Abstract
Venous thromboembolism (VTE) is the most frequent cause of preventable mortality in hospitalized patients and the third leading cause of mortality due to vascular diseases. We aim to describe patients with VTE who required hospitalization, their clinical characteristics, management and evolution after discharge. Prospective cohort which included patients with acute and symptomatic VTE who required hospitalization in a single tertiary center for their management in a 10 years´ period (between 2006 and 2016). Patients were included at the time of VTE diagnosis; we collected baseline characteristics, risk stratification and initial therapeutic approach. They were periodically, prospectively and systematically followed up to evaluate recurrence, bleeding and/or death. Time-to-event analysis was performed for these outcomes related to evolucion after discharge. 3457 confirmed VTE episodes were included for the analysis (1985 DVT, 930 PE and 542 DVT + DVT), corresponding to 3157 patients. Most were elderly, the median age was 68 years (SD 16) with a predominance of women 57% (1955). Most frequent predisposing factors were immobility (45%), active cancer (35%), recent surgery (33%), obesity (26%), recent hospitalization (22%) and previous VTE (21%). One-fourth of pulmonary embolism had sPESI 0 points. Mortality, recurrence and bleeding rates within 30 days were 14%, 10% and 5% respectively. High proportion of VTE require hospitalization for their management, even PE with low sPESI. Mortality and complication remain elevated. We encourage the development and maintenance of more VTE registries in Latin America, to fully understand local characteristics of this disease.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Highlights
-
VTE hospitalization steadily increased over time, particularly for PE events.
-
High proportion of VTE require hospitalization for their management, even PE with low sPESI.
-
LMWH was the most frequent initial treatment, and DOACs were rarely used and exceptional before 2015.
-
VTE patients have long hospital stay, high mortality, recurrence and bleeding rates.
-
We encourage the development and maintenance of more VTE registries in Latin America, to fully understand local characteristics of this disease.
Introduction
Venous thromboembolism (VTE) which includes deep vein thrombosis (DVT) and pulmonary embolism (PE) is the most frequent cause of preventable mortality in hospitalized patients [1] and the third leading cause of mortality due to vascular diseases [2].
An incidence of 1 in 1000 is estimated in the general population, although this is strongly associated with age [3] and 2% in hospitalized patients [4]. Mortality in PE varies between 8 and 17.4% at 3 months [5] In addition, it is associated with a high frequency of recurrence, bleeding, post-thrombotic syndrome and pulmonary hypertension [6].
One of the main sources of VTE data are randomized controlled trials, however, in this type of design, special groups of patients are usually excluded, such as elderly, frail, comorbid, obese, which are very important in practice everyday.
VTE’s clinical relevance has led to the development of registries in different parts of the world [7,8,9,10,11,12,13,14] which are an excellent tool to understand the characteristics of patients in an efficient, fast and systematic way, and that guarantees the avoidance of selection biases. Despite its usefulness and the importance of knowing real world data from local epidemiology, in Argentina and Latin America the use of registries has been limited.
The Hospital Italiano de Buenos Aires (HIBA) has developed an Institutional VTE Registry (RIET) since 2006 that includes all patients with an objective diagnosis of symptomatic VTE and that has a periodic and systematic follow-up after discharge. To our knowledge, there is no other active prospective registry in Latin America in continuous operation for so many years and with the inclusion of so many patients.
The main aim of this study is to describe the clinical characteristics, medical management, and outcome of all patients with acute and symptomatic VTE who required hospitalization (either for VTE management as the primary reason, or those with another reason of hospitalization who had a hospital-acquired VTE) at HIBA, during a 10 year period.
Methods
Design
We performed a prospective cohort study which included patients with acute and symptomatic VTE who required hospitalization in a tertiary level center (Hospital Italiano de Buenos Aires) for their management in a 10 year period (between 2006 and 2016).
Setting
The Hospital Italiano de Buenos Aires is a community-based tertiary care hospital in Buenos Aires city, Argentina. It carries approximately 200,000 admissions and 2,5 millions of outpatients visits annually. It counts with a problem-oriented electronic health record (EHR), in which clinical and administrative information is available, including prescriptions, diagnostic tests, and clinical evolution. The Thromboembolic Disease Institutional Registry (IRTD, or RIET in spanish) is integrated into the EHR system, both for the alert system for patient’s capture and for data storage.
Data collection proceeding
The RIET (Home-ClinicalTrials.gov, NCT01372514) is an observational, prospective registry active from 2006, which includes all outpatients and or hospitalized in general wards and intensive care units, with both surgical and medical-based pathologies, in which acute VTE is objectively diagnosed [12]. The registry was also evaluated and approved by the Institutional Review Board.
Recruitment was designed based on specific imagining and laboratory studies for VTE: D-dimer, computed pulmonary thorax 64 multi slice angio-tomography, lungs ventilation-perfusion scintigraphy, venous Doppler ultrasound of the lower and/or upper limbs or digital angiography of the lungs and/or veins of the lower and/or upper limb. Possible cases are captured for detection of eligible patients using a computerized alert system that reports whenever the physician requests one of the mentioned tests.
From the eligible patients recruited from the registry alert system, patients were included prospectively if met these criteria: 1. Over 17 years of age; 2. confirmed PE and/or DVT in limbs or upper extremities with validated diagnostic methods. All patients who refused to participate in the study after the informed consent process were excluded. For the purposes of this particular paper, only patients who required hospitalization for clinical management were included.
Patient evaluation was assessed by advanced medical students (as research trainees), who were specially trained, standardized and certified periodically for this objective. Data collection comes from the patient’s interview and from the EHR revision. All data obtained feedback from the EHR, completing the information for each included patient. This additional function allows the interaction between registries performed at the hospital to complete and improve the quality of the medical information for each patient [12].
Specially trained medical students carried out prospective data collection and performed the Wells score. They interviewed both the patient and the treating physician using a standardized data collection form. The standardized data collection form includes comorbidities, assessment of the risk factors of VTE, and treatment. The medical students were blinded to the results of the imaging test and the radiologists reporting the results were unaware of the Wells score. Collected data was also reviewed by other members of the study team to ensure that no data were missed.
The following variables were collected from patient medical records and by interviewing both the patient and the treating physician: clinical characteristics, history of heart failure, moderate renal failure (glomerular filtration rate—GFR— < 60 ml/min), severe renal failure (GFR < 30 ml/min), chronic obstructive pulmonary disease, use of estrogen by women at the moment of evaluation, history of surgery within 4 weeks, immobilization within 4 weeks, Charlson comorbidities score and body mass index. The length of hospitalization was calculated from time in days of admission to discharge or death.
Definitions of VTE
The presence of PE was defined using standardized criteria. Images for angio-CT scans were acquired using a 64-multislice CT scanner (Aquilion, Toshiba) using a standardized contrast infusion protocol. Pulmonary embolism was considered diagnosed when: 1-An angio-CT scan showed a filling defect in the main pulmonary artery, segmental or subsegmental branches; 2-A ventilation/perfusion pulmonary scan was reported as high or intermediate probability (with a positive compression whole leg ultrasound showing DVT) as defined by the PIOPED criteria; 3-Angiography demonstrating an intraluminal filling defect or the trailing edge of a thrombus obstructing a vessel; or 4- A whole leg venous ultrasound showing a non-compressible segment above the trifurcation of the popliteal vein showing a DVT associated with clinical symptoms for PE. The radiologists reporting the tests were unaware of the Wells score results. Information on the use of D-dimer was collected. Patients were evaluated using VIDAS D-dimer and/or BIO Merieux. All D-dimer levels of 500 ucg/L or less were considered normal. The clinical probability of PE was estimated using the modified version of the Wells score for all participants [15, 16]. DVT was considered present when was confirmed with a venous Doppler ultrasound.
Simplify Wells’ score ranged from 0 to a maximum of 12.5 points. Those with scores of ≤ 4 were categorized as PE unlikely, while those with more than 4 points were categorized as PE likely.
Outcomes from follow up
In order to assess outcomes related to evolution after discharge (defined as recurrence, bleeding and/or death), all patients were followed at 30 days, 3 and 12 months. We made a standardized telephone interview and a review of EHR.
Other variables definitions
Active Cancer: We define “active cancer” to those patients with cancer diagnosis or relapse in the last 5 years, and/or who are undergoing chemotherapy, radiotherapy, hormonal therapy or palliative care.
Elevated proBNP: the cut-off value used to define elevated proBNP was related to the normal values according to the age of the patients. These are: Adults up to 44 years: 125 pg/ml, 45 to 54 years: 172 pg/ml, 55 to 74 years: 350 pg/ml, and 75 years or older: 750 pg/ml. Those values above these cut-offs were defined as “elevated”.
Elevated sPESI score: the cutoff value used to define high risk was 1 point or higher.
Respiratory assistance: refers only to invasive ventilation.
Statistical analyses
Patients’ baseline characteristics were summarized using proportions for categorical variables and mean and standard deviation (SD) or median and interquartile range (IQR) for continuous variables, as appropriate. A conventional analysis was performed for descriptive and comparative statistics, considering a significant p value < 0.05.
Additionally, time-to-event analysis was performed for outcomes related to evolution after discharge. We presented recurrence, major bleeding and mortality rate at 30, 60, 90, 180 days and 1 year. The simplified PESI was calculated for all patients with PE to stratify PE events and its correlation with 30 days mortality [16].
To explore associated factors, we first characterized the study patients using univariable methods. Then, we selected potential contributing factors using multivariable models, using the cox proportional hazards regression model. We presented unadjusted and adjusted hazard ratios (HRs) with their accompanying 95% CIs.
All analyses were performed with the Stata v. 16 software.
Results
During the study period, a total of 3457 were included for analysis, corresponding to 3157 patients (see Fig. 1) who were hospitalized for their initial management. The proportion of patients admitted with VTE as the primary reason for hospitalization was 67.66% (2339), while the rest were hospital-acquired VTE.
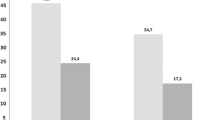
In the study period, the hospitalized VTE frequency increased considerably, DVT doubled (from 100 to 203 yearly) and PE increased 5 times (from 71 to 205 yearly). However, during the 10-year period of the study, a progressive reduction in proportional cases of DVT can be observed (from 74% in 2006 to 50% in 2016), at the expense of a proportional increase in PE cases (from 26% in 2006 to 50% in 2016), (see Fig. 2).
Most of the patients were women and elderly with a median age of 68 (SD 16), 64% were older than 65 years old and 25% of all the patients were 80 years old or older. The most common risk factors were immobility, active cancer, major surgery, obesity, recent hospitalization and VTE history. Sixty-nine percent had two or more risk factors (RF) and 37% had at least 3 RF (Table 1).
The most relevant clinical findings were limb pain (40.5%) and asymmetry (31%) in DVT cases and dyspnea (35%), tachycardia (33.5%), limb pain (9,5%) and asymmetry (8%), hypotension (7%) and blood oxygen saturation < 90% (1.8%) in PE cases.
To stratify the prognosis we performed the simplified PESI score (sPESI) to the patients with PE and those with PE combined with DVT. Twenty-two percent of PE and 29% of PE with DVT patients required hospitalization even with sPESI score of 0 points and most patients had 1 or 2 sPESI points. When analyzing PE cases annually, we found that the proportion of PE with 0 points in the sPESI, remained stable, without significant variations, between 28% and 31%, during the study period (Table 2).
More than 91.7% of cases received some kind of treatment. Most were LMWH (86%), of which 33% were prescribed since the beginning in combination with a vitamin K antagonist (VKA). Less than 2% of DVT and 0.6% of PE received an inferior cava vein (IVC) filter, respectively; and thrombectomy with or without fibrinolytics were indicated in 0.6% of the whole population. Very few patients were treated with DOACs during their hospitalization, and this was exceptional before 2015 (Table 3).
The median hospitalization length time was 10 days for VTE, 12 for DVT and 8,5 for PE, without statistically difference between all of them. During that time, the need for intensive care units (ICU) and respiratory assistance was 44% and 4% for DVT and 54% and 2,8% for those with PE, respectively. Most patients with PE received a cardiac ultrasound, of those 20% presented dilation or disfunction of the right ventricle and 16% had pulmonary hypertension. The biomarkers were elevated in most PE patients (Table 4).
PE patients with sPESI 0 had a 30-day mortality of 5% (95% CI 3–8%). Mortality at 30 days for patients with 1, 2 and 3 point sPESI was 12% (CI 10–15%), 22% (CI 18–26%) and 35% (CI 26–55%), respectively. In Fig. 3 it is represented by the 30 days mortality of patients with sPESI 0 vs the combination of the rest of patients (sPESI ≥ 1).
The overall mortality rate was 46% (n = 1612, 95% CI 45–48%). The mortality rate was 14% (95% CI 13–15%), 20% (95% CI 19–22%), 24% (95% CI 23–26%), 27% (95% CI 26–29%) and 35% (95% CI 33–36%) at 30, 60, 90, 180 days and 1 year, respectively.
The variables associated with higher mortality risk were PE, older age, active cancer, elevated proBNP value and the higher sPESI score. After adjustment only active cancer (HR 2.44 95% CI 1.97–3.03, p < 0.001), sPESI (HR 1.29 95% CI 1.13–1.48, p < 0.001) and proBNP (HR 1.01 95% CI 1.01–1.1, p 0.001) remained statistically significant.
Overall VTE recurrence rate was 15% (n = 527, 95% CI 15–16%). VTE recurrence rate was 10% (95% CI 10–12%), 12% (95% CI 11–13%), 13% (95% CI 12–14%) and 19% (95% CI 15–24%) at 30, 60, 90 days and 1 year, respectively. The only variable associated with higher recurrence risk was active cancer (HR 1.42 95% CI 1.12–1.78, p 0.003).
The overall bleeding incidence rate was 12% (N = 158, 95% CI 10–13%). The bleeding rate was 5% (95% CI 4–6%), 6% (95% CI 5–8%), 7% (95% CI 6–8%), and 10% (95% CI 8–12%) at 30, 60, 90 days and 1 year, respectively. The variables associated with a higher bleeding risk were anticoagulation therapy (HR 2.19 95% CI 1.38–3.5, p 0.001) and the use of IVC filter (HR 2.07 95% CI 1.3–3.29, p 0.002).
Discussion
In this study we described only those patients who had to be hospitalized for proper initial management (either due to the VTE severity or their associated comorbidities), as well as those who were already hospitalized for other reasons when they developed VTE, as a complication.
Despite CPGs recommendations about acute VTE home treatment [17], hospitalization increased (from 125 in 2006 to 408 in 2016) for patients with severe VTE events and/or major comorbidities. The increased VTE prevalence during the 10-year observation period may have several explanations. On the one hand, the alarm and case capture system was constantly improved through monitors and researchers training, quality control and continuous improvement in real time actions for the VTE registry [12]. On the other hand, the PE tripled, this could probably have been influenced by the increase in the incidental PE detection, found during follow-up controls in cancer patients. This fact was previously described in the literature [13, 14]. However, there is also an increase in the symptomatic DVT (without PE) cases, and this increase is not justified from studies conducted for other reasons, but a real increase. Another observation is that the DVT frequency was declining relatively in relation with PE frequency, which increased markedly. This could be explained by the increased DVT outpatient management from the emergency department, avoiding their hospitalization.
The mean age of the patients was similar to previous studies [18]; and most patients were elderly, older women over 65 years old and 25% were very old (over 80 years old). The advanced age of these patients is to be expected for several reasons. First, a high proportion of hospitalized patients belong to the hospital health insurance system (called Plan de Salud) that has 160,000 members, of which 64,000 are 65 years old or older. Besides, advanced age is an associated factor related to other comorbidities and frailty that explains hospitalization criteria.
In accordance with other studies, the most frequent VTE risk factors (RF) were immobility, active cancer, recent major surgery or hospitalization, obesity, and VTE history [19]. In fact, more than two-third of patients had at least two RF and more than one-third of the cases had three or more RF at the time of the VTE event. The high number of risk factors in our cohort can be explained by the fact that these are hospitalized patients, either due to a high risk of complications that prevents outpatient management and/or because they were hospitalized for other pathologies and developed VTE as a complication during their stay.
The PESI and sPESI scores accurately classified PE cases with low or high risk of adverse medical outcomes. Both scores were recently validated in our country in a cohort of 684 PE patients [20]. In our cohort of hospitalized patients, the median sPESI score was greater than 1; however, 22% of the PE patients and 29% of the PE patients combined with DVT had sPESI score of 0. Even when 0 sPESI cases might be candidates for home management, we think that there are several potential explanations that might justify the admission of these patients. First of all, the first recruited patients are from 2006, when clinical practice guidelines still did not recommend home DVT or PE treatment. More recently, ACCP [17] and ESC [21, 22] suggested categorizing patients according to their risk and selecting those with very low risk, with a sPESI of 0 points, as outpatient treatment. Another explanation could be the presence of any of the items in the Hestia score like a social reason for admission or frailty. Finally, nearly one-third (32%) were already hospitalized for another medical problem when VTE was diagnosed.
Less than 10% of cases did not receive any specific therapy because they were in the palliative care stage. Most cases received treatment with LMWH followed by VKA, 6% received parenteral NFH, 0.5% received thrombolytics and only 0.75% were treated with DOACs. This management seems adequate since they were hospitalized patients; on the other hand, the introduction of DOACs in Argentina occurred gradually during the years in which this study was carried out and they began to be used for well-selected outpatients and not during hospitalization. An interesting finding is that only 1.51% of VTE patients received an IVC filter and the main reasons for its use were active bleeding or the need for invasive procedures. This reflects institutional adherence to the recommendations of most scientific societies regarding the specific indications of IVC filters in VTE patients [23,24,25]. This recommendation reflects the lack of evidence on reductions in mortality and an increase in DVT incidence with the use of IVC filters [25].
It is striking that the median hospitalization for DVT (12 days) was longer than for PE (8 days); our interpretation for this tendency is that patients developed DVT when they were hospitalized for complex pathologies. This could be supported by the high requirement for ICU (44%) and mechanical ventilation (4%) among DVT patients. Another possible explanation is that incidental cases of PE (detected in cancer patients screening or control) were initially managed with hospitalization, but quickly discharged.
VTE recurrence and major bleeding incidence were similar to reports of Prandoni et al. and Arcelus et al. [25, 26]. We think that high it could be explained by the study population characteristics (cancer, elderly, others comorbidities), which increase both. In fact, we found that the combination of PE events with advanced age were associated with greater VTE recurrence and PE events, in accordance with previous reports [27]. On the other side, major bleeding was associated with anticoagulant therapy and the insertion of IVC filters. This last variable is probably a consequence of bleeding, and not a cause.
According to our findings, the overall mortality rate was high (18% at 90 days) and similar to the ICOPER report (17.4% at 90 days) [5]. Higher mortality was associated with PE diagnosis, active cancer, elevated proBNP value and the higher sPESI score. Although in our multivariate analysis, increasing age appears to be a protective factor for overall mortality, we interpret this result to be influenced by a survival bias. Although it would have been interesting to provide more data about mortality cause (directly related to VTE or not), this was not possible due to the death reporting code system, making it very difficult to discriminate with certainty the true cause. PE patients with sPESI 0 had a 30-day mortality rate much higher than other reports [28, 29]. However, our cohort only included hospitalized patients.
Some limitations must be mentioned. First, is a single-center study from a third level complexity hospital, which included systematically and consecutively all patients from the Institutional Registry. This information provides a good estimation of the current clinical management of VTE in different settings (outpatients, hospitalized patients -medical or surgical pathology- and critical care units). Second, it is a descriptive study (does not have the purpose to compare diagnostic, therapeutic or outcome strategies), but it is very useful to identify the true strategies used in real clinical local practice.
Registries are very important tools that provide real world data generated during routine clinical practice, analyzing effects of drugs over a longer period of time. We encourage the development and maintenance of more VTE registries to fully understand local characteristics of this disease. Our next challenge will be to include other Latin American medical centers to generate regional information.
Conclusion
VTE hospitalization steadily increased over time, particularly for PE events.
LMWH is the most frequent modality of initial treatment in hospitalized patients.
VTE patients have long hospital stay, high mortality, recurrence and bleeding rates.
The sPESI with 0 points maintains its ability to detect patients with lower risk; however, in hospitalized patients, the 30-day mortality of this subgroup is 5 times higher than that described when applied in the emergency department.
References
Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR et al (2008) Prevention of venous thromboembolism: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 133(6 Suppl):381S–453S
Grosse SD, Nelson RE, Nyarko KA, Richardson LC, Raskob GE (2016) The economic burden of incident venous thromboembolism in the United States: a review of estimated attributable healthcare costs. Thromb Res 137:3–10
Vázquez F, Posadas-Martínez M, Vicens J, de Quirós FGB, Giunta D (2013) Incidence rate of symptomatic venous thromboembolic disease in patients from a medical care program in Buenos Aires, Argentina: a prospective cohort [Internet]. Thromb J 11:16. https://doi.org/10.1186/1477-9560-11-16
Grande Ratti MF (2018) Incidence of hospital-acquired venous thromboembolic disease [Internet]. Revista de la Facultad de Ciencias Médicas 75:82. https://doi.org/10.31053/1853.0605.v75.n2.17243
Goldhaber SZ, Visani L, De Rosa M (1999) Acute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER). Lancet 353(9162):1386–1389
Chitsike RS, Rodger MA, Kovacs MJ, Betancourt MT, Wells PS, Anderson DR et al (2012) Risk of post-thrombotic syndrome after subtherapeutic warfarin anticoagulation for a first unprovoked deep vein thrombosis: results from the REVERSE study. J Thromb Haemost 10(10):2039–2044
Suárez Fernández C, González-Fajardo JA, Monreal Bosch M, Grupo del Registro (RIETE) (2003) Computerized registry of patients with thromboembolic disease in Spain (RIETE): background, objectives, methods, and preliminary results. Rev Clin Esp 203(2):68–73
Albertsen IE, Søgaard M, Goldhaber SZ, Piazza G, Skjøth F, Overvad TF et al (2020) Development of sex-stratified prediction models for recurrent venous thromboembolism: a Danish Nationwide Cohort Study. Thromb Haemost 120(5):805–814
Ohashi Y, Ikeda M, Kunitoh H, Sasako M, Okusaka T, Mukai H et al (2018) Venous thromboembolism in patients with cancer: design and rationale of a multicentre, prospective registry (Cancer-VTE Registry). BMJ Open 8(5):e018910
Ageno W, Haas S, Weitz JI, Goldhaber SZ, Turpie AGG, Goto S et al (2019) Characteristics and management of patients with venous thromboembolism: the GARFIELD-VTE Registry. Thromb Haemost 119(2):319–327
Lei J, Xu X, Ji Y, Yang Y, Yi Q, Chen H et al (2020) Rational and design of the China Pulmonary Thromboembolism Registry Study (CURES): a prospective multicenter registry. Int J Cardiol 1(316):242–248
Posadas-Martinez ML, Rojas LP, Vazquez FJ, De Quiros FB, Waisman GD, Giunta DH (2016) Statistical process control: a quality tool for a venous thromboembolic disease registry. J Regist Manag 43(2):82–86
Kempny A, McCabe C, Dimopoulos K, Price LC, Wilde M, Limbrey R et al (2019) Incidence, mortality and bleeding rates associated with pulmonary embolism in England between 1997 and 2015. Int J Cardiol 277:229–234. https://doi.org/10.1016/j.ijcard.2018.10.001
Barco S, Mahmoudpour SH, Valerio L, Klok FA, Münzel T, Middeldorp S et al (2020) Trends in mortality related to pulmonary embolism in the European Region, 2000-15: analysis of vital registration data from the WHO Mortality Database. Lancet Respir Med 8(3):277–287
Wells PS, Anderson DR, Rodger M, Ginsberg JS, Kearon C, Gent M et al (2000) Derivation of a simple clinical model to categorize patients probability of pulmonary embolism: increasing the models utility with the SimpliRED D-dimer. Thromb Haemost 83(3):416–420
Aujesky D, Obrosky DS, Stone RA, Auble TE, Perrier A, Cornuz J et al (2005) Derivation and validation of a prognostic model for pulmonary embolism. Am J Respir Crit Care Med 172(8):1041–1046
Guyatt GH, Norris SL, Schulman S, Hirsh J, Eckman MH, Akl EA et al (2012) Methodology for the development of antithrombotic therapy and prevention of thrombosis guidelines: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):53S–70S
Arcelus JI, Caprini JA, Monreal M, Suárez C, González-Fajardo J (2003) The management and outcome of acute venous thromboembolism: a prospective registry including 4011 patients. J Vasc Surg 38:916–922. https://doi.org/10.1016/s0741-5214(03)00789-4
Nordström M, Lindblad B, Bergqvist D, Kjellström T (1992) A prospective study of the incidence of deep-vein thrombosis within a defined urban population. J Intern Med 232:155–160. https://doi.org/10.1111/j.1365-2796.1992.tb00565.x
Burgos LM, Scatularo CE, Cigalini IM, Jauregui JC, Bernal MI, Bonorino JM et al (2020) External validation of prognostic scores for in-hospital and 30-day mortality in patients with pulmonary embolism in Argentina. Medicina 80(5):462–472
Cardiology (esc) European Society of, (ESC) European Society of Cardiology (2015) 2014 ESC Guidelines on the Diagnosis and Management of Acute Pulmonary Embolism [Internet]. Russ J Cardiol. https://doi.org/10.15829/1560-4071-2015-8-67-110
Saar JA, Maack C, European Society of Cardiology (2015) Diagnosis and management of acute pulmonary embolism. ESC guidelines 2014. Herz 40(8):1048–1054
Kearon C, Akl EA, Comerota AJ, Prandoni P, Bounameaux H, Goldhaber SZ et al (2012) Antithrombotic therapy for VTE disease: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141(2 Suppl):e419S–e496S
Osteresch R, Fach A, Hambrecht R, Wienbergen H (2019) ESC guidelines 2019 on diagnostics and management of acute pulmonary embolism. Herz 44(8):696–700
Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P et al (1998) A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. Prévention du Risque d’Embolie Pulmonaire par Interruption Cave Study Group. N Engl J Med 338(7):409–415
Prandoni P, Lensing AW, Cogo A, Cuppini S, Villalta S, Carta M et al (1996) The long-term clinical course of acute deep venous thrombosis. Ann Intern Med 125(1):1–7
Monreal M, Lafoz E, Ruiz J, Ma Callejas J, Arias A (1994) Recurrent pulmonary embolism in patients treated because of acute venous thromboembolism: a prospective study. Eur J Vasc Surg 8:584–589. https://doi.org/10.1016/s0950-821x(05)80595-x
Jiménez D, Aujesky D, Moores L, Gómez V, Lobo JL, Uresandi F et al (2010) Simplification of the pulmonary embolism severity index for prognostication in patients with acute symptomatic pulmonary embolism. Arch Intern Med 170(15):1383–1389
Masotti L, Panigada G, Landini G, Pieralli F, Corradi F, Lenti S et al (2016) Simplified PESI score and sex difference in prognosis of acute pulmonary embolism: a brief report from a real life study. J Thromb Thrombolysis 41(4):606–612
Funding
This manuscript has no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the Authors declare that they have no conflict of interest.
Ethics
Institutional review board approval.
Consent to participate
For this type of study, formal consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vázquez, F.J., Grande-Ratti, M.F., Zapiola, M.E. et al. Hospitalization for venous thromboembolic disease management: a 10 years Registry in Buenos Aires, Argentina. J Thromb Thrombolysis 52, 1187–1194 (2021). https://doi.org/10.1007/s11239-021-02459-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-021-02459-7