creatinine and CIT, to those of the EGF group, and all six DGF1 patients had needed dialysis because of volume overload. Moreover, it seemed that patients with DGF1 had a better mean eGFR than the patients in the other groups. Jayaram et al. [15] showed that patients with DGF who needed only one dialysis session could be distinguished from those with DGF who needed more than two dialysis sessions and had similar outcomes to patients with EGF. Most of them received dialysis treatment because of hyperkalemia. In that study, CIT and eGFR in the DGF1 group were also similar to those of the EGF group. Because of the small number of DGF1 cases included, this study could not conclude the level at which DGF1 is placed in the spectrum of ischemia–reperfusion injury after kidney transplantation. Nevertheless, we deduce that dialysis itself cannot predict poor graft function and that an objective and precise definition of DGF is needed.
Our study had some limitations. First, because of the small number of subjects included, the statistical power of our analyses was limited. This relates particularly to the small size of the DGF1 group; therefore, we cannot generalize the differences between this group and the EGF, SGF, and DGF2 groups. However, this study intended to find the characteristics of SGF in comparison with the severe form of ischemia–reperfusion injury. Thus, we think that the distinct characteristics of the DGF2 group might be lost if all patients who require dialysis are classified into the same group. In addition, baseline characteristics were different between groups, so it could be uncertain whether the results are caused by poor donor and recipient factors, or SGF itself. However, we included all variables known to influence renal function in multivariate analysis and found that the impact of SGF was independent of baseline characteristics as well as acute rejection or proteinuria. Lastly, despite our efforts to adjust for the variables that affect graft function, there could be confounders because of the retrospective design of the study. It is known that SGF shares risk factors with DGF [3]; thus, we thought that using variables related to DGF would be sufficient to adjust for confounders related to SGF.
In conclusion, renal function in the SGF group was analyzed systematically in this study. SGF exhibited different characteristics in terms of recipient, donor, and transplantation-related factors compared with EGF. Rather, SGF shares similar characteristics with DGF. We conclude that SGF may be an independent risk factor for poor renal function after DKT and that SGF may cause undesirable long-term outcomes. To confirm whether SGF affects long-term outcomes, a large-scale, long-term prospective cohort-based study is needed.
References
Cavaille-Coll M, Bala S, Velidedeoglu E, Hernandez A, Archdeacon P, Gonzalez G, Neuland C, Meyer J, Albrecht R (2013) Summary of FDA workshop on ischemia reperfusion injury in kidney transplantation. Am J Transplant 13(5):1134–1148
Humar A, Johnson EM, Payne WD, Wrenshall L, Sutherland DE, Najarian JS, Gillingham KJ, Matas AJ (1997) Effect of initial slow graft function on renal allograft rejection and survival. Clin Transplant 11(6):623–627
Humar A, Ramcharan T, Kandaswamy R, Gillingham K, Payne WD, Matas AJ (2002) Risk factors for slow graft function after kidney transplants: a multivariate analysis. Clin Transplant 16(6):425–429
Rodrigo E, Fernandez-Fresnedo G, Ruiz JC, Pinera C, Palomar R, Gonzalez-Cotorruelo J, Zubimendi JA, De Francisco AL, Sanz de Castro S, Arias M (2005) Similar impact of slow and delayed graft function on renal allograft outcome and function. Transplant Proc 37(3):1431–1432
Karatzas T, Gompou A, Bokos J, Dimitroulis D, Boletis J, Kostakis A, Kouraklis G, Zavos G (2011) Optimal utilization of expanded criteria deceased donors for kidney transplantation. Int Urol Nephrol 43(4):1211–1219
Ojo AO, Wolfe RA, Held PJ, Port FK, Schmouder RL (1997) Delayed graft function: risk factors and implications for renal allograft survival. Transplantation 63(7):968–974
Quiroga I, McShane P, Koo DD, Gray D, Friend PJ, Fuggle S, Darby C (2006) Major effects of delayed graft function and cold ischaemia time on renal allograft survival. Nephrol Dial Transplant 21(6):1689–1696
Yarlagadda SG, Coca SG, Formica RN Jr, Poggio ED, Parikh CR (2009) Association between delayed graft function and allograft and patient survival: a systematic review and meta-analysis. Nephrol Dial Transplant 24(3):1039–1047
Johnston O, O’Kelly P, Spencer S, Donohoe J, Walshe JJ, Little DM, Hickey D, Conlon PJ (2006) Reduced graft function (with or without dialysis) vs immediate graft function—a comparison of long-term renal allograft survival. Nephrol Dial Transplant 21(8):2270–2274
Raimundo M, Guerra J, Teixeira C, Santana A, Silva S, Homens CM, da Costa AG (2013) Intermediate early graft function is associated with increased incidence of graft loss and worse long-term graft function in kidney transplantation. Transplant Proc 45(3):1070–1072
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130(6):461–470
Kidney Disease: Improving Global Outcomes (KDIGO) Transplant Work Group (2009) KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant 9(Suppl 3):S1–155
Ekberg H, Tedesco-Silva H, Demirbas A, Vitko S, Nashan B, Gurkan A, Margreiter R, Hugo C, Grinyo JM, Frei U, Vanrenterghem Y, Daloze P, Halloran PF, ELITE-Symphony Study (2007) Reduced exposure to calcineurin inhibitors in renal transplantation. N Engl J Med 357(25):2562–2575
Gaston RS (2001) Maintenance immunosuppression in the renal transplant recipient: an overview. Am J Kidney Dis 38(6 Suppl 6):S25–S35
Jayaram D, Kommareddi M, Sung RS, Luan FL (2012) Delayed graft function requiring more than one-time dialysis treatment is associated with inferior clinical outcomes. Clin Transplant 26(5):E536–E543
Schroppel B, Legendre C (2014) Delayed kidney graft function: from mechanism to translation. Kidney Int 86(2):251–258
Kasiske BL, Israni AK, Snyder JJ, Patient Skeans MA, Outcomes in Renal Transplantation (PORT) Investigators (2011) The relationship between kidney function and long-term graft survival after kidney transplant. Am J Kidney Dis 57(3):466–475
Remport A, Molnar MZ, Ambrus C, Keszei A, Torok S, Vamos EP, Kiss I, Jaray J, Novak M, Rosivall L, Mucsi I (2010) Impaired renal function is associated with mortality in kidney-transplanted patients. Int Urol Nephrol 42(3):799–809
Nogueira JM, Haririan A, Jacobs SC, Weir MR, Hurley HA, Al-Qudah HS, Phelan M, Drachenberg CB, Bartlett ST, Cooper M (2009) The detrimental effect of poor early graft function after laparoscopic live donor nephrectomy on graft outcomes. Am J Transplant 9(2):337–347
Hellegering J, Visser J, Kloke HJ, D’Ancona FC, Hoitsma AJ, van der Vliet JA, Warle MC (2013) Poor early graft function impairs long-term outcome in living donor kidney transplantation. World J Urol 31(4):901–906
Nel D, Vogel J, Muller E, Barday Z, Kahn D (2012) Slow early graft function: a neglected entity after renal transplantation. Nephron Clin Pract 120(4):c200–c204
Akkina SK, Connaire JJ, Israni AK, Snyder JJ, Matas AJ, Kasiske BL (2009) Similar outcomes with different rates of delayed graft function may reflect center practice, not center performance. Am J Transplant 9(6):1460–1466
Leffondre K, Boucquemont J, Tripepi G, Stel VS, Heinze G, Dunkler D (2015) Analysis of risk factors associated with renal function trajectory over time: a comparison of different statistical approaches. Nephrol Dial Transplant 30(8):1237–1243
Schnitzler MA, Johnston K, Axelrod D, Gheorghian A, Lentine KL (2011) Associations of renal function at 1-year after kidney transplantation with subsequent return to dialysis, mortality, and healthcare costs. Transplantation 91(12):1347–1356
Moranne O, Maillard N, Fafin C, Thibaudin L, Alamartine E, Mariat C (2013) Rate of renal graft function decline after one year is a strong predictor of all-cause mortality. Am J Transplant 13(3):695–706
Li L, Astor BC, Lewis J, Hu B, Appel LJ, Lipkowitz MS, Toto RD, Wang X, Wright JT Jr, Greene TH (2012) Longitudinal progression trajectory of GFR among patients with CKD. Am J Kidney Dis 59(4):504–512
Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO (2012) Clinical practice guideline for the evaluation and management of chronic kidney disease (2013). Kidney Int Suppl 3:1–150
Perkins RM, Bucaloiu ID, Kirchner HL, Ashouian N, Hartle JE, Yahya T (2011) GFR decline and mortality risk among patients with chronic kidney disease. Clin J Am Soc Nephrol 6(8):1879–1886
Rosansky SJ, Glassock RJ (2014) Is a decline in estimated GFR an appropriate surrogate end point for renoprotection drug trials? Kidney Int 85(4):723–727
Yilmaz S, Yilmaz A, Hayry P (1995) Chronic renal allograft rejection can be predicted by area under the serum creatinine versus time curve (AUCCr). Kidney Int 48(1):251–258
Sumrani N, Hong J, Miles A, Markell M, Distant D, Fleishhacker J, Maursky V, Jean-Baptiste F, Sommer B (1996) Posttransplant serum creatinine area under the curve predicts renal allograft outcome. Transplant Proc 28(1):356–357
Hosgood SA, Barlow AD, Johari Y, Bankart MJ, Nicholson ML (2011) Early graft function defined by area under the curve serum creatinine 7 days post-transplant in a series of live donor kidney transplantation. J Surg Res 171(2):838–843
Gaber AO, Mulgaonkar S, Kahan BD, Woodle ES, Alloway R, Bajjoka I, Jensik S, Klintmalm GB, Patton PR, Wiseman A, Lipshutz G, Kupiec-Weglinski J, Gaber LW, Katz E, Irish W, Squiers EC, Hemmerich S (2011) YSPSL (rPSGL-Ig) for improvement of early renal allograft function: a double-blind, placebo-controlled, multi-center phase IIa study. Clin Transplant 25(4):523–533
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the institutional review board of the Samsung Medical Center.
Informed consent
As the study was retrospective and the subjects were deidentified, the IRB waived the need for written consent from patients.
Rights and permissions
About this article
Cite this article
Shin, Jh., Koo, E.H., Ha, S.H. et al. The impact of slow graft function on graft outcome is comparable to delayed graft function in deceased donor kidney transplantation. Int Urol Nephrol 48, 431–439 (2016). https://doi.org/10.1007/s11255-015-1163-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-015-1163-1