Abstract
Purpose
To evaluate the role of supersaturation in the in vivo absorption of fenofibrate (FFB), after oral administration in a medium-chain lipid-based formulation (MCLBF).
Methods
FFB was loaded at 90% and 20% w/w of saturated solubility in MCLBF. The two formulations were pre-dispersed in purified water at 5% w/w (ME90% and 20%, respectively) and orally administered to rats to measure in vivo luminal drug concentrations.
Results
FFB precipitated in the stomach due to lipid digestion by gastric lipases and loss of solubilization capacity. This was most significant for ME90%. For ME90%, a high degree of supersaturation was also observed in the duodenum, however, precipitated FFB crystals rapidly re-dissolved. The combination of supersaturation and rapid re-dissolution appeared to drive effective absorption in the upper intestine. For ME20%, FFB precipitated in the stomach but not in the crystalline form and rapidly re-dissolved. Supersaturation in the duodenum again appeared to be the major driver of oral absorption.
Conclusions
The data provide one of the first studies of in vivo luminal drug concentration, supersaturation and absorption from lipid based formulations and suggests that for FFB, whilst very high supersaturation may drive in vitro and in vivo precipitation, re-dissolution and drug absorption is rapid and efficient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lipid-based formulations (LBF) are an effective strategy to enhance the oral absorption of poorly water soluble drugs (PWSD) (1,2,3). LBF are (usually) isotropic mixtures of lipids, surfactants, and/or co-solvents in which the PWSD is pre-dissolved (4). Following oral administration, LBFs of this type (so called self-emulsifying drug delivery systems or SEDDS) disperse to form oil-in-water emulsions in the fluids present in the gastrointestinal (GI) tract. These emulsions are subsequently digested by gastric and intestinal lipases to form colloidal structures comprising lipid digestion products such as monoglycerides and fatty acids, surfactants and secreted bile components (5,6,7).
Formulation dispersion and digestion commonly leads to a reduction in the drug solubilization capacity of LBF, triggering drug supersaturation (8,9,10,11,12,13). This may result in improved absorption through an increase in thermodynamic activity (5,6,7). However, since supersaturation is thermodynamically unstable, this can also result in drug precipitation (14) commonly leading to poor drug absorption. The nature of the material that precipitates from the supersaturated state, including particle size and crystal form, can potentially overcome these limitations if the dissolution rate of the precipitate is high (15,16). This is particularly true where permeability is also high. LBFs therefore, often exhibit complex behaviour in the GI tract.
Lipid digestion in the GI tract can occur via interaction with both gastric and pancreatic lipases. Compared to pancreatic lipases in the small intestine, gastric lipase in the stomach has relatively low activity, especially at acid pH and is therefore thought not to contribute significantly to overall lipid digestion (17). However, Pedersen et al. (18) reported that human gastric lipase activity against tributyrin, a short chain triglyceride, was 7.4 ± 4.0 U/mL in a gastric fluid aspirate at pH 2.8. Based on this observation they suggested that up to 1.7 g of short chain triglyceride may be digested in the fasted stomach (18). Whilst lipase activity is likely to be much lower against the long chain lipids commonly found in the diet and many LBF, this suggests that gastric lipase may play a role in the digestion of some LBFs.
It is apparent therefore that drug absorption from LBF occurs as a result of a complex series of events including formulation dispersion, digestion by lipase enzymes in (potentially) the stomach and (almost certainly) the intestine and interaction with biliary secretions. This in turn may result in the generation of supersaturation and elevation of thermodynamic activity, promoting absorption, or precipitation. Precipitation may reduce absorption, but where re-dissolution is rapid and permeability high, this may not always be the case. The complexity of this process makes in vitro assessment complex. Progress has been made in the use of simple in vitro lipid digestion models that assess the likelihood of drug precipitation on interaction with lipase (19). These have the advantage of being relatively simple and are becoming more and more commonplace. They are also relatively conservative such that although formulations that resist precipitation on digestion ‘challenge’ usually result in good oral exposure, in some cases, even those that precipitate may lead to acceptable absorption. The latter is thought to reflect the lack of an absorption sink in vitro that may lead to overestimation of precipitation. As such models that include an in vitro or in situ absorption sink have been developed (20,21,22), and whilst more complex, appear to more effectively model in vivo events. In addition, in silico models have been developed in an attempt to model the impact of an absorption sink (10), although the accuracy of these models is highly dependent on the provision of high quality data sets to train the models. Experimental data therefore remains critical.
To this point, however, very few studies have attempted to validate these assumptions via assessment of the degree of drug supersaturation in vivo via sampling of luminal fluids. Consequently, similarly few efforts have been made to relate these observations to the outcomes measured in typical in vitro lipid digestion tests. In an attempt to address this gap in our understanding, the current study sampled and quantified concentrations of fenofibrate (FFB), a biopharmaceutics classification system class II drug (clog P = 5.28 (11)), in the stomach and intestine of rats over time after oral administration of an LBF. Drug solubility in the same fluids was also measured to allow calculation of an indicator of drug supersaturation. Fluorescein isothiocyanate dextran (FD-4, MW4000) was included in formulations as a non-absorbable marker and also quantified in luminal samples to account for water flux. The data obtained, alongside observations of drug precipitation in different luminal segments, was compared to in vitro lipid digestion test data to better understand the drivers of drug absorption from LBF. The data suggest that drug supersaturation is a key driver of drug absorption in vivo, that gastric lipolysis may be significant under some circumstances and that drug precipitation may not critically limit drug absorption, at least for FFB.
Materials and Methods
Materials
FFB, fenofibric acid (FFA), FD-4, sodium taurocholate (NaTC), Kolliphor EL, 4-bromophenylboronic acid (4-BPB), and porcine pancreatin extract (P7545, 8 × USP specifications activity) were purchased from Sigma-Aldrich (St. Louis, MO, USA). Captex 300, a medium-chain triglyceride, and Capmul MCM C8 EP/NF, a medium-chain mono- and di-glyceride, were obtained from Abitec Corporation (Columbus, OH, USA). Egg-lecithin was obtained from Lipoid (Lipoid GmbH, Ludwigshafen, Germany). All the other reagents were of analytical grade.
Preparation of Medium-Chain Lipid-Based Formulations (MCLBF) Loaded with FFB
Solubility Measurement of FFB in MCLBF
The formulation lipids (Captex 300 and Capmul MCM C8 EP/NF (1:1 w/w)) and surfactant (Kolliphor EL) were mixed at a ratio of 60:40 (w/w) to prepare MCLBF. The MCLBF (0.5 g) was then added to a 1.5 mL polypropylene tube (Interpath Service, Heidelberg West, Australia) containing an excess of FFB (80 mg). The tube was vortexed, sonicated (Soniclean Model 160HT, Soniclean, Thebarton, Australia) for 30 min, and incubated (Orbital Mixer Incubator, Ratek Instruments, Melbourne, Australia) at 37°C for 7 days. The tubes were centrifuged, and the supernatant was sampled at designated time points (1, 2, 3, 4, 5, 6 and 7 days). The supernatant was diluted with chloroform:methanol (2:1 v/v) and further diluted with acetonitrile and 50:50 acetonitrile:water prior to assay by high performance liquid chromatography (HPLC). The tubes were then re-vortexed, incubated again at 37°C and then resampled at the next time point. The value at which the solubility differed by less than 5% across two consecutive time points was regarded as the equilibrium solubility of FFB.
Preparation of MCLBF90% and 20%
Once the equilibrium solubility of FFB in MCLBF (7 days after onset of incubation at 37°C) was established (124 ± 7.3 mg/g), formulations were subsequently prepared at a drug load of 90% w/w (MCLBF90%) and 20% w/w (MCLBF20%) of the saturated solubility of FFB for further evaluation.
Phase Distribution of FFB after In Vitro Digestion and Dispersion
In Vitro Digestion Study
In vitro digestion studies were performed using a pH-stat titration unit (902 Titrando equipped with 804 Ti stand, Metrohm, Herisau, Switzerland) under conditions similar to those previously described (1,19,23). In this model, LBF are dispersed in model intestinal fluid and pancreatic lipase enzymes added to stimulate digestion. At various times after formulation dispersion and digestion, samples are taken and centrifuged to separate the digest into an undigested oil phase (OP), colloidal aqueous phase (AP), and pellet phase (PP).
In the current studies, a model intestinal fluid comprised lipolysis buffer (2 mM Tris maleate, 1.4 mM CaCl2・H2O, 150 mM NaCl, adjusted to pH 6.5 with NaOH) containing sodium taurocholate (NaTC) and egg-lecithin. Final concentrations of NaTC and egg-lecithin were 50 mM and 3.7 mM, respectively. These concentrations were based on the concentrations of bile acid and phospholipid previously measured in the rat upper small intestine (24).
MCLBF90% or 20% (0.375 g) was dispersed in 13.5 mL of lipolysis buffer in a temperature controlled (37°C) reaction vessel. After 10 min dispersion using an overhead propeller stirrer (length 102 mm, Metrohm, Mitcham, Australia) at 450 rpm (speed setting +3), 1.5 mL of pancreatin extract solution [equivalent to 10,000 tributyrin units (TBU)/mL in the extract, providing 1000 TBU/mL in the digest] was added to initiate digestion. The dispersed FFB concentrations were 2.80 and 0.62 mg/mL for MCLBF90% and 20%, respectively. The concentration of MCLBF in the buffer (approximately 2.5% w/w) was chosen to match 50% of the concentration of dispersed MCLBF in the dosing solutions for in vivo studies (5% w/w), realizing the expectation of a further ~2 fold dilution by biliary secretions, resulting in ~2.5% w/w in intestinal fluids. (see results section “Suspension administration”). After the onset of digestion, fatty acids released from the digestion of triglyceride were automatically titrated with 0.6 M NaOH to maintain the pH at 6.5 and to allow for quantitative determination of the degree of lipid digestion.
During digestion, samples (1 mL) were taken from the reaction vessel at 5, 15 and 30 min, and 5 μL/mL (0.5 M) 4-BPB (in methanol), a lipase inhibitor, added to the sample to inhibit further digestion. The samples were then centrifuged at 37°C at 21,000×g (FRESCO21, Thermo Fisher Scientific, MA, USA) for 15 min to separate AP and PP (since the digestion rate of MCLBF was very rapid, no OP was observed in samples at 15 and 30 min. For the sample at 5 min, a very small amount of OP was observed that could not be readily separated. As such the OP was included within the quantification of the AP at 5 min). The AP was collected and transferred into a pre-weighed plastic tube, and the collected volume was calculated gravimetrically. The collected AP was then diluted 200-fold with acetonitrile and/or 50:50 acetonitrile-water prior to HPLC assay. PP remaining in the sample tube was dissolved with acetonitrile (20 mL for MCLBF90% and 1 mL for MCLBF20%), and further diluted 2–5 fold with 50:50 acetonitrile-water to determine the FFB mass in PP.
In Vitro Dispersion Studies at Different pH
Lipolysis buffer (13.5 mL) at pH 2.4 or 6.5 was added to a temperature controlled (37°C) reaction vessel containing 0.375 g of MCLBF90% or 20%. The medium was stirred at 450 rpm (Metrohm overhead propeller stirrer, speed setting +3). Samples were taken at 30 min and centrifuged at 37°C at 21,000×g for 15 min. FFB concentration in the supernatant was determined by HPLC.
Animal Study
Animals
All experimental procedures were approved by the Institutional Animal Experimentation Ethics Committee (Monash Institute of Pharmaceutical Science, Monash University). Sprague Dawley male rats (244–298 g) were used for the study and sourced from the Monash Animal Research Platform. Two separate sets of animal experiments were conducted. In the first, formulations were administered orally by gavage to conscious rats and blood samples taken from an indwelling carotid artery cannula to allow quantification of plasma exposure of FFA as a function of time and formulation. In the second formulations were again administered orally by gavage to conscious rats, but at set time points animals were euthanised and luminal (gastric and intestinal content) content removed for quantification of FFB concentrations in different luminal areas as a function of time. Analogous experiments were conducted with blank (non-drug containing) formulations to obtain duodenal fluids in which to assess FFB equilibrium solubility.
Preparation of Formulations
Formulations (suspension and microemulsions) were prepared prior to the study. FFB (5.59 mg/mL) was suspended in 0.5% (w/v) carboxymethylcellulose sodium (CMC-Na) in Milli-Q water. LBFs of MCLBF90% or 20% were pre-dispersed in Milli-Q water at 5% (w/w) to obtain microemulsions ME90% (FFB 5.59 mg/mL) and ME20% (FFB 1.24 mg/mL), respectively). In studies where luminal concentrations were measured, FD-4 was dissolved into all formulations at a concentration of 0.72 mg/mL (190 μM.)
Cannulation of Carotid Artery for Blood Collection in Plasma Exposure Studies
Rats were anaesthetized throughout surgery using isoflurane (5% v/v for induction and 2.5% for maintenance). Body temperature was maintained on a 37°C heated pad (Ratek Warming Tray (Model WT1), Ratek, Boronia, Australia). A small incision was made just above the right carotid artery. The vessel was isolated and cannulated using 0.96 × 0.58 mm (o.d. × i.d.) polyethylene tubing filled with 10 IU heparin in saline as described previously (25). The cannula was tunneled to the back of the neck, exteriorized and connected to a swivel assembly to facilitate blood sampling in conscious freely moving animals. After surgery, rats were fasted overnight (up to 14 h) prior to experimentation (water was provided ad libitum).
Experiments to Evaluate Plasma Concentrations of FFA over Time after Oral Administration of FFB Formulations
LBF (1.5 mL of a 5% w/v dispersion of MCLBF90% or 20% in MilliQ water, forming ME90% and ME20% respectively) were administered to rats by oral gavage. Rats remained fasted until 240 min post dose. Blood samples were obtained from the carotid artery cannula at 15, 30, 60, 120, 180, 240, 360, 480, 600, 1440 min. Blood samples were centrifuged at 15,100×g for 5 min (Minispin™, Thermo Fisher Scientific, MA, USA), and plasma obtained. Internal standard (IS) solution of diclofenac sodium (50 μL, 10 μg/mL in acetonitrile) and 150 μL of acetonitrile was added to 50 μL of plasma for samples obtained after administration of the suspension and ME20% formulations, and internal standard (IS) solution of diclofenac sodium (50 μL, 10 μg/mL in acetonitrile) and 900 μL of acetonitrile was added to 50 μL of plasma for samples after administration of the ME90% formulation where plasma concentrations were higher. Precipitated proteins were removed by centrifugation at 15,100×g for 5 min (Minispin™, Thermo Fisher Scientific, MA, USA), and the supernatant was quantified by LC-MS/MS for fenofibric acid (FFA). FFB is quantitatively converted to FFA on first pass though the intestine and liver. As such FFA is the appropriate analyte (26,27).
Experiments to Assess Luminal Concentrations of FD-4 and FFB after Oral Administration of FFB Formulations
LBF (1.5 mL of a 5% w/v dispersion of MCLBF90% or 20% in MilliQ water forming ME90% and ME20% respectively) containing FD-4 were orally administered via gavage to fasted rats (n = 4 per time point). After 5, 15, 30, 60, 120 and 180 min, rats were anesthetized with isoflurane (5% v/v for induction and 2.5% v/v for maintenance). Blood samples were first collected directly from the right jugular vein. Subsequently rats were euthanized by direct injection of pentobarbitone sodium (50 mg/kg) into the left jugular vein, and the abdomen opened immediately. Individual GI sections were opened and luminal fluid was collected directly from the stomach, duodenum (1–4 cm from the pylorus), upper small intestine (10–30 cm from Treitz ligament), and lower small intestine (10–25 cm from the cecum).
Processing Luminal Samples
Luminal fluid samples were collected into two pre-weighed plastic tubes and the volume collected quantified gravimetrically. The luminal fluid in one tube was diluted (1 in 10 to 1 in 200) with buffered dimethyl sulfoxide (DMSO plus 1% v/v HEPES buffer (1 M, pH 7.0) without additional pretreatment. The buffer was added to neutralize stomach pH and to prevent potential degradation of FFB to FFA in the presence of gastric acid. Samples were diluted further with acetonitrile (1 in 10 to 1 in 150) for the assay of FFB or Tris buffer (1 in 6 to 1 in 20) (pH 7.7) for assay of FD-4. These (non-separated) samples gave a measure of total FFB concentrations in combined OP+AP + PP phases. Where lipids were completely digested in the GI tract, the concentration measured was in AP + PP, ie OP was not present. FD-4 concentrations were also analyzed as above.
In the second tube, luminal fluids were first centrifuged at 15,100×g for 5 min (Minispin™, Thermo Fisher Scientific, MA, USA) to separate fluids into OP + AP, and PP. The supernatant (AP + OP) was transferred into another pre-weighed tube. The transferred volume was calculated gravimetrically and diluted 1 in 10 to 1 in 200 with DMSO and further diluted with acetonitrile (1 in 3 to 1 in 30 based on the expected concentration) to determine the solubilized FFB concentration in OP+AP. Where lipid was completely digested in the GI tract, the solubilized concentration was FFB in AP only.
For the assay of FFB, 50 μL of diluted luminal content from above was added to 50 μL of internal standard (IS) solution (0.2 μg/mL albendazole in 50% acetonitrile) and FFB quantified by LC-MS/MS as below. FD-4 levels were assayed using a multi-label luminescence counter (Ensight™, PerkinElmer, MA, USA). The suspended FFB concentration (FFB concentration in PP) was calculated by subtracting the solubilized FFB concentration from the total FFB concentration.
Estimation of Supersaturation
Solubility Measurement of FFB in Lipolysis Buffer and AP from In Vitro Digestion
To determine the equilibrium solubility of FFB in the AP (n = 3) obtained after in vitro digestion, blank MCLBF (containing no drug) was dispersed in lipolysis buffer (containing 50 mM NaTC and 3.7 mM egg-lecithin) and digested under the same experimental condition as described in “In vitro digestion study”. Samples were collected at 5, 15 and 30 min and centrifuged to obtain the AP. The AP (1 mL) was then added to a plastic eppendorf tube with an excess of FFB (10 mg). The tube was mixed and incubated at 37°C for 24 h. Samples were taken and centrifuged at 21,000×g (FRESCO 21, Thermo Fisher Scientific, MA, USA), and the supernatant was diluted 1 in 10 with DMSO and then 1 in 10 in 50:50 v/v acetonitrile-water prior to HPLC assay. For reference, the solubility of FFB in lipolysis buffer containing NaTC and egg-lecithin (n = 4) was also measured in the same way as that in AP described above.
Solubility Measurement of FFB in Duodenal Fluid
After oral administration of 1.5 mL of blank 0.5% CMC-Na or ME formulation (containing no FFB) to rats, duodenal fluid was obtained at 5, 15, and 30 min as described above. The fluid (40–80 μL) was added to a plastic eppendorf tube containing an excess of FFB (1 mg). The tube was vortexed and incubated at 37°C for 24 h. Samples were centrifuged at 21,000×g (FRESCO 21, Thermo Fisher Scientific, MA, USA), and the supernatant removed and diluted 1 in 40 with 50% v/v acetonitrile in Milli-Q water for the 0.5% CMC-Na group, and diluted 1 in 10 with DMSO and a further 1 in 20 with 50% v/v acetonitrile in Milli-Q water for the ME group prior to HPLC determination.
Calculation of Supersaturation Ratio (SR) and Maximum SR (SRM)
The SR of FFB in the AP obtained during in vitro digestion and in the duodenal fluid was calculated using the following equation as previously described (28,29):
SR = FFB concentration in AP in vitro or in the duodenal fluid in vivo / FFB solubility in AP in vitro or in the duodenal fluid in vivo
The maximum SR (SRM), is the ratio between the theoretical maximum concentration of FFB in the AP (APMAX; calculated as the total quantity of FFB included in formulation diluted into the volume of fluid in the digestion vessel) and FFB solubility in the equivalent AP, ie.
Cross Polarized Light Microscopy (CPLM) of PP in Gastric Fluids
The PP collected from gastric samples after oral administration of 1.5 mL of blank ME (containing no FFB), ME90%, or ME20% were examined using CPLM to evaluate whether the material present was crystalline or amorphous. The gastric fluid was first centrifuged at 15,100×g for 5 min to collect PP. The obtained PP was analyzed under a microscope (Carl Zeiss, Oberkochen, Germany) equipped with crossed polarizing filters with images recorded using a Canon PowerShot A70 digital camera (Canon, Tokyo, Japan). In addition, the morphology of the original FFB powder, the FFB precipitate from the in vitro digestion of MCLBF90%, and the FFB precipitate spiked into PP obtained after dosing blank ME was evaluated using CPLM.
Assessment of the Effect of pH-Shift on the In Vitro Digestion of MCLBF20%
Lipolysis buffer (13.5 mL) (pH 6.5, no bile salt micelles) was added to 0.375 g of MCLBF20% in the digestion vessel. In vitro digestion was performed as described in “In vitro digestion study”. Samples were collected at 15 min and centrifuged at 21,000×g at 37°C for 15 min (FRESCO 21, Thermo Fisher Scientific, MA, USA) to collect the AP. At pH 6.5 the AP obtained was clear, and FFB was completely solubilized. The pH of the AP was then adjusted from 6.5 to 2.4 with 1 M HCl. After pH adjustment, the AP became turbid. This was attributed to the phase separation of undissociated ie protonated fatty acids (the pKa of caprylic acid, the main fatty acid from the triglyceride used for MCLBF (Captex), is 4.71) (30). The sample was centrifuged at 21,000×g to separate the AP and PP. The mass of FFB in each phase was quantified using HPLC. The PP was analyzed by CPLM and X-ray diffraction (XRD-7000; Shimadzu Corporation, Kyoto, Japan). The applied voltage and current were 40 kV and 30 mA, respectively. The samples were scanned between 5° and 40° (2θ), with a step size of 0.02° and a count time of 0.6 s.
Quantification of FD-4, FFB and FFA in Various Samples
FD-4 Determination
A multi-label luminescence counter (Ensight™, PerkinElmer, MA, USA) was used for the quantification of FD-4 in luminal samples. The wavelengths were set at 490 and 520 nm for excitation and emission, respectively. Inter-assay variability was accurate to 105.2, 105.8, and 99.2% and precise to 3.4, 4.78, and 0.6% at low (0.038 μg/mL, 0.01 μM), medium (4.54 μg/mL, 1.2 μM), and high (11.4 μg/mL, 3 μM) concentrations of quality control standards (n = 6), respectively.
FFB Determination in Samples from In Vitro Experiments
FFB concentrations in samples obtained from in vitro experiments were determined using a Shimadzu HPLC system comprising LC-30 AD binary pump and SPD-M30A UV detector (Shimadzu Corporation, Kyoto, Japan). A Zorbax Eclipse XDB-C18 column (2.1 × 50 mm, I.D., 5 μm, Agilent Technologies, California, USA) was used at 40°C. The mobile phase comprised of MilliQ water and acetonitrile at a ratio of 40:60 v/v and was run isocratically at a flow rate of 0.3 mL/min. FFB was detected at a wavelength of 288 nm, and the retention time of FFB was 5.2 min. The assay was validated for accuracy and precision using replicate quality control samples (n = 6). Validation was deemed acceptable at low (0.05 μg/mL), medium (1 μg/mL), and high (5 μg/mL) when concentrations were within ±10% of target (± 15% at the LLOQ).
FFB and FFA Determination in Samples from In Vivo Experiments
Analysis of FFB in luminal fluid and FFA in plasma was performed using a Shimadzu 8050 UHPLC triple quadrupole mass spectrometer (UHPLC-MS/MS, Shimadzu, Kyoto, Japan). The column was a Phenomenex Kintex C18 column (50 × 2.1 mm, 2.6 μm, CA, USA) and samples were analyzed at 40°C.
For FFB, 0.1% v/v formic acid in Milli-Q water and methanol were used as the mobile phase at a ratio of 27:73 v/v and the flow rate was 0.3 mL/min. FFB and albendazole (IS) were detected in positive ion mode. Multiple reaction monitoring was performed at m/z 361.2 > 233.1 for FFB and m/z 266.2 > 234.1 for albendazole. The retention times of FFB and albendazole were 2.4 and 0.8 min, respectively. The assay was validated using replicate QC samples at low (0.01 μg/mL), medium (0.5 μg/mL), and high (2 μg/mL) concentration (n = 6) and was accurate and precise to ±10% of target (± 15% at the LLOQ).
For FFA analysis, the mobile phase comprised 0.1% formic acid in Milli-Q water, and methanol at a ratio of 25:75 v/v and a flow rate of 0.2 mL/min. MS analysis was undertaken using negative mode electrospray ionisation. The transition monitored for quantification was m/z 317.2 > 231 for FFA and 293.9 > 250.1 for diclofenac. The retention times of FFA and diclofenac were 1.4 and 1.6 min, respectively. Two sets of plasma standards were prepared to reflect the different plasma concentration ranges anticipated for the different formulations administered. For the standard curve employed to assay samples obtained after dosing ME90%, 50 μL of FFA in acetonitrile (0.1–100 μg/mL) and 50 μL of diclofenac sodium in acetonitrile (10 μg/mL) were added to 50 μL of blank plasma. Plasma proteins were precipitated by the further addition of 850 μL acetonitrile. For plasma samples obtained after administration of the suspension and ME20% formulations, 50 μL of FFA in acetonitrile (0.05–20 μg/mL) and 50 μL of diclofenac sodium in acetonitrile (10 μg/mL) was added to 50 μL of blank plasma. Plasma proteins were then precipitated by the further addition of 100 μL acetonitrile. After centrifugation to remove precipitated protein, the resulting supernatants were used as standards, providing FFA concentrations in the range of 0.005–5 μg/mL and 0.01–4 μg/mL for analysis of ME90% and ME20% samples, respectively. The assay was validated at low (0.005 or 0.01 μg/mL), medium (0.5 or 0.8 μg/mL), and high (5 or 4 μg/mL) concentrations of replicate quality control standards (n = 6). Assays were accurate and precise to within ±10% (± 15% at the LLOQ).
The experimental plasma samples obtained after oral administration of formulations were processed in the same way as the plasma standards described above (described in subsection “Plasma concentration measurement of FFA”) except that FFA in acetonitrile (50 μL) was not added into samples and an equivalent volume of acetonitrile was added instead.
Statistical Analysis
The unpaired Student’s t test (in vitro digestion study and solubility measurement of FFB in duodenal fluid) or one-way ANOVA followed by a Dunnett’s multiple comparisons test (measurement of plasma FFA concentration) was conducted using the statistical software SPSS Student Version 13.0 J (TokyoTosho Co., Ltd., Japan). p-values equal to and less than 0.05 were regarded as statistically significant.
Results
In Vitro Dispersion and Digestion Studies
An in vitro dispersion study for MCLBF90% and 20% was conducted to evaluate the potential for FFB precipitation at pH 2.4 and 6.5 (Fig. 1a). On dispersion of both formulations FFB was completely solubilized for 30 min, regardless of pH or drug loading level.
The fate of FFB after in vitro dispersion and digestion of medium chain lipid based formulations (MCLBF) containing drug at 90% or 20% of saturated solubility in the formulation. Panel A shows the proportion of drug recovered in the aqueous phase (AP) and pellet phase (PP) after formulation dispersion at pH 2.4 and 6.5. Panel B shows drug recovery in the AP and PP after formulation digestion with pancreatic lipase. Results are expressed as mean values with vertical bars showing the S.D. of three experiments. **p < 0.01; % of FFB in AP was significantly higher than that of MCLBF90%.
The fate and phase distribution of FFB after in vitro digestion is presented in Fig. 1b. For MCLBF90%, 41.7 ± 12.4% of FFB was present in the PP at 5 min, and increased to 89.8 ± 3.0% at 15 min i.e., FFB rapidly precipitated after the onset of digestion. In our previous study (29), it was revealed that the threshold SRM for precipitation of FFB on LBF digestion was 3. The data here showing rapid precipitation is therefore consistent with a very high initial SRM (11.3) that drives supersaturation and drug precipitation. Under these circumstances supersaturation was not maintained (SR at 30 min = 0.98 ± 0.27). In contrast, SRM was low (2.51) for MCLBF20% and drug precipitation was not observed. In this case moderate supersaturation was maintained for 30 min (SR at 30 min = 1.97) (this value was slightly lower than that of the SRM because of dilution of the digest with titrated NaOH across the digestion period). The absolute solubility data for FFB in the lipolysis buffer containing NaTC and egg-lecithin and in the AP obtained from the in vitro digestion of blank (non-drug containing) formulation is summarized in Table S1, and compared to the measured FFB concentrations obtained on digestion of the equivalent drug loaded formulations in order to provide the in vitro supersaturation ratio data described above.
Plasma Concentration-Time Profiles of FFA
The plasma concentration-time profiles of FFA after oral administration of the FFB formulations are shown in Fig. 2a. Since formulations were loaded at different proportions of maximum solubility, the absolute dose administered was different. Data are therefore also expressed dose-normalised (% dose/mL) [FFA concentration (μg/mL) in plasma/FFA equivalent mass (μg) in dose (converted from FFB) × 100)] in Fig. 2b for comparison. The corresponding pharmacokinetic parameters are summarised in Table I.
Plasma FFA concentration-time profiles after oral administration of FFB formulations (n = 4 for suspension, n = 3 for ME90%). Plasma samples were sequentially collected from the carorid artery over time. Vertical axes are expressed as concentration i.e. mass/volume (a) and % dose/mL (b). Results are expressed as mean values with vertical bars showing the S.D. of three or four experiments.
After administration of the suspension formulation, the plasma concentration gradually increased until 240 min (Fig. 2), and the Cmax and the area under the plasma concentration-time curve from 0 to 1440 min (AUC0–1440min) were 0.19 ± 0.05%/mL and 109.1 ± 30.6%/mL*min (Table I). When FFB was administered as ME20%, the Cmax (0.75 ± 0.06%/mL) and the AUC0–1440min (288.1 ± 69.4%/mL*min) were significantly higher (dose normalised) than after that obtained with the suspension formulation (Table I). For ME90%, although most of the FFB precipitated within 15 min after in vitro digestion (Fig. 1b), the Cmax (0.67 ± 0.25%/mL) and AUC0–1440min (354.9 ± 49.4%/mL*min) were also significantly improved and dose normalised exposure was similar to that obtained with ME20% (Table I).
Luminal Concentrations of FD-4 and FFB
The luminal concentration-time profiles for FD-4 and FFB after oral administration of the three different formulations are shown in Figs. 3, 4, and 5. The vertical axis displays concentration as a proportion (%) of the concentration in the initial dosing solution (ie in the dosing solution that was gavaged) for FD-4 (0.72 mg/mL in the dosing solution) and FFB (5.59 mg/mL for the suspension and ME90% and 1.24 mg/mL for ME20%). The data show the solubilized concentrations of FD-4 (ie in solution), solubilized FFB and suspended FFB (ie particles). The data are expressed as a % of the dosing solution to show dilution or concentration relative to the dose.
Luminal concentration-time profiles of FD-4 and FFB in different intestinal segments after oral administration of the suspension formulation. Results are expressed as mean values with vertical bars showing the S.D. of four experiments (data for solubilized FFB at 60 and 120 min in the lower small intestine were n = 3). Solubilized FD-4 and FFB is the concentration in the AP of aspirated fluid relative to the concentration in the dosing suspension. Suspended FFB is the concentration of FFB suspended in aspirated fluid.
Luminal concentration-time profiles of FD-4 and FFB in different intestinal segments after oral administration of the ME90% formulation. Results are expressed as mean values with vertical bars showing the S.D. of four experiments. Solubilized FD-4 and FFB is the total concentration in the AP plus oil phase (OP) of aspirated fluid relative to the concentration in the dosing suspension. Suspended FFB is the concentration of FFB suspended in the aspirated fluid.
Luminal concentration-time of FD-4 and FFB in different intestinal segments after oral administration of the ME20% formulation. Results are expressed as mean values with vertical bars showing the S.D. of four experiments. Solubilized FD-4 and FFB is the total concentration in the AP plus oil phase (OP) of aspirated fluid relative to the concentration in the dosing suspension. Suspended FFB is the concentration of FFB suspended in aspirated fluid.
The luminal concentration-time profiles for FD-4, solubilized FFB and suspended FFB are also grouped per intestinal segment and shown after administration of each formulation in Fig. S2–4 in the supplementary material.
Luminal Concentrations after Administration of FFB Suspension
After administration of the FFB suspension formulation (which like the other formulations also contained FD-4) (Fig. 3), the concentration of FD-4 in the stomach dropped rapidly, consistent with gastric emptying of FD-4 and dilution of the remaining FD-4 with secreted gastric juice. In the small intestine, duodenal concentrations of FD-4 (expressed as a % of the dosing concentration) were 59.8 ± 14.0% at 5 min, indicating that FD-4, a non-absorbable marker, was diluted approximately two-fold, presumably due to biliary secretions. In the upper small intestine and most notably in the lower small intestine, FD-4 concentrations exceeded the concentration in the dosing solution (ie. >100%), suggesting concentration in the intestinal lumen due to water absorption from the GI tract. This observation is consistent with previously reported results within our group (31,32,33). Interestingly, data for luminal concentrations of FD-4 were remarkably consistent across all formulations (Fig. 3-5, Fig. S2 for direct comparison) suggesting that the different formulations had little impact on transit or fluid secretion.
After administration of the suspension formulation, the concentrations of solubilized FFB were very low at all time points and in all segments. Instead, suspended particles of FFB were present in the solid state in all GI segments, presumably reflecting the low solubility and dissolution rate of FFB. In the stomach, suspended FFB concentrations exceeded FD-4 concentrations, especially at timescales longer than 30 min after oral administration, suggesting slower gastric emptying of the solid particles compared to the FD-4 in solution (34). In the duodenum and upper and lower small intestine, the suspended FFB concentrations were similar to those of the non-absorbable marker FD-4 suggesting simple convection of suspended particles down the gut. In the lower small intestine, FD-4 and suspended FFB concentration were relatively high, suggesting significant water re-absorption. In the lower small intestine (but not the upper), the concentration of suspended FFB was slightly lower than that of the non-absorbable marker consistent with some (albeit limited), drug absorption.
Luminal Concentrations after Administration of ME90%
After administration of ME90% (Fig. 4) solubilized FFB concentrations in the stomach were initially high (62.5 ± 20.3%, at 5 min) but decreased very rapidly (7.8 ± 14.0% at 15 min). In parallel, suspended FFB increased from 10.8 ± 7.3% at 5 min to 42.8 ± 39.6% at 60 min. These data suggest rapid precipitation of FFB in the stomach. In the duodenum, solubilized FFB concentrations were present up to 30 min and were present at higher concentrations than that of precipitated/suspended FFB, although some suspended FFB was apparent over similar timeframes. Beyond 30 min, concentrations of solubilized or suspended FFB were very low in the duodenum and FFB was essentially not measurable further down the small intestine. The data are consistent with very rapid absorption of material that empties into the duodenum, especially considering the relatively high concentration of suspended FFB in the stomach up to 2 h post dose (that presumably continues to empty into the duodenum over this time period).
Luminal Concentrations after Administration of ME20%
In spite of very different in vitro digestion profiles compared to ME90% (Fig. 1b), oral administration of ME20% (Fig. 5) led to very similar GI solubilization profiles, the latter consistent with the similar extents of in vivo exposure. Thus, solubilized FFB concentrations were initially high in the stomach, but dropped rapidly and at the same time suspended/precipitated levels of FFB increased over the same 15–30 min period. Consistent with ME90%, solubilized FFB levels in the stomach remained low for the rest of the experiment and suspended FFB levels gradually dropped from 30 mins to 2 h, presumably reflecting gastric emptying of suspended FFB into the duodenum. Interestingly, for both ME90% and ME20%, solubilized FFB levels in the duodenum at 15 and 30 min were significantly higher than in the stomach, and lower than levels of suspended FFB in the stomach. These data suggest emptying of suspended FFB into the duodenum followed by rapid resolubilization into intestinal fluids. Again neither solubilized nor suspended FFB was recovered in the upper or lower small intestine suggesting complete absorption in the upper GI tract.
Plasma Concentrations in Luminal Sampling Studies
Plasma samples were also taken from animals that were sacrificed to provide luminal concentration-time profiles and assayed for FFA (Fig. S1 and Table S2). The data were broadly consistent with the equivalent data taken during bioavailability assessment in animals with carotid artery cannulas (Fig. 2). In general plasma concentrations in animals where individual terminal plasma samples were taken were slightly lower than those obtained in sequential samples in animals with carotid artery cannulas. It is not clear why these differences occurred, although data were variable in all cases. Nonetheless the broad trends in plasma exposure were consistent with the luminal concentration time data providing confidence in cross study comparisons. Thus, the persistence of suspended material after administration of the suspension correlated with low but ongoing absorption, whereas more rapid (and similar) absorption from the two lipid formulations was consistent with no evidence of FFB in the small intestine beyond 30–60 min.
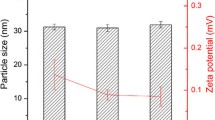
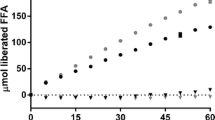
Correlation of the Solubility of FFB in In Vitro Digestion Fluids with Solubility in In Vivo Duodenal Fluids
Figure 6 shows FFB solubility in duodenal fluids obtained at 5, 15 and 30 min after administration of blank suspension and blank lipid vehicle formulations. This in vivo solubility data is compared with the in vitro solubility data in Table S3 and Fig. S5. In vivo, when the blank CMC-Na solution (0.5%) was administered to rats and duodenal fluid removed, FFB solubility in the duodenal fluids was 41.8 ± 8.2, 38.0 ± 5.8, and 40.1 ± 9.0 μg/mL at 5, 15, and 30 min, respectively. This was very similar to FFB solubility in the lipolysis buffer containing bile salt and phospholipid employed in the in vitro digestion test (46.8 ± 0.25 μg/mL), suggesting similar baseline (ie in the absence of lipid formulations) solubilising conditions in vitro and in vivo. After administration of the blank ME formulation, luminal solubility significantly increased to 201.1 ± 59.6, 104.1 ± 6.4, and 85.4 ± 3.0 μg/mL at 5, 15, and 30 min, respectively (Fig. 6). The in vivo solubility values, however, were generally lower than the solubilities measured in the AP obtained from in vitro digestion of the same blank formulation (386.9 ± 14.1, 290.2 ± 17.8 and 267.5 ± 2.6 μg/mL at 5, 15 and 30 min, respectively, Table S3 and Fig. S5). The lower FFB solubility in vivo versus in vitro and therefore reduced solubilising ‘power’ in vivo versus in vitro most likely reflects absorption of formulation digestion products in vivo, leading to a change in the structure of intestinal colloids and lowered solubilization capacity. It is unlikely to reflect a difference to the intrinsic solubilizing power of the intestinal fluids in the absence of formulation materials since in vitro and in vivo solubility in the absence of formulation was similar (~40 μg/mL as described above).
Luminal concentration-time of FD-4 and FFB in different intestinal segments after oral administration of the ME20% formulation. Results are expressed as mean values with vertical bars showing the S.D. of four experiments. Solubilized FD-4 and FFB is the total concentration in the AP plus oil phase (OP) of aspirated fluid relative to the concentration in the dosing suspension. Suspended FFB is the concentration of FFB suspended in aspirated fluid.
Correlation of the In Vivo Duodenal Concentrations of FFB and SR-Time Profile with FFB Concentrations during In Vitro Lipid Digestion
The measured duodenal concentrations of solubilized FFB after administration of the three formulations (rather than the solubility described in the previous section) are shown in Fig. 7a (this is the same data as that shown in Figs. 3-5 but expressed in μg/mL). The solubilized FFB concentrations at 5 min were 7.9 ± 3.0, 1671.4 ± 307.5, and 329.7 ± 164.3 μg/mL for suspension, ME90%, and ME20%, respectively. Measured concentrations in vitro and in vivo and the SR are compared in Table S4 and Fig. S6 and S7. Interestingly, extremely good correlation between in vitro and in vivo AP concentrations was apparent for ME90%. It seems likely however, that the similarity in solubilized drug concentrations occurred via different processes. Thus, the decrease in drug concentrations in the AP in the duodenum from 5 to 30 min in vivo most likely reflected FFB absorption, rather than precipitation since precipitated/suspended drug levels did not increase over the same time frame. In contrast, in vitro, the similar drop in solubilized drug concentration over the same timescale resulted from drug precipitation, since drug absorption was not possible in the absence of an absorption sink. For ME20% the FFB AP concentrations in vitro were much higher than in vivo, reflecting both a lack of precipitation and a lack of absorption.
The supersaturation ratio (SR) was also calculated by dividing the measured concentration by the corresponding duodenal solubility at each time point (Fig. 7b). After administration of the suspension formulation, the SR values were always less than 1 (0.04–0.19), suggesting that absorption was limited by dissolution and solubilization (since high lipophilicity and high intestinal permeability limit the likelihood of permeation limitations) (35). For the ME20% system, moderate supersaturation with SR values of 1.43–1.92 was apparent for 30 min, and the SR values were similar to the SR values from in vitro digestion of MCLBF20% (1.34–1.97) (Fig. S7). However, the similarity in SR values was again likely coincidental. Thus, in vitro, solubilized concentrations were high due to a lack of drug precipitation (Fig. S6) and the solubility was also high due to a lack of absorption of lipid digestion products (Fig. S5) – leading to an SR of 1–2. In contrast in vivo solubilized concentrations were low (Fig. S6) presumably due to drug absorption and solubility was also low due to absorption of digestion products (Fig. S5), as such the combination of (different) events also led to an SR of 1–2.
For the ME90% system, the SR was high (8.31 ± 1.53) in vivo at 5 min, and decreased slowly to 4.75 ± 1.96 at 15 min and 1.07 ± 1.28 at 30 min. In contrast in vitro the SR was significantly lower (3.61 ± 0.61 at 5 min and 1.04 ± 0.29 at 15 min) (Fig. S7). Since the solubilized concentration were very similar in vitro and in vivo the differences in SR largely reflect differences in solubility, thus the lower drug solubility in intestinal fluids in vivo (due to absorption of lipid digestion products) resulted in higher SR. This is consistent with previous studies that have identified lipid absorption and a reduction in the solubilizing capacity of bile salt-lipid micelles as a driver of supersaturation and drug absorption (7).
CPLM of PP from Gastric Fluid Sample
The PP obtained after in vitro digestion of the MCLBF90% formulation (no precipitation was evident from MCLBF20%) and gastric fluid samples obtained after oral administration (in vivo) of the ME90% and ME20% formulations was analyzed by CPLM (Fig. 8a–f). The micrographs of the original FFB powder used to generate formulations was also assessed and revealed large birefringent crystals with a geometric diameter of ~50 μm (Fig. 8a). In contrast, the morphology of the FFB that precipitated during in vitro digestion of MCLBF90% changed to rod-like birefringent structures (Fig. 8b). However, XRD analysis revealed that the crystal form was the same (or very similar) as that of the original FFB (Fig. S8). When blank ME was orally administered, no birefringence was observed in gastric samples (Fig. 8c) consistent with a lack of crystalline material. Interestingly, no FFB crystals were observed in the PP from gastric fluid samples after administration of ME20% (Fig. 8d), in spite of clear evidence of in vivo precipitation of FFB. The data thus suggest that precipitated FFB was present in an amorphous form in the PP. In contrast, after administration of ME90%, birefringent rod-like crystals were clearly observed in the gastric PP (Fig. 8e), with the crystal morphology appearing similar to that in PP of blank ME spiked with FFB precipitate from an in vitro digestion (Fig. 8f). This suggests that FFB precipitated in the crystalline form in the stomach after administration of ME90%, but in the amorphous form after administration of ME20%.
pH-Shift Method for AP from In Vitro Digestion of MCLBF20%
To explore why suspended/precipitated FFB (FFB in PP) was present in the stomach (acidic pH) in vivo after administration of ME20%, whereas in vitro digestion studies under intestinal conditions (pH 6.5) suggested limited precipitation, attempts were made to evaluate the influence of pH on drug precipitation. These studies were stimulated not because of an expectation of an intrinsic effect of pH on drug solubility, since FFB is not ionisable. Rather studies were conducted to explore whether differences in fatty acid ionisation in the stomach may change drug distribution (realizing that lipid digestion was seemingly occurring in the stomach under presumably lower pH conditions (Fig. 9)). To assess this, in vitro digestion experiments were first conducted in the absence of bile salts (ie pseudo gastric conditions), but at neutral pH (since we had access only to intestinal lipase that has limited activity at gastric pH). After digestion, the pH was dropped to pH 2.4 to evaluate the impact of fatty acid protonation on drug phase behaviour. After digestion of ME20% at pH 6.5, even in the absence of bile salts, FFB was completely solubilized in the AP (98.0 ± 0.06%). In contrast, when the pH was shifted to 2.4 (Fig. 9a), the majority of the FFB precipitated and was recovered in the PP (59.6 ± 10.0%). This likely reflects reduced ionisation of fatty acid at acidic pH, phase separation of fatty acid and drug association with the phase separated fatty acid lipid domains. The PP obtained after pH-shift was also analyzed under CPLM and XRD. No FFB crystals were observed in the PP (Fig. 9b), and no specific peak was detected in the XRD diffractogram (Fig. 9c), suggesting that FFB was present in a non-crystalline form in the PP. These data are consistent with the in vivo luminal sampling data.
The effect of pH on FFB precipitation from digested ME20%. Panel A shows FFB distribution between the aqueous phase (AP) and pellet phase (PP) of an in vitro digestion experiment after initial digestion of ME20% at pH 6.5 followed by pH shift to pH 2.4 (mean ±SD, n = 3). Panel B shows CPLM images obtained after pH shift (pH 2.4) of AP samples where no evidence of crystallinity was seen. Panel C shows XRD data confirming the lack of crystalline material in the pellet obtained at pH 2.4.
Discussion
To evaluate and predict the performance of LBF more accurately, an improved understanding of the effects of intraluminal processing on drug absorption is required. Data of this type is also required to underpin the development of improved predictive in vitro dissolution methodologies and PBPK models for LBF. However, data describing drug concentration and supersaturation in the GI tract in vivo after oral administration of LBF and concomitant absorption behaviour is essentially lacking in the literature. The current study therefore sought to measure in vivo solubilization, supersaturation and precipitation over time after oral administration of LBF of FFB and to correlate these data with 1) in vivo absorption profiles and 2) simple in vitro measures of drug solubilization during formulation digestion.
In vitro dispersion and digestion testing revealed that digestion of MCLBF20% (Fig. 1a and b) resulted in almost complete solubilization of FFB, whereas digestion of MCLBF90% (Fig. 1b) resulted in significant drug precipitation. From the in vitro experiments, less effective absorption of FFB might therefore be expected for MCLBF90%. In contrast, when plasma exposure was evaluated in vivo after oral administration of the same formulations, drug absorption from ME90% was essentially the same as that after oral administration of ME20% (Fig. 2 and Table I).
The data therefore suggest that drug absorption from the ME90% formulation is more effective that would be predicted from simple lipid digestion experiments, and potentially that drug precipitation was less evident in vivo than in vitro. One potential explanation for this observation is rapid drug absorption in vivo, thereby reducing supersaturation and drug precipitation from the digesting lipid formulation (1). Bevernage et al. (36) previously evaluated the influence of absorption on supersaturation and precipitation of loviride, a BCS Class II drug, by assessment of in vitro precipitation from a supersaturated solution, with or without the presence of an absorption sink (Caco-2 monolayer). In these studies, the extent of supersaturation of loviride in an in vitro system with an absorption sink was significantly higher than that without absorption sink. The authors concluded that precipitation from the supersaturated state was suppressed (and therefore supersaturation higher) because of ‘escape’ of the drug from the system via the absorption sink – in effect preventing a critical degree of supersaturation (and therefore initiation of precipitation) being reached. Thus, absorption processes that are present in the GI tract, but not in a closed in vitro digestion system, may have suppressed precipitation of FFB in the current experiments, increasing the oral absorption of FFB from the ME90% formulation. Consistent with this suggestion Sassene et al. (37) evaluated the precipitation of FFB in the rat GI tract after oral administration of a long-chain triglyceride formulation using XRD and polarized light microscopy. They observed FFB precipitation in the stomach 90 min after oral administration (the extent of the precipitation was uncertain), but could not find FFB crystals in the intestine, suggesting the likelihood of re-dissolution of the precipitate. However, the methods employed gave only qualitatively evidence of precipitation, and in vivo solubilization and supersaturation were not examined. In the current study therefore, the solubilization, supersaturation, precipitation and absorption behaviour of FFB after oral administration of a LBF of FFB was evaluated in detail in vivo.
In vivo profiling of FFB solubilization and precipitation revealed that in the stomach, suspended/precipitated FFB was rapidly (>15 min) apparent after oral administration of ME90% (Fig. 4), and birefringent FFB crystals were also observed under CPLM (Fig. 8e). This suggests that FFB precipitation was triggered by digestion of the formulation by gastric lipase, since drug precipitation on formulation dispersion was not evident in vitro (Fig. 1a) and drug was well solubilized in vivo at the first (5 min) measured timepoint (Fig. 4). The activity of gastric lipase is lower than that of pancreatic lipase (17), and is suppressed at acidic pH in the fasted stomach. As such gastric digestion has been thought to have a relatively minor impact on LBF digestion. However, Bakala-N’Goma et al. (38) have previously shown that recombinant dog gastric lipase is able to digest a range of LBF and has some activity against an LFCS Type IIIA LBF (classification according to Pouton et al. (39)) containing medium-chain triglycerides - a formulation similar to that employed here. The current data, and data in the literature, therefore suggest that gastric digestion of medium chain LBF is possible (Fig. 4). One explanation for the larger than expected degree of gastric digestion may be the large effective surface area of the dispersed oil droplets in the ME90% dispersion. Type IIIA LBFs generally form microemulsions in water (39,40) resulting in very small lipid droplets with a high surface area to mass ratio. Lipase is also typically more active against medium-chain rather than long chain triglyceride (41,42).
For the ME20% system, although FFB was completely solubilized after in vitro dispersion and digestion (Fig. 1a and b), phase separated FFB was rapidly detected in vivo in gastric fluid samples (Fig. 5). In contrast to ME90%, however, the precipitated FFB was not crystalline (Fig. 8d). From the results of the pH-shift experiment (Fig. 9), one of the reasons for this effect may be drug sequestration into lipid microdomains comprising protonated fatty acids, leading to centrifugation of a mixed amorphous phase of drug and lipid digestion products. The same effect is likely to also occur for ME90%, but in this case, the much larger degree of supersaturation appears to have resulted in phase separation of crystalline FFB rather than amorphous FFB being the dominant process. The recovery of amorphous forms of (especially) weak bases on precipitation from LBF has been reported previously (23,43,44,45,46). In some of these previous cases (46), the effects were suggested to reflect molecular association with non-protonated (ie charged) fatty acids. Here, however, FFB is uncharged and phase separation appears to occur most readily at pHs where the FA is also uncharged. A charge-based molecular interaction is therefore unlikely and the effects observed more likely represent phase separation of a mixed lipid-drug phase.
After administration of the FFB suspension, drug was very poorly solubilized in the duodenum and very poorly absorbed, consistent with high FFB lipophilicity and low water solubility (Fig. 3). In contrast, after administration of ME20%, FFB was rapidly absorbed as FFB passed through the upper small intestine (Fig. 5). Although FFB precipitated in the stomach after administration of ME20%, it did so in a molecularly dispersed ie amorphous state (Fig. 8d). As such dissolution from the solid state is likely to have been rapid since the dissolution rate limitation associated with the crystalline form is avoided. Undigested ME20% that emptied from the stomach, was also seemingly rapidly digested in the duodenum. This has the potential to induce FFB supersaturation (Fig. 7b) at the absorptive site, leading to improvements in oral absorption (Fig. 2).
For the ME90% system, although FFB precipitate was present in the crystalline state in the PP in the stomach (Fig. 8e), on emptying into the intestine, the FFB precipitate was rapidly re-dissolved and drug absorbed (Fig. 4). The rapid re-dissolution likely reflects enhanced solubilization capacity of the intestinal fluid resulting from the formation of mixed micelles of bile components and digestion products (Fig. 6). The high extent of supersaturation of FFB after oral administration of ME90% (the SR was 8.31 and 4.75 at 5 min and 15 min, respectively), is also likely to have driven enhanced absorption (Fig. 7b). Interestingly, in vivo, supersaturation was maintained up to 15 min (SR = 4.75, Fig. 7b), whereas in vitro, precipitation/crystallisation of FFB from ME90% resulted in rapid decay in supersaturation (SR at 15 min = 1.04). The more sustained supersaturation in vivo likely results from two major drivers. Firstly, lipid absorption decreases the solubilisation capacity of mixed bile salt-lipid micelles and this continues as lipid is absorbed over 30 min (Fig. S5). The decrease in solubilisation capacity results in an increase in supersaturation as previously described (7). Secondly, continued drug absorption results in drug ‘escape’ from the system preventing attainment of the peak supersaturation levels required to initiate crystallization (as described previously in vitro (36)). In this way, lipid absorption drives drug supersaturation and drug absorption that in turns protects against drug precipitation. The efficiency of this process is evident in the fact that in the upper and lower small intestine (ie further down the intestine from the duodenum), very low levels of FFB were recovered suggesting either complete absorption in these regions, or upstream GI regions (Fig. 4). Thus, the duodenum was the main region for supersaturation and absorption for this BCS Class II drug.
Conclusions
Here we show the impact of lipid digestion on the in vivo supersaturation/absorption behaviour of a PWSD after oral administration as a MCLBF. This was achieved by directly measuring the in vivo luminal concentration-time profiles of FFB in different regions of the GI tract. After oral administration of ME90%, supersaturation was induced by LBF digestion and precipitation occurred in the stomach forming crystalline FFB. However FFB absorption was high, suggesting rapid re-dissolution in the duodenum. Notably no FFB was seen in regions below the duodenum in vivo consistent with rapid re-dissolution and absorption. In contrast, whilst FFB was recovered from a pellet phase in vivo after administration of ME20%, it is likely that this reflected drug association with protonated fatty acid and FFB was not present in the pellet in the crystalline form. This presumably enhanced re-dissolution and absorption.
In summary, LBF formulations of FFB are digested in the rat stomach in vivo leading to drug precipitation. This precipitate may be crystalline when drug loads and the resulting extent of supersaturation is high, or amorphous at lower drug loads, the latter resulting from phase separation of protonated released fatty acids. In both cases, however, re-dissolution of particulate FFB occurs rapidly, and drug absorption is sufficiently effective that drug is not evident in regions of the GI tract below the duodenum. Thus supersaturation, re-dissolution of both crystalline and amorphous drug and rapid absorption (probably reflecting the high intestinal permeability of FFB), conspire to drive drug absorption from LBF in the highest reaches of the GI tract. The data determined here may help in the development of improved predictive absorption models and the translation of in silico and in vitro data to in vivo outcomes.
Abbreviations
- AP:
-
Aqueous phase
- 4-BPB:
-
4-bromophenylboronic acid
- CPLM:
-
Cross polarized light microscopy
- DMSO:
-
Dimethyl sulfoxide
- FFB:
-
Fenofibrate
- FFA:
-
Fenofibric acid
- FD-4:
-
Fluorescein isothiocyanate dextran 4000
- GI:
-
Gastrointestinal
- HPLC:
-
High performance liquid chromatography
- IS:
-
Internal standard
- LBF:
-
Lipid based formulation
- MCLBF:
-
Medium-chain lipid based formulation
- ME:
-
Microemulsion
- OP:
-
Oil phase
- PP:
-
Pellet phase
- PWSD:
-
Poorly water soluble drugs
- NaTC:
-
Sodium taurocholate
- AUC0-1440min :
-
The area under the plasma concentration–time curve from 0 to 1440 min
References
Feeney OM, Crum MF, McEvoy CL, Trevaskis NL, Williams HD, Pouton CW, et al. 50years of oral lipid-based formulations: provenance, progress and future perspectives. Adv Drug Deliv Rev. 2016;101:167–94.
Rezhdo O, Speciner L, Carrier R. Lipid-associated oral delivery: mechanisms and analysis of oral absorption enhancement. J Control Release. 2016;240:544–60.
Pandey V, Kohli S. Lipids and surfactants: the inside story of lipid-based drug delivery systems. Crit Rev Ther Drug Carrier Syst. 2018;35:99–155.
Zaichik S, Steinbring C, Caliskan C, Bernkop-Schnürch A. Development and in vitro evaluation of a self-emulsifying drug delivery system (SEDDS) for oral vancomycin administration. Int J Pharm. 2019;554:125–33.
Yeap YY, Trevaskis NL, Quach T, Tso P, Charman WN, Porter CJH. Intestinal bile secretion promotes drug absorption from lipid colloidal phases via induction of supersaturation. Mol Pharm. 2013;10:1874–89.
Yeap YY, Trevaskis NL, Porter CJH. The potential for drug supersaturation during intestinal processing of lipid-based formulations may be enhanced for basic drugs. Mol Pharm. 2013;10:2601–15.
Yeap YY, Trevaskis NL, Porter CJH. Lipid absorption triggers drug supersaturation at the intestinal unstirred water layer and promotes drug absorption from mixed micelles. Pharm Res. 2013;30:3045–58.
Williams HD, Trevaskis NL, Yeap YY, Anby MU, Pouton CW, Porter CJH. Lipid-based formulations and drug supersaturation: harnessing the unique benefits of the lipid digestion/absorption pathway. Pharm Res. 2013;30:2976–92.
Anby MU, Williams HD, McIntosh M, Benameur H, Edwards GA, Pouton CW, et al. Lipid digestion as a trigger for supersaturation: evaluation of the impact of Supersaturation stabilization on the in vitro and in vivo performance of self-emulsifying drug delivery systems. Mol Pharm. 2012;9:2063–79.
Stillhart C, Imanidis G, Griffin BT, Kuentz M. Biopharmaceutical modeling of drug supersaturation during lipid-based formulation digestion considering an absorption sink. Pharm Res. 2014;31:3426–44.
Bevernage J, Forier T, Brouwers J, Tack J, Annaert P, Augustijns P. Excipient-mediated supersaturation stabilization in human intestinal fluids. Mol Pharm. 2011;8:564–70.
Gao P, Shi Y. Characterization of supersaturatable formulations for improved absorption of poorly soluble drugs. AAPS J. 2012;14:703–13.
Gao P, Akrami A, Alvarez F, Hu J, Li L, Ma C, et al. Characterization and optimization of AMG 517 supersaturatable self-emulsifying drug delivery system (S-SEDDS) for improved oral absorption. J Pharm Sci. 2009;98:516–28.
Koyama H, Ito M, Terada K, Sugano K. Effect of seed particles on precipitation of weak base drugs in physiological intestinal conditions. Mol Pharm. 2016;13:2711–7.
Sugita M, Kataoka M, Sugihara M, Takeuchi S, Yamashita S. Effect of excipients on the particle size of precipitated pioglitazone in the gastrointestinal tract: impact on bioequivalence. AAPS J. 2014;16:1119–27.
Thomas N, Holm R, Garmer M, Karlsson JJ, Müllertz A, Rades T. Supersaturated self-nanoemulsifying drug delivery systems (super-SNEDDS) enhance the bioavailability of the poorly water-soluble drug simvastatin in dogs. AAPS J. 2013;15:219–27.
Koziolek M, Carrière F, Porter CJH. Lipids in the stomach - implications for the evaluation of food effects on oral drug absorption. Pharm Res. 2018;35:55.
Pedersen PB, Vilmann P, Bar-Shalom D, Müllertz A, Baldursdottir S. Characterization of fasted human gastric fluid for relevant rheological parameters and gastric lipase activities. Eur J Pharm Biopharm. 2013;85:958–65.
Williams HD, Sassene P, Kleberg K, Bakala-N'Goma JC, Calderone M, Jannin V, et al. Toward the establishment of standardized in vitro tests for lipid-based formulations, part 1: method parameterization and comparison of in vitro digestion profiles across a range of representative formulations. J Pharm Sci. 2012;101:3360–80.
Crum MF, Trevaskis NL, Williams HD, Pouton CW, Porter CJH. A new in vitro lipid digestion - in vivo absorption model to evaluate the mechanisms of drug absorption from lipid-based formulations. Pharm Res. 2016;33:970–82.
Suys EJA, Chalmers DK, Pouton CW, Porter CJH. Polymeric precipitation inhibitors promote Fenofibrate Supersaturation and enhance drug absorption from a type IV lipid-based formulation. Mol Pharm. 2018;15:2355–71.
Keemink J, Mårtensson E, Bergström CAS. Lipolysis-permeation setup for simultaneous study of digestion and absorption in vitro. Mol Pharm. 2019;16:921–30.
Khan J, Rades T, Boyd BJ. Lipid-based formulations can enable the model poorly water-soluble weakly basic drug Cinnarizine to precipitate in an amorphous-salt form during in vitro digestion. Mol Pharm. 2016;13:3783–93.
Tanaka Y, Hara T, Waki R, Nagata S. Regional differences in the components of luminal water from rat gastrointestinal tract and comparison with other species. J Pharm Pharm Sci. 2012;15:510–8.
Sahbaz Y, Williams HD, Nguyen TH, Saunders J, Ford L, Charman SA, et al. Transformation of poorly water-soluble drugs into lipophilic ionic liquids enhances oral drug exposure from lipid based formulations. Mol Pharm. 2015;12:1980–91.
Weil A, Caldwell J, Strolin-Benedetti M. The metabolism and disposition of fenofibrate in rat, Guinea pig, and dog. Drug Metab Dispos. 1988;16:302–9.
Weil A, Caldwell J, Strolin-Benedetti M. The metabolism and disposition of 14C-fenofibrate in human volunteers. Drug Metab Dispos. 1990;18:115–20.
Williams HD, Sassene P, Kleberg K, Calderone M, Igonin A, Jule E, et al. LFCS consortium. Toward the establishment of standardized in vitro tests for lipid-based formulations, part 3: understanding supersaturation versus precipitation potential during the in vitro digestion of type I, II, IIIA, IIIB and IV lipid-based formulations. Pharm Res. 2013;30:3059–76.
Devraj R, Williams HD, Warren DB, Porter CJH, Pouton CW. Choice of nonionic surfactant used to formulate type IIIA self-emulsifying drug delivery systems and the physicochemical properties of the drug have a pronounced influence on the degree of drug supersaturation that develops during in vitro digestion. J Pharm Sci. 2014;103:1050–63.
Dupont-Leclercq L, Giroux S, Henry B, Rubini P. Solubilization of amphiphilic carboxylic acids in nonionic micelles: determination of partition coefficients from pKa measurements and NMR experiments. Langmuir. 2007;23:10463–70.
Tanaka Y, Goto T, Kataoka M, Sakuma S, Yamashita S. Impact of luminal fluid volume on the drug absorption after oral administration: analysis based on in vivo drug concentration-time profile in the gastrointestinal tract. J Pharm Sci. 2015;104:3120–7.
Tanaka Y, Sugihara M, Kawakami A, Imai S, Itou T, Murase H, et al. In vivo analysis of supersaturation/precipitation/absorption behavior after oral administration of pioglitazone hydrochloride salt; determinant site of oral absorption. Eur J Pharm Sci. 2017;106:431–8.
Tanaka Y, Kawakami A, Nanimatsu A, Horio M, Matsuoka J, Wada T, et al. In vivo evaluation of supersaturation/precipitation/re-dissolution behavior of cinnarizine, a lipophilic weak base, in the gastrointestinal tract: the key process of oral absorption. Eur J Pharm Sci. 2017;96:464–71.
Kadono K, Yokoe J, Ogawara K, Higaki K, Kimura T. Analysis and prediction of absorption behavior for theophylline orally administered as powders based on gastrointestinal-transit-absorption (Gita) model. Drug Metab Pharmacokinet. 2002;17:307–15.
Takano R, Furumoto K, Shiraki K, Takata N, Hayashi Y, Aso Y, et al. Rate-limiting steps of oral absorption for poorly water-soluble drugs in dogs; prediction from a miniscale dissolution test and a physiologically-based computer simulation. Pharm Res. 2008;25:2334–44.
Bevernage J, Brouwers J, Annaert P, Augustijns P. Drug precipitation-permeation interplay: supersaturation in an absorptive environment. Eur J Pharm Biopharm. 2012;82:424–8.
Sassene PJ, Michaelsen MH, Mosgaard MD, Jensen MK, Van Den Broek E, Wasan KM, et al. In vivo precipitation of poorly soluble drugs from lipid-based drug delivery systems. Mol Pharm. 2016;13:3417–26.
Bakala-N'Goma JC, Williams HD, Sassene PJ, Kleberg K, Calderone M, Jannin V, et al. Toward the establishment of standardized in vitro tests for lipid-based formulations. 5. Lipolysis of representative formulations by gastric lipase. Pharm Res. 2015;32:1279–87.
Pouton CW. Formulation of poorly water-soluble drugs for oral administration: physicochemical and physiological issues and the lipid formulation classification system. Eur J Pharm Sci. 2006;29:278–87.
Pouton CW. Lipid formulations for oral administration of drugs: non-emulsifying, self-emulsifying and 'self-microemulsifying' drug delivery systems. Eur J Pharm Sci. 2000;11:S93–8.
Han SF, Yao TT, Zhang XX, Gan L, Zhu C, Yu HZ, et al. Lipid-based formulations to enhance oral bioavailability of the poorly water-soluble drug anethol trithione: effects of lipid composition and formulation. Int J Pharm. 2009;379:18–24.
Devraj R, Williams HD, Warren DB, Mohsin K, Porter CJH, Pouton CW. In vitro assessment of drug-free and fenofibrate-containing lipid formulations using dispersion and digestion testing gives detailed insights into the likely fate of formulations in the intestine. Eur J Pharm Sci. 2013;49:748–60.
Khan J, Hawley A, Rades T, Boyd BJ. In situ lipolysis and synchrotron small-angle X-ray scattering for the direct determination of the precipitation and solid-state form of a poorly WaterSoluble drug during digestion of a lipid-based formulation. J Pharm Sci. 2016;105:2631–9.
Sassene PJ, Knopp MM, Hesselkilde JZ, Koradia V, Larsen A, Rades T, et al. Precipitation of a poorly soluble model drug during in vitro lipolysis: characterization and dissolution of the precipitate. J Pharm Sci. 2010;99:4982–91.
Stillhart C, Imanidis G, Kuentz M. Insights into drug precipitation kinetics during in vitro digestion of a lipid-based drug delivery system using in-line raman spectroscopy and mathematical modeling. Pharm Res. 2013;30:3114–30.
Sassene PJ, Mosgaard MD, Löbmann K, Mu H, Larsen FH, Rades T, et al. Elucidating the molecular interactions occurring during drug precipitation of weak bases from lipid-based formulations: a case study with cinnarizine and a long chain self-nanoemulsifying drug delivery system. Mol Pharm. 2015;12:4067–76.
Acknowledgments
This research was partially supported by the Nagai Foundation Tokyo research grant 2018.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guest Editor: Sheng Qi
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 769 kb)
Rights and permissions
About this article
Cite this article
Tanaka, Y., Tay, E., Nguyen, TH. et al. Quantifying In Vivo Luminal Drug Solubilization -Supersaturation-Precipitation Profiles to Explain the Performance of Lipid Based Formulations. Pharm Res 37, 47 (2020). https://doi.org/10.1007/s11095-020-2762-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-020-2762-9