Abstract
Background Dexmedetomidine, an α2-receptor agonist, provides potent sedation, analgesia, and anxiolysis without respiratory depression and is used in a variety of surgical and procedural situations. Aim of the review The aim of this study was to estimate the incidence of bradycardia in pediatric patients who received dexmedetomidine as a sole agent for any procedural, intensive care or surgical sedation. Method Literature was searched in electronic databases and studies were selected by following pre-determined eligibility criteria. Meta-analyses were carried out by pooling the percent incidence of bradycardia to attain a weighted overall effect size. Age-wise subgroup analyses and meta-regression analyses for the identification of factors affecting the incidence were also performed. Results Data of 2835 patients from 21 studies were included. The mean age was 62.21 ± 35.68 months. Initial, maintenance and total doses of dexmedetomidine (mean ± standard deviation) were 1.63 ± 0.33 μg/kg body weight, 0.86 ± 0.68 μg/kg/h, and 26.7 ± 20.8 μg/kg. The overall incidence of bradycardia (95% confidence interval) was 3.067 (2.863, 3.270)%; P < 0.0001. However, range was wider (0–22%) with 9 studies observed 0% incidence. The mean change in the heart rate was −17.26 (−21.60, −12.92); P < 0.00001. In the meta-regression analyses, age, body weight and dexmedetomidine dose were not significantly associated with the incidence of bradycardia. The minimum heart rate observed during the dexmedetomidine treatment period was positively associated with baseline heart rate. Conclusion Incidence of bradycardia in dexmedetomidine treated pediatric patients is 3%.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Impacts on practice
-
In pediatric patients treated with dexmedetomidine, a 3% incidence of bradycardia can be expected.
-
Age, body weight, gender, dexmedetomidine dosage and route of administration do not significantly affect the incidence of bradycardia as side-effect in children.
-
Minimum heart rate during sedation with dexmedetomidine has a positive association with the baseline heart rate.
Introduction
Dexmedetomidine is a highly selective agonist to transmembrane G protein coupled central α2-receptors. It provides potent sedation, analgesia, and anxiolysis by decreasing central nervous system sympathetic output. Dexmedetomidine administration is also associated with decrease in blood pressure and heart rate without respiratory depression [1–3]. Sleep electroencephalographic evaluations show that dexmedetomidine sedation resembles S2 sleep in humans [4]. These properties make it a suitable option for sedation in the intensive care unit (ICU) and in a variety of surgical and procedural situations. Opioid-sparing effects of dexmedetomidine further increase the spectrum of its utility [5].
The sedative and anxiolytic effects of dexmedetomidine result primarily from its activity in the locus ceruleus of brainstem where it reduces central sympathetic output, resulting in increased firing of inhibitory neurons [6]. Dexmedetomidine hyperpolarizes the neuronal membranes of dorsal horn of the spinal cord by the activation of G-protein coupled K+ channels to produce antinociceptive effects [7]. It has far higher affinity for α2 receptors than clonidine (widely used α2-adrenoceptor analogue), and has a shorter half-life (2–3 h) than clonidine (12–24 h) [8].
In pediatric patients, the use of dexmedetomidine is limited at present and its efficacy and safety is not fully established [9]. Available data suggests that the use of dexmedetomidine provides better hemodynamic stability, opioid and benzodiazepine sparing effects and increased comfort [10–12] and has also been found to be a useful sedative in pediatric burn patients [13, 14]. However, in clinical studies, the incidence of bradycardia with the use of dexmedetomidine is reported with a wide range with many studies found zero incidence [15–18], even with relatively higher doses [19], and others have reported higher incidence of up to 22% [20, 21]. This has necessitated to examine this variability in the incidence of bradycardia in studies which utilized dexmedetomidine anesthesia in pediatric patients as this area is not previously reviewed.
Aim of the review
The aim of this study was to systematically review the relevant studies which utilized dexmedetomidine as a sole anesthetic in pediatric populations and measured heart rate and the incidence of bradycardia periodically throughout the study, and to carry out a pooled analysis of the incidence bradycardia and change in the heart rate during the study reported in these studies.
Method
This study was performed by following PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [22]. Important features of method are presented in Table 1.
Relevant research articles were retrieved from electronic databases after a systematic literature search by using several combinations of primary and secondary key terms/phrases. Final selection of the studies for meta-analysis was based on eligibility criteria mentioned in Table 1. Outcome measures for the present study were: (1) incidence of bradycardia; (2) HR change during the study period; and (3) minimum HR during the study. Definition of ‘pediatric patients’ was borrowed from the American Academy of Pediatrics which defines pediatric patients, i.e. young humans of day 1–21 years of age.
For the meta-analysis, percent incidence values were either extracted raw from research articles or calculated from the numerical data provided in the articles and then were used in a pooled analysis to have inverse variance weighted overall estimate as well as subgroup estimates under random-effects model. Stata software (version 12 SE; Stata Corporation, Texas, US) was used for meta-analysis. Changes in HR were calculated from minimum HR during the study and baseline values. The meta-analysis of HR change was carried out by using RevMan (version 5.3; Cochrane Collaboration) software.
In the metaregression analyses, outcome variables (incidence of bradycardia, and minimum heart rate during the study) were tested against several explanatory variables including sample size, age, body weight, gender, initial or maintenance dose, total dosage, and baseline HR. Restricted maximum likelihood method was used in the meta-regression analyses. Metaregression analyses were also performed with Stata software.
Results
Twenty-one studies [15–21, 23–36] were included in this meta-analysis (Fig. 1). After identifying 212 potential abstracts, 54 were selected for full-text article retrieval and of these 21 articles were used for data extraction. At study selection stage, 33 studies were excluded because either the studies used dexmedetomidine in combination with other anesthetic/s; or the studies investigated hemodynamic effects but did not report the incidence of bradycardia or change in HR; or were the case reports.
Of the included studies, 8 were the randomized controlled trials (RCTs), 2 were prospective non-RCTs, and 11 studies involved retrospective analyses. Twelve of these studies utilized dexmedetomidine anesthesia for radiological, endoscopic and electrophysiological diagnosis, 2 for surgery, 2 for dentistry procedures, 2 for burn patients’ sedation, 2 for ICU sedation and 1 for intubation purposes. Route of dexmedetomidine administration was intravenous (IV) in 15 studies, intramuscular (IM) in 4 and intranasal (IN) in 3 studies (one study investigated both IN and IM routes).
From the included studies, data of 2835 patients (age: 62.21 ± 35.68 months; weight 22.36 ± 10.5 kilograms and 58.4 ± 13.3% males) were used in this meta-analysis. Initial, maintenance and total doses of dexmedetomidine as mean ± standard deviation (range) used in these studies were 1.63 ± 0.33 (0.4–4) µg/kg body weight, 0.86 ± 0.68 (0.4–2) µg/kg/h and 26.7 ± 20.8 (0.36–98.6) µg/kg, respectively. In these patients, 13.36 ± 12.57% received rescue anesthesia after dexmedetomidine’s failure to achieve adequate anesthesia (14 studies data).
Overall, the incidence of bradycardia achieved a statistical significance. Random effects meta-analysis revealed that the percent incidence of bradycardia (95% confidence interval) in this sample of patients was 3.067 (2.863–3.270)%; P < 0.00001 (Fig. 2). Incidence of bradycardia in various subgroups with regards to study design and age are presented in Table 2.
A forest graph showing the results of a meta-analysis of the percent incidence of bradycardia in the included studies and age-wise subgroup analysis. Dash line represents overall effect size. In the study identities, Mason 2011 (A, MRI and B, CT groups), and Tammam and Wahba [20] (A, IV and B, IM routes of administration)
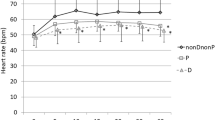
A pooled analysis of the studies which measured baseline heart rate and periodic heart rate during the study revealed that dexmedetomidine anesthesia was associated with a decrease in the heart rate of −17.26 [−21.60, −12.92]; P < 0.00001 beats per minute during the study (Fig. 3). Baseline heart rate was 103.66 (101.30, 106.02) beats per minute in this population of pediatric patients. Mean change in heart rate during dexmedetomidine treatment in three age groups of this pediatric population are given in Table 3.
Forest graph showing the results of the meta-analysis of mean change in heart rate during the dexmedetomidine treatment and age-wise subgroup analysis. In studies identities, Ahmed 2015 (A, 1 bolus and B, 2 boluses of initial doses), and Tammam and Wahba [20] (A, IV and B, IM routes of administration)
Nine of the included studies observed 0% incidence of bradycardia. In these studies, average initial dose of dexmedetomidine was 1.35 ± 0.62 µg/kg, maintenance dose was 0.82 ± 0.66 µg/kg/h and the total dose used was 7.12 ± 10.29 µg/kg. Mean change in the heart rate during the study duration in these studies was −8.92 [−15.32, −2.52]. Meta-regression analysis with all included studies did not identify a significant relationship between initial, or maintenance, or total dose of dexmedetomidine with either incidence of bradycardia or mean change in heart rate during sedation.
In the meta-regression analyses (Table 4), incidence of bradycardia was not significantly associated with sample size, age, body weight, initial or maintenance dose, total dosage, or baseline heart rate. Minimal heart rate during the study was positively associated with baseline heart rate (coefficient: 1.34; P = 0.002) but inversely associated with percentage of females (coefficient: −5.2; P = 0.016). However, in multivariate metaregression analysis with percentage of females and baseline heart rate as explanatory variables, female gender was not significantly associated with minimum HR during the study.
Discussion
We have found that the incidence of bradycardia in children sedated with dexmedetomidine ranged from 0 to 22% to average at 3% in a population in which heart rate decreased to about 17 beats per minute on average during the study. In this population, about 13% patients required rescue medication. Dexmedetomidine use ranged from diagnostic procedures to ICU and burn sedation and three routes of administration were utilized.
Whereas, in adults, low doses of dexmedetomidine are reported to be effective, in pediatric patients relatively higher doses are required to achieve satisfactory sedation and doses up to 2 μ/kg/h are reported to be safe and well-tolerated [21]. Our meta-regression analyses could not find a significant relationship between dexmedetomidine dose and incidence of bradycardia. Indeed, incidence of bradycardia has been reported with as low as 0.3 µg/kg/h dose [37] and other authors have also suggested that the bradycardia incidence does not appear to be dexmedetomidine dose-dependent [38].
The most common route of dexmedetomidine administration is IV but IM and IN are also found to exhibit comparable effectiveness in some conditions [18, 32, 33, 39]. Incidence of bradycardia was about 5% in studies which used IV route, 2% with IM route and 0% with IN route in this meta-analysis. However, studies with IN route were comparatively less and thus more data will be required to refine this synthesis.
In the present study, we have found that minimum HR during dexmedetomidine sedation had a positive association with the baseline HR. Baseline HR is an important prognostic factor in many conditions requiring anesthesia e.g. baseline HR variability has been reported to predict future hemodynamic events under general anesthesia that can be used to identify high risk cardiovascular patients [40]. In patients with a variety of conditions, under spinal or epidural anesthesia, baseline HR has been found to predict the incidence of severe bradycardia [41, 42].
In the present study, female gender also had an independent significantly inverse association with minimum HR during the study. However, female gender was also inversely correlated with baseline heart rate (correlation coefficient: −0.634; P = 0.025). Therefore, we performed multivariate metaregression analyses. After adjusting for baseline HR, female gender was not significantly associated with minimal HR during the study. While studying 57,240 spinal or epidural anesthesia records, it was found that the incidence of bradycardia was 10.2% and among others male gender was identified as a significant risk factor for the incidence of bradycardia [42].
Dexmedetomidine causes bradycardia by the activation of neurons in the medullary vasomotor center, reducing norepinephrine and resultant central sympatholytic effects in the form of decreased heart rate and/or blood pressure [8]. However, bradycardia and hypotension does not always occur simultaneously [21] and bradycardia is not associated with the clinical signs of cardiovascular compromise may not need any treatment [32]. Indeed, treatment of bradycardia with glycopyrrolate to normotensive children is reported to cause hypertensive episode [43], which otherwise could be beneficial to bradycardiac hypotensive children [23].
Use of dexmedetomidine is required to be made with caution in hemodynamically unstable patients. Patients receiving cardiac drugs such as stimulants, β-blockers, and antiarrhythmics may also enhance the risk of dexmedetomidine induced bradycardia [16]. Berkenbosch et al. [44] reported a case of an infant receiving digoxin who developed bradycardia upon dexmedetomidine sedation. Combinational use of dexmedetomidine e.g. with ketamine is suggested as a strategy to reduce the chances of hemodynamic effects [8]. Al-Taher et al. [24] speculated that no incidence of bradycardia in their study may be attributed to the premedication with atropine sulphate.
Whereas, dexmedetomidine may pose potentially adverse effects on the cardiovascular system, especially in hemodynamically unstable patients, this can be fruitful if used perioperatively for tachyarrhythmias in pediatric patients with heart conditions [45–47]. Hammer et al. [16] in an electrophysiological evaluation study have reported that dexmedetomidine depressed sinus and atrioventricular nodal function in children. However, it is not clear whether the dexmedetomidine’s potential antiarrhythmic effects are due to a direct action on the heart’s conduction system, or the result of decreasing plasma catecholamines, or due to its sympatholytic and sympathomimetic effects on CNS, or due to more than one aforementioned mechanisms [25].
Tramer et al. [48] have shown that propofol sedation is associated with increased risk of bradycardia after analyzing data from 1200 young and adult patients from 17 randomized controlled trials. Furthermore, data from over 250 published or monitoring reports indicated that risk of mortality from propofol-induced bradycardia is 1.4 per 100,000 patients [48]. In a review of 209 children with Down syndrome, it was noticed that incidence of bradycardia was common during sevoflurane anesthesia [49]. Although, fentanyl and remifentanil are also reported to cause bradycardia occasionally [50–52], the potential for causing bradycardia is not reviewed for these anesthetics.
Thus, with regards to the incidence of bradycardia, use of dexmedetomidine anesthesia appears to be safer and manageable as no mortality was reported in the included studies of this meta-analysis. Nevertheless, caution should be made with younger children especially with cardiovascular conditions. Combinational use of dexmedetomidine with other suitable anesthetics can also be a fruitful strategy in hemodynamically unstable or cardiovascular patients.
Among the limitations of the present study, high statistical heterogeneity may be attributed to methodological and clinical heterogeneity. Patients with a variety of conditions and requirements are included owing to the less availability of studies with controlled and comparative designs. Another source of high heterogeneity could be traced from the range of total dose which was considerably large between the studies and might had also influenced the overall incidence of bradycardia. Lesser data were available with regards to the duration of anesthesia or the timing of bradycardia incidence which otherwise could help in the prognosis assessment. Thus, future studies with more homogeneous data can confirm these findings. To include studies with 0% incidence of bradycardia, a value of 0.001% instead of 0% was used to meta-analyze all the included studies owing to the statistical software requirement. This may also have minor effect on the weight distribution of all studies.
Conclusion
Bradycardia is an important side effect of many anesthetics. Use of dexmedetomidine is increasing in clinical practice and investigations. Incidence of the bradycardia in the pediatric patients receiving dexmedetomidine as a sole sedative is estimated at 3%, although between-study variation is high. Moreover, dexmedetomidine treatment is associated with decrease in heart rate of about 17 beats per minute. Among the prognostic factors, baseline heart rate is identified as the determinants of minimum heart rate but not bradycardia incidence during dexmedetomidine treatment. More randomized data is required for the refinement of these outcomes, however.
References
Buck ML. Dexmedetomidine Use in Pediatric Intensive Care and Procedural Sedation. J Pediatr Pharmacol Ther. 2010;15(1):17–29.
Hoy SM, Keating GM. Dexmedetomidine: a review of its use for sedation in mechanically ventilated patients in an intensive care setting and for procedural sedation. Drugs. 2011;71(11):1481–501.
Mantz J, Josserand J, Hamada S. Dexmedetomidine: new insights. Eur J Anaesthesiol. 2011;28(1):3–6.
Huupponen E, Maksimow A, Lapinlampi P, Sarkela M, Saastamoinen A, Snapir A, Scheinin H, Scheinin M, Merilainen P, Himanen SL, Jaaskelainen S. Electroencephalogram spindle activity during dexmedetomidine sedation and physiological sleep. Acta Anaesthesiol Scand. 2008;52(2):289–94.
Christensen A. Update on dexmedetomidine for adult ICU sedation. Conn Med. 2009;73(8):469–72.
Kim KH. Safe sedation and hypnosis using dexmedetomidine for minimally invasive spine surgery in a prone position. Korean J Pain. 2014;27(4):313–20.
Ishii H, Kohno T, Yamakura T, Ikoma M, Baba H. Action of dexmedetomidine on the substantia gelatinosa neurons of the rat spinal cord. Eur J Neurosci. 2008;27(12):3182–90.
Tobias JD. Dexmedetomidine: Applications in pediatric critical care and pediatric anesthesiology. Pediatr Crit Care Med. 2007;8(2):115–31.
Plambech MZ, Afshari A. Dexmedetomidine in the pediatric population: a review. Minerva Anestesiol. 2015;81(3):320–32.
Whalen LD, Di Gennaro JL, Irby GA, Yanay O, Zimmerman JJ. Long-term dexmedetomidine use and safety profile among critically ill children and neonates. Pediatr Crit Care Med. 2014;15(8):706–14.
Gupta P, Whiteside W, Sabati A, Tesoro TM, Gossett JM, Tobias JD, Roth SJ. Safety and efficacy of prolonged dexmedetomidine use in critically ill children with heart disease. Pediatr Crit Care Med. 2012;13(6):660–6.
Lam F, Ransom C, Gossett JM, Kelkhoff A, Seib PM, Schmitz ML, Bryant JC, Frazier EA, Gupta P. Safety and efficacy of dexmedetomidine in children with heart failure. Pediatr Cardiol. 2013;34(4):835–41.
Walker J, Maccallum M, Fischer C, Kopcha R, Saylors R, McCall J. Sedation using dexmedetomidine in pediatric burn patients. J Burn Care Res. 2006;27(2):206–10.
Sheridan RL, Keaney T, Shank E, Cascia G, Martyn JAJ, Weber J. Dexmedetomidine infusion in pediatric burns. J Burn Care Res. 2007;28:S49–186.
Ergul Y, Unsal S, Ozyilmaz I, Ozturk E, Carus H, Guzeltas A. Electrocardiographic and electrophysiologic effects of dexmedetomidine on children. Pacing Clin Electrophysiol. 2015;38(6):682–7.
Hammer GB, Drover DR, Cao H, Jackson E, Williams GD, Ramamoorthy C, Van Hare GF, Niksch A, Dubin AM. The effects of dexmedetomidine on cardiac electrophysiology in children. Anesth Analg. 2008;106(1):79–83.
Koroglu A, Demirbilek S, Teksan H, Sagir O, But AK, Ersoy MO. Sedative, haemodynamic and respiratory effects of dexmedetomidine in children undergoing magnetic resonance imaging examination: preliminary results. Br J Anaesth. 2005;94(6):821–4.
Mason KP, Lubisch NB, Robinson F, Roskos R. Intramuscular dexmedetomidine sedation for pediatric MRI and CT. AJR Am J Roentgenol. 2011;197(3):720–5.
Hasanin AS, Sirab AM. Dexmedetomidine versus propofol for sedation during gastrointestinal endoscopy in pediatric patients. Egypt J Anaesth. 2014;30(1):21–6.
Tammam TF, Wahba SS. Quality of MRI pediatric sedation: comparison between intramuscular and intravenous dexmedetomidine. Egypt J Anaesth. 2013;29(1):47–52.
Mason KP, Zurakowski D, Zgleszewski SE, Robson CD, Carrier M, Hickey PR, Dinardo JA. High dose dexmedetomidine as the sole sedative for pediatric MRI. Paediatr Anaesth. 2008;18(5):403–11.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009. doi:10.1371/journal.pmed.1000097.
Ahmed SS, Unland T, Slaven JE, Nitu ME. High dose dexmedetomidine: effective as a sole agent sedation for children undergoing MRI. Int J Pediatr. 2015. doi:10.1155/2015/397372.
Al Taher WMA, Mansour EE, El Shafei MN. Comparative study between novel sedative drug (dexmedetomidine) versus midazolam–propofol for conscious sedation in pediatric patients undergoing oro-dental procedures. Egypt J Anaesth. 2010;26(4):299–304.
Burbano NH, Otero AV, Berry DE, Orr RA, Munoz RA. Discontinuation of prolonged infusions of dexmedetomidine in critically ill children with heart disease. Intensive Care Med. 2012;38(2):300–7.
Carroll CL, Krieger D, Campbell M, Fisher DG, Comeau LL, Zucker AR. Use of dexmedetomidine for sedation of children hospitalized in the intensive care unit. J Hosp Med. 2008;3(2):142–7.
Dewhirst E, Fedel G, Raman V, Rice J, Barry N, Jatana KR, Elmaraghy C, Merz M, Tobias JD. Pain management following myringotomy and tube placement: intranasal dexmedetomidine versus intranasal fentanyl. Int J Pediatr Otorhinolaryngol. 2014;78(7):1090–4.
Fagin A, Palmieri T, Greenhalgh D, Sen S. A comparison of dexmedetomidine and midazolam for sedation in severe pediatric burn injury. J Burn Care Res. 2012;33(6):759–63.
Ghali AM, Mahfouz AK, Al-Bahrani M. Preanesthetic medication in children: a comparison of intranasal dexmedetomidine versus oral midazolam. Saudi J Anaesth. 2011;5(4):387–91.
Lin H, Faraklas I, Sampson C, Saffle JR, Cochran A. Use of dexmedetomidine for sedation in critically ill mechanically ventilated pediatric burn patients. J Burn Care Res. 2011;32(1):98–103.
Mason KP, Lubisch N, Robinson F, Roskos R, Epstein MA. Intramuscular dexmedetomidine: an effective route of sedation preserves background activity for pediatric electroencephalograms. J Pediatr. 2012;161(5):927–32.
Mason KP, Robinson F, Fontaine P, Prescilla R. Dexmedetomidine offers an option for safe and effective sedation for nuclear medicine imaging in children. Radiol. 2013;267(3):911–7.
Sheta SA, Al-Sarheed MA, Abdelhalim AA. Intranasal dexmedetomidine vs midazolam for premedication in children undergoing complete dental rehabilitation: a double-blinded randomized controlled trial. Paediatr Anaesth. 2014;24(2):181–9.
Siddappa R, Riggins J, Kariyanna S, Calkins P, Rotta AT. High-dose dexmedetomidine sedation for pediatric MRI. Paediatr Anaesth. 2011;21(2):153–8.
Subramanyam R, Cudilo EM, Hossain MM, McAuliffe J, Wu J, Patino M, Gunter J, Mahmoud M. To pretreat or not to pretreat: prophylactic anticholinergic administration before dexmedetomidine in pediatric imaging. Anesth Analg. 2015;121(2):479–85.
Tammam TF. Comparison of the efficacy of dexmedetomidine, ketamine, and a mixture of both for pediatric MRI sedation. Egypt J Anaesth. 2013;29(3):241–6.
Chrysostomou C, Di Filippo S, Manrique AM, Schmitt CG, Orr RA, Casta A, Suchoza E, Janosky J, Davis PJ, Munoz R. Use of dexmedetomidine in children after cardiac and thoracic surgery. Pediatr Crit Care Med. 2006;7(2):126–31.
Tokuhira N, Atagi K, Shimaoka H, Ujiro A, Otsuka Y, Ramsay M. Dexmedetomidine sedation for pediatric post-Fontan procedure patients. Pediatr Crit Care Med. 2009;10(2):207–12.
Talon MD, Woodson LC, Sherwood ER, Aarsland A, McRae L, Benham T. Intranasal dexmedetomidine premedication is comparable with midazolam in burn children undergoing reconstructive surgery. J Burn Care Res. 2009;30(4):599–605.
Hanss R, Renner J, Ilies C, Moikow L, Buell O, Steinfath M, Scholz J, Bein B. Does heart rate variability predict hypotension and bradycardia after induction of general anaesthesia in high risk cardiovascular patients? Anaesth. 2008;63(2):129–35.
Chatzimichali A, Zoumprouli A, Metaxari M, Apostolakis I, Daras T, Tzanakis N, Askitopoulou H. Heart rate variability may identify patients who will develop severe bradycardia during spinal anaesthesia. Acta Anaesthesiol Scand. 2011;55(2):234–41.
Lesser JB, Sanborn KV, Valskys R, Kuroda M. Severe bradycardia during spinal and epidural anesthesia recorded by an anesthesia information management system. Anesthesiology. 2003;99(4):859–66.
Mason KP, Zgleszewski S, Forman RE, Stark C, DiNardo JA. An exaggerated hypertensive response to glycopyrrolate therapy for bradycardia associated with high-dose dexmedetomidine. Anesth Analg. 2009. doi:10.1213/ane.0b013e3181948a6f.
Berkenbosch JW, Tobias JD. Development of bradycardia during sedation with dexmedetomidine in an infant currently receiving digoxin. Pediatr Crit Care Med. 2003;4(2):203–5.
Chrysostomou C, Beerman L, Shiderly D, Berry D, Morell VO, Munoz R. Dexmedetomidine: a novel drug for the treatment of atrial, junctional tachyarrhythmias during the perioperative period for congenital cardiac surgery: a preliminary study. Anesth Analg. 2008;107(5):1514–22.
Chrysostomou C, Sanchez-de-Toledo J, Wearden P, Jooste EH, Lichtenstein SE, Callahan PM, Suresh T, O’Malley E, Shiderly D, Haney J, Yoshida M, Orr R, Munoz R, Morell VO. Perioperative use of dexmedetomidine is associated with decreased incidence of ventricular and supraventricular tachyarrhythmias after congenital cardiac operations. Ann Thorac Surg. 2011;92(3):964–72.
Rajput RS, Das S, Makhija N, Airan B. Efficacy of dexmedetomidine for the control of junctional ectopic tachycardia after repair of tetralogy of Fallot. Ann Pediatr Cardiol. 2014;7(3):167–72.
Tramèr MR, Moore RA, McQuay HJ. Propofol and bradycardia: causation, frequency and severity. Br J Anaesth. 1997;78(6):642–51.
Kraemer FW, Stricker PA, Gurnaney HG, McClung H, Meador MR, Sussman E, Burgess BJ, Ciampa B, Mendelsohn J, Rehman MA, Watcha MF. Bradycardia during induction of anesthesia with sevoflurane in children with Down syndrome. Anesth Analg. 2010;111(5):1259–63.
Reid JE, Mirakhur RK. Bradycardia after administration of remifentanil. Anesthesiology. 1997;87(4):1019–20.
DeSouza G, Lewis MC, TerRiet MF. Severe bradycardia after remifentanil. Br J Anaesth. 2000;84(3):422–3.
Hawley P. Case report of severe bradycardia due to transdermal fentanyl. Palliat Med. 2013;27(8):793–5.
Funding
None.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gong, M., Man, Y. & Fu, Q. Incidence of bradycardia in pediatric patients receiving dexmedetomidine anesthesia: a meta-analysis. Int J Clin Pharm 39, 139–147 (2017). https://doi.org/10.1007/s11096-016-0411-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-016-0411-5