Abstract
Purpose
There is limited data regarding Pituitary Stalk Interruption Syndrome (PSIS) from India. Moreover, the pathophysiological link between perinatal events and PSIS is unclear. We aim to elucidate the predictors of PSIS among patients with growth hormone deficiency (GHD) and perinatal events in PSIS by comparing cohorts of PSIS and genetically proven GHD without PSIS.
Methods
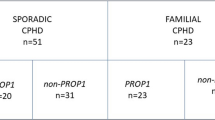
Among 179 GHD patients, 56 PSIS and 70 genetically positive GHD (52-GHRHR, 15-POU1F1, and 3-PROP1) patients were included. Perinatal events, clinical anomalies, pituitary hormone deficiency, and imaging findings were recorded. We compared PSIS-isolated GHD (PSIS-IGHD) subgroup with GHRHR-IGHD and PSIS-combined pituitary hormone deficiency (PSIS-CPHD) subgroup with POU1F1/PROP1-CPHD.
Results
PSIS patients (45 males, median age: 12.5 years) most commonly presented with short stature. At last follow-up (median age: 17.35 years), gonadal (during pubertal-age), thyroid and cortisol axes were affected in 81.6%, 62.5%, and 62.5%. 10/13 (77%) of PSIS children with initial IGHD diagnosis manifested hypogonadism during pubertal age. Male predominance, sporadic presentation, and clinical anomalies were significantly higher in both PSIS subgroups than in the respective genetic subgroups. Breech presentation was higher in PSIS-CPHD than POU1F1/PROP1-CPHD (44.4% vs 5.5%, p = 0.004). Neonatal hypoglycemia (22% vs. 0%, p = 0.05) and jaundice (42 vs. 5%, p = 0.004) were higher in PSIS-CPHD than PSIS-IGHD.
Conclusion
Later age at presentation and frequent hypogonadism were observed in our PSIS cohort. Male sex, sporadic presentation, clinical anomalies, and breech presentation predicted PSIS at presentation. Breech presentation in PSIS is likely due to stalk interruption rather than hormonal deficiency.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pituitary stalk interruption syndrome (PSIS), a rare disorder with an incidence of ~ 5 per million live births, is defined as a radiologic triad of an interrupted/thin/non-visualized pituitary stalk, ectopic posterior pituitary (EPP), and anterior pituitary hypoplasia (APH) [1]. Hormone deficiency pattern in PSIS patients is either isolated growth hormone deficiency (IGHD) or combined pituitary hormone deficiency (CPHD). Besides, they may have extra-pituitary birth defects. Most PSIS patients present in childhood with short stature (80%), whereas early neonatal (jaundice, hypoglycemia, micropenis, cryptorchidism) or late pubertal (hypogonadism) presentations are less common [1]. Most PSIS patients with CPHD and about one-third with IGHD have hypogonadism on follow-up [2]. Polygenic and environmental factors are implicated in PSIS pathogenesis, and familial occurrence (~ 5%) is rare [3,4,5,6].
The association of breech presentation and PSIS has been consistently documented. Breech presentation (BP) was earlier thought of as a cause of perinatal infundibular injury. However, later observation of PSIS association with extra-pituitary birth defects favored the antenatal origin of this disorder, and BP is considered an effect of PSIS [7, 8]. However, the pathophysiological link between BP and PSIS is unknown. PSIS patients with CPHD have a significantly higher proportion have BP than those with IGHD, and the former subgroup is also associated with a severe anatomical defect in terms of non-visualised pituitary stalk (NVPS) and EPP located at median eminence [9, 10]. Whether BP is related to the severity of PSIS structural defect or is compounded by additional hormonal factors is unclear. Comparison of PSIS cohort with those matched for hormonal deficiencies but with no potential for structural abnormalities of posterior pituitary and pituitary stalk may resolve this enigma.
There is limited data regarding PSIS from the Indian subcontinent [11, 12]. Hence, we aim to describe the phenotypic details of our PSIS cohort presenting at varying ages from western India. Further, to elucidate the phenotypic predictors of PSIS at presentation and explore the pathophysiological link between PSIS and perinatal events, we aim to compare PSIS patients with growth hormone deficiency (GHD) patients without PSIS and established genetic diagnosis (GHRHR, POU1F1, and PROP1).
Methods
This retrospective study was conducted in a tertiary care center from Western India after approval from Institutional Ethics Committee (IEC-II/EC/OA-68/2019) with waiver of consent. The records (January 2002–May 2021) of idiopathic GHD patients (n = 179, excluding cases due to neoplastic, inflammatory, ischemic, or post-radiation pituitary insult) managed at our center were screened for inclusion in the study. The diagnosis of GHD was based on peak GH of < 7 ng/ml in patients < 18 years (clonidine stimulation test, insulin tolerance test, or glucagon stimulation test), or < 3 ng/ml for those aged ≥ 18 years on GH stimulation test (glucagon stimulation test) with low age and sex-matched serum insulin-like growth factor 1 (IGF-1) level [13]. CPHD was defined as the co-existence of GHD with any other anterior pituitary hormone deficiency (thyroid, cortisol, or gonadal axes). Central hypothyroidism was defined as low free/total thyroxine (T4) with low or inappropriately normal thyroid-stimulating hormone (TSH) levels. Central hypocortisolism was defined as 8.00 am serum cortisol of < 5 μg/dl, and/or serum cortisol < 18 μg/dl during the insulin tolerance test or 250 µg synacthen stimulation test (wherever available). Central hypogonadism was defined as the absence of pubertal onset by the chronological age of ≥ 14 and ≥ 13 years in males and females, respectively, and/or poor pubertal progression with low or inappropriately normal serum follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels. Gonadal axis evaluation was not performed in prepubertal patients. A water deprivation test was advised if polyuria was present. Patients with intact pituitary hormonal axes at initial evaluations were subjected to repeat evaluation at regular intervals whereas routine evaluation for recovery of hormonal axes was not performed except for that of GHD in a subset of patients during the transition period [14]. All hormonal assays were performed using a chemiluminescence assay (Advia Centaur CP, Siemens Healthcare) with intra- and inter-assay coefficients of variation of < 10%.
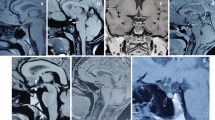
Pituitary magnetic resonance imaging (MRI) was performed using a 1.5 Tesla unit with T1/T2-weighted sagittal and coronal sections with/without gadolinium contrast enhancement. The maximal height of the pituitary gland was measured perpendicular to the sella turcica and considered hypoplastic when less than − 2 SD for age and sex. Pituitary stalk was recorded as thin, interrupted, or non-visualised [15]. Location of the posterior pituitary was recorded as eutopic or ectopic (along the stalk or at median eminence). In addition, any extra pituitary malformations on imaging (EPMI) were recorded. Sellar volume was calculated as antero-posterior diameter × height × oblique diameter × 0.52 in mid-sagittal plane, and sellar volume < 10th centile for the chronological age-sex matched controls was considered low [16]. Additionally, clinically identifiable anatomical (skeletal/ophthalmic) anomalies (CIAA) were noted. Routine, standardized investigations for birth defects were not performed. History of neonatal hypoglycemia and prolonged neonatal jaundice were recorded.
We identified 56 GHD patients with PSIS. This cohort of GHD patients with PSIS has not been genotyped yet. Phenotypic data, including demographics, clinical presentation, history of perinatal events (BP, persistent hypoglycemia, prolonged jaundice/cholestasis, micropenis, and cryptorchidism), family history, hormonal, radiological, and treatment outcomes, were recorded. In addition, GHD patients without PSIS and established genetic diagnoses (GHRHR, POU1F1, and PROP1) (n = 70) were also included for the comparison. The methods of genetic analysis have been described previously [17]. To elucidate the phenotypic predictors of PSIS at presentation and the pathophysiological link between PSIS and perinatal events, patients with PSIS and IGHD (PSIS-IGHD, n = 20) were compared with GHD patients having pathogenic variants in GHRHR (GHRHR-IGHD, n = 52), and patients with PSIS and CPHD (PSIS-CPHD, n = 36) were compared with GHD patients having pathogenic variants in POU1F1/PROP1 (POU1F1/PROP1-CPHD, n = 18).
Statistical analysis
All categorical variables were expressed in actual numbers and percentages and continuous variables as mean ± standard deviation or median and interquartile range as applicable. The categorical variables were compared using the χ2 test, whereas continuous variables were compared using independent t‐test or Mann–Whitney U tests in normally and non-normally distributed data, respectively. A p-value of less than 0.05 was considered significant. All statistical analyses were done with SPSS version 27.0 (IBM, Armonk, NY).
Results
Baseline characteristics of PSIS cohort
Amongst 179 idiopathic GHD patients, 56 patients (31.3%) had MRI evidence of PSIS. Of these 56 PSIS patients, 45 (80.3%) were males, and 36 (64.3%) had CPHD at initial diagnosis. At presentation gonadal (among post-pubertal patients), thyroid, and cortisol axes were affected in 94%, 59%, and 59%, respectively. This cohort’s clinical, hormonal, and radiological details are given in Table 1 and per-patient details in supplemental data. The median age was 12.5 years (6.25–16.75) at diagnosis. Three patients (5.3%) presented during infancy, 36 (64.3%) during childhood (1–14 years) with short stature, and 17 (30.4%) after 14 years of age. Among the patients presenting in infancy, all three were males with CPHD (with both cortisol and thyroid axis affection) and micropenis, two of them had persistent hypoglycemia (one boy presented with hypoglycemic seizure) and cholestasis (one boy underwent liver biopsy). Among the late presenters, 16 (11 males) patients presented with delayed puberty, and one male patient with normal pubertal development presented for short stature. All patients had an apparent sporadic presentation. There was BP in 20 (36%), neonatal hypoglycemia in 8 (14.2%), prolonged neonatal jaundice in 16 (28.4%), and micropenis/cryptorchidism in 10 (22.2%). ClAA (skeletal and/or ophthalmic birth defects) were present in 18 (32%). The mean height SDS was − 4.63 ± 1.91 with a peak serum GH of 0.86 ± 1.13 ng/ml. Hyperprolactinemia was present in 13 (30.2%) patients. None of the patients had diabetes insipidus. On MRI, the anterior pituitary was hypoplastic in 50 (89%), the stalk was non-visualised in 22 (39%), and EPMI was seen in 20 (36%) patients. Patients with PSIS-CPHD had higher prevalence of neonatal hypoglycemia (22% vs 0%, p = 0.05), prolonged neonatal jaundice (42% vs 5%, p = 0.004), hyperprolactinemia (42.8% vs 6.67%, p = 0.01) and non-visualised stalk (50% vs 20%, p = 0.02) than PSIS-IGHD (Table 1). Peak serum GH (ng/ml) was similar between PSIS-IGHD (1.08 ± 1.17) and PSIS-CPHD (0.70 ± 1.09) groups. All the six patients (initial diagnosis: IGHD) that were evaluated for the recovery of GH axis during the transition period had persistent GHD.
Follow-up characteristics of PSIS cohort
At the last follow-up [median age: 17.35 (12.1–20.6) years], gonadal (among post-pubertal patients), thyroid, and cortisol axes were deficient in 81.6%, 62.5%, and 62.5%, respectively. PSIS patients treated with recombinant growth hormone therapy (n = 32) at a mean age of 9.18 ± 5.70 years, at a dose of 20 units/m2/week, for a mean duration of 53.03 ± 36.18 months improved their height SDS from − 4.39 ± 1.73 to − 2.10 ± 1.82. Amongst 20 patients with the initial diagnosis of IGHD, 10 had additional hormonal deficits (gonadal axis: 10, thyroid axis: 2, cortisol axis: 1) on follow-up [median age: 15.6 (12.9–18.0) years]. Among these 20 IGHD patients, follow-up ≥ 13 years of age in girls or ≥ 14 years of age in boys was available for 13 patients, of whom10 (77%) were hypogonadal. Amongst 36 patients with the initial diagnosis of CPHD, five had additional hormonal deficits (gonadal axis: 5, cortisol axis: 1) on follow-up [median age: 18.2 (10.3–21.9) years]. All 16 patients with the initial diagnosis of CPHD and age ≥ 13 years of age in girls or 14 years of age in boys were hypogonadal. Among the remaining 20 CPHD patients, follow-up ≥ 13 years of age in girls or 14 years of age in boys was available for seven patients, of whom five (71.4%) were hypogonadal. Overall, 21/23 (91.3%) CPHD patients had evidence of hypogonadism in the pubertal age.
Comparison between PSIS cohort and GHD patients with established genetic diagnoses and without PSIS
Clinical details of PSIS-IGHD patients (n = 20) were compared with GHRHR-IGHD patients (n = 52) (Table 1). Male predominance (75% vs 46.2%, p = 0.03, OR 3.5), sporadic presentation (100% vs 42.4%, p < 0.001), CIAA (25% vs 0%, p = 0.001) and EPMI (20% vs 0%, p = 0.009) were significantly more common, whereas preterm deliveries (20% vs 5.8%, p = 0.07), and BP (20% vs 5.8%, p 0.07) tended to be more frequent in the PSIS-IGHD cohort.
Clinical details of PSIS-CPHD cohort (n = 36) were compared with POU1F1/PROP1-CPHD patients (n = 18) (Table 1). Male predominance (83.3% vs 44.4%, p = 0.003, OR 6.25), sporadic presentation (100% vs 36.4%, p < 0.001), BP (44.4% vs 5.5%, p = 0.004, OR 13.6), CIAA (36% vs 0%, p = 0.002), EPMI (44.4% vs 0%, p < 0.001) were significantly more common in the PSIS-CPHD cohort, whereas preterm deliveries (13.9% vs 0%, p = 0.09) showed a higher trend in latter subgroup.
The sellar volume was low in all PSIS patients but was comparable to that of the genetic cohort (113.04 ± 95.56 vs. 128.78 ± 58.2 mm3, p = 0.65) (supplemental data).
Discussion
In this large monocentric series of PSIS patients from Western India, the most common presentation was in childhood with short stature (64.3%), followed by delayed puberty (28.5%) in adolescence. Neonatal hypoglycemia, neonatal jaundice, hyperprolactinemia, and NVPS were significantly higher in PSIS-CPHD patients than in the PSIS-IGHD patients. Most PSIS patients had hypogonadism on evaluation at pubertal age (IGHD: 77%, CPHD: 91.3%), while new-onset cortisol (IGHD: 5%, CPHD: 33%) and thyroid (IGHD: 20%, CPHD: 0%) axis deficiencies were less common. Male predominance, sporadic presentation, CIAA, and EPMI were more frequent in the PSIS-IGHD patients than GHRHR-IGHD patients. Male predominance, sporadic presentation, BP, CIAA, and EPMI were more frequent in the PSIS-CPHD patients than those with POU1F1/PROP1-CPHD.
Median age at diagnosis of PSIS varied from 2.5 (range 0–16.3) years in a French cohort to 25 (range 22–28) years in a Chinese series (Table 2) [8, 9, 18,19,20,21,22,23]. The age at presentation was largely influenced by whether the report was published from pediatric or adult endocrine departments. Our endocrine unit caters to both pediatric and adult patients; hence, our cohort had patients presenting at varied ages (range 0.3–37). In a PSIS cohort from Spain, though 30.8% were diagnosed in adulthood (≥ 18 years), most had received growth hormone or sex steroids prior [24]. In our series, 23.2% (13/56) of patients received the first medical attention for hormonal deficiency in adulthood (≥ 18 years), suggesting a delay in diagnosis and/or specialist referral probably due to resource constraint settings.
In this study, male sex, sporadic presentation, BP, CIAA, and EPMI predicted PSIS in both IGHD and CPHD groups. Several PSIS series have reported a higher male to female ratio (1.7–6.9) among PSIS patients (Table 2), which has been hypothesized to be due to a role of X-linked recessive genes, sex chromosome-environmental interactions, or an unexplained male susceptibility to prenatal insults[25].
Sporadic presentation as a predictor of PSIS in our series may be skewed due to comparison with the genetic cohorts. Nevertheless, several other series have reported a rarity (0–8.8%) of familial occurrence with PSIS (Table 2). Many pathogenic and candidate genes have been implicated but with a low yield (~ 5%) [1]. This re-affirms the minimal role of monogenic factors in the pathogenesis of PSIS. Another specific association with PSIS is extra pituitary birth defects, described in 4–52% of patients (Table 2). The presence of CIAA and EPMI can predict an early diagnosis of PSIS. Association with birth defects in PSIS could be explained by defects in early embryonic development, which may concurrently involve various organ systems. Notably, all of our PSIS patients had a smaller sellar volume than the age-sex matched controls although the normative data used was not population- and imaging method-specific [16]. However, this is not a unique feature of PSIS as similar finding was also noted in the genetic cohort.
The prevalence of BP [36%, IGHD: 20%, CPHD: 40%) was high in our PSIS cohort, which is consistent with most previous reports (19–91.5%) (Table 2). This is in contrast to IGHD/CPHD patients with established genetic diagnoses in whom the prevalence of BP is comparable to the general population [26]. Hence, a history of BP in IGHD/CPHD patients should raise clinical suspicion for PSIS. However, the pathophysiological link between BP and PSIS is unknown. The high prevalence of BP in PSIS cohorts but not in IGHD/CPHD patients with molecular diagnosis suggests a strong association of BP with stalk interruption rather than pituitary hormonal deficiency. We hypothesize that the lack of a yet-unknown factor from the fetal hypothalamic-pituitary axis that regulates fetal head engagement may be responsible for the frequent occurrence of BP in PSIS.
Perinatal events like neonatal hypoglycemia (22% vs. 0%) and jaundice (42 vs. 5%) were higher in the PSIS-CPHD cohort than the PSIS-IGHD but were comparable in PSIS-IGHD vs. GHRHR-IGHD and PSIS-CPHD vs. POU1F1/PROP1-CPHD. Thus, these perinatal events seem to be related to CPHD rather than PSIS per se. The majority (7/8) of patients with hypoglycemia had hypocortisolemia in our cohort. Glucose homeostasis in hypopituitarism, as in normal individuals, is primarily dependent upon the balance between insulin secretion and the secretion of hormones antagonistic to insulin, mainly cortisol [27]. Three of our PSIS infants presented with persistent hypoglycemia and/or cholestasis-related concerns had CPHD with both cortisol and thyroid deficiency. In a larger series of neonates with PSIS, hypoglycemia (15/16) and cholestasis (5/16) were common. Cholestasis was implicated due to cortisol deficiency with additive roles for GH or/and the TSH deficiencies [28]. Reduced immunohistochemical expression of bile canalicular transport proteins has been demonstrated in infants with cholestasis and CPHD [29]. Early diagnosis and appropriate hormonal replacements mitigate hypoglycemia and cholestasis in infants with CPHD.
In our cohort, PSIS-CPHD patients had a high prevalence of pubertal hypogonadism (91.3%) which is similar to most other PSIS-CPHD cohorts (80–100%) [2, 7, 24, 30, 31]. In contrast, progression to pubertal hypogonadism in patients with initial diagnosis of PSIS-IGHD is widely variable [(0% (0/6), 33% (2/6), 64% (7/11), and 77% (13/17)] [2, 7, 24, 31]. Besides small sample size and comparison bias, variable severity of PSIS may contribute to this variability. Pubertal patients with IGHD with preserved gonadal axis may have a milder defect in hypothalamic-pituitary connection (trophic hormones) than those with IGHD progressing to hypogonadism. Following the continuum, patients with the most severe defect have multiple hormone deficiencies, including cortisol and thyroid axis. Our study showed that a higher proportion of PSIS-CPHD patients than PSIS-IGHD had absent stalk and hyperprolactinemia. Functional hyperprolactinemia (secondary to stalk interruption) may have an additive role in the pathogenesis of central hypogonadism. Prepubertal markers of hypogonadism (micropenis/cryptorchidism) were common [91% (10/11)] in PSIS children who developed hypogonadism in adolescence [2]. Similarly, in another French series of 53 post-pubertal patients, micropenis was more common in PSIS-CPHD than PSIS-IGHD (69% vs. 13%) [22]. Hence, the history of micropenis/cryptorchidism in childhood is a clinical predictor of pubertal hypogonadism.
Many series have reported the occurrence of new-onset thyroid and cortisol deficiencies during follow-up, as also noted in three of our patients, of whom two had an initial diagnosis of IGHD. These observations suggest that either development of new-onset additional hormone deficiencies or the unmasking of a pre-existing gonadotropin deficiency is common overtime in PSIS-IGHD [32]. Interestingly, the reasons for the delayed development of anterior pituitary hormonal deficiencies in PSIS are not clear. It may be due to a failure to meet increased demand for hormonal production as the child grows, especially in the peri- and post-pubertal period. However, exploring a role for additional mechanisms such as the development of autoimmunity following a possible intrauterine vascular insult to the pituitary, akin to that proposed in Sheehan syndrome and traumatic brain injury, may be interesting [33, 34].
This is one of the largest series from the Indian subcontinent of PSIS and highlights late presentation and higher involvement of gonadal axis on follow up. Further, comparison with genetically diagnosed cases of IGHD/CPHD (eutopic posterior pituitary and normal stalk) provides additional insights into the association of perinatal events with PSIS or hormone deficiencies. However, our study is limited by retrospective study design and unavailability of genetics and gonadotropin stimulation tests in all patients.
To conclude, later age at presentation and higher evolution to hypogonadism were observed in our cohort. Male sex, sporadic presentation, associated CIAA and EPMI, and BP predicted PSIS at presentation as compared to genetic cohort. Breech presentation is likely due to stalk interruption rather than pituitary hormonal deficiency, in contrast neonatal hypoglycemia and jaundice are probably due to multiple hormone deficiency rather than structural defect per se. Further studies are warranted to understand the genetics of PSIS in Asian Indian patients.
References
Vergier J, Castinetti F, Saveanu A et al (2019) Pituitary stalk interruption syndrome: etiology and clinical manifestations. Eur J Endocrinol 181:R199–R209. https://doi.org/10.1530/EJE-19-0168
Rottembourg D, Linglart A, Adamsbaum C et al (2008) Gonadotrophic status in adolescents with pituitary stalk interruption syndrome. Clin Endocrinol (Oxf) 69:105–111. https://doi.org/10.1111/j.1365-2265.2007.03155.x
Zwaveling-Soonawala N, Alders M, Jongejan A et al (2018) Clues for polygenic inheritance of pituitary stalk interruption syndrome from exome sequencing in 20 patients. J Clin Endocrinol Metab 103:415–428. https://doi.org/10.1210/jc.2017-01660
Fang X, Zhang Y, Cai J et al (2020) Identification of novel candidate pathogenic genes in pituitary stalk interruption syndrome by whole-exome sequencing. J Cell Mol Med 24:11703–11717. https://doi.org/10.1111/jcmm.15781
Brauner R, Bignon-Topalovic J, Bashamboo A, McElreavey K (2020) Pituitary stalk interruption syndrome is characterized by genetic heterogeneity. PLoS ONE 15:1–19. https://doi.org/10.1371/journal.pone.0242358
Guo QH, Wang CZ, Wu ZQ et al (2017) Multi-genic pattern found in rare type of hypopituitarism: a whole-exome sequencing study of han chinese with pituitary stalk interruption syndrome. J Cell Mol Med 21:3626–3632. https://doi.org/10.1111/jcmm.13272
Pinto G, Netchine I, Sobrier ML et al (1997) Pituitary stalk interruption syndrome: a clinical-biological-genetic assessment of its pathogenesis. J Clin Endocrinol Metab 82:3450–3454. https://doi.org/10.1210/jc.82.10.3450
Simon D, Hadjiathanasiou C, Garel C et al (2006) Phenotypic variability in children with growth hormone deficiency associated with posterior pituitary ectopia. Clin Endocrinol (Oxf). https://doi.org/10.1111/j.1365-2265.2006.02484.x
Melo ME, Marui S, Carvalho LR et al (2007) Hormonal, pituitary magnetic resonance, LHX4 and HESX1 evaluation in patients with hypopituitarism and ectopic posterior pituitary lobe. Clin Endocrinol (Oxf) 66:95–102. https://doi.org/10.1111/j.1365-2265.2006.02692.x
Chen S, Léger J, Garel C et al (1999) Growth hormone deficiency with ectopic neurohypophysis: anatomical variations and relationship between the visibility of the pituitary stalk asserted by magnetic resonance imaging and anterior pituitary function. J Clin Endocrinol Metab 84:2408–2413. https://doi.org/10.1210/jcem.84.7.5849
Dutta P, Bhansali A, Singh P et al (2009) Congenital hypopituitarism: clinico-radiological correlation. J Pediatr Endocrinol Metab 22:921–928. https://doi.org/10.1515/JPEM.2009.22.10.921
Kulkarni C, Moorthy S, Pullara S et al (2012) Pituitary stalk transection syndrome: comparison of clinico-radiological features in adults and children with review of literature. Indian J Radiol Imaging 22:182–185. https://doi.org/10.4103/0971-3026.107179
Jadhav S, Diwaker C, Lila AR et al (2021) POU1F1 mutations in combined pituitary hormone deficiency: differing spectrum of mutations in a Western-Indian cohort and systematic analysis of world literature. Pituitary 24:657–669. https://doi.org/10.1007/s11102-021-01140-9
Grimberg A, Divall A, Allen DB (2016) Hormone research in guidelines for growth hormone and insulin-like growth factor-I treatment in children and adolescents: growth hormone deficiency, idiopathic short stature, and primary insulin-like growth factor-I deficiency. Horm Res Paediatr 19104:361–397. https://doi.org/10.1159/000452150
Jagtap VS, Acharya SV, Sarathi V et al (2012) Ectopic posterior pituitary and stalk abnormality predicts severity and coexisting hormone deficiencies in patients with congenital growth hormone deficiency. Pituitary 15:243–250. https://doi.org/10.1007/s11102-011-0321-4
Chilton LA, Dorst JP, Garn M (1983) The volume of the seila turcica in children : new standards. AJR 140:797–801. https://doi.org/10.2214/ajr.140.4.797
Kale S, Gada JV, Jadhav S et al (2020) Genetic spectrum and predictors of mutations in four known genes in asian indian patients with growth hormone deficiency and orthotopic posterior pituitary: an emphasis on regional genetic diversity. Pituitary 23:701–715. https://doi.org/10.1007/s11102-020-01078-4
Bar C, Zadro C, Diene G et al (2015) Pituitary stalk interruption syndrome from infancy to adulthood: clinical, hormonal, and radiological assessment according to the initial presentation. PLoS ONE 10:1–12. https://doi.org/10.1371/journal.pone.0142354
Wang W, Wang S, Jiang Y et al (2015) Relationship between pituitary stalk (PS) visibility and the severity of hormone deficiencies: PS interruption syndrome revisited. Clin Endocrinol (Oxf) 83:369–376. https://doi.org/10.1111/cen.12788
Wang F, Han J, Shang X, Li G (2019) Distinct pituitary hormone levels of 184 Chinese children and adolescents with multiple pituitary hormone deficiency: a single-centre study. BMC Pediatr 19:1–9. https://doi.org/10.1186/s12887-019-1819-6
Wang Q, Hu Y, Li G, Sun X (2014) Pituitary stalk interruption syndrome in 59 children: the value of MRI in assessment of pituitary functions. Eur J Pediatr 173:589–595
Pham LL, Lemaire P, Harroche A et al (2013) Pituitary stalk interruption syndrome in 53 postpubertal patients: factors influencing the heterogeneity of its presentation. PLoS ONE. https://doi.org/10.1371/journal.pone.0053189
Guo Q, Yang Y, Mu Y et al (2013) Pituitary stalk interruption syndrome in Chinese people: clinical characteristic analysis of 55 cases. PLoS ONE. https://doi.org/10.1371/journal.pone.0053579
Fernandez-Rodriguez E, Quinteiro C, Barreiro J et al (2011) Pituitary stalk dysgenesis-induced hypopituitarism in adult patients: prevalence, evolution of hormone dysfunction and genetic analysis. Neuroendocrinology 93:181–188. https://doi.org/10.1159/000324087
Deal C, Hasselmann C, Pfäffle RW et al (2013) Associations between pituitary imaging abnormalities and clinical and biochemical phenotypes in children with congenital growth hormone deficiency: data from an international observational study. Horm Res Paediatr 79:283–292. https://doi.org/10.1159/000350829
Hofmeyr GJ, Hannah M, Lawrie TA (2015) Planned caesarean section for term breech delivery. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD000166
Adamkin DH, Papile LA, Baley JE et al (2011) Clinical report—postnatal glucose homeostasis in late-preterm and term infants. Pediatrics 127:575–579. https://doi.org/10.1542/peds.2010-3851
Mauvais FX, Gonzales E, Davit-Spraul A et al (2016) Cholestasis reveals severe cortisol deficiency in neonatal pituitary stalk interruption syndrome. PLoS ONE 11:1–12. https://doi.org/10.1371/journal.pone.0147750
Grammatikopoulos T, Deheragoda M, Strautnieks S et al (2018) Reduced hepatocellular expression of canalicular transport proteins in infants with neonatal cholestasis and congenital hypopituitarism. J Pediatr 200:181–187. https://doi.org/10.1016/j.jpeds.2018.05.009
Kandemir N, Yordam N, Cila A, Besim A (2000) Magnetic resonance imaging in growth hormone deficiency: relationship between endocrine function and morphological findings. J Pediatr Endocrinol Metab 13:171–178. https://doi.org/10.1515/JPEM.2000.13.2.171
Maghnie M, Larizza D, Triulzi F et al (1991) Hypopituitarism and stalk agenesis: a congenital syndrome worsened by breech delivery? Horm Res 35:101–108. https://doi.org/10.1159/000181883
Otto AP, França MM, Correa FA et al (2015) Frequent development of combined pituitary hormone deficiency in patients initially diagnosed as isolated growth hormone deficiency: a long term follow-up of patients from a single center. Pituitary 18:561–567. https://doi.org/10.1007/s11102-014-0610-9
Tanriverdi F, De BA, Bizzarro A et al (2008) Antipituitary antibodies after traumatic brain injury: is head trauma-induced pituitary dysfunction associated with autoimmunity ? Eur J Endocrinol. https://doi.org/10.1530/EJE-08-0050
De BA, Kelestimur F, Sinisi AA et al (2008) Anti-hypothalamus and anti-pituitary antibodies may contribute to perpetuate the hypopituitarism in patients with Sheehan’s syndrome. Eur J Endocrinol. https://doi.org/10.1530/EJE-07-0647
Funding
The authors did not receive any financial support for the submitted work.
Author information
Authors and Affiliations
Contributions
CD and PT contributed equally as first author. ARL conceived the presented idea. CD and PT collected and analyzed the data with the help of SSM, MK, and BK. CD and SSM wrote the manuscript in consultation with VS, ARL, TB, NS and VP. Genetic analysis was done by SA. Final version of the manuscript was checked by all authors.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare that are relevant to the content of this article.
Participant's informed consent
This was a retrospective study approved by the Institutional ethics committee with a waiver of consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Diwaker, C., Thadani, P., Memon, S.S. et al. Pituitary stalk interruption syndrome: phenotype, predictors, and pathophysiology of perinatal events. Pituitary 25, 645–652 (2022). https://doi.org/10.1007/s11102-022-01243-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-022-01243-x