Abstract
Introduction
Spinal deformities present a common finding in patients affected with Marfan syndrome (MFS). More specifically, sagittal spine imbalances reflect the typical finding of such deformities. Observing spino-pelvic radiographs, we focused on eliciting any correlation between the pelvic incidence (PI), sacral slope (SS) and thoracolumbar kyphosis measurements, and categorising them according to a sagittal spinal classification system.
Materials and methods
One hundred seventy patient records were found over a 6 year period, and further refined to incorporate a total of 44 patients. 25 males and 19 females with an average age of 20 years at imaging. Electronic and hard copies of radiographs were used and measurements were made with virtual Cobb meters, rulers and protractors.
Results
The mean PI was significantly different between type-I (46°) and type-II spines (35°) (p = 0.04), and the values for each class were as follows: type IA—53°, type IB—44°, type IC—36°, type IIA—42°, and type IIB—34°. Type II spines had a lower PI compared to type IA spines (p = 0.037) and to that of an unaffected population. Statistically significant differences were noted in SS between groups (t test; p < 0.001), and ANOVA demonstrated that the largest differences between spinal classes were found in SS.
Conclusion
In our study, PI values were much higher in type I compared to type II spines. Type II spines had PI values as expected, however, had higher than expected SS values. SS followed a down trending pattern across all spinal classes. Type IIA spines had a much greater preponderance for male patients. Overall, we wish to highlight in particular that type II spines were associated with a much lower PI and SS, and report these differences in pelvic morphology and sagittal spine patterns seen in MFS patients. The pelvic tilt and sacral slope parameters observed in our Type II spines may further reflect and characterize the deformity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Marfan Syndrome (MFS) is an autosomal dominant condition that affects 1 in 5000 people. The mutation involved affects the formation of connective tissue [1], an essential component found ubiquitously in and around most structures of the human body, and most commonly comprising the cardiovascular, musculoskeletal systems as well as the eyes [2, 3].
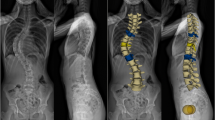
Focusing on the spine, abnormal curvatures both in the sagittal and coronal (scoliosis) planes are seen in more than 60% of MFS patients [4,5,6]. Moreover, precise morphological changes to the vertebrae as part of this condition have been described by Demetracopoulos and Sponseller [7], and included increased vertebral scalloping, a higher prevalence of lumbosacral transitional vertebrae, lengthened transverse process distance, and a reduction in pedicle width and laminar thickness. Regarding the classification of curvatures, previous studies have focused on criteria that differentiate according to, for example, the presence or absence of negative values for intervertebral sagittal rotation [8], typical versus atypical patterns based on a review that focused on common orientations seen in an adolescent idiopathic scoliosis control group [9], and finally via type I and type II spines. The latter were defined according to the kyphosis-lordosis vertebral level of transition, being further subdivided into A, B and C in line with the degree of sagittal curvature seen in these areas (Fig. 1), and this is the classification system which we chose to use when analyzing our radiographs.
Sagittal spinal classification system based on the transition of the kypholordotic junction. Type-I spine = the transition between the kyphosis and the lordosis is situated at the level of the second lumbar vertebra or higher. 1A normal kyphosis (20–50° [Avg. 35°]) and lordosis (20–80° [Avg. 60°]). 1B kyphosis of less than 20°. 1C kyphosis which exceeds 50°. Type-II spine the transition is situated below the level of the second lumbar vertebra. 2A an extensive (longer) kyphosis which involves the thoracolumbar junction. 2B an inversion of the spinal curvature with a thoracic lordosis, thoracolumbar kyphosis and a low-set lumbar lordosis
The specific aim of our study was to further delineate the imbalances seen in the sagittal spinal curvature, since this relates to the more representative population of MFS patients. We compared these values with their corresponding pelvic parameters to highlight any correlated patterns that may have occurred between these variables, with a view to elucidating any associations between pelvic parameters and sagittal curvatures of the thoracic and lumbar spine. To date, the most comprehensive study published on the topic was by Loubresse et al. [10], which demonstrated that MFS patients had lower pelvic incidence (PI) values, a strong positive correlation between PI and sacral slope (SS), and statistically significant differences in PI values between the type I and II spines [definitions in Fig. 1]. They demonstrated that type I spines were associated with much higher PI and lower SS values which resulted in a significantly more retroverted pelvis with minimal capacity for the lumbar spine to maintain sagittal balance. We built upon this study by restricting our patients to those with scoliosis measurements of < 40º, again because we felt that this represented the more typical population of MFS patients.
Patients and methods
We reviewed sagittal spine radiographs of MFS patients over a 6 year period. 170 patients were studied, and the following exclusion criteria applied: (1) patients with lateral scoliosis measurements of > 40º, (2) whether or not landmarks were visible on the quality of available radiographs (e.g. only post-op scans with hardware in-situ being available, femoral heads absent from the field of view/obscured from under-penetrated images). This left 44 appropriate for study; 25 males and 19 females, with an average age of 20 ± 14 years at imaging. Electronic as well as hard copies of radiographs were used as available. The electronic radiographs were analyzed and viewed using medical imaging software (Ultravisual—Wisconsin, USA), which allowed us to make accurate measurements with virtual cobb meters as well as rulers/protractors used to calculate spinal and pelvic parameters, respectively. The same method was employed for the hard copies of radiographs using a physical Cobb angle protractor.
We classified patients according to a previously described sagittal spinal classification system. Pelvic parameters (PI, pelvic tilt (PT) and SS) and spinal parameters (thoracic kyphosis, lumbar lordosis and thoracolumbar kyphosis) were measured in the sagittal plane (Fig. 2), and we looked for any correlations/patterns between these sets of measurements, as well as with other documented variables including age, gender and height [11]. ‘Expected’ PI, SS and PT values were calculated using the following equation: PI = PT + SS. We also compared our values with that of an unaffected population. Spinal and pelvic parameters for an unaffected population in this instance have been derived from studies conducted on Western populations [12,13,14], including that by Loubresse et al. Some juveniles and young adolescents whose deformities are still evolving may have also been included in our patient population, and it would be prudent for readers to be cognizant of this (Fig. 3).
Illustration demonstrating pelvic incidence, pelvic tilt and sacral slope angles on a sagittal radiograph. Pelvic Incidence—angle between center of sacrum (right angle) and center of femoral head (also calculated via = PT + SS). Pelvic Tilt—angle between center of femoral head (right angle) and center of sacrum. Sacral Slope—angle between superior endplate of sacrum and a horizontal line
Demonstrating differences in pelvic parameters between A type-IA patients and B II-A patients. These differences in pelvic positioning may contribute to the overall sagittal spinal imbalances observed (A kypholordotic transition at the L1 vertebra in type-IA and B kypholordotic transition at the L3 vertebra in type-IIA)
Statistical analysis
Independent-student t tests and a one-way analysis of variance were performed to assess for differences primarily in radiographic pelvic parameters between groups. All spinal and pelvic measurements were carried out by two independent observers; SS and AM. Bland–Altman analysis was performed to assess for levels of agreement between results collected by both observers [Graph 1, Table 1].
Results
Overall, the number of patients comprising each sagittal spine class were as follows; 16 as type IA (36.3%), 7 as type IB (15.9%), 9 as type IC (20.5%), 9 as type IIA (20.5%) and 3 as type IIB (6.8%). The distribution for all of our collected results for pelvic and spinal parameters is displayed in Graph 2.
The mean PI was significantly different between type-I (46°) and type-II spines (35°) (p = 0.04).
The mean PI values for each sagittal spine class were as follows: type IA—53° (SD 15.0, 95% CI 45–60), type IB—44° (SD 16.0, 95% CI 30–54), type IC—36° (SD 18.9, 95% CI 24–48), type IIA—42° (SD 14.6, 95% CI—30–49), and type IIB—34° (SD 20.5, 95% CI 12–59) (p = 0.040) [Table 2].
Overall, for the study group of 44 patients, the mean PI was 45° (SD 16.7, 95% CI 15–88), mean PT was 11.8° (SD 12.2, 95% CI − 16–45) and mean SS was 35.3° (SD 12.3, 95% CI 3–59). The mean thoracic kyphosis was 42.9° (SD 19.2, 95% CI 11–90) and mean lumbar lordosis was 44.8° (SD 13.5, 95% CI 16–79).
Post hoc analysis demonstrated that type II spines had a lower PI compared to type IA and IB spines (p = 0.037). Another pattern that emerged was that PI values decreased chronologically moving from type I to type II spines; from 53 to 34° [Table 2].
There was a statistically significant difference noted in SS between groups (independent student t test; p < 0.001), and one-way analysis of variance (ANOVA) demonstrated that the largest differences between spinal classes were found in this pelvic parameter in particular [Table 3]. More specifically, the differences were between type IIA and IA (p < 0.001), IIA and IB (p = 0.016), and IIA and IC (p = 0.018) spines [Table 4]. There was no significant difference in PT between groups (p = 0.187). With regards to comparison of our results to that of an unaffected population, thoracic kyphosis measurements were closest to MFS patients with type IA or IIB spines, while lumbar lordosis measurements were closest to those with type IA and IC spines. PI, SS and PT values of type IA spines were the closest to resemble that of an unaffected population.
When observing for associations between these variables, the following were found: a strong positive correlation between SS and lumbar lordosis (Pearson’s correlation coefficient (PCC) = 0.8, p = < 0.0001) [Graph 3]. Other positive correlations were found between PI and SS (PCC = 0.5, p = 0.0003), PI and PT (PCC = 0.5, p = 0.0003), and PI and lumbar lordosis (PCC = 0.3, p = 0.023). A negative correlation existed between PT and lumbar lordosis (PCC = 0.3, p = 0.04).
Further analysis of our data revealed that type IIA spines demonstrated a considerably greater preponderance for males over females (M:F ratio = 8:1). The mean age for type I and II spines at the time of imaging was between 16 and 18 years, but class IC stood out at 26.9 years. There was no significant correlation between the height of patients (measured from the midpoint of the sacral end plate to the midpoint of the superior end plate of T1 vertebra) and PI (PCC = − 0.2, p = 0.3). Lastly, Bland Altman analysis of inter-observer reliability between both of our observers’ measurements revealed that > 95% of our recorded values were contained within upper and lower limits of agreement, revealing reliability in the measurement of our parameters.
Discussion
We have demonstrated how the position of the pelvis is related to the sagittal curvatures of the spine in patients with MFS. Specifically, type-II spines were associated with a significantly lower pelvic incidence and sacral slope compared to type-I spines, as well as to an unaffected population. While pelvic incidence remains a fixed primary parameter, sacral slop and pelvic tilt are dynamic parameters which vary in inverse relationship to each other, to accommodate for postural changes and extra-pelvic factors such as muscle weakness and contracture, as an adaptive response. Furthermore, perhaps the syndrome’s effect on connective tissue may facilitate spino-pelvic changes even with minor misalignments in either/or parameter, and especially so during growth phases.
The study by Loubresse et al. demonstrated the following—MFS patients had lower PI values, constituting a more retroverted pelvis, a strong positive correlation between PI and SS, and statistically significant differences in PI values between type I and II spines. They demonstrated that type I spines were associated with much higher PI and lower than expected SS values which resulted in a significantly more retroverted pelvis with minimal capacity for the lumbar spine to maintain sagittal balance. Our study’s findings also found that MFS patients had lower PI values, however, that this was most pronounced in those with type II spines. Similarly, we also found a positive correlation between PI and SS. Interestingly, whereas Loubresse et al. found statistically significant differences in PI between type I and II spines, we found statistically significant differences in SS (as well as in lumbar lordosis and thoracic kyphosis) between the two groups. Thus, we postulate that perhaps it is the sacral slope angle (rather than/in addition to PI) that initially adapts to the change in kypholordotic transition point in these patients, and thus explains the spino-pelvic parameters seen in this group of patients. These differences in SS were also more specifically between type IIA and IA (p < 0.001), IIA and IB (p = 0.016), and IIA and IC (p = 0.018) spines [Table 4], further supporting the notion that perhaps it is the size of the SS that adapts to the initial development of the kypholordotic junction beneath the level of the second lumbar vertebra. Our observations reveal that such changes can then go on to cause an extensive thoracolumbar kyphosis or an inversion of the spinal curvatures with a thoracic lordosis, thoracolumbar kyphosis and a low-set lumbar lordosis in type II spines. This hypothesis is further supported by our findings of a very strong statistically significant positive correlation between SS and lumbar lordosis, which Loubresse et al. also found in their results. They, however, even went on as far as to suggest that this correlation could explain the morphology of the thoracic spine in type IA, B and C patients.
We did not have the same level of difference between our PI and corresponding SS values in each spinal class when compared to Loubresse et al. suggesting that our patients had a lesser degree of pelvic retroversion. This in turn does not seem to explain the reason behind our patients’ lumbar spinal imbalances. Our findings of significantly lower PI and SS values in type II compared to type I spines, however, could also support the idea that it is in fact both of these pelvic parameters that adapt to not only the adolescent transition point of the kypholordotic junction, but also to the thoracic and kyphotic spinal changes seen in these patients. This is further supported by their direct relationship to one another (PI = SS + PT), the latter two variables being inversely related. Our measurements for lumbar lordosis did not display any sort of association with thoracic kyphosis, perhaps suggesting that one does not influence the other. These patterns did, however, mirror those found by Loubresse et al.
Conclusion
In our study, PI values were higher in type I compared to type II spines, and type IA had the same average PI as an unaffected population. SS overall followed a down trending pattern across the classes; however, our data revealed that type II spines still had a higher than expected SS, which we have previously suggested could be an adaptive response to the lower kypholordotic transition point in these patients. Lastly, it was interesting to note that type IIA spines had a much greater preponderance for male patients, considering MFS usually has an equal predilection for males and females. It is also this class of patients that typically develops the extensive thoracolumbar kyphosis.
Overall, we wish to highlight in particular that type II spines were associated with a lower pelvic incidence and sacral slope, and report these differences in pelvic morphology and sagittal spine patterns seen in MFS patients. The pelvic tilt and sacral slope parameters observed in our Type II spines may further reflect and characterize the deformity. Overall, the correlated patterns from our study will provide valuable information when evaluating MFS patients with spinal pathology. The hope is that such measurements will lead to better understanding of spino-pelvic development.
Key points
-
Pelvic incidence was much higher in type I compared to type II spines.
-
Type II spines were associated with a lower pelvic incidence and sacral slope compared to type I spines.
-
Type IIA spines had a much greater preponderance for male patients.
-
Sacral slope followed a down trending pattern across the spinal classes.
Data availability
All patient identifier information was removed from radiographs prior to analysis. This includes both electronic and physical radiographs.
References
Dietz H, Cutting GR, Pyeritz RE et al (1991) Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature 352:337–339
Kainulainen K, Karttunen L, Puhakka L et al (1994) Mutations in the fibrillin gene responsible for dominant ectopia lentis and neonatal Marfan syndrome. Nat Genet 6(1):64–69
Erkula G, Jones KB, Sponseller PD et al (2002) Growth and maturation in Marfan syndrome. Am J Med Genet 109:100–115
Sponseller PD, Hobbs W, Riley LH 3rd et al (1995) The thoracolumbar spine in Marfan syndrome. J Bone Joint Surg (American) 77(6):867–876
Robbins PR, Moe JH, Winter RB (1975) Scoliosis in Marfan’s syndrome: its characteristics and results of treatment in thirty-five patients. J Bone Joint Surg 57:358–368
Tallroth K, Malmivaara A, Laitinen ML et al (1995) Lumbar spine in Marfan syndrome. Skeletal Radiol 24:337–340
Demetracopoulos CA, Sponseller PD (2007) Spinal deformities in Marfan syndrome. Orthop Clin North Am 38(4):563–572
Glard Y, Pomero V, Collignon P et al (2008) Sagittal balance in scoliosis associated with Marfan syndrome: a stereoradiographic three-dimensional analysis. J Child Orthop 2(2):113–118
Spiegel DA, Flynn JM, Stasikelis PJ et al (2003) Scoliotic curve patterns in patients with Chiari I malformation and/or syringomyelia. Spine J (American) 28(18):2139–2146
Loubresse CG, Mullins M, Moura B et al (2006) Spinal and pelvic parameters in Marfan’s syndrome and their relevance to surgical planning. J Bone Joint Surg 88(4):515–519
Labelle H, Roussly P, Berthonnaud E et al (2005) The importance of spino-pelvic balance in L5–S1 developmental spondylolysthesis: a review of pertinent radiologic measurements. Spine 30(6):27–34
Jentzsch T, Geiger J, Bouaicha S et al (2013) Increased pelvic incidence may lead to arthritis and sagittal orientation of the facet joints at the lower lumbar spine. BMC Med Imaging 5(13):34
Vrtovec T, Janssen MM, Pernuš F et al (2012) Analysis of pelvic incidence from 3-dimensional images of a normal population. North Am Spine J 37(8):479–485
Legaye J, Duval-Beaupère G, Hecquet J et al (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103
Funding
This study did not require funding.
Author information
Authors and Affiliations
Contributions
SJS—made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work;—drafted the work or revised it critically for important intellectual content;—approved the version to be published; and—agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. AM—made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work;—drafted the work or revised it critically for important intellectual content;—approved the version to be published; and—agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. PDS—made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work;—drafted the work or revised it critically for important intellectual content;—approved the version to be published; and—agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This is a retrospective radiological study. Ethical approval was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Suresh, S.J., Margalit, A. & Sponseller, P.D. Evaluating the sagittal spinal and pelvic parameters in Marfan syndrome patients affected by scoliosis. Spine Deform 10, 873–881 (2022). https://doi.org/10.1007/s43390-022-00484-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00484-x