Abstract
Background
Health-related quality of life (HRQoL) is an important outcome in coronary heart disease (CHD). However, variability in HRQoL indicators suggests a need to consider domain coverage. This review applies a globally accepted framework, the International Classification of Functioning, Disability and Health (ICF), to map HRQoL measures that are reliable and valid among people with CHD.
Methods
The Embase, Pubmed and PsycInfo databases were searched, with 10 observational studies comparing HRQOL among 4786 adults with CHD to 50949 controls identified. Study reporting quality was examined (QualSyst). Hedges’ g statistic (with 95% CIs and p values) was used to measure the effect size for the difference between group means (≤ 0.2 small, ≤ 0.5 medium, ≤ 0.80 large difference), and between-study heterogeneity (tau, I2 test) examined using a random effects model.
Results
Adults with CHD reported lowered HRQoL (gw = − 0.418, p < 0.001). Adjusted mean differences in HRQoL ratings, controlling for socio-demographics, were smaller but remained significant. Large group differences were associated with individual measures of activity and participation (WHOQOL g = − 1.199, p < 0.001) and self-perceived health (SF 36 g = − 0.616, p < 0.001).
Conclusions
The ICF provides a framework for evaluating and understanding the impact of CHD on HRQoL. The results demonstrate that HRQoL goes beyond physical symptoms, with activity limitations, social support and participation, and personal perceptions identified as key ICF domains in CHD assessment. Further investigations are needed to unravel the dynamic and inter-relationships between these domains, including longitudinal trends in HRQoL indicators.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Coronary heart disease (CHD) remains one of the most common, costly and preventable health problems, worldwide [1, 2]. The disease burden of CHD is often estimated using measures of health-related quality of life (HRQoL). HRQoL refers to people’s capacity to perform daily activities (i.e. functioning) in addition to their life perspective (i.e. well-being) and subjective management of their health condition [3]. Although the influence of CHD on HRQoL is well studied, few studies have used concurrent or historical controls to provide evidence that CHD has a dramatic effect on HRQoL. Available comparative data also do not provide consistent evidence: some persons with CHD appear to manage their psychological symptoms [4, 5], while others perceive themselves as unable to cope, reporting significantly poorer HRQoL—even after adjusting for age and gender-specific changes [6] or number of comorbidities [7]. As such, the distinct impact of CHD on HRQoL remains unclear.
Conceptual differences across generic HRQoL measures may, in part, explain these discrepant findings. Researchers can select single-item (e.g. Visual Analogue Scale; VAS) or multiple-item (e.g. Short Form Health Survey; SF-36) measures, although there are concerns about VAS being inferior to choice-based methods for measuring a complex construct such as HRQoL [8]. Moreover, some multi-item measures define HRQoL domains more inclusively than others. For example, the World Health Organisation Quality of Life-BREF (WHOQOL-BREF) conceptualises ‘psychological health’ as encompassing an individual’s cognitive function, self-esteem, body image and feelings—however, this construct is limited to anxiety and depression in the EuroQOL-5D [9]. Similarly, the 36-item Short Form Health Survey (SF-36) comprises of eight domains with a focus on physical and psychosocial functioning, whereas the WHOQOL-BREF is based on a four-domain structure which includes daily living, bodily image and appearance, relationships and environmental-financial resources [10]. Given the multi-dimensional structure of HRQoL, it is important that measures and their subscales be examined individually and, where possible, domain-specific content compared [11].
The International Classification of Functioning, Disability and Health (ICF), developed in 2001 by the World Health Organisation (WHO [12]), can be used to provide an assessment framework for HRQoL in CHD. In brief, the ICF considers the individual’s level and pattern of “functioning” as central to assessment, treatment planning and outcome [12]. The ICF systematically groups a person’s health condition by means of four separate, but related constructs: (1) the physiological and emotional processes that occur within the human body (body structures and function); (2) limitations and restrictions in life activities and subsequent participation levels; and contextual variables: (3) social and attitudinal environment alongside (4) internal personal factors (refer to Fig. 1). Each construct comprises a hierarchical system of domains which are numerically coded. In doing so, the ICF allows for a concurrent focus on physical, psychological and social well-being in multi-disciplinary assessment and treatment intervention, in addition to reinforcing the need to utilise integrative measures of functioning [13, 14]. However, in its original form, the ICF comprises an exhaustive list of some 1400 domains [12]. As evidence of the promise to integrative translational science, ICF core sets have been developed to help guide multi-disciplinary rehabilitation assessment. This includes brief and comprehensive core sets for CHD [15].
The current systematic review, with meta-analysis, applies the ICF to explore the unique implications of CHD on HRQoL. This includes physical and psychological symptoms which affect daily physical and social activities in the living environment, while taking into account personal factors that may impact on HRQoL. Our primary research question was: Which HRQoL indicators, as defined by the ICF, differentiate adults living with CHD in comparison to non-clinical peers? By translating and mapping existing HRQoL measures by ICF domains, we hope to facilitate current understanding and evaluation of ICF concepts in CHD management whilst also promoting a standardised way to document and assess HRQoL in this cohort [12].
Method
Literature search
The Embase, PsycINFO and PubMed databases were searched from inception (Embase 1947; PsycINFO 1967; Pubmed 1996) to December 2017 for studies that examined HRQoL in persons with CHD relative to an independent control group (i.e. general population). PRISMA guidelines [16] were followed, with key CHD (e.g. ‘coronary heart disease’, ‘coronary occlusion’) and HRQoL (e.g. ‘quality of life’) terms tailored to the Emtree (Embase), Thesaurus (PsycINFO) and MeSH (Pubmed) vocabulary (see logic grids in Table A, online supplementary material). Search terms were checked for accuracy by a research librarian. Additionally, the reference lists of eligible studies and relevant CHD reviews [11, 17, 18] were hand-searched and one corresponding author contacted requesting additional statistical information. Although this process did not lead to the discovery of any new studies, it helped to ensure that all relevant papers were identified. Searches were conducted by the first author (J.L) and fourth author (E.P) independently and discrepancies resolved through consensus. The study protocol is registered on the PROSPERO database (registration CRD42018085687).
Eligibility criteria and study selection
For a study to be included in this review, it needed to (a) recruit an adult sample (i.e. age ≥ 18 years) with CHD, as determined by medical examination (e.g. electrocardiography, CT angiography), clinical interview [e.g. Braunwald clinical classification; 19] or patient-reported information (e.g. symptom checklist). Studies also had to utilise (b) a validated (single or multi-item) HRQoL measure [3, 20] and (c) an independent group design, whereby individuals with CHD were compared to a non-clinical control group (i.e. general population, healthy peers). Finally, studies had to (d) provide parametric data to calculate standardised mean group differences in the form of Hedges’ g (e.g. means, standard deviations, standard errors); and (e) be published in English to allow results and methodological details to be extracted effectively and to ensure methodological rigour [21].
Studies which referenced population norms as comparative HRQoL data were ineligible, given that early normative data may not be representative due to changes in population composition over time [i.e. age, education, economic status; 22, 23]. In addition, CHD intervention studies (e.g. coronary artery bypass grafting, cardiac rehabilitation) were excluded unless there was a true baseline period in which data prior to the intervention was available.
The initial literature search produced 11,766 potentially relevant studies, from which 1497 duplicates were identified and removed. The titles and abstracts of the remaining 10,269 studies were screened against the eligibility criteria, resulting in a final sample of 10 independent studies [4,5,6,7, 24,25,26,27,28,29] with no overlapping data identified (see Fig. 2). To ensure that studies were selected in an unbiased, rigorous manner, a subset of 30 studies were independently checked by two co-authors (D.S.D, P.J.T), with unanimous inter-rater agreement.
Data collection and preparation
As per the PRISMA guidelines [16], key sample demographics (e.g. age, gender, N), study characteristics (e.g. country, HRQoL measurement, recruitment source, design) and effect size data (e.g. means, SDs) were extracted from each study using a purposely formulated data extraction spreadsheet. Three studies provided variance estimates (i.e. 95% confidence intervals) or exact p values, requiring data conversions [30].
To facilitate data interpretation, individual effect estimates were grouped according to the four ICF domains and 11 categories, each represented by a numeric code: body functions and structures (i.e. anatomy, physiology, psychology of the human body: memory, energy and drive, hearing, continence, pain, emotional functions); activities and participation (i.e. recreation and leisure, moving around, carrying out daily routine); environmental and personal factors (i.e. general health perception, gender) [13, 31, 32]. The linking process was jointly conducted by the first (J.L) author in consultation with the second author (D.S.D) and in accordance with the ICF rules [14, 33]. The results are displayed in Table B of the online supplementary material.
Study reporting quality
Included studies were evaluated for their methodological rigour or reporting detail using the QualSyst [34]. Each item, per study, was rated as ‘Yes’ (score of 2; adequately addressed), ‘Partial’ (score of 1; partially addressed), ‘No’ (score of 0; not addressed’) or not applicable. Two scores were calculated: a summary score for each study (score range: 0–22), reflecting the extent to which studies fulfilled each criteria, and the percentage of studies receiving scores of 2, 1 and 0 for each item. Three criteria specific to intervention studies (random allocation, blinding of investigators, blinding of subjects) were excluded from calculation of the summary score. The first (J.L) and fourth author (E.P) completed this quality appraisal independently. Inter-rater reliability was substantial to excellent (Cohen’s kappa 0.71–0.91), with high agreement ranging from 82 to 100%.
Statistical analysis
Comprehensive Meta-analysis Software (CMA, Version 3.0 Englewood, NJ: Biostat Inc) was utilised for the data analysis. Specifically, standardised mean differences were calculated to estimate the extent to which CHD and control groups differed in self-reported HRQoL. Given the dissimilarity in sample sizes within and between studies, Hedges’ g, which utilises a standard deviation weighted by sample size, was the most suitable estimate [35]. Cohen’s [36] guidelines for the interpretation of g were applied whereby small effect ≥ 0.2, a moderate effect ≥ 0.5, and a large effect ≥ 0.8.
When calculating g, studies that used the same HRQoL measure were pooled, with individual effect estimates weighted by the inverse of the variance (gw), accommodating for higher variability inherent in smaller sample sizes [37]. Composite HRQoL measures and their individual subscales were both examined to avoid confounding or masking any differences that may be present at the individual subscale level. If a study provided more than one effect estimate for a single ICF domain, an average g was obtained for that study prior to pooling. Similarly, from the single longitudinal study reviewed [29], only baseline comparative data were utilised—although HRQOL changes over time were noted. The direction of g was standardised so that a negative value reflected lower HRQoL among those with CHD. The precision of both individual and weighted effect sizes was determined by calculating confidence intervals (95% CIs), with p values additionally calculated to determine the statistical significance of g. Forest plots illustrated the distribution of effect sizes across studies.
Given the pervasive ‘file drawer’ problem, whereby significant and strong results are more likely to be published, some publication bias may be possible [38]. Fail-safe N statistics (Nfs) were calculated to determine how many hypothetical publications would be required to reverse both individual g’s reported by included studies and pooled gw’s to a small, statistically unimportant effect size (i.e. g = 0.2, [38]). In general, the larger the Nfs, the more robust the estimate. For this review, a Nfs was considered adequate if it exceeded the number of studies that contributed to an effect estimate.
To account for the amount and nature of variation in effect size estimates, two measures of between-study heterogeneity were used: the tau statistic (τ), which is analogous to a standard deviation for the overall gw effect [37], and I2—which is expressed as a percentage [39]. Given that I2 may be underpowered when the number of studies being meta-analysed is small [37], individual effect sizes for each study that contributed to a mean g were additionally examined. These analyses were performed using a random effects model [40, 41].
Moderator analyses
The relative contribution of a key methodological characteristic—the use of demographically matched CHD and control groups—to variability in HRQoL effect estimates was examined with Cochran’s Q test [37]. This analysis used a mixed-effect model, consisting of a random effects model within subgroups and a fixed effect model across subgroups [37].
Results
Study characteristics
Nine journal articles and one conference abstract, published over a 20-year period (1997–2017), were included in this review (see Table 1). This included nine cross-sectional and one longitudinal study. Studies originated from Europe (Nstudies = 3) and Asia (Nstudies = 2), with single studies from Canada, Australia, the United Kingdom and United States. Alonso et al.’s [6] multi-national study involved eight participating countries. An additional four studies accessed general population-based surveys, contributing to 90% of the total sample [25,26,27, 29].
Sample characteristics
The coronary group represented a mixture of 4786 persons with myocardial infarction (41%) or angina pectoris (47%; see Table 2). Both chronic and acute forms were represented. Time since diagnosis was not routinely specified (Nstudies = 3). Consistent with global data [42], the CHD group was older [t(14) = 2.47, p = 0.026] and comprised a higher proportion of males [χ2(1) = 51.06, p < 0.0001]. Self-reported prevalence of CHD comorbidities and risk factors, as reported by seven studies, included hypertension (55%), arthritis (54%), hyperlipidemia (45%), obesity (43%), diabetes (31%), chronic pain (26%), respiratory disease (21%), alcohol dependence (28%), current smoking (26%), depressed mood or anxiety (12%). In four studies, participants were also prescribed anti-thrombotic, anti-hypersensitive medication and/or beta blockers.
Study reporting quality
The average quality assessment score was 21.1 (SD = 1.1, range 19–22)—excluding the single conference abstract [26], which lacked detail on study content to allow a full evaluation of reporting quality (QualSyst score = 12). Studies provided a clear description of their objectives, experimental design and comparison (non-CHD) group (Criterion 1–3: 91% fulfilled). Key sample characteristics (e.g. age, gender) that can help to confirm the generalisability of findings were described (Criterion 4: 73% fulfilled). Most studies also clearly defined and justified their HRQoL measures (Criterion 5: 91% fulfilled) and had a sufficiently powered sample size (Criterion 6: 82% fulfilled). Statistical analyses were specified (e.g. adjusting for age; Criterion 7: 91% fulfilled), although estimates of variance (e.g. standard deviations, confidence intervals) were not routinely reported (Criterion 8: 64% fulfilled). Sample confounds were controlled by recruiting demographically matched controls or via covariate adjustments (Criterion 9: 91% fulfilled). Finally, significant and non-significant results were sufficiently explained (Criterion 10: 82% fulfilled), and conclusions supported (Criterion 11: 100% fulfilled). In sum, internal validity of studies was generally high with the majority attempting to minimise potential sources of methodological biases.
Group differences in composite HRQoL
Seven studies examined HRQoL in samples with chronic CHD using composite scores (e.g. SF-36) or single items (e.g. EQ-VAS), with Garster et al. [25] comparing six generic indexes (Table 3). Persons with CHD consistently reported lower HRQoL in comparison to healthy peers (p ≤ 0.001). However, individual effect estimates varied in magnitude—even among studies employing the same instrument. Alonso et al.’s [6] multi-national study produced the most conservative estimate for the SF-36 physical summary score (g = − 0.368, CI − 0.431, − 0.304). Notably, this trial made adjustments for multiple covariates (age, gender, marital status, education and mode of SF-36 administration). Garster et al. [25] and Lee et al. [26] both reported greater problem frequencies among their CHD group across EQ-5D dimensions (mobility, self-care, usual activities, pain/discomfort, anxiety/depression); however, country heterogeneity was evident. Garster et al. [25] weighted their index score to the US population (g = − 0.400, CI − 0.525, − 0.275), whereas Lee et al. [26] achieved a large group difference utilising the Korean preference weight (g = − 0.657, CI − 0.732, − 0.582). Tavella et al.’s [27] conference abstract was identified as an outlier for the SF-36 mental component (g = − 0.489, CI − 0.567, − 0.41)—removing this study from the analysis moderately reduced the heterogeneity (gw = − 0.139, CI − 0.242, − 0.036, p ≤ 0.001; I2 = 60.76%; Nstudies = 3).
There were no significant differences in effect estimates (QB (1) = 0.519, p = 0.471) between studies which controlled for socio-demographic factors among their samples (gw = − 0.347, CI − 0.542, − 0.153, p = 0.001; Nstudies = 4) and those which did not (gw = − 0.455, CI − 0.673, − 0.236, p ≤ 0.001; Nstudies = 3). This analysis may, however, be underpowered.
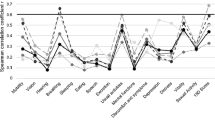
Group differences in HRQoL domains
Five cross-sectional studies, involving newly diagnosed patients (Nstudies = 2) and those with long-standing CHD (Nstudies = 3), provided data for three multi-dimensional HRQoL measures (15-D, SF-36, WHOQOL; Table 4). Subscales typically mapped onto the ICF bodily functions and sensations domain, followed by activity and participation levels (Nstudies = 4) and the personal impact of CHD (Nstudies = 3). A single study explored group perceptions of the living environment [5].
Bodily function-oriented measures
The largest group difference was associated with memory functions: those with CHD reported more cognitive problems. To a lesser extent, this group also experienced greater physical symptoms, namely lowered energy/fatigue, hearing loss, incontinence, chronic pain and mental health. However, pain experiences following CHD varied. Seo et al. [4] identified significantly (p < 0.001) low scores on the SF-36 bodily pain subscale among gender- and age-matched patients with acute coronary syndrome (g= − 0.644, CI − 0.976, − 0.312), as is typical of a person who has very severe and extremely limiting pain. In comparison, Lalonde et al. [7] reported comparable ratings between their chronic CHD sample and asymptomatic healthy participants (g = − 0.081, CI − 0.238, 0.075, p = 0.308). Notably, this latter result did not change substantially, even after controlling for the number of self-reported comorbid conditions [7]. These findings may, however, be characterised by publication bias.
Activity- and participation-oriented measures
The largest mean difference was associated with recreation and leisure: newly diagnosed patients reported more problems in their social relationships (WHOQOL). Those with longer-term CHD also reported difficulty adapting to the social changes caused by their illness (SF-36 social functioning), although the associated group difference was small in magnitude. Similarly, a decrease in physical activity after disease onset (moving around) and problems with the ability to physically carry out daily routines, such as self-care, were consistently reported by those with CHD. These ICF categories were, however, associated with a high degree of inconsistency in effect estimates.
Environment-focused measures
Only Srivastava et al. [5] explored group differences in the living environment. This included the general environment (e.g. noise, air pollution), financial stability, recreation, transportation, and availability and accessibility of health and social services. Those with CHD perceived their HRQoL as being commensurate with peers.
Personal factors measures
Three studies investigated the personal impact of CHD on current and future health expectations, categorised as a personal factor in the ICF: individuals with CHD reported poorer functioning (SF-36 general functioning subscale). Again there was variation in effect estimates. Alonso et al. [6] reported a small to medium and significant group difference (g = − 0.423, CI − 0.487, − 0.360, p < 0.001), additionally noting that the impact of CHD was similar across the eight countries studied. Zaninotto et al. [29] provided gender-specific data, reporting no group differences on the Control, Autonomy, Self-realisation, Pleasure scale (CASP 19) (g = 0.085, CI − 0.047, 0.218, p = 0.208) after adjustments were made for covariates. Interestingly, this same study [29] reported a progressive decline in HRQoL among males with CHD at 2- and 4-year follow-up, whereas men and women in the control group had similar changes in HRQoL over time [29]. Conversely, Lee et al [26] and Unsar et al [28] identified female gender, along with older age, as independently and adversely affecting HRQoL for those with CHD, even after adjusting for comorbidities [26].
Discussion
Using the ICF as a scheme for the classification of CHD-related HRQoL, this review synthesised data from 10 independent studies, most of good quality. Pooled effect estimates were primarily in a negative direction: those with CHD reported worsening cognitive, somatic and psychological symptoms which set them apart from controls of their own age. Generic HRQoL indices (e.g. SF-36, ED-5D) captured these differences; however, multi-dimensional HRQoL measures allowed for more precise assessment, as demonstrated by the larger effect sizes associated with some subscale scores.
It is not unexpected that symptoms such as fatigue, pain and lowered mood, as direct or indirect consequences of CHD [43, 44], differentiated CHD patients from peers. However, HRQoL following CHD remains primarily operationalised at the level of body function and structure and resulting impairment on activities and participation. This includes a reliance on index scores which focus overly on physical and mental health (e.g. SF-36). The role of personal (socio-demographic) predictors of HRQoL also remains unclear, with population-based data revealing mixed findings [26, 29].
It follows that other characteristics, aside from gender, may lead to HRQoL differences for those with CHD. This includes the potential role of race and ethnicity—an area which remains understudied. Minority groups have been shown to experience higher traditional CHD risk factors, independently of socioeconomic factors [45]. Trajectories of recovery also need to be considered in the assessment process [46]. For example, physical symptoms often improve in a steady, linear direction following cardiac surgery, whereas emotional difficulties (e.g. depression, anxiety) show early improvements that gradually dissipate—with individuals having difficulty returning to their normal roles and social functioning [47]. This suggests a need to utilise validated generic and more nuanced, CHD-specific measures in combination to obtain an initial understanding of patients’ health-related concerns [48, 49]. The value of such multilevel assessments, which allow for person-centric assessment, is being increasingly realised [8].
Age-related decline in HRQoL is another consideration. Interestingly, the pooled effect size associated with generic HRQoL indices in our review was lower (gw = − 0.396, CI − 0.524, − 0.269) albeit statistically comparable (i.e. overlapping CIs) to a recent meta-analysis of the paediatric CHD literature (gw = − 1.31, CI −6.51 to 3.89 [50]). In this latter review, however, paediatric patients reported comparable or better social functioning than controls [50]. The large group differences we noted for the social HRQoL domain may reflect age-related health comorbidities (e.g. diabetes, hypertension), which disproportionally affect elderly CHD patients and can significantly limit daily activity and performance [44]. Future CHD research should report age at diagnosis in addition to prevalence and severity of comorbidities across age categories, to better inform interventional research. Indeed, the high frequency of multiple, medical comorbidities reported by studies in this review suggests that there should be a greater focus on their contribution to disease burden and HRQoL in CHD [1, 2].
It is also important to consider characteristics of the individual’s environment. Preliminary research has certainly identified access barriers to health service use (e.g. accessibility, affordability, acceptability) which can impede HRQoL in CHD [51]. Additionally, the importance of social networks and connections—which are often fostered in the workplace—may also give rise to ‘quality of life’ opportunities for those with CHD [47]. Future CHD research might therefore consider the moderating role of living alone and employment, both indices of social support, on HRQoL.
Use of the ICF to better understand HRQoL issues for those with CHD, including “what” HRQoL components to measure or assess and “how” to select the most informative HRQoL measures, is, however, not without its problems. In particular, categorisation of global HRQoL components (e.g. WHOQOL-BREF physical, psychological, social and environmental subscales), which represent a combination of body functioning, activity and participation components, is difficult to compartmentalise within ICF domains and subdomains. The interconnectedness among ICF components was also problematic. In particular, we had difficulties distinguishing between ‘activities’ and ‘participation’ in our mapping process. Finally, subjective HRQoL items and subscales relating to general health perceptions, attitudes and beliefs that fit into the personal component also remain uncategorised in the ICF. Further work is needed to map the domain and facet structure of available HRQoL measures to the ICF.
Clinical implications
The current findings highlight the importance of comprehensive biopsychosocial assessment and monitoring soon after diagnosis of CHD. HRQoL, as a universal construct, covers multiple dimensions of functioning. As such, singular assessments focused on just physical, psychological or social elements are too narrowly defined to represent individual functioning for those with a chronic condition such as CHD. Measures of HRQoL should also be selected to provide information on the domains in which CHD is associated with health status disparities in comparison to the general population. This assessment should go beyond physical impairment, incorporating an individual’s lived experience of health, such as their ability to self-manage cardiac symptoms and sequelae (both physical and mental) in addition to their social re-engagement (i.e. community participation, independent living).
To date, the monitoring and evaluation of HRQoL posits conceptual and practical challenges with use of disparate indicators that are not framed on a common interpretive framework. The ICF provides this common framework and language, allowing for multi-disciplinary treatment teams to communicate transparently about the functioning and health of people with CHD in their treatment and care [52]. Linking HRQoL measures to ICF domains can also help to identify aspects of health and functioning which are not being considered in an individual’s rehabilitation [52]. This might include intimate relationships, individual attitudes and coping styles—considered to be critical ICF categories across chronic illness groups [53, 54]. Depending on the specific users’ need, up to four levels of ICF categories can be included in an individual assessment. This allows functioning to be described at a broad level (i.e. by ICF domain) but also at a more granular, detailed level (e.g. mild, moderate, severe CHD). Specifications are additionally provided which take into account cultural variation and differences across the life span [55].
Study limitations
The present findings need to be considered in the context of methodological limitations that arose during data selection and analysis. First, concerns regarding publication bias were addressed using a common fail-safe N method. While more informative tests (e.g. funnel plot asymmetry, Begg’s test) are available, these analyses are not recommended when few studies are being pooled [56, 57]. For these reasons, we adopted a conservative method for calculating Nfs (i.e. Nfs had to exceed the number of published studies in a particular analysis; [36]), in addition to calculating p values and CIs. These stringent criteria ensured that we minimised the number of false-positive effects. Similarly, subgroup analysis of potential medical moderators (e.g. newly diagnosed vs longer-term CHD, CHD type) and additional methodological characteristics (e.g. use of single vs. multi-item HRQoL scores) was not possible due to the small number of studies included in this review [58]. The limited data in our meta-analysis may have also contributed to a bias in estimation of heterogeneity [59]. Finally, the reliance on cross-sectional data prevented exploration of changes in HRQoL and the importance of ICF components across the lifetime trajectory of CHD. Longitudinal research is needed to investigate temporal patterns in HRQoL for those living with CHD.
Conclusions
Informed by the ICF, this review collates existing data comparing HRQoL ratings in the CHD population with control groups. The pooled findings confirm that the repercussions of CHD uniquely impact physical, mental and social functioning. The capacity to monitor both global and domain-specific HRQoL indicators with ICF mapping allows for comprehensive assessment and monitoring of evolving health care needs over time.
Change history
06 June 2018
In the original publication of the article, the surname of one of the co-authors was misspelled as ‘Mpfou’. This has been updated in this correction.
References
*References with an asterisk demote studies included in current review
Moran, A. E., Forouzanfar, M. H., Roth, G. A., Mensah, G. A., Ezzati, M., Murray, C. J. L., et al. (2014). Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: The Global Burden of Disease 2010 study. Circulation, 129(14), 1483–1492.
Pandya, A., Gaziano, T. A., Weinstein, M. C., & Cutler, D. (2013). More Americans living longer with cardiovascular disease will increase costs while lowering quality of life. Health Affairs (Project Hope), 32(10), 1706–1714.
Karimi, M., & Brazier, J. (2016). Health, health-related quality of life, and quality of life: What is the difference? Pharmacoeconomics, 34(7), 645–649.
*Seo, J., Lee, Y., Kang, S., Chun, H., Pyun, W. M., Park, S. H., et al. (2015). Poor health-related quality of life and proactive primary control strategy may act as risk factors for acute coronary syndrome. Korean Circulation Journal, 45(2), 117–124.
*Srivastava, S., Shekhar, S., Bhatia, M. S., Manjeet, S., & Dwivedi, S. (2017). Quality of life in patients with coronary artery disease and panic disorder: A comparative study. Oman Medical Journal, 32(1), 20–26.
*Alonso, J., Ferrer, M., Gandek, B., Ware, J., Aaronson, N., Mosconi, P., et al. (2004). Health-related quality of life associated with chronic conditions in eight countries: Results from the International Quality of Life Assessment (IQOLA) Project. Quality of Life Research, 13, 283–298.
*Lalonde, L., Clarke, A. E., Joseph, L., Mackenzie, T., & Grover, S. A. (2001). Health-related quality of life with coronary heart disease prevention and treatment. Journal of Clinical Epidemiology, 54(10), 1011–1018.
Payakachat, N., Ali, M. M., & Tilford, J. M. (2015). Can the EQ-5D detect meaningful change? A systematic review. PharmacoEconomics, 33(11), 1137–1154.
Busija, L., Pausenberger, E., Haines, T. P., Haymes, S., Buchbinder, R., & Osborne, R. H. (2011). Adult measures of general health and health-related quality of life: Medical Outcomes Study Short Form 36-Item (SF-36) and Short Form 12-Item (SF-12) Health Surveys, Nottingham Health Profile (NHP), Sickness Impact Profile (SIP), Medical Outcomes Study Short Form 6D (SF-6D), Health Utilities Index Mark 3 (HUI3), Quality of Well-Being Scale (QWB), and Assessment of Quality of Life (AQOL). Arthritis Care & Research, 63(S11), S383-S412.
Hand, C. (2016). Measuring health-related quality of life in adults with chronic conditions in primary care settings: Critical review of concepts and 3 tools. Canadian Family Physician, 62(7), e375-e383.
Stevanović, J., Pechlivanoglou, P., Kampinga, M. A., Krabbe, P. F. M., & Postma, M. J. (2016). Multivariate meta-analysis of preference-based quality of life values in coronary heart disease. PLoS ONE, 11(3), e0152030.
World Health Organization. (2001). International classification of functioning, disability and health. Geneva: World Health Organization.
Madden, R., Glozier, N., Fortune, N., Dyson, M., Gilroy, J., Bundy, A., Llewellyn, G., Salvador-Carulla, L., Lukersmith, S., Mpofu, E., & Madden, R. (2015). In search of an integrative measure of functioning. International Journal Environmental Research and Public Health, 12, 5815–5832.
Peterson, D. B., Mpofu, E., & Oakland, T. (2010). Concepts and models in disability, functioning and health. In E. Mpofu & T. Oakland (Eds.), Rehabilitation and health assessment: Applying ICF guidelines (pp. 3–26). New York: Springer.
Cieza, A., Stucki, A., Geyh, S., Berteanu, M., Quittan, M., Simon, A., et al. (2004). ICF Core Sets for chronic ischaemic heart disease. Journal of Rehabilitation Medicine, 36, 94–99.
Moher, D., Liberati, A., Tetzlaff, J., & Altman, D. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151(4), 264–269.
Foxwell, R., Morley, C., & Frizelle, D. (2013). Illness perceptions, mood and quality of life: A systematic review of coronary heart disease patients. Journal of Psychosomatic Research, 75(3), 211–222.
Dickens, C., Cherrington, A., & McGowan, L. (2012). Depression and health-related quality of life in people with coronary heart disease: A systematic review. European Journal of Cardiovascular Nursing, 11(3), 265–275.
Calton, R., Satija, T., Dhanoa, J., Jaison, T. M., & David, T. (1998). Correlation of Braunwald’s clinical classification of unstable angina pectoris with angiographic extent of disease, lesion morphology and intra-luminal thrombus. Indian Heart Journal, 50(3), 300–306.
Thompson, D. R., & Yu, C. M. (2003) Quality of life in patients with coronary heart disease-I: Assessment tools. Health and Quality of Life Outcomes, 1(1), 42.
Jüni, P., Holenstein, F., Sterne, J., Bartlett, C., & Egger, M. (2002). Direction and impact of language bias in meta-analyses of controlled trials: Empirical study. International Journal of Epidemiology, 31(1), 115–123.
Garratt, A. M., & Stavem, K. (2017). Measurement properties and normative data for the Norwegian SF-36: Results from a general population survey. Health and Quality of Life Outcomes, 15, 51.
Kendall, P. C., Marrs-Garcia, A., Nath, S. R., & Sheldrick, R. C. (1999). Normative comparisons for the evaluation of clinical significance. Journal of Consulting and Clinical Psychology, 67(3), 285–299.
*Claesson, M., Burell, G., Birgander, L. S., Lindahl, B., & Asplund, K. (2003). Psychosocial distress and impaired quality of life—Targets neglected in the secondary prevention in women with ischaemic heart disease. European Journal of Cardiovascular Prevention and Rehabilitation, 10, 258–266.
*Garster, N. C., Palta, M., Sweitzer, N. K., Kaplan, R. M., & Fryback, D. G. (2009). Measuring health-related quality of life in population-based studies of coronary heart disease: Comparing six generic indexes and a disease-specific proxy score. Quality of Life Research, 8, 1239–1247.
*Lee, H. T., Shin, J., Lim, Y. H., Kim, K. S., Kim, S. G., Kim, J. H., et al. (2015). Health-related quality of life in coronary heart disease in Korea: The Korea National Health and Nutrition Examination Survey 2007 to 2011. Angiology, 66(4), 326–332.
*Tavella, R., Cutri, N., Adams, R., & Beltrame, J. (2010). Health status of stable patients with obstructive or non-obstructive coronary artery disease compared with healthy controls. Heart, Lung and Circulation, 6, 728.
*Unsar, S., Sut, N., & Durna, Z. (2007). Health-related quality of life in patients with coronary artery disease. Journal of Cardiovascular Nursing, 22(6), 501–507.
*Zaninotto, P., Sacker, A., Breeze, E., McMunn, A., & Steptoe, A. (2016). Gender-specific changes in well-being in older people with coronary heart disease: Evidence from the English Longitudinal Study of Ageing. Aging & Mental Health, 20(4), 432–440.
Higgins, J. P. T., & Green, S. (2011). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. http://handbook.cochrane.org. Accessed 22 Jan 2018.
Cieza, A., & Stucki, G. (2005). Content comparison of health-related quality of life (HRQOL) instruments based on the international classification of functioning, disability and health (ICF). Quality of Life Research, 14(5), 1225–1237.
Grotkamp, S. L., Cibis, W. M., Nüchtern, E. A. M., von Mittelstaedt, G., & Seger, W. K. F. (2012). Personal factors in the International classification of functioning, disability and health: Prospective evidence. The Australian Journal of Rehabilitation Counselling, 18(1), 1–24.
Cieza, A., Geyh, S., Chatterji, S., Kostanjsek, N., Ustu¨n, B., & Stucki, G. (2005). ICF linking rules: An update based on lessons learned. Journal of Rehabilitation Medicine, 37, 212–218.
Kmet, L. M., Lee, R. C., & Cook, L. S. (2004) Standard quality assessment criteria for evaluating primary research papers from a variety of fields. Alberta Heritage Foundation for Medical Research Edmonton. Report No.: 1-896956-77-7.
Ellis, P. D. (2010). The essential guide to effect sizes. New York: Cambridge University Press.
Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155.
Borenstein, M., Hedges, L. V., Higgins, J. P. T., & Rothstein, H. R. (2009). Introduction to meta-analysis. Londres: Wiley.
Lipsey, M. W., & Wilson, D. B. (2001). Practical meta-analysis. Thousand Oaks, CA: Sage.
Higgins, J. P. T., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ: British Medical Journal, 327(7414), 557–560.
Huedo-Medina, T. B., Sánchez-Meca, J., Marín-Martínez, F., & Botella, J. (2006). Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychological Methods, 11(2), 193.
Borenstein, M., Hedges, L. V., Higgins, J. P., & Rothstein, H. R. (2010). A basic introduction to fixed-effect and random-effects models for meta-analysis. Research Synthesis Methods, 1(2), 97–111.
Benjamin, E. J., Blaha, M. J., Chiuve, S. E., Cushman, M., Das, S. R., Deo, R., et al. (2017). Heart disease and stroke statistics-2017 update: A report from the American Heart Association. Circulation, 135(10), e146-e603.
Khayyam-Nekouei, Z., Neshatdoost, H., Yousefy, A., Sadeghi, M., & Manshaee, G. (2013). Psychological factors and coronary heart disease. ARYA Atherosclerosis, 9(1), 102–111.
Tusek-Bunc, K., & Petek, D. (2016). Comorbidities and characteristics of coronary heart disease patients: Their impact on health-related quality of life. Health and Quality of Life Outcomes, 14, 1.
Leigh, J. A., Alvarez, M., & Rodriguez, C. J. (2016). Ethnic minorities and coronary heart disease: An update and future directions. Current Atherosclerosis Reports, 18(2), 9.
Tully, P. J. (2013). Quality-of-Life measures for cardiac surgery practice and research: A review and primer. The Journal of Extra-Corporeal Technology, 45(1), 8–15.
Le Grande, M. R., Elliott, P. C., Murphy, B. M., Worcester, M. U. C., Higgins, R. O., Ernest, C. S., et al. (2006). Health related quality of life trajectories and predictors following coronary artery bypass surgery. Health and Quality of Life Outcomes, 4, 49.
Gierlaszyńska, K., Pudlo, R., Jaworska, I., Byrczek-Godula, K., & Gąsior, M. (2016). Tools for assessing quality of life in cardiology and cardiac surgery. Kardiochirurgia i Torakochirurgia Polska = Polish Journal of Cardio-Thoracic Surgery, 13(1), 78–82.
Thompson, D. R., Ski, C. F., Garside, J., & Astin, F. (2016). A review of health-related quality of life patient-reported outcome measures in cardiovascular nursing. European Journal of Cardiovascular Nursing, 15(2), 114–125.
Schrøder, M., Boisen, K. A., Reimers, J., Teilmann, G., & Brok, J. (2016). Quality of life in adolescents and young adults with CHD is not reduced: A systematic review and meta-analysis. Cardiology in the Young, 26, 415–425.
Asadi-Lari, M., Packham, C., & Gray, D. (2003). Unmet health needs in patients with coronary heart disease: Implications and potential for improvement in caring services. Health and Quality of Life Outcomes, 1, 26–26.
Hwang, K., & Mpofu, E. (2010). Health care quality assessments. In E. Mpofu & T. Oakland (Eds.), Rehabilitation and health assessment: Applying ICF guidelines (141–161). New York: Springer.
World Health Organisation (2003). The ICF checklist. Geneva: WHO. http://www.who.int/classifications/icf/training/icfchecklist.pdf. Accessed 24 Apr 2018.
Weigl, M., Cieza, A., Andersen, C., Kollerits, B., Amann, E., & Stucki, G. (2004). Identification of relevant ICF categories in patients with chronic health conditions: A Delphi exercise. Journal of Rehabilitation Medicine, 44, 12–21.
World Health Organisation. (2013). How to use the ICF: A practical manual for using the International Classification of Functioning, Disability and Health (ICF). Exposure draft for comment. October 2013. Geneva: WHO.
Sterne, J. A., Sutton, A. J., Ioannidis, J. P. A., Terrin, N., Jones, D. R., Lau, J., Carpenter, J., Rücker, G., Harbord, R. M., Schmid, C. H., Tetzlaff, J., Deeks, J. J., Peters, J., Macaskill, P., Schwarzer, G., Duval, D., Altman, D. G., Moher, D., & Higgins, J. P. T. (2011). Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ British Medical Journal, 343, d4002.
Begg, C. B., & Mazumdar, M. (1994). Operating characteristics of a rank correlation test for publication bias. Biometrics, 50, 1088–1101.
Sedgwick, P. (2013) Meta-analyses: Heterogeneity and subgroup analysis. BMJ: British Medical Journal, 346, f4040.
von Hippel, P. T. (2015). The heterogeneity statistic I2 can be biased in small meta-analyses. BMC Medical Research Methodology, 15, 1–8.
Acknowledgements
The authors would like to thank Maureen Bell, Research Librarian at the University of Adelaide, for assistance with the electronic database searches.
Funding
The research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Le, J., Dorstyn, D.S., Mpfou, E. et al. Health-related quality of life in coronary heart disease: a systematic review and meta-analysis mapped against the International Classification of Functioning, Disability and Health. Qual Life Res 27, 2491–2503 (2018). https://doi.org/10.1007/s11136-018-1885-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-018-1885-5