ABSTRACT
Purpose
The objective of this study was to develop high-content gemcitabine PEGylated liposomes to reverse gemcitabine resistance in pancreatic tumour cells. The mechanism of drug loading into liposomes was also investigated.
Methods
To increase the drug entrapment efficiency (EE) and drug loading (DL), a novel passive loading approach named Small Volume Incubation method (SVI) was developed and compared to the reverse phase evaporation (REV) and remote loading methods. The in vitro cytotoxicity was evaluated using MIA PaCa-2 and Panc-1 cell lines.
Results
The EE for remote loading was 12.3 ± 0.3%, much lower than expected and a burst release was observed with the resultant liposomes. Using the optimized SVI method, increased EE (37 ± 1%) and DL (4%, w/w) were obtained. The liposomes (200 ± 5 nm) showed minimal drug leakage, good stability, and significant improvement in cytotoxicity to the gemcitabine-resistant pancreatic cancer cell lines.
Conclusions
Remote loading was not suitable for loading gemcitabine into liposomes. pKa > 4.6 for basic drugs and intra-liposomal precipitation of loaded compounds were suggested as an additional requirement to the current criteria for remote loading using ammonium sulphate gradient (pKa < 11). High DL is essential for liposomes to reverse gemcitabine resistance in pancreatic cell lines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Gemcitabine, a weak base with pKa 3.6, is a potent anti-cancer drug commonly used for the treatment of pancreatic cancer and other solid tumours, such as lung cancer, bladder cancer and metastatic breast cancer (1–3). Furthermore, gemcitabine is a prodrug which must be taken up by the cell and phosphorylated within the cell to form the active moiety, gemcitabine triphosphate, which inhibits the synthesis of DNA (2). However, after systemic administration, gemcitabine is rapidly converted into the inactive metabolite by cytidine deaminase and excreted through the urine with a half life ranging from 9 to 22 min, which limits its anti-cancer effect (4–7). Furthermore, multidrug resistance (MDR) has been reported, significantly reduced the clinical efficacy of gemcitabine (8).
Liposomes are nontoxic vesicular drug carriers with an aqueous core enclosed in one or more phospholipid bilayers with the capacity to accommodate both water soluble and lipid soluble drugs. It has been well documented that the cytotoxicity of many anti-cancer drugs is increased both in vitro and in vivo by using liposomes as carriers (9–11). In addition cell culture studies have indicated that liposomes are taken into cells via endocytosis which may increase the efficiency of drug delivery for compounds such as gemcitabine which require active transport into the cell (2). PEGylated liposomes such as Doxil® have been employed as carriers for a number of drugs to obtain a longer circulating time in vivo (12–14). To date, a number of research groups have investigated PEGylated liposomal delivery of gemcitabine, and have shown enhanced tumour cytotoxicity both in vitro cell culture and in vivo tumour models. For liposome formulation, high drug entrapment efficiency (EE) and drug loading (DL) are desirable. Apart from any economic advantage, a high DL could increase the amount of drug loading into liposomes which leads to further increase in the anti-tumour effect as well as reduction of the side effects caused by phospholipids and cholesterol (15,16). However, the DL for gemcitabine is less than 1% to date, which limits its anti-cancer effect (10,17,18), especially for the gemcitabine resistant cell lines.
Currently several methods have been reported for loading gemcitabine into liposomes. These include the thin film hydration (TFH) method, the reverse phase evaporation vesicle (REV) method and a remote loading method using an ammonium sulphate gradient (10,17,19). With the TFH and REV methods, an EE of 47% (17) and 67% (10) was achieved for gemcitabine respectively, but in both methods the liposomes were >1μm, and thus regarded as unsuitable for tumour targeting. With a reduction in size of the liposomes to 200 nm by extrusion, the EE reduced dramatically to around 5%, corresponding to a decrease in the total inner aqueous core volume (20–22).
Remote (or active) loading of a weak base into liposomes using trans-membrane gradients of ammonium sulphate, is one of the most widely used approaches for achieving a high EE. Based on the literature, this method is suitable for loading a weak base with a pKa ≤ 11 and log P value ranging from −2.5 to 2.0 (23–25). According to the above requirements, gemcitabine (pKa = 3.6, log P = −1.4) would appear to be a good candidate for remote loading, and EEs of over 90% have been reported for gemcitabine by this method since 2004 (9,19,26–28). However, our substantial data and some other studies reported a low EE of less than 20% using this method (29,30). This raised the question of whether gemcitabine is suitable for remote loading using ammonium sulphate. If not, the current prerequisites of pKa ≤ 11 and log P (−2.5 to 2.0) need to be re-considered. There is a crucial need to investigate the mechanism by which gemcitabine is loaded into liposomes when ammonium sulphate gradient is used.
The aim of this study was to investigate the mechanism for gemcitabine loading into liposomes and to develop liposomes of acceptable size with high EE and DL for reversing gemcitabine resistance in pancreatic cancer cell lines. Furthermore, a novel method for the preparation of gemcitabine loaded liposomes was developed to improve the EE, DL and their in vitro effects on the cytotoxicity using gemcitabine-resistant cell lines. The effect of the freeze-thaw process on micelle formation was also addressed.
MATERIALS AND METHODS
Materials
The phospholipids, 1,2-dipalmitoyl-sn-glycero-3-phospocholinemonohydrate (DPPC) and N-(carbonyl-methoxypolyethylene-glycol-2000)-1,2-distearoyl-sn-glycero-3-phospho-thanolamine (DSPE-MPEG2000) were purchased from Lipoid (Steinhausen, Switzerland). Cholesterol, gemcitabine (purity >98%) and 3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyl-tetrazolium bromide (MTT) for cytotoxicity studies were purchased from Sigma (Auckland, New Zealand). Milli-Q water was prepared using a water purification system (Millipore Corp., Bedford, MA, USA). All the other materials for this study were of analytical grade.
Reverse Phase Evaporation Method (REV)
Thin film was prepared as follows: the lipid mixture (10 mg in total) of DPPC: cholesterol: DSPE-MPEG2000 was used to prepare liposomes at a molar ratio of 6:3:1 unless otherwise stated. The mixture was dissolved in 1 ml of chloroform: methanol (3:1, v/v). The thin film of the lipid was then obtained by removal of the organic solvent using a rotary evaporator under a vacuum condition (R-215, Büchi, Switzerland). Further traces of the organic solvent were removed by flowing nitrogen at 45°C for 40 min.
The lipid thin film was hydrated using 1 ml of diethyl ether, mixed with 0.5 ml of gemcitabine hydrochloride solution (1 mM) and sonicated for 2 min. The diethyl ether was then removed by rotary evaporation, followed by extrusion (10 times) through a 200 nm pore size polycarbonate membrane with a sterilized extrusion device (Gastight, Hamilton, New Zealand). The free un-entrapped gemcitabine was then removed by gel filtration through a Sephadex G50 column (Sigma-Aldrich, Auckland, New Zealand).
Thin Film Hydration (TFH)-Extrusion Method
The thin film, prepared as described above, was hydrated with 0.5 ml of 1 mM gemcitabine hydrochloride solution with stirring at 45°C for 40 min. The multilamellar liposomes were then submitted to 10 cycles of freezing (with liquid nitrogen) and thawing (with a water base at 4°C). The liposome suspension was extruded through 400 nm and then 200 nm pore size polycarbonate membrane filters with a stainless steel extruder. The free gemcitabine was removed by gel filtration using a Sephadex G50 column.
Since the freeze-thaw cycling time is crucial for the particle size distribution of the resultant liposomes, three freeze-thaw time spans (3, 5 and 7 min) were investigated. The freeze-thaw cycle was fixed at 10 for the major studies.
Remote Loading Using Ammonium Sulphate Gradient
Liposomes were prepared as described in the literature (19,26). The lipid thin film was hydrated with 0.5 ml of 250 mM ammonium sulphate solution with stirring at 45°C for 40 min. Thereafter the process followed was the same as the TFH-extrusion method described above. Free ammonium sulphate was removed by ultracentrifuge at 186,000×g (FLA-55, Beckman, USA) at 4°C for 1 h. Finally, the liposome pellet was resuspended in 0.5 ml of isotonic gemcitabine solution (1 mM) and kept at 60°C for 3 h.
To explore whether the ammonium sulphate gradient could effectively improve the EE of gemcitabine, different ammonium sulphate gradients were investigated (120 mM and 250 mM) compared with PBS buffer (pH 7 and 5.5).
Passive Loading with Small Volume Incubation (SVI) Methods
A novel method was developed for gemcitabine loading. Firstly, blank liposomes were obtained through the TFH-extrusion method using phosphate buffer (pH 7, 50 mM, adjusted with NaCl to isotonic) as the hydration solution. The liposomes were then ultracentrifuged at 186,000×g at 4°C for 1 h, the supernatant was removed, and 20 μl of concentrated (25 mM) gemcitabine isotonic solution was added to the liposome pellets. The total amount of gemcitabine was maintained at the same level as for the remote loading method described above. After vortexing for 3 min, the mixture was incubated at 60°C for 3 h. Finally the mixture was constituted to 0.5 ml with isotonic sodium chloride solution (pH adjusted to 7).
To further improve drug loading (drug-to-lipid ratio) the above method (SVI1) was modified by using 20 μl of gemcitabine suspension (1.5 mg) for drug loading (SVI2). The dissolution from this suspension was found to be fast enough for a complete drug loading into the liposomes at 60°C. Taking the effect of osmotic pressure into consideration, the empty liposomes were prepared with Milli-Q water instead of PBS buffer. All the other processes were the same as that used in SVI1.
In addition, blank liposomes loaded with ammonium sulphate (250 mM) were also used for drug loading with the SVI2 method for investigation of in vitro release.
Particle Size, Zeta Potential and Morphology
The particle size distribution and zeta potential of liposomes prepared by different methods were measured by a laser diffraction particle analyzer (Nano-ZS Malvern Instruments Ltd, UK).
The morphology of the liposomes was examined by transmission electron microscopy (TEM) (FEI Tecnai G2 Spirit Twin 120Kv) using negative staining. Briefly, a 3 mm 200-mesh copper grid was put on top of one drop of liposome suspension (0.2 mg/ml). After 2 min incubation, the surplus was removed by filter paper, and the liposome sample on the mesh stained with 2% uranyl acetate solution and incubated for a further 1 min. The sample was dried at room temperature before use.
Entrapment Efficiency (EE) and Drug Loading (DL)
The EE of gemcitabine in liposomes was measured via a gel-filtration method using a Sephadex G50 column (bead size, 20–80 μm). The free gemcitabine was separated completely from the liposomes after 10 min, and 100 μl of the filtered liposome suspension was diluted with 900 μl of 10% triton-X 100 solution and sonicated for 15 min before analysis for gemcitabine using a validated reverse-phase HPLC method. A HP 1200 series liquid chromatograph comprising a quaternary pump, vacuum degasser, auto-sampler injector, thermostated column compartment and diode array detector was used, with data acquisition by Chemstation software (Agilent Corporation, Germany).
Entrapment efficiency (EE) and drug loading (DL) were calculated using the following equations:
where Min is the drug amount entrapped, Mtotal the total drug amount used in preparation and Mlip the total mass of liposomes containing the drug. For the liposomes prepared with REV without extrusion, the particle size (> 1 μm) was too large to pass through the Sephadex column. The EE of gemcitabine was measured using a dilution and ultra-filtration method (50 kDa) (20). Briefly, 0.1 ml of the liposome suspension was diluted with 0.9 ml PBS buffer (pH 7.0), and un-entrapped gemcitabine (Cfree) was separated by ultra-filtration. The gemcitabine concentration was then measured, and the EE calculated using the following equation.
where C total is the total gemcitabine concentration after dilution with PBS.
Release Profiles
The release rates for gemcitabine from various liposomes were investigated using a dialysis method. Cellulose acetate dialysis bags (molecular weight cut off 12–14 kDa) containing 1 ml of the liposome suspension were placed in 50 ml release medium (phosphate buffer solution, pH 7.4, 50 mM, adjusted with sodium chloride to isotonic). The release medium was kept at 37°C with stirring throughout the experiment. At different time intervals, a 0.1 ml sample was withdrawn and replaced with the same volume of fresh medium. Samples were analyzed by HPLC and the % of the drug released was calculated.
The Ritger-Peppas model was used to investigate the kinetics of gemcitabine release from the liposomes:
where Mt/M∞ presents the fraction of drug released at time t, K is the constant of the release rate, and n stands for the diffusion exponent which is an indicator of the mechanism of drug release. In spherical carriers, n ≤ 0.43 indicates a Fickian diffusion; if 0.43 ≤ n ≤ 0.85, a non-Fickian transport; and if n ≥ 0.85, a zero order drug release mechanism dominates (31,32).
In addition, release profiles from different liposomes were compared using a similarity factor (f 2). f 2 is a logarithmic transformation of the sum-squared error of the differences in % release between two formulations (Tj and Rj) through all the time points. The f 2 may range from 0 to 100, and it has been suggested by the U.S. Food and Drug Administration (FDA) that if the f 2 is between 50 and 100, the two profiles are considered to be similar (33).
where m represents the total time points, and; wj is an optional weight factor.
In Vitro Cytotoxicity
Pancreatic cancer cell lines, MIA PaCa-2 and PANC-1 (both gifts from the Auckland Cancer Society Research Centre) were cultured in Dulbecco’s Modified Eagle’s Medium (DMEM) supplemented with 10% FBS, 100 U/ml penicillin and 100 μg/ml streptomycin (complete DMEM) and maintained in an incubator with 5% CO2/95% air at 37°C.
The MTT cell viability assay was used to evaluate the cytotoxic effects of various gemcitabine liposomes in MIA PaCa-2 and PANC-1 cell lines. Gemcitabine solution and a mixture of drug solution with empty liposomes were used as references. Cells were seeded at 5 × 103 cells/well in a 96-well plate in phenol-red free complete DMEM and incubated for 24 h. Cells were treated in triplicate with free gemcitabine, gemcitabine liposomes, empty liposomes and empty liposomes plus free gemcitabine, and incubated for 24 and 48 h. At each time point, the medium was removed and the cells were washed with PBS. The MTT (Sigma-Aldrich) was dissolved in PBS (5 mg/ml) and then further diluted in phenol-red free complete DMEM to 0.5 mg/ml. A volume of 100 μl of MTT solution was added to each well and incubated for 2 h, after which the medium was removed and the precipitated formazan dissolved in 100 μL DMSO on a shaker for 10 min. Samples were read at 540 nm on a plate reader (Molecular Devices). The background absorbance of medium only controls was subtracted from the sample readings, and cytotoxicity was expressed as a percentage of control (untreated cells). Experiments were conducted at least in duplicate (n = 6, for each experiment).
Stability
The physicochemical stability of the gemcitabine loaded liposomes prepared by the SVI method was investigated. Liposomes were stored in the form of ultra-centrifuged pellets or suspension (in PBS buffer) at 4°C away from light. Particle size, zeta potential of liposomes and chemical stability of the drug were monitored over 3 months.
Statistical Analysis
Results are mainly expressed as mean ± SD. Data were compared by two-way ANOVA (Analysis of Variance) with Tukey’s multiple comparisons test using Origin 8.0 and the p value for significance was set at 0.05.
RESULTS
The REV Method
With the REV method, the EE of gemcitabine measured before extrusion was 54.2 ± 0.1% (n = 3), similar to that reported (10). However, the liposome was larger than 1,000 nm. After extrusion through a 200 nm membrane, the liposomal size was reduced to 200 ± 5 nm, but the EE also decreased to 5.4 ± 0.1%, with a DL of 0.08 ± 0.001%.
TFH-Extrusion Method
The EE of gemcitabine prepared by the TFH method with passive loading (volume 0.5 ml) was 5.7 ± 0.2%, with a particle size of 200 ± 5 nm. The DL was 0.08 ± 0.001% similar to the REV. As shown in Fig. 1, with 3 min for each freeze-thaw cycling, small liposomes or micelles with a particle size less than 50 nm were produced. It was difficult to separate these small particles from the supernatant by ultracentrifuge. In contrast, 5 min and 7 min resulted in a narrower particle size distribution, and larger pellets. No significant difference was found between 5 min and 7 min (p > 0.05). Interestingly, these small particles were not observed in the liposomes prepared with low level of DSPE-MPEG2000 (3% in molar ratio) even where no freeze-thaw process was applied.
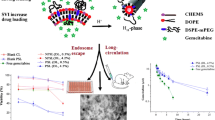
Transmission electron micrographs of liposome suspensions. (a) is the sample prepared with a 3 min freeze-thaw time; (b) is obtained by 5 min freeze-thaw time; (for (a) and (b) the formulation was DPPC: cholesterol: DSPE-MPEG2000 = 6: 3: 1), and (c) is the liposomes prepared with less DSPE-MPEG2000 and no freeze-thaw process (DPPC: cholesterol: DSPE-MPEG2000 = 6: 3: 0.3).
Remote Loading of Gemcitabine Using Ammonium Sulphate Gradient
In remote loading, different ammonium sulphate gradients, 0 (isotonic PBS buffer, pH 7 and pH 5.5), 120 and 250 mM (both at pH 5.5) were compared to evaluate the impact of ammonium sulphate on EE. Without ammonium sulphate, the EE of gemcitabine at pH 7 and 5.5 was 7.6 ± 0.2% and 7.9 ± 0.3%, respectively. Increasing the concentration of ammonium sulphate from 120 to 250 mM only increased the EE from 9.7 ± 0.2% to 12.4 ± 0.4%. The particle size of the liposomes was kept at 200 ± 10 nm. The highest DL using ammonium sulphate gradient was 0.18 ± 0.006%.
Passive Loading with SVI Methods and the Optimized Conditions
With both passive loading and remote loading, the EE was increased dramatically when the gemcitabine solution was condensed to a small volume (from 500 μl to 20 μl).
With the SVI1 method, the optimized incubation time on the EE of gemcitabine was determined to be 3 h to give an EE of 37.0 ± 1% with a particle size of 200 ± 10 nm. Increasing the loading time from 3 to 4 h showed little increase in EE (p > 0.05), suggesting that 3 h was sufficient to reach the equilibrium for drug loading.
The EE for SVI2 where a small volume of drug suspension was used for drug loading was 30 ± 1% which was slightly lower than SVI1, 37%. However, the drug loading increased 8-fold from 0.5% to 4.0%, which is the highest drug loading reported for gemcitabine-liposomes to date [10].
Drug Release Profile
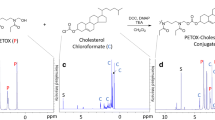
The liposomes prepared without ammonium sulphate, either with SVI1 or SVI2, showed little release (<4%) at 1 h, and no more than 10% at 24 h (Fig. 2). Despite the different drug levels in the liposomes, their % release profiles were similar (f 2 was 83 (33)). In contrast, a burst release from the liposomes within 15 min (40–60%) was observed when ammonium sulphate was used in any of the methods. Furthermore, the release rate from the conventional remote loaded liposomes was significantly reduced when the release medium (290 mOsm) was adjusted to be isotonic to the liposomal cores (550 mOsm).
Drug release profiles from liposomes prepared with SVI1 method (inverted triangle), SVI2 method (black circle) (both without the use of ammonium sulphate), conventional remote loading method (white square) and SVI2 method with ammonium sulphate (white circle), and the liposomes prepared with conventional remote loading method when dialysis medium adjusted to 550 mOsm (black square). Data are mean ± SD (n = 3).
The calculated exponent in the Ritger-Peppas equation (n) for gemcitabine released from liposomes prepared by SVI1, SVI2, remote loading, and SVI2 plus remote loading was 0.021, 0.27, 0.08 and 0.072, respectively, indicating Fickian diffusion as the major mechanism for drug release.
In Vitro Cytotoxicity
A strong resistance to free gemcitabine was demonstrated in both MIA PaCa-2 and PANC-1 cell lines with cytotoxicity remaining relatively constant within the gemcitabine concentration from 10 to 200 μM. Surprisingly, repeated experiments demonstrated that the liposomes of low DL (0.17–0.5%, w/w) prepared with either the remote loading or SVI1 did not show improved cytotoxicity compared to the drug solution at this concentration range. Higher concentrations could not be investigated as the empty liposomes showed significant cytotoxicity.
In contrast, treatment with gemcitabine liposomes prepared by SVI2 with a high drug loading (drug to lipid ratio 4%, w/w) (L-gem (SVI2)) was significantly more cytotoxic than free gemcitabine at 100 and 200 μM after 24 h, and at 50, 100 and 200 μM in MIA PaCa-2 cells after 48 h (Fig. 3). Similarly, in PANC-1 cells, gemcitabine liposomes were significantly more cytotoxic than free gemcitabine at 100 and 200 μM at 24 h and at 50, 100 and 200 μM at 48 h after treatment. Blank liposomes (L-blank, SVI2) in the presence or absence of free gemcitabine were not significantly cytotoxic after 24 h exposure, but did display some toxicity in both cell lines after 48 h exposure. However, the cytotoxicity was to a much lesser extent when compared to liposomal gemcitabine.
Stability
The particle size and zeta potential were stable regardless of whether the liposomes were stored in the form of pellets or suspension for 2 months. However after 3 months, the zeta potential for both the liposome pellet and suspension decreased by approximately 5 mV. In addition, gemcitabine was chemically stable in both pellets and suspension forms over this time frame (p > 0.05) Table I.
DISCUSSION
In this study, different methods for preparation of gemcitabine loaded liposomes were investigated. Efforts were made to understand the mechanism by which the drug was loaded into the liposomal aqueous core to increase the entrapment efficiency and drug loading. For the REV method, initially a w/o emulsion was formed to increase the inner aqueous liposomal core, and hence the EE of gemcitabine was increased to 54.2%, similar to that previously reported (10). However, the size of the liposomes, greater than 1,000 nm was too large for in vivo use to exploit the enhanced permeability and retention effect (34,35). Extrusion of the liposomes was able to reduce their size and the total volume of the inner aqueous core was reduced, leading to a decrease in EE to ~ 6%.
The TEM data indicated that both the freeze-thaw time and the amount of DSPE-MPEG2000 were crucial to the liposome size. The 3 min thaw in 45°C water bath was not long enough to completely warm it up to above the transition temperature of DPPC (41°C), reducing the efficiency of the freeze-thaw process. Furthermore, the low efficiency of the freeze-thaw step led to a lack of uniformity of the lipid bilayers, especially in the presence of DSPE-MPEG2000. As reported, the addition of PEGylated lipids could cause a decrease in the particle size, and even the formation of micelles with a particle size less than 50 nm due to the polarity of the PEG chain (36,37) As a result, the poor distribution of DSPE-MPEG2000 caused by the inefficient freeze-thaw (3 min) led to a higher ratio of DSPE-MPEG2000 in certain areas of the bilayers. When the multilamellar liposomes passed through the polycarbonate membrane, the higher ratio of DSPE-MPEG2000 would facilitate the formation of smaller liposomes or even micelles. In contrast, with 5 min of the liposome suspension at 45°C, which was above the transition temperature of DPPC (41°C), no liposomes with a particle size less than 50 nm were observed.
Figure 4 shows the proposed mechanism of the remote loading for the weak base, gemcitabine. With the diffusion of the ammonia, the pH of the internal aqueous core would reduce as low as pH 3.6 (24). In our study, the external pH was controlled (pH 7) using isotonic PBS buffer. The pH gradient is the direct driving force for weak bases, such as doxorubicin, by maintaining the drug ionized inside the liposomes and thus makes it unable to diffuse to the external liposomal media (16,38). In this case, there was a concentration gradient of unionized weak base between the internal and external environment. When the weak base inside the liposome achieves its maximum concentration, a precipitate would be formed, which would further maintain the transmembrane concentration gradient of the unionized weak base. For example, the pKa of doxorubicin is 8.68, and when the pH inside the liposomes is 3.6, the concentration of the ionized doxorubicin is 120,000 times higher than the unionized moiety. However, if the pH of the extra liposomal medium is fixed at 8.68, the initial concentration of unionized and ionized doxorubicin will be the same, and there is a large transmembrane concentration gradient of unionized doxorubicin. The driving force will not disappear until the inside concentration of the unionized doxorubicin is equal with the outside. As a result, the EE of doxorubicin is usually over 90% using an ammonium sulphate gradient. However, in the case of gemcitabine with a pKa of 3.6, even if the internal pH of the liposomes reaches 3.6, the concentration ratio of unionized and ionized gemcitabine would be 1:1. If the external pH of the liposomes was adjusted to 7, the concentration ratio of the unionized to ionized gemcitabine would be 2500:1 (the ionized species is negligible). When the equilibration is achieved, the concentration of unionized gemcitabine in the liposomal core is equal to that in the outside media. Therefore, the total concentration of gemcitabine (ionized and unionized) in the liposomes will only be twice that in the external medium, which would be too low to precipitate, hence the driving force with precipitation of inner gemcitabine does not exist. This assumption also explains why the EE for remote loading was 2 times higher compared to passive loading, TFH, without ammonium sulphate (12.4 ± 0.4% versus 5.7 ± 0.2%).
As reported in the current literature, a pKa ≤ 11 is only one prerequisite when ammonium sulphate is used for the remote loading of a weak base (23,25). There must be a minimum pKa limit for the candidate to achieve an acceptable EE. Since ammonium sulphate can only reduce the pH to 3.6 (24), a minimum pKa value of 4.6 for basic drugs will be needed to maintain the majority (≥ 90) of the drug molecules to be ionised and locked in the liposomal aqueous cores. The release study also highlighted the important role of osmotic pressure on gemcitabine release. Higher intra-liposomal osmotic pressure generated by 250 mM ammonium sulphate (550 mOsm) and loaded gemcitabine (SVI2) caused a burst release of gemcitabine. Therefore, precipitation of loaded drug in the liposome aqueous core is desirable to reduce the intra-liposomal osmotic pressure to prevent drug leakage.
In this study, a novel method named small volume incubation (SVI), where a small volume of condensed drug solution was used for drug loading, was found to be effective in incorporating the drug in the liposome. Based on this observation, the mechanism for drug loading was considered to be passive diffusion. In this case the drug loading will reach maximum when the drug concentration gradient cross the bilayers is zero. Therefore the EE will be determined by the ratio of the volume of the inner aqueous core, Vin, to the volume of the external medium, Vex. After equilibration of the system, the EE of any drug can be calculated according to Eq. 6 (20).
As reported, if the total lipid of unilamellar liposomes is fixed, the V in is proportional to the vesicle particle size (20). This is why the reverse evaporation method gave a high EE with giant liposomes, but reduced in size was reduced by extrusion. The small volume incubation method minimizes the external volume of the drug solution to achieve a higher EE. The less the external volume, the higher the EE will be. The small volume incubation method is a passive loading process, which can increase the EE of drugs with high water solubility. In contrast using the REV method to increase the EE of gemcitabine to 67% (10), usually resulted in liposomes of more than 1,000 nm (without extrusion) with an unacceptable Polydispersity Index over 0.5. A particle size of 1,000 nm is not acceptable due to its quick clearance from the bloodstream and the loss of its EPR effect.
The rapid release of gemcitabine from liposomes prepared via remote loading may be explained by the high osmotic pressure of the inner aqueous core, 550 versus 290 mOsm for the release medium. The higher osmotic pressure inside the liposome may cause it to swell due to the influx of water, and thus cause leakage of the gemcitabine. The data showed Fickian transport for gemcitabine, indicating that the gemcitabine gradient across the bilayers is the crucial factor controlling drug release. For the in vivo evaluation, a slower drug release is preferred in order to deliver more drugs to the tumour and limit entry to the healthy tissues.
The physicochemical stability of the liposome stored in the form of pellet was equal with suspensions. However, less drug leakage was expected from the pellet than from the suspensions, which could be predicted with the drug release data (Fickian transport).
In the cytotoxicity study, the free gemcitabine plus empty liposome was used as a reference to evaluate the importance of drug loading. In other words, if gemcitabine was not loaded and maintained in the liposome, the mixture of these two did not enhance the cytotoxicity of gemcitabine. For the liposome prepared by remote loading and SVI1 method with low gemcitabine concentration (25 mM, 20 μl), the cytotoxicity was similar to that of the empty liposome plus free gemcitabine, whereas the liposomes prepared by remote loading were even less cytotoxic, possibly due to the rapid leakage caused by higher internal osmotic pressure (550 mOsm, 250 mM ammonium sulphate). As liposomes are considered to be taken up via energy-mediated endocytosis, followed by release of drug from the endosome, allowing an efficient delivery to the cytoplasm and consequently the nucleus (39,40), a higher drug loading means a greater amount of drug could be taken up by the cell using the same amount of energy. This is consistent with other reports (15,16). Furthermore, according to the release study, a high drug loading can generate a greater gemcitabine gradient, resulting in a sustained drug release rate. Therefore, the current study highlighted that a high drug loading has both increased the economic implication in the manufacture and implication in the cytotoxicity.
CONCLUSIONS
This is the first study demonstrating that the remote loading method using ammonium sulphate gradient is not effective to increase EE for basic drugs with a low pKa, such as gemcitabine. Furthermore, the ammonium sulphate in the liposomes core caused rapid drug leakage due to the higher osmotic pressure. The minimum pKa of weak bases for remote loading should be > 3.6 to achieve at least a 2-fold increase in EE, compared to normal passive loading. pKa > 4.6 and intra-liposomal precipitation of loaded compounds were suggested in order to achieved higher EE and avoid burst release caused by ammonium sulphate (250 mM, 550 mOsm). Although the freeze-thaw effect on liposome size has been reported, the ability to remove micelles in the presence of a high ratio of PEGylated lipid is a novel finding. Liposomes with high content of gemcitabine (4.0%, w/w) and acceptable size were obtained with the new Small Volume Incubation method. The present in vitro study also indicated that high drug content in the liposomes is vital to improve gemcitabine’s cytotoxicity in resistant pancreatic cancer cell lines. Therefore the high drug-loaded liposomes deserve further investigation.
Abbreviations
- DL:
-
Drug loading
- EE:
-
Entrapment efficiency
- MDR:
-
Multidrug resistance
- MTT:
-
3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyl-tetrazolium bromide
- PEG:
-
Polyethylene glycol
- REV:
-
Reverse phase evaporation
- SVI:
-
Small volume incubation
- TFH:
-
Thin film hydration
REFERENCES
Toscbi L, Finoccbiaro G, Bartolini S, Gioia V, Cappuzzo F. Role of gemcitabine in cancer therapy. Future Oncol. 2005;1:7–17.
Hilbig A, Oettle H. Gemcitabine in the treatment of metastatic pancreatic cancer. Expert Rev Anticancer Ther. 2008;8:511–23.
Mylonakis N, Athanasiou A, Ziras N, Angel J, Rapti A, Lampaki S, et al. Phase II study of liposomal cisplatin (LipoplatinTM) plus gemcitabine versus cisplatin plus gemcitabine as first line treatment in inoperable (stage IIIB/IV) non-small cell lung cancer. Lung Cancer. 2010;68:240–7.
Abbruzzese JL, Grunewald R, Weeks EA, Gravel D, Adams T, Nowak B, et al. A phase I clinical, plasma, and cellular pharmacology study of gemcitabine. J Clin Oncol. 1991;9:491–8.
Storniolo AM, Allerheiligen SR, Pearce HL. Preclinical, pharmacologic, and phase I studies of gemcitabine. Semin Oncol. 1997;24:S7-2–7.
Kohne AKC-H, Haufe TFJPT, Schleyer PGGEE. Pharmacokinetics of gemcitabine in a patient with end-stage renal disease: effective clearance of its main metabolite by standard hemodialysis treatment. Cancer Chemother Pharmacol. 2003;51:266–70.
Kuenen BBC, Rosen L, Smit EF, Parson MRN, Levi M, Ruijter R, et al. Dose-finding and pharmacokinetic study of cisplatin, gemcitabine, and SU5416 in patients with solid tumors. J Clin Oncol. 2002;20(6):1657–67.
Ali S, Ahmad A, Banerjee S, Padhye S, Dominiak K, Schaffert JM, et al. Gemcitabine sensitivity can be induced in pancreatic cancer cells through modulation of miR-200 and miR-21 expression by curcumin or its analogue CDF. Cancer Res. 2010;70(9):3606–17.
Celia C, Grazia M, Paolino CD, Bulotta S, Ventura CA, Russo D, et al. Improved in vitro anti-tumoral activity, intracellular uptake and apoptotic induction of gemcitabine-loaded pegylated unilamellar liposomes. J Nanosci Nanotechnol. 2008;8:2102–13.
Kim I-Y, Kang Y-S, Lee DS, Park H-J, Choi E-K, Oh Y-K, et al. Antitumor activity of EGFR targeted pH-sensitive immunoliposomes encapsulating gemcitabine in A549 xenograft nude mice. J Control Release. 2009;140:55–60.
Federico C, Morittu VM, Britti D, Trapasso E, Cosco D. Gemcitabine-loaded liposomes: rationale, potentialities and future perspectives. Int J Nanomedicine. 2012;7:5423–36.
Suzuki R, Takizawa T, Kuwata Y, Mutoha M, Ishiguro N, Utoguchi N, et al. Effective anti-tumor activity of oxaliplatin encapsulated in transferrin–PEG-liposome. Int J Pharm. 2008;346:143–50.
Barenholz Y. Liposome application: problems and prospects. Curr Opin Colloid Interface Sci. 2001;6:66–77.
Slepushkin VA, Simões S, Dazin P, Newman MS, Guo LS, Pedroso de Lima MC, et al. Sterically stabilized pH-sensitive liposomes. J Biol Chem. 1997;272(4):2382–8.
Lee RJ, Low PS. Folate-mediated tumor cell targeting of liposome-entrapped doxorubicin in vitro. Biochim Biophys Acta. 1995;1233:134–44.
K-i O, Una K, Minatoa K, Tanakab K-i, Higakia K, Kimura T. Determinants for in vivo anti-tumor effects of PEG liposomal doxorubicin: importance of vascular permeability within tumors. Int J Pharm. 2008;359:234–40.
Graeser R, Bornmann C, Esser N, Ziroli V, Jantscheff P, Unger C, et al. Antimetastatic effects of liposomal gemcitabine and empty liposomes in an orthotopic mouse model of pancreatic cancer. Pancreas. 2009;38:330–7.
Cosco D, Bulotta A, Ventura M, Celia C, Calimeri T, Perri G, et al. In vivo activity of gemcitabine-loaded PEGylated small unilamellar liposomes against pancreatic cancer. Cancer Chemother Pharmacol. 2009;64:1009–20.
Celano M, Calvagno MG, Bulotta S, Paolino D, Arturi F, Rotiroti D, et al. Cytotoxic effects of Gemcitabine-loaded liposomes in human anaplastic thyroid carcinoma cells. BMC Cancer. 2004;4(63):1–5.
Xua X, Khanb MA, Burgessa DJ. Predicting hydrophilic drug encapsulation inside unilamellar liposomes. Int J Pharm. 2012;432:410–8.
Bansal SS, Celia C, Ferrati S, Zabre E, Ferrari M, Palapattu G, et al. Validated RP-HPLC method for the simultaneous analysis of gemcitabine and LY-364947 in liposomal formulations. Curr Drug Targets. 2013;14:1–9.
Hong M-S, Lee SJ, Oh Y-K, Kim C-K. pH-sensitive, serum-stable and long-circulating liposomes as a new drug delivery system. J Pharm Pharmacol. 2002;54:51–8.
Zucker D, Marcus D, Barenholz Y, Goldblum A. Liposome drugs’ loading efficiency: a working model based on loading conditions and drug’s physicochemical properties. J Control Release. 2009;139:73–80.
Bolotin EM, Cohen R, Bar LK, Emanuel N, Ninio S, Lasic DD, et al. Ammonium sulfate gradients for efficient and stable remote loading of amphipathic weak bases into liposomes and ligandoliposomes. J Liposome Res. 1994;4(1):455–79.
Cern A, Golbraikh A, Sedykh A, Tropsha A, Barenholz Y, Goldblum A. Quantitative structure -property relationship modeling of remote liposome loading of drugs. J Control Release. 2011. doi:10.1016/j.jconrel.2011.11.029.
Paolino D, Cosco D, Racanicchi L, Trapasso E, Celia C, Iannone M, et al. Gemcitabine-loaded PEGylated unilamellar liposomes vs GEMZAR®: biodistribution, pharmacokinetic features and in vivo antitumor activity. J Control Release. 2010;144:144–50.
Cosco D, Paolino D, Cilurzo F, Casale F, Fresta M. Gemcitabine and tamoxifen-loaded liposomes as multidrug carriers for the treatment of breast cancer diseases. Int J Pharm. 2012;422:229–37.
Calvagno MG, Celia C, Paolino D, Cosco D, Iannone M, Castelli F, et al. Effects of lipid composition and preparation conditions on physical-chemical properties, technological parameters and in vitro biological activity of gemcitabine-loaded liposomes. Curr Drug Deliv. 2007;4:89–101.
Møkleby T. Active loading of gemcitabine into liposomes [Master]. University of Tromsø; 2009.
Gravem H. Gemcitabine-containing liposomes. University of Tromsø; 2006.
Vali AM, Toliyat T, Shafaghi B, Dadashzadeh S. Preparation, optimization, and characterization of topotecan loaded PEGylated liposomes using factorial design. Drug Dev Ind Pharm. 2008;34:10–23.
El-Gibaly I, Abdel-Ghaffar SK. Effect of hexacosanol on the characteristics of novel sustained-release allopurinol solid lipospheres (SLS): factorial design application and product evaluation. Int J Pharm. 2005;294:33–51.
Costa P. An alternative method to the evaluation of similarity factor in dissolution testing. Int J Pharm. 2001;220:77–83.
Maruyama K. Intracellular targeting delivery of liposomal drugs to solid tumors based on EPR effects. Adv Drug Deliv Rev. 2011;63:161–9.
Juliano RL, Stamp D. The effect of particle size and charge on the clearance rates of liposomes and liposome encapsulated drugs. Biochem Biophys Res Commun. 1975;63(3):651–8.
Zhanga T, Li Y, Mueller A. Phase structure of liposome in lipid mixtures. Chem Phys Lipids. 2011;164:722–6.
Garbuzenko O, Barenholz Y, Priev A. Effect of grafted PEG on liposome size and on compressibility and packing of lipid bilayer. Chem Phys Lipids. 2005;135:117–29.
Cui J, Li C, Guo W, Li Y, Wang C, Zhang L, et al. Direct comparison of two pegylated liposomal doxorubicin formulations: is AUC predictive for toxicity and efficacy? J Control Release. 2007;118:204–15.
Kirkham M, Parton RG. Clathrin-independent endocytosis: new insights into caveolae and non-caveolar lipid raft carriers. Biochim Biophys Acta. 2005;1745:273–86.
Huang RB, Mocherla S, Heslinga MJ, Charoenphol P, Eniola-Adefeso O. Dynamic and cellular interactions of nanoparticles in vascular-targeted drug delivery. Mol Membr Biol. 2010;27:190–205.
ACKNOWLEDGMENTS AND DISCLOSURES
The financial support for this study was provided by New Zealand Cancer Society (Grant Number 3627223). The authors also wish to acknowledge the support of a Doctorial Scholarship for Hongtao Xu provided by The University of Auckland, New Zealand. The authors declare that they have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Xu, H., Paxton, J., Lim, J. et al. Development of High-Content Gemcitabine PEGylated Liposomes and Their Cytotoxicity on Drug-Resistant Pancreatic Tumour Cells. Pharm Res 31, 2583–2592 (2014). https://doi.org/10.1007/s11095-014-1353-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-014-1353-z