Abstract
Introduction
Axial skeleton arthropathy and osteoporotic vertebral fractures are common findings in acromegalic patients and can result in severe spinal deformity.
Objective
To investigate the presence of spinal fractures and deformities, sagittal imbalances, and spinopelvic compensatory mechanisms in acromegalics.
Patients and methods
58 patients with acromegaly from a referral neuroendocrinology center were prospectively evaluated by panoramic spine radiographs to detect the presence of fractures and scoliosis, to measure thoracic kyphosis, lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT) and sagittal vertical axis (SVA). Sagittal imbalance criteria were considered: thoracic kyphosis > 50°, PI-LL > 10°, PT > 20° and SVA > 5 cm. Their medical records were analyzed for clinical and laboratorial data.
Results
The prevalence of fractures was 13.8%, predominantly in the thoracic spine, with mild and anterior wedge compressions. Scoliosis was present in 34.5% of the cases, all with degenerative lumbar curve apex. Thoracic kyphosis > 50º occurred in 36.8% of patients, PI-LL > 10° in 48.3%, PT > 20° in 41.4% and SVA > 5 cm in 12.1%.
Conclusion
Increased number of vertebral fractures and high prevalence of spinal deformities related to sagittal imbalance were detected, indicating the importance of monitoring bone comorbidities in acromegaly, with radiological evaluation of the spine as part of the follow up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acromegaly is a rare disease caused by excess secretion of growth hormone (GH) and insulin-like growth factor 1 (IGF-1), in more than 70% of cases associated with a pituitary macroadenoma [1, 2]. It has an estimated prevalence of 28–137 cases per million [3]. The most characteristic clinical changes are those that occur in soft tissues, skin, bones and joints, although there is a wide spectrum in the intensity of these findings. Although mortality associated with acromegaly is progressively normalizing [4], possibly due to drug treatment, morbidity is still high, mainly related to hypertension, diabetes mellitus, sleep apnea and arthropathy [5]. Descriptions of spinal involvement are classic in the literature [6], generally being restricted to kyphosis and chest deformities, but without further exploration of other parameters with possible functional repercussions.
The objective of this study was to evaluate the spine in patients with acromegaly, especially in relation to osteoporotic fractures, spinopelvic balance and their compensatory mechanisms.
Patients and methods
The study included 58 acromegalic patients recruited between April 2017 and May 2019, from a cohort at a referral Neuroendocrinology Center in Southern Brazil. Our study was performed in accordance with the Helsinki recommendations. Written informed consents were obtained from the participants, and the study was approved by the Ethics Committee of our university hospital.
Medical records were reviewed for clinical, laboratory and imaging, surgical, and anatomopathological information on the pituitary adenoma, treatment modalities, and follow up data. The diagnosis of acromegaly was established on clinical and hormonal bases (baseline and/or suppressed GH < 1 ng/mL and IGF-1 above the upper limit of normality corresponding to gender and age).
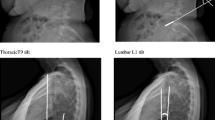
The patients were submitted to panoramic radiographs of the total and pelvic spine, anteroposterior and lateral, in orthostatic position, in the same institution. On radiographs, using the Cobb method [7] were measured thoracic kyphosis, lumbar lordosis (LL), sacral slope (SS), pelvic incidence (PI), pelvic tilt (PT) and sagittal vertical axis (SVA) (Fig. 1). Thoracic kyphosis was measured from the upper endplate of the most cranial detectable vertebra (usually T2 or T3) to the lower endplate of T12; LL from the upper endplate of L1 to the upper endplate of S1. The PI describes the anatomical shape of the pelvis and interferes with the spinal position. A low PI value implies lower values of other pelvic parameters and lesser lordosis. It is measured from the angle formed between a line perpendicular to the midpoint of the sacral endplate, and a line that connects this point to the central axis of the femoral head. PT is a pelvic position parameter; higher values indicate pelvic retroversion, a compensatory mechanism of sagittal imbalance, resulting in shifting of the axis of gravity backwards. It is measured from the angle between a line connecting the midpoint of the sacral endplate to the axis of the femoral head and a vertical line (perpendicular to the ground). SVA is the distance from the posterosuperior point of the sacral endplate to a vertical plumb line from C7 and it gives us a general idea of the patient balance. The validation of the obtained measurements was made through the formula: PI = SS + PT.
Scoliosis was defined by the presence of any lateral curvature of the spine above 10° by the Cobb method. The presence of vertebral fracture was verified by the semi-quantitative method of Genant [8]. Positive findings were independently reviewed by a second evaluator, a radiologist with experience in musculoskeletal pathology, and discordant cases were resolved by consensus.
Sagittal spinal deformities, determinants of sagittal imbalance, were determined by 4 criteria: dorsal or thoracic kyphosis > 50°, mismatch between PI and LL greater than 10° (PI-LL > 10°), PT > 20° and SVA > 5 cm [9, 10].
After analysis of descriptive parameters, for comparison between groups the t-test or Mann Whitney were used, according to the distribution of data. The comparison of categorical variables was performed by Fisher's exact test, and for the correlation study the Pearson coefficient. The evaluation was performed using the Statistical Package for Social Sciences (SPSS), version 22.0, using as significance level p < 0.05.
Results
Acromegaly features
The sample consisted of 58 patients, 35 (60.3%) men, with age at study entry 50.8 ± 12.7 (27–74) years and age at diagnosis of acromegaly 42.4 ± 12.5 years. MRI evaluation of the sellar region showed 49 macroadenomas (84.5%) and tumor invasion to the cavernous and/or sphenoid sinuses in 39.3% of the cases. Prolactin was elevated in 20 (34.4%) patients, up to 100 ng/mL in 11, between 101 and 200 ng/mL in 5 and above 200 ng/mL in 4.
Except for one patient, the others underwent pituitary adenomectomy and, in 3 cases, surgical reintervention. The Ki-67 index in tumor samples, available in 25 cases, was equal to or greater than 3% in 36% of them, with a maximum value of 8%. Radiotherapy was performed on five subjects.
In the last evaluation, complementary drug therapy was used in 40 cases: octreotide in 18 (45%), association of octreotide and cabergoline in 21 (52.5%) and, in 1 case, cabergoline alone.
In the last image, 46.6% had no tumor in the sellar region, 31% had tumor residue without extension or invasion and 20.7% had invasion to the cavernous (n = 11) or sphenoid sinus (n = 1).
Of the total sample, 16 (27.6%) individuals were cured considering IGF-1 level below 1.2 ULN (Upper Limit of Normality), GH less than 1 ng/mL and no lesion in the sellar region; 23 individuals showed biochemical control with drug use, according to the same criteria, constituting a total of 69.6% of individuals without active disease at the time of the evaluation.
Regarding the clinical variables, 12 cases (20.7%) had Type 2 Diabetes Mellitus and 44.8% were hypertensive. Headache was a complaint of 31% of the sample. 20.6% of the patients used 6 or more continuous medications (none to 10), and 19% of the sample used antidepressants drugs. Specific physical activity, such as walking, swimming, among others, was reported by 20.7% of individuals. Among the deficient hormonal axes, of particular interest to the study, 28 (48.3%) patients were hypogonadic, whether due to tumor-associated central etiology or primary gonadal failure such as menopausal women (with elevated gonadotropins).
Radiological findings
Spinal fractures were diagnosed in 8 patients (13.8%), and 3 of them had two fractures, totaling 11 fractures. There was a predominance of thoracic involvement (8 vertebrae). The most affected vertebrae were T11, T12 and L3, with 2 occurrences each. The classification of fractures revealed that 10 (90.9%) were grade 1 and one grade 2. Regarding the type of bone depression, 7 fractures (63.6%) had anterior wedge compression, and 4 had medium depression. The presence of vertebral osteoporotic fracture was related to low IGF-1 (p = 0.011) and GH (p = 0.014) values at diagnosis.
Anteroposterior (AP) radiographs reveled 20 (34.5%) cases of scoliosis, all degenerative, with the apex of the curve at the lumbar spine. Curve severity ranged from 10° to 25°.
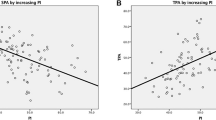
Thoracic kyphosis ranged from 20 to 73° (mean 46.7°) and in 21 cases (36.8%) was greater than 50°, one of the criteria used to define sagittal deformity. Lumbar lordosis ranged from 14 to 70° (mean 44.8°) and PI ranged from 30 to 122° (mean 53.5°). The PI-LL > 10°, which is the second criteria used to define sagittal imbalance, occurred in 28 patients (48.3%). The largest difference - and theoretically the most serious - was 82°.
The SS ranged from 13 to 50° (average 33.7°) and the PT between -6 to 72° (average 19.8°). Another criteria of sagittal imbalance, PT > 20°, was identified in 24 patients (41.4%).
SVA, the fourth criteria used for imbalance, ranged from − 6.9 to + 14.2 cm. Of these, 7 patients (12.1%) had SVA > 5 cm, meaning an excessively anterior sagittal shifting. SVA above 5 cm was correlated with increasing age (p = 0.03) and hypogonadism (p = 0.04). Fig. 2 exemplifies SVA > 5 cm (Fig. 2a), PT > 20º (Fig. 2b) and osteoporotic vertebral fracture (Fig. 2c).
Discussion
Clinical features
The results regarding the mean age at diagnosis, the predominance of macroadenomas, the percentage of invasive adenomas and hyperprolactinemia, as well as the prevalence of headache, diabetes mellitus, arterial hypertension and hypogonadism are consistent with those described in the literature [1, 2, 11,12,13,14,15,16,17,18,19]. A possible difference is related to gender, where we find two thirds of male patients, while in other series women predominate [17].
Transsphenoidal surgery was the first therapeutic option as established [17, 20, 21], complemented by somatostatin analogs and/or dopaminergic agonists. Of the 57 patients who underwent surgery, performed by the same experienced neurosurgeon, 27.6% were considered cured, while a recent review mentions cure percentages of 44.5% for suprasellar tumors, 33% for suprasellar tumors with visual impairment and 41.5% for tumors with parasellar and/or sphenoid invasion [19]. Regarding drug therapy, rigorously conducted trials demonstrate a 25–45% rate of biochemical control [5], resulting in uncontrolled disease in approximately one third of patients [3]. The percentage of active disease (31.4%) observed here may reflect previous very high GH/IGF-1 values, predominance of men in the sample, and non-use of a second generation SST analog or GH receptor antagonist treatment. Factors associated with the so-called “real world” should also be taken into account, such as the result of the last IGF-1 being eventually the first postoperative evaluation, failure in the drug distribution through the State system, or return to consultation after loss follow-up, in a context where the loss of follow-up in these patients is high, up to 17.6% [22, 23].
Radiological endpoints
Osteoporotic vertebral fractures in acromegalic patients are a frequent feature in the literature [6]. They occur independently of disease activity [24] and in the presence of normal Bone Mineral Density (BMD), making BMD a poor predictor of fracture risk in acromegaly. The reasons for the paradoxical skeletal fragility are the compromised bone turnover caused by the excess of GH and IGF-1 and changes in bone microarchitecture compromising its quality.
Bonadonna et al. [25] described fractures in acromegalic women in the proportion of 52.8% versus 30.6% in controls, while Mazziotti et al. [26] first described fractures in acromegalic men at 57.5% versus 22.6% in controls. Wassenaar et al. [27] followed by Padova et al. [28], Madeira et al. [29], and Mazziotti et al. [30] found respectively, 59, 39, 10.6 and 42% of fracture prevalence. In the current study, the percentage of individuals with fractures was 13.8%, close to that observed by Madeira et al. [29]. As most studies are cross-sectional, it is difficult to determine which fractures occurred in the active phase of acromegaly and which occurred after the biochemical control of the disease. In a prospective study, Claessen et al. [31] observed a 20% incidence of fractures in patients with remission disease, above of what is usually found in the general population, which is about 5–7% in postmenopausal women. The annual incidence of osteoporotic fractures can reach 30% [5].
The location of the fractures observed here, predominantly thoracic, and their type, predominantly low grade and in the anterior edges of the vertebrae, is described in another study [27]. These features possibly contribute to dorsal hyperkyphosis, a classic finding in acromegaly since its earliest descriptions [32]. Some patients develop barrel-shaped thorax as a result of changes in vertebral and rib morphology [33]. Vertebral osteoporotic fractures correlated, in the present series, with low GH and IGF-1 levels at diagnosis. There are no studies relating fracture occurrence with GH/IGF-1 levels, but positively with duration of active disease [6, 34]. We did not find a commonly established association between fractures and hypogonadism.
Scoliosis is a common finding in diseases with high stature, including pituitary gigantism itself, as shown in the first descriptions of the disease [35], but there are few reports of scoliosis in acromegalic adults. Scarpa et al. [36] found 15% of lumbar scoliosis in a sample of 54 acromegalics, while in one-third of our series the patients had low-grade degenerative lumbar scoliosis that, in the general population, has a lower risk of progression [37]. On the other hand, kyphosis is more commonly described in acromegaly, although without exploration over the degree of its severity or the spinopelvic compensatory mechanisms that occur when it is present. While we detected thoracic hyperkyphosis in 36.8%, for Scarpa et al. [36] it occurred in 21% of patients with acromegaly.
In recent years, there has been an increased interest among the spine specialists over the concept of Sagittal Balance, based on the growing recognition of problems related to incongruence of sagittal plane alignment after spinal surgeries with fusion and consequent failure to treat pain. Recent analysis suggests that sagittal imbalance may be a more critical parameter for clinical symptoms than coronal imbalance and therefore, although more difficult to measure, deserves as much or more attention than scoliosis.
Chronic exposure to high levels of GH, IGF-I, and insulin can potentially alter the physiological balance of the spine, through inducing disproportion in vertebral body diameters and impaired trophism of both facet joint and intervertebral disc [36]. The higher incidence of progressive osteoporotic compressions could also theoretically contribute to vulnerability for kyphotic deformity. Medical literature does not explore sagittal balance deviations in the acromegalic population. Despite being a relatively new concept in spine surgery, still without consensus on definitive diagnostic parameters, with the four criteria for determining deformity and sagittal imbalance used here, the number of patients with deformity draws attention. We observed marked thoracic kyphosis in one third of cases, marked incompatibility between pelvic incidence and lumbar lordosis in almost half of the sample, excessive pelvic tilt (PT) in more than 40% and anteriorization of the sagittal vertical axis (SVA) in over 10%. of the cases. The consequences of this may be chronic back pain, secondary to erector spinae overload, disc and facet degeneration in the spine, fatigue of the thigh and quadriceps extensors, accelerated arthrosis of the sacroiliac joints and lower limbs, among others. Initially retroversion of the pelvis may compensate for the loss of sagittal balance, but with time and the progression of degenerative changes, the trunk's accommodation capacity is exceeded, which is associated with increased energy expenditure for maintaining upright posture, causing functional disability [38]. In the later stages, the patient depends on support for standing, such as canes, walkers, and may even lose the ability to stand and walk completely. Significant imbalance and postural deviations have been reported in acromegalic patients evaluated by photogrammetry and stabilometry [39]. To the authors' knowledge, there is no data on spinopelvic balance that can be compared with the acromegalic population evaluated here.
The current study has limitations, starting with the fact that acromegaly is a rare disease, which requires multicenter studies or national registries to minimize biases usually associated with small samples. It is also mandatory a long follow up period for monitoring the progression of comorbidities. Finally, and most importantly, the results regarding sagittal balance, because they are original, need validation.
In summary, we found in a sample of acromegalics a fracture prevalence slightly higher than that observed in non-acromegalic menopausal women, and a high number of cases of lumbar degenerative scoliosis and thoracic hyperkyphosis. We highlight the findings regarding sagittal imbalance, so far not described in acromegaly. Parameters related to excessive trunk anteriorization (SVA > 5 cm) and compensatory mechanisms (high PT and mismatch between LL and PI) were present in a large number of cases.
Current guidelines on acromegaly already include follow up of patients with lumbar and thoracic spine X-ray every 2–3 years in the presence of risk factors or symptoms [19, 20]. Screening at diagnosis with conventional radiographs is also suggested by Wassenaar and colleagues and Mazziotti et al. [26, 27]. These indications rest on the fact that osteoporotic vertebral fractures are a warning for increased risk of hip fractures [40, 41], which do have a major impact on morbidity and mortality. In addition, acromegalic patients have a tendency to kyphotic deformity, with sagittal imbalance and its consequent compensatory mechanisms, which lead to chronic pain and functional limitations.
In conclusion, the authors introduce new parameters for the monitoring of bone comorbidities in acromegaly, suggest radiological follow up of the spine and emphasize the importance of a multidisciplinary approach in centers of excellence in the management of this disease that chronically impacts organic and emotional health, and that has great financial and social repercussions.
References
Mestron A, Webb SM, Astorga R, Benito P, Catala M, Gaztambide S, Gomez JM, Halperin I, Lucas-Morante T, Moreno B, Obiols G, de Pablos P, Paramo C, Pico A, Torres E, Varela C, Vazquez JA, Zamora J, Albareda M, Gilabert M (2004) Epidemiology, clinical characteristics, outcome, morbidity and mortality in acromegaly based on the Spanish Acromegaly Registry (Registro Español de Acromegalia, REA). Eur J Endocrinol 151:439–446
Dineen R, Stewart PM, Sherlock M (2017) Acromegaly. QJM 110(7):411–420. https://doi.org/10.1093/qjmed/hcw004
Lavrentaki A, Paluzzi A, Wass JA, Karavitaki N (2017) Epidemiology of acromegaly: review of population studies. Pituitary 20(1):4–9. https://doi.org/10.1007/s11102-016-0754-x
Bollerslev J, Heck A, Olarescu NC (2019) Management of endocrine disease: individualized management of acromegaly. Eur J Endocrinol 1:19–0124. https://doi.org/10.1530/EJE-19-0124
Melmed S, Bronstein MD, Chanson P, Klibanski A, Casanueva FF, Wass JAH, Strasburger CJ, Luger A, Clemmons DR, Giustina A (2018) A consensus statement on acromegaly therapeutic outcomes. Nat Rev Endocrinol 14(9):552–561. https://doi.org/10.1038/s41574-018-0058-5
Mazziotti G, Frara S, Giustina A (2018) Pituitary diseases and bone. Endocr Rev 39(4):440–488. https://doi.org/10.1210/er.2018-00005
Cobb JR (1948) The American Academy of Orthopedic Surgeons Instructional Course Lectures, vol 5. Edwards, Ann Arbor, MI
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8(9):1137–1348. https://doi.org/10.1002/jbmr.5650080915
Schwab F, Ungar B, Blondel B, Buchowski J, Coe J, Deinlein D, DeWald C, Mehdian H, Shaffrey C, Tribus C, Lafage V (2012) Scoliosis research society—Schwab adult spinal deformity classification: a validation study. Spine 37(12):1077–1082. https://doi.org/10.1097/BRS.0b013e31823e15e2
Yang C, Yang M, Chen Y, Wei X, Ni H, Chen Z, Li J, Bai Y, Zhu X, Li M (2015) Radiographic parameters in adult degenerative scoliosis and different parameters between sagittal balanced and imbalanced ADS patients. Medicine 94(29):e1198. https://doi.org/10.1097/MD.0000000000001198
Losa M, Von Werder K (1997) Pathophysiology and clinical aspects of the ectopic GH-releasing hormone syndrome. Clin Endocrinol 47(2):123–135. https://doi.org/10.1046/j.1365-2265.1997.2311048.x
Banerjee A, Patel K, Wren AM (2003) Acromegaly—clinical manifestations and diagnosis. Pharm J 13:273–278
Melmed S (2006) Medical progress: acromegaly. N Engl J Med. 355(24):2558–2573. https://doi.org/10.1056/NEJMra062453
Nachtigall L, Delgado A, Swearingen B, Lee H, Zerikly R, Klibanski A (2008) Extensive clinical experience: changing patterns in diagnosis and therapy of acromegaly over two decades. J Clin Endocrinol Metab 93:2035–2041. https://doi.org/10.1210/jc.2007-2149
Trouillas J (2014) In search of prognostic classification of endocrine pituitary tumors. Endocr Pathol 25:124–132. https://doi.org/10.1007/s12022-014-9322-y
Lugo G, Pena L, Cordido F (2012) Clinical manifestations and diagnosis of acromegaly. Int J Endocrinol 2012:540398. https://doi.org/10.1155/2012/540398
Mercado M, Gonzalez B, Vargas G, Ramirez C, de los Monteros ALE, Sosa E, Jervis P, Roldan P, Mendoza V, López-Félix B, Guinto G, (2014) Successful mortality reduction and control of comorbidities in patients with acromegaly followed at a highly specialized multidisciplinary clinic. J Clin Endocrinol Metab 99(12):4438–4446. https://doi.org/10.1210/jc.2014-2670
Dreval AV, Trigolosova IV, Misnikova IV, Kovalyova YA, Tishenina RS, Barsukov IA, Vinogradova AV, Wolffenbuttel BH (2014) Prevalence of diabetes mellitus in patients with acromegaly. Endocr Connect 3(2):93–98. https://doi.org/10.1530/EC-14-0021
Collao A, Grasso LFS, Giustina A, Melmed S, Chanson P, Pereira AM, Pivonello R (2019) Acromegaly. Nat Rev Dis Primers 5(1):20. https://doi.org/10.1038/s41572-019-0071-6
Katznelson L, Laws ER Jr, Melmed S, Molitch ME, Murad MH, Utz A, Wass JA (2014) Acromegaly: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 99(11):933–3951. https://doi.org/10.1210/jc.2014-2700
Abu Dabrh AM, Mohammed K, Asi N, Farah WH, Wang Z, Farah MH, Prokop LJ, Katznelson L, Murad MH (2014) Surgical interventions and medical treatments in treatment-naïve patients with acromegaly. J Clin Endocrinol Metab 99(11):4003–4014. https://doi.org/10.1210/jc.2014-2900
Kasuki L, Marques NV, Nuez MJ, Leal VL, Chinen RN, Gadelha MR (2013) Acromegalic patients lost to follow-up: a pilot study. Pituitary 16(2):245–250. https://doi.org/10.1007/s11102-012-0412-x
Maione L, Brue T, Beckers A, Delemer B, Petrossians P, Borson-Chazot F, Chabre O, François P, Bertherat J, Cortet-Rudelli C, Chanson P (2017) French Acromegaly Registry Group. Changes in the management and comorbidities of acromegaly over three decades: the French Acromegaly Registry. Eur J Endocrinol 176(5), 645–655 Doi: 10.1530/EJE-16-1064.
Dalle Carbonare L, Micheletti V, Cosaro E, Valenti MT, Mottes M, Francia G, Davì MV (2018) Bone histomorphometry in acromegaly patients with fragility vertebral fractures. Pituitary 21:56–64. https://doi.org/10.1007/s11102-017-0847-1
Bonadonna S, Mazziotti G, Nuzzo M, Bianchi A, Fusco A, De Marinis L, Giustina A (2005) Increased prevalence of radiological spinal deformities in active acromegaly: a cross-sectional study in postmenopausal women. J Bone Miner Res 20(10):1837–1844. https://doi.org/10.1359/JBMR.050603
Mazziotti G, Bianchi A, Bonadonna S, Cimino V, Patelli I, Fusco A, Pontecorvi A, De Marinis L, Giustina A (2008) Prevalence of vertebral fractures in men with acromegaly. J Clin Endocrinol Metab 93(12):4649–4655. https://doi.org/10.1210/jc.2008-0791
Wassenaar MJ, Biermasz NR, Hamdy NA (2011) High prevalence of vertebral fractures despite normal bone mineral density in patients with long-term controlled acromegaly. Eur J Endocrinol 164(4):475–483. https://doi.org/10.1530/EJE-10-1005
Padova G, Borzì G, Incorvaia L, Siciliano G, Migliorino V, Vetri M, Tita P (2011) Prevalence of osteoporosis and vertebral fractures in acromegalic patients. Clin Cases Miner Bone Metab 8(3):37–43
Madeira M, Neto LV, de Paula Paranhos Neto F, Barbosa Lima IC, Carvalho de Mendonça LM, Gadelha MR, Fleiuss de Farias ML, (2013) Acromegaly has a negative influence on trabecular bone, but not on cortical bone, as assessed by high-resolution peripheral quantitative computed tomography. J Clin Endocrinol Metab 98(4):1734–1741. https://doi.org/10.1210/jc.2012-4073
Mazziotti G, Bianchi A, Porcelli T, Mormando M, Maffezzoni F, Cristiano A, Giampietro A, De Marinis L, Giustina A (2013) Vertebral fractures in patients with acromegaly: a 3-year prospective study. J Clin Endocrinol Metab 98(8):3402–3410. https://doi.org/10.1210/jc.2013-1460
Claessen KM, Kroon HM, Pereira AM, Appelman-Dijkstra NM, Verstegen MJ, Kloppenburg M, Hamdy NA, Biermasz NR (2013) Progression of vertebral fractures despite long-term biochemical control of acromegaly: a prospective follow-up study. J Clin Endocrinol Metab 98(12):4808–4815. https://doi.org/10.1210/jc.2013-2695
de Herder WW (2016) The history of acromegaly. Neuroendocrinology 103(1):7–17. https://doi.org/10.1159/000371808
AlDallal S (2018) Acromegaly: a challenging condition to diagnose. Int J Gen Med 11:337–343.
Chiloiro S, Mazziotti G, Giampietro A, Bianchi A, Frara S, Mormando M, Pontecorvi A, Giustina A, De Marinis L (2018) Effects of pegvisomant and somatostatin receptor ligands on incidence of vertebral fractures in patients with acromegaly. Pituitary 21(3):302–308. https://doi.org/10.1007/s11102-018-0873-7
Mammis A, Eloy JA, Liu JK (2010) Early descriptions of acromegaly and gigantism and their historical evolution as clinical entities. Neurosurg Focus 29(4):E1
Scarpa R, De Blasi D, Pivonello R, Marzullo P, Manguso F, Sodano A, Oriente P, Lombardi G, Colao A (2004) Acromegalic axial arthropathy: a clinical case–control study. J Clin Endocrinol Metab 89(2):598–603
Silva FE, Lenke LG (2010) Adult degenerative scoliosis: evaluation and management. Neurosurg Focus 28(3):E1. https://doi.org/10.3171/2010.7.FOCUS10160
Pratali R, Luz CO, Barsotti CEG, Santos FPE, Oliveira CEAS (2014) Analysis of sagittal balance and spinopelvic parameters in a brazilian population sample. Coluna/Columna 13(2):108–111. https://doi.org/10.1590/S1808-18512014130200399
Lopes AJ, da Silva DP, Kasuki L, Gadelha MR, Camilo GB, Guimarães FS (2014) Posture and balance control in patients with acromegaly: results of a cross-sectional study. Gait Posture 40(1):154–159. https://doi.org/10.1016/j.gaitpost.2014.03.014
Black DM, Arden NK, Palermo L, Pearson J, Cummings SR (1999) Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 14(5), 821–828 Doi: 10.1359/jbmr.1999.14.5.821.
Melton LJ, Atkinson EJ, Cooper C, O'Fallon WM, Riggs BL (1999) Vertebral fractures predict subsequent fractures. Osteoporos Int 10(3):214–221
Funding
No funding has been received for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest for this project.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The project was approved by the institution's Research Ethics Committee.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
de Azevedo Oliveira, B., Araujo, B., dos Santos, T.M. et al. The acromegalic spine: fractures, deformities and spinopelvic balance. Pituitary 22, 601–606 (2019). https://doi.org/10.1007/s11102-019-00991-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-019-00991-7