Abstract
Purpose
The primary purpose was to test the effectiveness of two telephone-delivered psychosocial interventions for maintaining and improving quality of life (QOL) (psychological, physical, social, and spiritual well-being) among 71 prostate cancer survivors and the 70 intimate or family partners who were supporting them in their recovery.
Methods
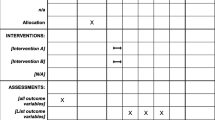
This study used a three-wave repeated measures experimental design. Both the interpersonal counseling intervention (TIP-C) and health education attention condition (HEAC) were delivered using the telephone.
Results
Improvements in depression, negative affect, stress, fatigue, and spiritual well-being were significantly higher for survivors in the HEAC than for those in the TIP-C condition. Partners in the HEAC condition showed significantly greater improvements in depression, fatigue, social support from family members, social well-being, and spiritual well-being compared to partners in the TIP-C condition. The results revealed superior outcomes for those assigned to the HEAC intervention.
Conclusions
The psychosocial interventions in this study were effective in maintaining or improving the QOL for prostate cancer survivors and their partners. Both the survivor and their intimate partner or family member benefitted from the interventions. Future research is needed to determine the optimal timing and client characteristics for each intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In 2010, 217,730 men will be diagnosed with prostate cancer [1]. With early diagnosis, prostate cancer is highly treatable, reflected in 5-year survival rates of almost 99%. As the death rate from cancer declines, the number of people living with prostate cancer continues to increase. The significant numbers of prostate cancer survivors and their families emphasize the need for increased attention to survivorship and quality of life (QOL) (psychological, physical, social, and spiritual well-being) [2, 3]. The purpose of this study was to test the efficacy of two psychosocial interventions to improve the QOL for men with prostate cancer and their intimate partners or family social network members (all called “partners” in this study).
Psychological distress in men with prostate cancer can negatively influence QOL during cancer treatment. The incidence of clinically significant levels of depression and anxiety in prostate cancer survivors has been reported as 16 and 12%, respectively [4], which is higher than population norms for older males. For prostate cancer patients on Androgen Deprivation Therapy, the risk of major depressive disorder is 8 times the national rate for men and 32 times the rate for those over age 65 [5]. Depression is associated with decreased compliance with adjuvant therapy and a number of cognitive and functional impairments [6, 7]. Rates of anxiety with associated feelings of nervousness and worrying about prostate cancer have also been reported between 25 and 50%, which is higher than population norms [8, 9]. High levels of perceived stress have been associated with higher rates of depression and anxiety, tumor progression [10] and lower QOL in adults with cancer [11].
Intimate partners, family members, and close friends also report high levels of psychological distress, often higher than levels reported by survivors [12, 13]. Approximately 32 to 50% of caregivers have significant psychological distress or mood disturbance [14]. Braun et al. [12] found that about 40% of cancer patients’ spouses scored above the cutoff for clinically significant levels of depression on the Beck Depression Inventory-II. When patients meet the criteria for psychiatric disorder, caregivers are 7.9 times more likely to meet the criteria as well, and vice versa [15].
Fatigue, a common physical symptom of prostate cancer, is experienced by the majority of cancer survivors and generally worsens over the treatment course [16]. Butt et al. [17] reported that fatigue was the top-rated symptom when cancer patients were asked what their “most important symptom or concern” was to monitor. Fatigue ranked as most important for 10 of the 11 diagnoses and had strong associations with reduced QOL.
Prostate cancer can also result in significant erectile, urinary, and bowel dysfunction [18]. Depending upon the particular treatment, the incidence of erectile dysfunction ranges from 59 to 91%, hot flashes range from 50 to 75%, and loss of libido from 59 to 65% [18–20]. These side effects have deleterious consequences for the QOL of cancer survivors and their intimate partners [21–23].
Social support, an indicator of social well-being, has received extensive attention in the context of QOL for cancer patients [24] and plays a critical role in physical and psychological well-being [25–27]. Krongrad et al. [28] studied the survival of 146,979 men with prostate cancer and found that those who were married, suggesting higher social integration and availability of support, had a significantly longer mean survival. Social support may help to alleviate psychological distress in cancer patients though its beneficial effects on cognitive processing [29].
A final QOL dimension that has received little attention is the spiritual well-being of prostate cancer survivors [30], although spiritual well-being is considered an important predictor of, and resource for, QOL in cancer patients [2, 31]. Gall [32] found that relationship to God was a significant predictor of role, social, and emotional functioning after controlling for age and illness severity among men with prostate cancer.
Although psychosocial interventions are rarely offered to prostate cancer survivors, there is promising evidence of their effectiveness for helping to maintain QOL [33–35]. The provision of interventions for spouses and family members is even less common, although there is evidence that such interventions can have beneficial effects [21, 23, 27, 36, 37]. Our interventions are provided to both members (cancer survivor and social network member partner) of the dyad. The fundamental assumptions from social support or interpersonal theories enacted through our interventions are that (1) cancer diagnosis and treatment affects the survivors’ entire social network, not just the cancer survivor, (2) close social network members exert a mutual influence on each others’ QOL, and (3) emotions are highly interdependent. Although we include a social network member partner, we do not specify what type of network member may participate.
Two prominent areas of need for prostate cancer survivors and their partners are (1) maintenance of psychosocial well-being, such as minimizing psychological distress and improving interpersonal functioning [38], and (2) meeting informational needs for increased understanding of the illness and its effects [39, 40]. Interventions that target the psychological distress and provide information to increase knowledge about cancer can help the survivor to decrease the uncertainty and related psychological distress during the cancer experience [41]. Given the two areas of identified need for prostate cancer and their partners, we developed two psychosocial interventions designed to target these processes and tested their effectiveness for improving QOL outcomes in prostate cancer survivors and their partners.
Methods
This study used a repeated measures experimental design to test two different telephone-delivered interventions for improving quality of life (QOL). The 8-week telephone interpersonal counseling (TIP-C) intervention was developed from standard interpersonal psychotherapy (IPT) [42–46], combined with cancer education. It was modified to be delivered over the telephone to reduce barriers to accessing the intervention. Like IPT, the initial session identified interpersonal problem areas, established a treatment contract, and defined symptoms within an interpersonal context. The intervention addressed (1) mood and affect management, (2) emotional expression, (3) interpersonal communication and relationships, (4) social support, and (5) cancer information. The TIP-C intervention targets the social support behaviors of both cancer survivors and their partners using interpersonal communications techniques. Interpersonal communication facilitates processing stressful affective reactions to cancer diagnosis and treatment, marshalling instrumental support for assistance with roles and functions, informational support for advice and information, and appraisal support for gauging and adjusting to the stressor. A master’s prepared nurse or social worker with psychiatric and oncology expertise delivered the intervention. After the baseline assessment (average of 56 min), sessions averaged 31 min (SD = 7.0) for both survivors and partners. During this same period, the partners received a session every other week (4 sessions) to discuss the partner’s own physical and emotional well-being. The counseling intervention was tailored to the participant’s/dyad’s specific needs and interests while still adhering to a structured protocol.
The second intervention was an 8-week health education attention condition (HEAC), also delivered over the telephone. Participants received written materials from the National Cancer Institute about prostate cancer diagnosis and treatments [47], and health-related topics such as nutrition during cancer [48, 49], exercise to decrease fatigue [50], resources for cancer survivors [51, 52], and quitting smoking [53]. Survivors received weekly telephone calls to review these materials. After the baseline assessment (average of 59 min), sessions averaged 28 min (SD = 6.2) for both survivors and partners. The HEAC was delivered by research assistants (RA); only one was a health profession student and the rest were from non-health disciplines. The RA received training in how to review the written materials. No counseling was offered in the HEAC. During this same period, the partners received telephone calls every other week for a total of 4 sessions.
Both interventions had manuals and were delivered by counselors/research assistants trained in the intervention for which they were responsible. Interventions were recorded, and the investigators reviewed the recordings of each intervention, giving feedback to the interveners to maintain intervention fidelity and prevent intervention drift. Interventionists had to maintain > 90% on protocol implementation at all times.
Sample
A convenience sample of 71 men with prostate cancer and 70 social network members participated in this study. Eligibility criteria included a diagnosis of prostate cancer, currently undergoing or had completed treatment within the past 6 months, ability to speak English, no physical or psychological disabilities that would prevent participating in the interventions, and availability of a social network member who was willing to participate in the investigation. The partner could be anyone within the survivor’s social network whom he felt was significant to his recovery. Although most men selected spouses, men were not restricted to spouses given some were also widowed, divorced, single or had spouses unable to participate (e.g., spouse too ill).
Cancer survivors and their partners were recruited from regional cancer centers and Veteran’s Administration centers, cancer support groups, and from oncologists’ offices through announcements by staff and distribution of study brochures. A smaller portion was recruited from research study websites through which interested individuals could volunteer to enroll.
Thirty-six men and their partners were randomly assigned to the TIP-C intervention and 35 men and their partners to the HEAC. Descriptive information about the demographic characteristics of the men and their partners appears in Table 1. At baseline, there were no significant differences for demographic characteristics between groups. Table 2 lists the illness characteristics of the prostate survivors. Treatment included prostatectomy (almost 30%), radiation (56%), and hormone therapy (42%). Table 3 lists the survivors’ and partners’ chronic illnesses and medications. All of the men listed at least one other chronic illness, with an average of 1.82 (SD = 1.5) illnesses and 4.64 (SD = 3.7) medications. Partners averaged 2.35 (SD = 2.5) chronic illnesses with 2.29 (SD = 2.3) medications.
Procedure
Upon recruitment and after informed consent, the project director used a table of random numbers to assign men and their partners to one of two interventions. All participants completed baseline assessments over the telephone that included the instruments described here plus others not relevant to the present report. Separate calls were made to the survivor and partner for all interventions and assessments at times that were convenient for the individual. For those participants who lived together, the importance of privacy was stressed and participants were recommended to schedule calls at times when their partner would be away or in a separate part of the home. Following baseline assessment, all men received 8 weekly phone calls and their partners received 4 calls, one every other week, as part of the interventions. Adherence was determined as the number of sessions each participant completed. Adherence by the survivors was high in both TIP-C (86%) and HEAC (89%). Adherence rates for partners were 85% for the TIP-C and 93% for the HEAC.
Participants completed the second (T2) assessment (T1 + 8 weeks) within the week of their final intervention session, and the 3rd and final assessment (T3) 8 weeks later (T2 + 8 weeks). After each assessment, participants were sent a $10 gift card from a local retail merchant to thank them for their time.
At T1, 71 prostate cancer survivors and their partners were enrolled (Fig. 1) and by T2, 5 survivors and their partners withdrew from the study (T1–T2 attrition rate = 7%). By T3, an additional 2 dyads were lost to follow-up because they declined to complete the T3 assessment (T1–T3 attrition = 10%). There were no significant differences for demographic or illness characteristics between those that discontinued and those that completed the study.
Measures
Psychological Well-being was examined using measures of depression, positive and negative affect, and perceived stress. Symptoms of depression were measured using the 20-item Center for Epidemiological Studies-Depression Scale (CES-D) [54]. Scores range from 0 to 60. The CES-D has strong evidence of satisfactory reliability and validity [55]. Cronbach’s alpha values over T1–T3 were ≥0.88 for participants in this study. Positive and negative affect was assessed with the 20-item Positive and Negative Affect Schedule (PANAS) [56]. Scores range from 10 to 50 on each scale. The PANAS has been used extensively with satisfactory reliability and demonstrated convergent and construct validity [57, 58]. Cronbach’s alpha values were >0.87 for positive affect and ≥0.86 for negative affect. Participants’ current subjective appraisals of stress were assessed with the 10-item Perceived Stress Scale (PSS) [59]. The PSS has a scale range of 0–40. The PSS has demonstrated satisfactory reliability and validity in numerous studies [60] with a Cronbach’s alpha in this study ≥0.88.
Physical Well-being was assessed using two scales: fatigue and the urinary, bowel, and sexual functioning subscales from the UCLA Prostate Cancer Index [19, 20]. Fatigue was measured using the 20-item Multidimensional Fatigue Inventory (MFI), which has demonstrated satisfactory reliability and validity in cancer populations [61]. In this analysis, we combined the subscales of the MFI to form a global measure of fatigue with Cronbach’s alpha values ≥0.89. Participants completed the Index to assess their prostate specifichealth-related quality of life. This Index has sound psychometric qualities, demonstrating good internal consistency, test–retest reliability, and validity [62]. Cronbach’s alpha values were ≥0.74 in this study.
Social Well-being was assessed using two scales: social well-being [3] and social support from family [63]. The 8-item social well-being scale was modified to assess interpersonal well-being as impacted by the experience of prostate cancer. Cronbach’s alpha values were ≥0.78. Social support from family was assessed using the 20-item Perceived Social Support-Family scale (PSS-FA) [63]. The PSS-FA scale has a strong record of psychometric quality, correlating with variables such as degree of relational reciprocity, and intangible and tangible support from family members [63]. Cronbach’s alpha values were ≥0.79 for survivors and ≥0.89 for partners.
Spiritual Well-Being was assessed using the 8-item spiritual well-being subscale of the Quality of Life-Breast Cancer version questionnaire that assesses the influence of participants’ illness on their spirituality [2]. Rewording of the items on this subscale was not required. Response options ranged from 1 (not at all) to 10 (a great deal). Cronbach’s alpha values were 0.78 for survivors and 0.74 for partners at baseline.
Statistical analysis
Level 1 growth curve analyses (GCAs)
Multi-Level Modeling (MLM) was performed using SAS PROC MIXED. Individual growth curve parameters were obtained by Maximum Likelihood (ML) estimation, quantifying the systematic changes in criterion scores over time by empirically fitting regression lines for all criterion variables on which repeated measures were obtained. The following growth curve parameters were estimated: (1) the intercept, representing the starting value on each criterion variable prior to experimental treatment and (2) the natural logarithmic slope, using the unstandardized regression weights, representing the direction and magnitude of average change in status on each criterion variable over time. Because we expected negatively accelerated functions for the growth curves, the slopes were theoretically pre-specified to be curvilinear; a natural logarithmic transformation of time was therefore performed prior to the GCAs. An unstructured covariance matrix was specified in the MLM, in which all the variances and covariances among repeated observations were freely estimated and thus permitted to be different from each other.
The comparison of the mean Level 1 growth curve parameters against a population value of zero and across the two conditions found (1,69) degrees of freedom for their associated F tests, and statistical power available to detect an effect size of dz = 0.35, which is 0.83 for both tests. Growth curves or “chronometric” parameter estimates from the Level 1 GCAs were used for further statistical modeling, which is Level 2 GCAs [64–66] This approach had three advantages over more traditional alternatives because (1) it did not assume equal numbers of repeated observations across all subjects [67] or (2) homogeneity of rates or change (equal slopes) across all subjects (cf. [68–70]; and 3) it estimated growth curve parameters, intercepts and slopes, based on all observations available for each individual, which are much more reliable than the scores measured at each cross-sectional time wave [59, 71].
Level 2 GCAs
This analysis consisted of two successive components: (1) the comparison and testing of mean Level 1 chronometric growth curve parameters against zero and (2) the comparison and testing of mean Level 1 chronometric growth curve parameters against each other across treatment conditions. The comparison of mean Level 1 chronometric growth curve parameters against a population value of zero is an intrinsic part of the MLM analysis. After the individual-level parameter estimates were exported from this procedure, the comparison of mean Level 1 chronometric growth curve parameters across experimental treatment conditions was performed by simple analyses of variance.
Results
Differences between groups and changes over time
Means and standard deviations for the QOL outcomes over time are presented for survivors in Table 4 and for partners in Table 5. Table 6 presents a summary of the prostate cancer survivors’ mean slopes for every criterion variable by group (TIP-C or HEAC). Because none of the variables has a true zero, intercepts are not presented. Prior to analyzing the slopes, however, all intercepts were tested for significant differences between the two treatment groups. No significant differences were found, confirming that random assignment resulted in equivalent groups on all of the QOL outcomes at baseline.
Changes in the outcomes as a function of treatment condition were examined in two ways. First, we examined whether there was significant change on any of the outcomes within either group. The statistical significance of the difference from zero for each of the mean slopes is indicated by an asterisk (*) in Table 6. The survivors in the TIP-C condition did not exhibit any significant changes on any of the QOL outcomes over time. In contrast, the men in the HEAC condition showed significant changes on 5 of the 9 outcomes, all in the direction of improved QOL. There was significant improvement in all four QOL dimensions over the course of the study: psychological well-being [decreased depression (b = −3.6012), negative affect (b = −2.8142), perceived stress (b = −3.1142)], physical well-being [decreased fatigue (b = −5.2955)], social well-being [increased social support from family members (b = 1.5593), and spiritual well-being (b = 2.6108)].
Second, to determine the effectiveness of the interventions, the magnitude of the slopes for each outcome was compared across the two groups. Results showed that improvements in depression, negative affect, perceived stress, fatigue, and spiritual well-being were significantly higher in magnitude for survivors in HEAC than for those in the TIP-C condition.
Table 7 contains results for the partners in the two different interventions. All intercepts were tested for equivalence between the two treatment groups. These tests found no significant differences, indicating that the groups were statistically equivalent on all outcomes at baseline. As seen in Table 7, the partners in the TIP-C condition had significant changes over time for depression (b = −2.2679). There was significant improvement in their psychological well-being over the course of the investigation. In the HEAC condition, similar to the findings for the survivors in the HEAC, partners demonstrated improvement in multiple dimensions of QOL over the course of the study: Psychological well-being [depression (b = −3.8946)], social well-being [social support from family (b = 1.6075), social well-being (b = 4.4571)], and spiritual well-being (b = 4.0452).
The magnitude of the slopes was also examined for the partners. Partners in the HEAC condition evidenced significantly greater improvements in depression, fatigue, social support from family members, social well-being, and spiritual well-being compared to partners in TIP-C.
Discussion
The primary aim of this investigation was to test the effectiveness of two telephone-delivered psychosocial interventions for maintaining and improving QOL among prostate cancer survivors and the partners who were supporting them in their recovery. The TIP-C intervention focused on appraisal of social relationships, how they are affected by cancer diagnosis and treatment, and effective management of potential emotional distress. The HEAC provided health education about prostate cancer and healthy lifestyle practices. The results revealed superior outcomes for the HEAC for both prostate cancer survivors and their partners. The salutary outcomes of the HEAC were evident in both slopes that were significantly different from zero, indicating upward trajectories on QOL over the course of the investigation, and by a significantly higher magnitude of many of the QOL slopes compared to those of the participants in the TIP-C.
The prostate cancer survivors in the TIP-C showed stable profiles on QOL outcomes. Although this suggests that the TIP-C did not affect significant change in these survivors, it should be noted that the QOL for these prostate cancer survivors and partners was relatively high. More importantly, there was no evidence of significant deterioration of QOL in this group. Among a sample of aging prostate cancer patients and survivors, arresting deterioration in QOL is not necessarily a trivial outcome. At the same time, survivors in HEAC showed statistically significant improvements over time for outcomes in all four QOL dimensions. Further, their improvements were all significantly better than the corresponding outcomes of the survivors in the TIP-C. In all probability, the initial emotional reactions and psychological distress typically experienced after diagnosis and during early treatment had already been resolved when these men entered the study, given the substantial elapsed time since diagnosis. Similarly, the lack of significant change found for the UCLA Prostate Cancer Index was again likely due to the stability in their QOL given the number of years living with the disease. Another possible explanation for the lack of significant findings for the TIP-C might be due to the modest dose of the intervention, although previous research with female survivors and their male partners found significant QOL improvements for those assigned to TIP-C using this same dose [55, 72, 73]. There may be a gender effect or a dose and gender interaction effect, with men needing a larger dose for equivalent effectiveness. Future research may need to examine the effectiveness of the intervention when the dose is larger (e.g., 50 min session) and to compare effectiveness of the intervention by examining the dose and gender interaction.
The partners in this investigation who were mostly spouses or other immediate family members also showed greater improvement in QOL in the HEAC. The rates of depression found at baseline in this sample were consistent with rates noted in the literature [12, 15], and both interventions decreased depression over the course of the investigation. It is noteworthy that partners in both conditions evidenced statistically significant improvements in depression, even with a reduced dose of the intervention (4 sessions) compared to the 8 sessions for the survivors. However, HEAC partners had statistically significant improvements in three of the four QOL dimensions, and all of these improvements were significantly stronger in magnitude than the corresponding changes for those in the TIP-C condition. Future research should examine the effect when partners also receive 8 sessions and when partners and survivors receive the intervention simultaneously.
The efficacy of the HEAC for this sample of prostate cancer survivors and their partners is consistent with studies demonstrating a connection between unmet informational needs or distorted perceptions of cancer and effective adjustment [39, 40]. Lack of information and distorted perceptions of cancer can impede effective contact with and utilization of health care services, and can exaggerate psychological distress among men with prostate cancer, even when they are 18 months beyond completion of treatment [40]. The results of the present study suggest that information-based interventions, with relatively simple designs and delivery requirements can facilitate substantial improvements in multiple QOL dimensions for prostate cancer survivors and their partners.
It is important to note that the length of time since diagnosis was extensive and highly varied in this sample. Cancer patients and their families often evidence greatest adjustment-related demands in the initial months after diagnosis, after which psychological distress often dissipates [74]. The fact that many participants were so far into the survivorship trajectory may explain the preponderance of stable profiles for the QOL outcomes. This also raises the question of whether the TIP-C could have been more effective for participants earlier in the survivorship trajectory, when acute coping with emotional reactions and alignment of close relationships is a more novel and critical demand.
In contrast, the HEAC focused on delivery of information that is more globally beneficial to QOL such as nutrition, exercise, and cancer resources. Although it could be argued that informational needs should be less in survivors who are further out in treatment, these survivors and partners all had unmet needs for information, perhaps because they had either forgotten the information or the information had changed since their earlier cancer education. Health information might more strongly meet the needs of survivors and their partners who have already successfully navigated some of the demands inherent in the early stages of cancer diagnosis and treatment and are further along in their cancer journey.
In conclusion, these results should be interpreted with caution given the small, predominantly white sample where QOL was relatively high. However, the psychosocial interventions in this study were effective in improving the multiple dimensions of QOL for men with prostate cancer and their partners. Both the survivor and their intimate partner or family member benefitted from the interventions. However, future research needs to answer the question, “who benefits from which intervention at what point in their cancer journey?” to better meet the needs of prostate cancer survivors and their partners.
References
ACS (2010). Cancer Facts & Figures, 2010: American Cancer Society.
Ferrell, B. R., Grant, M., Funk, B., Otis-Green, S., & Garcia, N. (1998). Quality of life in breast cancer. Part II: Psychological and spiritual well-being. Cancer Nursing, 21(1), 1–9.
Ferrell, B. R., Grant, M., Funk, B., Otis-Green, S., & Garcia, N. (1997). Quality of life in breast cancer. Part I: Physical and social well-being. Cancer Nursing, 20(6), 398–408.
Sharpley, C. F., & Christie, D. R. (2007). An analysis of the psychometric profile and frequency of anxiety and depression in Australian men with prostate cancer. Psycho-oncology, 16(7), 660–667.
Pirl, W. F., Siegel, G. I., Goode, M. J., & Smith, M. R. (2002). Depression in men receiving androgen deprivation therapy for prostate cancer: A pilot study. Psycho-oncology, 11(6), 518–523.
Jacobsen, P. B., & Jim, H. S. (2008). Psychosocial interventions for anxiety and depression in adult cancer patients: Achievements and challenges. CA: A Cancer Journal for Clinicians, 58(4), 214–230.
Bennett, G., & Badger, T. A. (2005). Depression in men with prostate cancer: A Review. Oncology nursing forum, 32(3), 545–556.
Korfage, I. J., Essink-Bot, M. L., Janssens, A. C., Schroder, F. H., & de Koning, H. J. (2006). Anxiety and depression after prostate cancer diagnosis and treatment: 5-year follow-up. British Journal of Cancer, 94(8), 1093–1098.
Mehnert, A., Lehmann, C., Schulte, T., & Koch, U. (2007). Presence of symptom distress and prostate cancer-related anxiety in patients at the beginning of cancer rehabilitation. Onkologie, 30(11), 551–556.
Thaker, P. H., Lutgendorf, S. K., & Snood, A. K. (2007). The neuroendocrine impact of chronic stress in cancer. Cell Cycle, 6(4), 430–433.
Faul, L. A., Jim, H. S., Williams, C., Loftus, L., & Jacobsen, P. B. (2010). Relationship of stress management skills to psychological distress and quality of life in adults with cancer. Psycho Oncology, 19(1), 102–109.
Braun, M., Mikulincer, M., Rydall, A., Walsh, A., & Rodin, G. (2007). Hidden morbidity in cancer: Spouse caregivers. Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology, 25(30), 4829–4834.
Segrin, C.,& Badger, T. (2010). Psychological distress in different social network members of breast and prostate cancer patients. Research in nursing & health. (Journal Article).
Butler, S. B., Turner, W., Kaye, L. W., Ruffin, L., & Downey, R. (2005). Depression and caregiver burden among rural elder caregivers. Journal of Gerontological Social Work, 46, 47–63.
Bambauer, K. Z., Zhang, B., Maciejewski, P. K., et al. (2006). Mutuality and specificity of mental disorders in advanced cancer patients and caregivers. Social Psychiatry and Psychiatric Epidemiology, 41(10), 819–824.
Danjoux, C., Gardner, S., & Fitch, M. (2007). Prospective evaluation of fatigue during a course of curative radiotherapy for localised prostate cancer. Supportive Care in Cancer : Official Journal of the Multinational Association of Supportive Care in Cancer, 15(10), 1169–1176.
Butt, Z., Rosenbloom, S. K., Abernethy, A. P. et al. (2008). Fatigue is the most important symptom for advanced cancer patients who have had chemotherapy. Journal of the National Comprehensive Cancer Network (JNCCN). 6(5), 448–455.
Michaelson, M. D., Cotter, S. E., Gargollo, P. C., Zietman, A. L., Dahl, D. M., & Smith, M. R. (2008). Management of complications of prostate cancer treatment. CA: A Cancer Journal for Clinicians, 58(4), 196–213.
Litwin, M. S., Hays, R. D., Fink, A., et al. (1998). The UCLA prostate cancer index: Development, reliability and validity of a health related quality of life measure. Medical Care, 36, 1002–1012.
Litwin, M. S. G. D. (2003). Quality of life following definitive therapy for localized prostate cancer: Potential impact of multiple therapies. Current Opinions in Urology, 13(2), 153–156.
Manne, S., Badr, H., Zaider, T., Nelson, C., & Kissane, D. (2010). Cancer-related communication, relationship intimacy and psychological distress among couples coping with localized prostate cancer. Journal of Cancer Survivorship, 4, 74–85.
Sanders, S., Pedro, L. W., Bantum, E. O., & Galbraith, M. E. (2006). Couples surviving prostate cancer: Longterm intimacy needs and concerns following treatment. Clinical Journal of Oncology Nursing, 10(4), 503–508.
Couper, J., Bloch, S., Love, A., Duchesne, G., MacVean, M., & Kissane, D. (2009). Coping patterns and psychological distress in female partners of prostate cancer patients. Psychosomatics, 50(4), 375–382.
Baider, L., Ever-Hadani, P., Goldzweig, G., Wygoda, M. R., & Peretz, T. (2003). Is perceived family support a relevant variable in psychological distress? A sample of prostate and breast cancer couples. Journal of Psychosomatic Research, 55(5), 453–460.
Badger, T. A., Braden, C. J., Longman, A. J., & Mishel, M. M. (1999). Depression burden, self-help interventions, and social support in women receiving treatment for breast cancer. Journal of Psychosocial Oncology, 17(2), 17–35.
Turner-Cobb, J. M., Sephton, S. E., Koopman, C., Blake-Mortimer, J., & Spiegel, D. (2000). Social support and salivary cortisol in women with metastatic breast cancer. Psychosomatic Medicine, 62(3), 337–345.
Manne, S., Babb, J., Pinover, W., Horwitz, E., & Ebbert, J. (2004). Psychoeducational group intervention for wives of men with prostate cancer. Psycho-oncology, 13(1), 37–46.
Krongrad, A., Lai, H., Burke, M. A., Goodkin, K., & Lai, S. (1996). Marriage and mortality in prostate cancer. Journal of Urology, 156(5), 1696–1700.
Roberts, K. J., Lepore, S. J., & Helgeson, V. (2006). Social-cognitive correlates of adjustment to prostate cancer. Psycho-oncology, 15(3), 183–192.
Brady, M. J., Peterman, A. H., Fitchett, G., Mo, M., & Cella, D. (1999). A case for including spirituality in quality of life measurement in oncology. Psycho-oncology, 8, 417–428.
Medicine Io (2007). Cancer care for the whole patient: Meeting psychosocial health needs. Washington, D.C.: National Academies Press.
Gall, T. L. (2004). Relationship with god and quality of life of prostate cancer survivors. Quality of Life Research : An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 13, 1357–1368.
Penedo, F. J., Dahn, J. R., Molton, I., et al. (2004). Cognitive-behavioral stress management improves stress-management skills and quality of life in men recovering from treatment of prostate carcinoma. Cancer, 100(1), 192–200.
Penedo, F. J., Molton, I., Dahn, J. R., et al. (2006). A randomized clinical trial of group-based cognitive-behavioral stress management in localized prostate cancer: Development of stress management skills improves quality of life and benefit finding. Annals of Behavioral Medicine : A Publication of the Society of Behavioral Medicine, 31(3), 261–270.
Penedo, F. J., Traeger, L., Dahn, J., et al. (2007). Cognitive behavioral stress management intervention improves quality of life in Spanish monolingual hispanic men treated for localized prostate cancer: Results of a randomized controlled trial. International Journal of Behavioral Medicine, 14(3), 164–172.
Northouse, L. L., Mood, D. W., Montie, J. E., et al. (2007). Living with prostate cancer: Patients’ and spouses’ psychosocial status and quality of life. Journal of Clinical Oncology : Official Journal of the American Society of Clinical Oncology, 25(27), 4171–4177.
Couper, J., Bloch, S., Love, A., Macvean, M., Duchesne, G. M., & Kissane, D. (2006). Psychosocial adjustment of female partners of men with prostate cancer: A review of the literature. Psycho-oncology, 15(11), 937–953.
Ezer, H., Ricard, N., Bouchard, L., Souhami, L., Saad, F., Aprikian, A., et al. (2006). Adaptation of wives of prostate cancer following diagnosis and 3 months after treatment: A test of the family adaptation theory. International Journal of Nursing Studies, 43, 827–838.
Docherty, A., Brothwell, C. P., & Symons, M. (2007). The impact of inadequate knowledge on patient and spouse experience of prostate cancer. Cancer Nursing, 30, 58–63.
Traeger, L., Penedo, F. J., Gonzalez, J. S., Dahn, J. R., Lechner, S. C., Schneiderman, N., et al. (2009). Illness perceptions and emotional well-being in men treated for localized prostate cancer. Journal of psychsomatic Research, 67, 389–397.
Bailey Jr, D. E., Wallace, M., & Mishel, M. H. (2007) Watching, waiting and uncertainty in prostate cancer. Journal of clinical nursing. 16, 734–741.
Klerman, G. L., Weissman, M. M., Rounsaville, B. J., & Chevron, E. S. (1994). Interpersonal psychotherapy of depression. Northvale, NJ: Jason Aronson.
Klerman, G. L., & Weissman, M. M. (1993). New applications of interpersonal psychotherapy. Washington, DC: American Psychological Association.
Weissman, M. M., & Markowitz, J. C. (1998). An overview of interpersonal psychotherapy. In J. C. Markowitz (Ed.), Interpersonal psychotherapy (pp. 1–33). Washington, DC: American Psychiatric Press.
Weissman, M. M., Markowitz, J. C., & Klerman, G. L. (2000). Comprehensive guide to interpersonal psychotherapy. New York: Basic Books.
Hinrichsen, G. A., Cloughtery, K. P. (2006). Interpersonal psychotherapy for depressed older adults. Washington, DC: American Psychological Association.
National Cancer I (2008). What you need to know about prostate cancer. Vol NIH Publication No. 08-1576. Washington, DC.
Institute NC (2009). Eating hints for cancer patients: Before, during and after treatment. Washington DC: NIH.
Department of A, Department of H, Human S. Dietary Guidelines for Americans (2009). Vol 12/03/2009. Washington, DC: Department of Agriculture (USDA); Department of Health and Human Services (HHS).
Aging NIo (2009). Exercise and physical activity. Washington DC: NIH.
Institute NC (2009). NCI National Organization Database. 2009; https://cissecure.nci.nih.gov/factsheet/FactSheetSearch8_1.aspx. Accessed Web Page, 2009.
Institute NC (2009). How to find resources in your own community, Vol. 2009.
National Cancer I (2007). Quitting smoking: Why to quit and how to get help—National Cancer Institute. Vol 2009: National Cancer Institute.
Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401.
Badger, T. A., Segrin, C., Dorros, S. M., Meek, P. M., & Lopez, A. M. (2007). Depression and anxiety in women with breast cancer and their partners. Nursing research. 56, 44–53.
Watson, D., Clark, L. A., & Tellegan, A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scale. Journal of Personality and Social Psychology, 54, 1063–1070.
Manne, S., & Schnoll, R. (2001). Measuring cancer survivors’ psychological distress and well-being: A factor analytic assessment of the Mental Health Inventory. Psychological Assessment, 13, 99–109.
Melvin, G. A., & Molloy, G. N. (2000). Some psychometric properties of the positive and negative affect schedule among Australian youth. Psychological Reports, 86, 1209–1212.
Cohen, J. C., & Cohen, P. (Eds.) (1983). Applied multiple regression/correlation analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum.
Cohen, S., & Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98(2), 310–357.
Meek, P. M., Nail, L. M., Barsevick, A., et al. (2000). Psychometric testing of fatigue instruments for use with cancer patients. Nursing Research, 49(4), 181–190.
Karakiewicz, P. I., Kattan, M. W., et al. (2003). Cross-cultural validation of the UCLA prostate cancer index. Urology, 61(2), 302–307.
Procidano, M. E., & Heller, K. (1983). Measures of perceived social support from friends and from family: Three validation studies. American Journal of Community Psychology, 11(1), 1–24.
Figueredo, A. J., Brooks, A., Leff, S., & Sechrest, L. (2000). A meta-analytic approach to growth curve analysis. Psychological Reports, 87, 441–465.
Rogosa, D. S., & Saner, H. (1994) Longitudinal data analysis examples with random coefficient models. Presented at the Rand Conference in October 1993, Manuscript cited with permission.
Willett, J. S., & Sayer, A. G. (1994). Using covariance structure analysis to detect correlates and predictors of individual change over time. Psychological Bulletin, 166, 363–381.
McKnight, P. E., McKnight, K. M., Sidani, S., & Figuerdo, A. J. (2004). The applied researcher’s guide to missing data. New York: Guildford.
Gibbons, R., Hedeker, D., Waternauz, C., & Davis, J. (1988). Random regression models: A comprehensive approach to the analysis of longitudinal psychiatric data. Psychopharmacology Bulletin, 24, 438–443.
Raudenbush, S. W., & Bryk, A. S. (1992). Hierarchical linear models: Applications and data analysis methods. Newbury Park, CA: Sage.
Rogosa, D., Brandt, D., & Zimowski, M. (1982). A growth-curve approach to the measurement of change. Psychological Bulletin, 92, 726–748.
Sutcliffe, J. (1980). On the relationship of reliability to statistical power. Psychological Bulletin, 88, 509–515.
Badger, T., Segrin, C., Meek, P., Lopez, A. M., & Bonham, E. (2004). A case study of telephone interpersonal counseling for women with breast cancer and their partners. Oncology Nursing Forum, 31(5), 997–1003.
Badger, T., Segrin, C., Meek, P., Lopez, A. M., Bonham, E., & Sieger, A. (2005). Telephone interpersonal counseling with women with breast cancer: Symptom management and quality of life. Oncology Nursing Forum, 32(2), 273–279.
Henselmans, I., Sanderman, R., Baas, P. C., SMink, A., & Ranchor, A. V. (2009). Personal control after a breast cancer diagnosis: Stability and adaptive value. Psycho-oncology, 18(1), 104–108.
Acknowledgments
Funding for this R21 study (R21CA113409) was provided by the National Cancer Institute to Terry Badger. We gratefully thank our recruitment sites: Arizona Cancer Center, Veteran’s Affairs Health Care Systems in Phoenix and Tucson. This material is the result of work supported with the resources and the use of facilities at the Veteran’s Affairs Health Care Systems in Phoenix and Tucson. We thank Maria Figueroa, Xochitl Gaxiola, Jeannine Thomas, Jen Riech, and Karina Othon-Tapia. The contents of this publication do not represent the views of the Department of Veterans Affairs or the United States Government.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Badger, T.A., Segrin, C., Figueredo, A.J. et al. Psychosocial interventions to improve quality of life in prostate cancer survivors and their intimate or family partners. Qual Life Res 20, 833–844 (2011). https://doi.org/10.1007/s11136-010-9822-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-010-9822-2