Abstract
Purpose
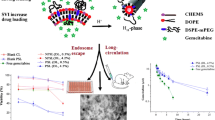
PEGylated pH-sensitive liposomes (PSL) dual-loaded with gemcitabine and curcumin were investigated for the potential application in gemcitabine-resistant pancreatic ductal adenocarcinoma (PDAC) treatment. Curcumin was employed as an inhibitor of the efflux transporter, multidrug resistance protein 5 (MRP5) in PDAC cells.
Methods
Liposomes were prepared with gemcitabine in the core and curcumin in the bilayers. The effects of curcumin on pH-sensitivity and ‘endosome escape’ of PSL with different PEGylation were investigated using a calcein self-quench assay. The effects of curcumin on intracellular gemcitabine concentrations, and cytotoxicity to a MIA PaCa-2 PDAC cell line was evaluated. The pharmacokinetics were investigated in rats following intravenous injection.
Results
The addition of curcumin to the PSL bilayers (0.2-1 mol%)slightly decreased the pH-sensitivity of PSL, but to a less extent than PEGylation (0–5 mol%). Co-treatment with curcumin increased gemcitabine cellular accumulation in a concentration-dependent manner, and resulted in synergistic cytotoxicity towards MIA PaCa-2cells.Both these effects were augmented by the use of PSL, particularly when the two drugs were co-loaded in PSL. In rats, the dual-drug loaded PSL produced significantly reduced (p < 0.05) plasma clearance (CL) and volume of distribution (Vd) for both drugs, alongside 3 to 4-fold increases in the area-under-the-concentration-time curves compared to the free drugs. Additionally, curcumin slightly increase the plasma concentrations of gemcitabine possibly also via the MRP5 inhibition effect.
Conclusion
Co-delivery of curcumin with gemcitabine using PSL not only increased the intracellular gemcitabine concentration thus cytotoxicity to MIA PaCa-2 cells but also significantly improved the pharmacokinetic profiles for both drugs.

Graphical Abstract
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic ductal adenocarcinoma (PDAC), comprising 90% of pancreatic cancer, is a highly aggressive tumour with a 2–9% five-year survival rate (1). The poor prognosis is mainly due to its metastatic nature and a low response to chemotherapies (2).The rapid development of multidrug resistance (MDR) is another major contributing factor to chemotherapeutic failure (3, 4). A commonly reported mechanism for MDR involves high expression of ATP-binding cassette (ABC) efflux transporters, such as P-glycoprotein (P-gp), and multidrug resistance proteins 1–9 (MRP1 - MRP9) (5) which facilitate the efflux of anticancer drugs from cancer cells (3, 4). Furthermore, ABC transporters also play a potential role in cancer development and progression (6). Therefore, targeting ABC transporters is important to develop more effective tumour therapies.
Gemcitabine, a nucleoside analogue, is the first-line chemotherapy for the treatment of PDAC. After administration, gemcitabine (prodrug) is phosphorylated in the cell to its active moieties which inhibits DNA synthesis (7, 8). However, before reaching its target, about 90% of it is rapidly inactivated by cytidine deaminase, resulting in a short half-life ranging from 32 to 94 min in patients (8). Moreover, the rapid development of chemoresistance has been common (9): although gemcitabine can enter cells, the drug may be ejected by the ABC transporters, leading to insufficient intracellular concentrations at its DNA target (6, 10, 11). Thus it is essential to deliver a large dose to the cancer cells, overwhelming the efflux transporters.
Curcumin is a naturally occurring polyphenolic compound found in the rhizomes of Curcuma longa. It has intrinsic anticancer activity (12, 13) and is capable of reversing chemoresistance, such as vincristine ingastric carcinoma SGC7901 (14) and vinblastine in KB-V1 cells by decreasing P-gp expression and function (15, 16). In a phase II clinical study, oral administration of curcumin increased the response rate to gemcitabine treatment in patients with advanced pancreatic cancer without causing toxicity (17). However, curcumin has a low water solubility (log P 2.5) and poor in vivo stability which limited its bioavailability and subsequently the anticancer effect (12, 18). Curcumin is reported to sensitize pancreatic cancer cells to gemcitabine via modulation of micro RNAs, such as miR-200 and miR-21, which play important roles in cancer recurrence and anti-apoptotic effects (9).Therefore,curcumin has been employed as a chemo-sensitizing agent in combination with anti-cancer drugs delivered using different nanomedicine platforms to improve treatment of various cancers (19) . Previously, over-expression of MRP5 efflux transporters has been reported to be associated with gemcitabine resistance in PDAC and lung cancer cells (5, 20, 21). Paxton’s group confirmed the over-expression of MRP5 in PDAC cell models (PANC-1 and MIA PaCa-2) decreased cellular accumulation and sensitivity to gemcitabine. However, these deficits were reversed by inhibition of MRP5 with curcumin (22).
Liposomes, considered to be the most versatile drug carriers capable of incorporating both hydrophilic and lipophilic compounds, have been intensively investigated for anti-cancer drug delivery (23,24,25). Since the discovery by Alec Bangham in the1960s (26), liposomes have undergone significant refinement, particularly with the PEGylation technology– the surface coating with polyethylene glycol (PEG) polymers (27,28,29,30). Liposomal nanoparticles can be internalized into cells via endocytosis, delivering a large payload to the cancer cells (8, 31).A distinct advantage of liposomes is that they may carry multiple drugs (such as gemcitabine and curcumin) in the same systems, synchronizing the drug pharmacokinetics at the systemic and even cellular level (32). However, after endocytosis, the traditional non-pH-sensitive liposome (NPSL) can be entrapped in the endosomes and, within 35 min, transferred to lysosomes (33). This process may reduce the extent of intracellular drug availability to its site of action, such as DNA, both due to the ‘entrapment’ and the degradation by lysosomal enzymes (33, 34). To circumvent this limitation, pH-sensitive liposomes (PSL) have been suggested as an approach to enhance the cytoplasmic delivery via ‘endosome escape’ (11, 12). PSLs are stable at neutral pH but destabilize under acidic conditions, for example, in endosomes or lysosomes (pH 5–5.5), (35, 36). To prevent the rapid clearance of PSL by the reticulo-endothelial system, same as to conventional liposomes, PEGylation is required to provide steric inhibition of opsonization, increasing the circulation time (37). A long half-life >6 h is considered to be vital to achieve tumour targeting (38). However, PEGylation can remarkably reduce the pH-sensitivity of the PSL (39). Therefore, the PEGylation degree of PSL should be leveraged for both long circulation and pH-sensitivity.
In this study, a PSL delivery system with an optimal degree of PEGylation, was designed for dual delivery of gemcitabine and curcumin to potentize gemcitabine treatment of PDAC. It was hypothesized that after systemic delivery, superior intracellular drug delivery would be achieved through endosome escape of PSL. Then, curcumin, would inhibit MRP5-mediated gemcitabine efflux, and thus maintain the cellular concentration of gemcitabine at a lethal level. To determine the PEGylation degree of PSL, a calcein leakage assay (39) was employed to investigate the pH-sensitivity of various PEGylated PSLs. The effects of curcumin on the pH-sensitivity of PSL, cellular concentration and cytotoxicity of gemcitabine were evaluated in a MIA PaCa-2 cell line, which was proven to over-express MRP5 (21). Finally, the pharmacokinetics of liposomal formulations were compared with free drug solutions in rats.
Materials and Methods
Materials
To prepare PSL, 1,2-dioleoyl-sn-glycero-3-phosphoethanolamine (DOPE), cholesteryl hemisuccinate (CHEMS), and N-(carbonyl-methoxypolyethylene-glycol-2000)-1,2-distearoyl-sn-glycero-3-phospho-thanolamine (DSPE-mPEG2000) were purchased from Avanti Polar Lipids (Alabama, USA). For preparation of NPLS, phospholipid 1,2-dipalmitoyl-sn-glycero-3-phospocholinemonohydrate (DPPC) was gift from Lipoid (Steinhausen, Switzerland). Gemcitabine (purity >98%), curcumin (purity >80%), cholesterol, and 3-(4, 5-dimethylthiazol-2-yl)-2, 5-diphenyl-tetrazolium bromide (MTT) for cytotoxicity studies were purchased from Sigma (Auckland, New Zealand). The MIA PaCa-2 cell line was from the Auckland Cancer Society Research Centre, University of Auckland. Milli-Q water was prepared using a water purification system (Millipore Corp., Bedford, USA). All the other chemical materials were of analytical grade.
Sprague-Dawley (SD) rats of 6–8 weeks were used in the pharmacokinetic study which was conducted at the Vernon Jansen Unit, The University of Auckland. Animals were handled according to the standards relating to the care and management of experimental animals of New Zealand. The experimental protocol was approved by the University’s Animal Experiment Committee (ethics number 001228).
Preparation of Gemcitabine and Curcumin Loaded PSL
PSL with or without PEGylation (DOPE: CHEMS: DSPE-mPEG2000 at molar ratios of 6:4:0, 6:4:0.3 or 6:4:0.5) were prepared using the thin-film hydration extrusion method (40). Conventional non-pH sensitive liposomes (NPSL) were composed of DPPC: cholesterol: DSPE-mPEG2000 at molar ratios 6:3:0.28.
Firstly, the mixture of lipids including DSPE-mPEG2000 (10 mg) with curcumin (0, 0.1, 0.05, or 0.025 mg for investigation of its influence on the pH-sensitivity and 0.2 mg in dual-drug loaded PSL) was dissolved in 1 ml of solvent, a mixture of chloroform: methanol (volume ratio 3:1). The organic solvent was then removed using an R-215rotary evaporator under vacuum conditions (Büchi, Switzerland). The resulting lipidic thin-film was hydrated using 1 ml of phosphate buffer solution (PBS) (10 mM, pH 7.4) and extruded through polycarbonate membranes with pore size 400 nm and 200 nm with a stainless steel Avanti Polar extruder. The liposomes were pelleted by ultra-centrifuged at 186,000 g at 4°C for 1 h.
In addition to the above “pre-insertion” technique, post-insertion was also applied to PEGylate curcumin-loaded PSL and NPSL as it potently enhance the long-circulation property and pH-sensitivity (39). Briefly, DSPE-mPEG2000 in aqueous solutions (possibly micelles) prepared using thin-film hydration method was added to preformed non-PEGylated liposomes and incubated for 1 h. Drug loading efficiency and PEGylation degree were compared to determine the suitable PEGylation method.
Gemcitabine was loaded into the above liposomes using the Small Volume Incubation (SVI) method previously reported (31). By taking advantage of the small molecule size of gemcitabine which enables the drug to diffuse into liposomes, this method improved the drug loading efficiency by increase the trans-liposomal drug concentration gradient. Briefly, a 20 μl aliquot of gemcitabine isotonic solution (25 mmol or 0.3 mg) in PBS (10 mM, pH 7.4; adjusted to 320 mOsm with sodium chloride) was added to the liposomal pellet. After vortexing to suspend the liposomes in the drug solution, the mixture was kept at 60°C for 3 h. By reducing extra−/intra liposomal aqueous phase volume ratio during the drug loading process, a relatively high entrapment efficiency (EE) for gemcitabine was obtained (31).
Characterization of Calcein, Gemcitabine, and Curcumin Loaded PSL
The particle size, and distribution (indicated by the polydispersity index; PDI), zeta potential of drug-loaded liposomes were measured by a Nano-ZS Zetasizer based on dynamic light scattering (Malvern Instruments Ltd., UK). Milli-Q water at 25°C was used as dilution media. Measurement was performed in triplicate to obtain the average values.
To observed the liposomal morphology, one drop of liposome suspension (0.2 mg/ml of lipids in PBS) was placed on a 3 mm 200-mesh copper grid, and stained with a 2% uranyl acetate solution. After a 2 min incubation, the surplus was removed by filter paper. The sample was then dried at room temperature before examined using a transmission electron microscope (TEM) (FEI Tecnai G2 Spirit Twin 120Kv).
To determine the EE and drug loading content (DL), a gel-filtration method based on a Sephadex G50 column (bead size 20–80 μm, Sigma) was used to separate liposomes from un-encapsulated drug(s). To determine the drug mass encapsulated in liposomes (Min), an aliquot of 100 μl filtered liposome suspension was taken and dissolved with 900 μl of 10% Triton-X100. The released gemcitabine and curcumin was analysed using a validated reversed phase HPLC (40). The EE and DL were obtained using the following equations:
Where; Mtotalis the total drug mass used in preparation and Mlipis the mass of drug loaded liposomes.
pH-Sensitivity of the Liposomal Bilayers
The PSLs were prepared as described above except that a concentrated calcein solution (80 mM in PBS) was used to hydrate the thin-films. The DPPC based NPSL were used as a reference formulation. The un-entrapped calcein was removed by a Sephadex G50 column. A calcein self-quenching assay was used to investigate the effect of the addition of curcumin and PEGylation (DSPE-mPEG2000 3% versus 5%) on the pH-sensitivity of the resulting PSL (41). Calcein is self-quenching with a ‘bell-shaped’ fluorescence-concentration profile. Strong fluorescence intensities were found when concentrations reduced, approximately proportional to the concentrations in the range of 0.1–10 μM (42). Thus the leaked calcein from the liposome diluted by the medium sufficiently will result in an increase in fluorescence.
Briefly, after Sephadex G50 column filtration, 100 μL of calcein loaded liposome sample was collected and mixed with 900 μL PBS (0.15 M with 1 mM EDTA) at different pH levels (5.0 to 7.4). After incubation at 37°C for 10 min, 200 μL of the mixture containing release calcein was transferred to a 96-well plate, and fluorescence was measured with a plate reader (Ex/Em: 470/509 nm). The total fluorescence was obtained by destroying the liposome with 10% of Triton-X 100 and then diluted with PBS (7.4) 100 times. To correct the pH effect on the fluorescent intensity, standard curves (0.1–5 μM) were prepared at the corresponding PBS for the determination of the amount of calcein. The percent release, R (%), was calculated as follows:
where M7.4 was the mass of calcein released at pH 7.4, MpH was the mass released into each of acidic buffers, and M100% was the mass of the total calcein entrapped in the liposomes.
Curcumin Effect on Gemcitabine Cellular Accumulation in MIA PaCa-2 Cells
To evaluate the MRP5 inhibitory effect of curcumin on the cellular accumulation of gemcitabine, a MIA PaCa-2 cell line that had been previously demonstrated to over-express MRP5 was used (22). The cells were maintained in a Dulbecco’s Modified Eagle’s Medium (DMEM) supplemented with 10% fetal bovine serum, 100 UI/ml penicillin, and 100 μg/ml streptomycin in complete DMEM. The cells were seeded into a 6-well plate at a density of 8 × 106 cells/2 ml/well. Following an incubation at 37°C for 24 h, cells were treated with 1 ml complete DMEM containing free gemcitabine at a fixed concentration (100 μM) and curcumin at different concentrations (0–100 μM) either in liposomes or as solutions pre-dissolved in 1% DMSO. A gemcitabine solution, rather than liposomal formulation, was used to avoid any influence of the liposome on the cellular uptake of gemcitabine. After 3 h incubation, the cells were washed 3 times with PBS. The washed cells were lysed with 1.5 ml ethanol with the aid of sonication for 30 min to extract the intracellular gemcitabine. The lysates were centrifuged at 125 × g for 5 min, the supernatant was collected, evaporated to dryness using a concentrator, and the residue re-dissolved with 100 μl of a 10% Triton-X100 solution and vortexing for 3 min. After further centrifugation, the supernatant was analyzed for gemcitabine by HPLC (31). Experiments were conducted in triplicate.
A preliminary MTT study showed no toxicity to the cells following the treatment with all the formulations at these concentration levels for 3 h.
In Vitro Drug Release Profiles
The release profiles from the gemcitabine-curcumin dual-loaded PSL were investigated using cellulose acetate dialysis bags (MWCO 12–14 kDa). Liposomes (from 20 mg lipids)were suspended in 1 ml PBS (pH 7.4)were dialyzed against 50 ml of the release medium phosphate buffer(50 mM, pH 7.4, 320 mOsm) which was maintained at 37°C. At different time intervals, 10 μl of the liposomal sample was withdrawn from the dialysis bags, dissolved in a 10% Triton-X100 solution, and analyzed with HPLC (40) to determine the drug released. The Ritger-Peppas model was used to investigate the drug release kinetics (43, 44):
where \( \frac{M_t}{M_{\infty }} \) represents the proportion of drug released at time t with a release rate constant; K. The n value stands for the diffusion exponent, with n ≤ 0.43 indicating a Fickian diffusion from the carriers dominates, whereas; 0.43 ≤ n ≤ 0.85 denotes a non-Fickian transport dominates; and n ≥ 0.85, a zero-order drug release mechanism.
In Vitro Cytotoxicity
The MTT cell viability assay was used to evaluate the cytotoxic effects of various liposome formulations in the MIA PaCa-2 cells. The PSL with a PEGylation degree of 3% was used in this study. Cells were seeded in a 96-well plate at 5000 cells/well and incubated for 24 h in phenol-red free DMEM. Cells in each well (n = 3) were treated with PSL loaded with gemcitabine or curcumin, or both (curcumin to gemcitabine molar ratio 1:1, approximately 1.5:1 w/w).The free drugs and blank liposomes were used as references. Following treatment for 24, 48, and 72 h, the medium was removed and the cells washed with PBS prior to MTT cell viability assay. Samples were read at 540 nm on a plate reader (Molecular Devices, USA). The background absorbance from the medium was subtracted, and cell viability was calculated as % of the control (medium treated) cells. The experiments were run in duplicate.
Pharmacokinetics
The pharmacokinetics of gemcitabine and curcumin co-loaded in PSL (PEGylated with 3% mol DSPE-mPEG2000) was investigated following intravenous (i.v.) administration with a solution containing free drugs as a reference. To investigate the potential effect that curcumin on the pharmacokinetics gemcitabine, a gemcitabine alone solution was added as a control.
Twelve SD rats (male; weighting 200 ± 5 g) were randomly divided into three formulation groups (n = 4); dual-drug loaded PSL, free drug combination in solution and a free gemcitabine solution. Each formulation (1 mL) was injected via the tail vein at an equivalent dose of 1 mg/kg gemcitabine and 1.2 mg/kg curcumin. Blood samples (100–200 μl) were collected from the tail vein before injection and at 0, 15 min, 30 min, and up to 24 h following injection. Animal behaviours were closely monitored for any signs of stress or systemic toxicity.
After centrifugation, the plasma (50 μl) was mixed with 0.5 ml acetonitrile. After mixing by vortexing for 3 min, the proteins were precipitated, and sample was centrifuged. The supernatant was collected. The precipitant was mixed with a further 0.5 ml acetonitrile and the extraction process repeated. The combined supernatants were evaporated to dryness using a concentrator and the residue was dissolved with 50 μl Triton-X100 solution (10%) by vortexing for 3 min. After centrifugation to remove the particulate matters, the supernatant was subjected to HPLC analysis. The gradient method for the simultaneous determination of gemcitabine and curcumin (40) was used. No interference was observed from the plasma and the extraction recovery of each concentration was >95% for both gemcitabine and curcumin. The assay was linear in the concentration range of 0.1–10 μM for both drugs with satisfactory intra- and inter-day precision and accuracies (40).
The non-compartmental model was used to calculate the pharmacokinetic parameters for gemcitabine and curcumin using WinNonlin® version 5.3 (Pharsight, Mountain View, USA).
Statistical Analysis
Data are expressed as means ± standard deviation (SD). The one-way Analysis of Variance (ANOVA) with Tukey’s multiple comparisons was used for statistical analysis using Origin 8.0 software with p value 0.05 set for significance.
Results
In this study, various PEGylated liposomes were successfully prepared with thin-film hydration with DSPE-mPEG2000 added in the lipid phase (pre-insertion method). It is worth noting that the “post-insertion” technique was also applied to PEGylate curcumin-loaded PSL and NPSL as this approach would leverage the long-circulation property and pH-sensitivity better than the pre-insertion method (39). However, when incubating liposomes with the DSPE-mPEG2000 solution (possibly micelles), there was a significant relocation of curcumin from the liposome bilayer to the micelles. Furthermore, the attachment efficiency of the DSPE-mPEG2000 was reduced to an unacceptable level (< 20%). Therefore, the post-insertion technique was dropped.
Characterization of Gemcitabine and Curcumin Loaded PSL
With the modified SVI method, EE for gemcitabine of 35.1 ± 0.5% and 92 ± 1% for curcumin was obtained. This is much higher compared to 5.5% EE for gemcitabine previously reported using either a thin film hydration extrusion or reverse-phase evaporation method (31)).The PSL had a uniform particle size and a slightly negative zeta potential (Table I). DL (w/w) was 0.5 ± 0.01% (1.7 ± 0.02%, in molar ratio) and 0.9 ± 0.02% (2.7 ± 0.01%, in molar ratio) for gemcitabine and curcumin, respectively. As shown in Fig. 1, the resulting PSL were unilamellar with their size corresponding to that obtained by the particle analyzer. In addition, encapsulation of gemcitabine, curcumin, or calcein did not alter the PSL’s particle size.
Effects of Curcumin Incorporation and PEGylation on pH-Sensitivity
As shown in Fig. 2A, the addition of curcumin (DL, 0.25–1%) decreased the pH-sensitivity of the liposomes when pH < 6.0 in a DL dependent manor (p < 0.05).
The PEGylation with DSPE-mPEG2000 was demonstrated to have a stronger effect in reducing the PSL pH-sensitivity, compared to the presence of curcumin in the membrane(Fig. 2). Increasing PEG density from 3% to 5% reduced the pH-responsiveness at pH 5.5–6 but not at pH 5. Addition of curcumin to the bilayers, however, only showed little negative effect the pH-sensitivities of the PEGylated PSLs investigated.
Based on these results, PSL with 3% mol DSPE-mPEG2000 was finalized for the next in vitro and in vivo studies.
Effect of Curcumin on the Cellular Accumulation of Gemcitabine in MIA PaCa-2
The effect of curcumin loaded PSL, NPSL (both with 3% PEGylation), water solution, and blank liposomes on gemcitabine accumulation were evaluated using MIA PaCa-2 cells. As shown in Fig. 3, the accumulation of gemcitabine increased with the increase in curcumin concentration, for all curcumin formulations. In addition, the ability of the curcumin formulations to enhance the cellular accumulation of gemcitabine was ranked as PSL > solution > NPSL at high concentrations. However, at low concentrations NPSL were superior to PSL, however at 50 and 100 μM, curcumin in PSL increased cellular accumulation of gemcitabine about 30 times, compared to a 5-time increase by non pH-sensitive liposomal curcumin.
Interestingly, the blank liposome also increased gemcitabine cellular accumulation at high lipid concentrations (equal to the lipid concentration of liposomes containing curcumin 50–100 μM) (p < 0.0001).
In Vitro Drug Release Profiles
The release of gemcitabine and curcumin from PSL followed a similar trend with gemcitabine approximately 10% slower than curcumin at each of the time points over 24 h (Fig. 4).
For both gemcitabine and curcumin, exponents (n) from the Ritger-Peppas equation were below 0.43, indicating a Fickian diffusion mechanism predominated.
Combination Effect of Curcumin on Cytotoxicity of Gemcitabine
A strong gemcitabine-resistance was observed in the MIA PACa-2 cells with no significant cytotoxic effects (cell viability >96%) even at the concentration up to 25 μM after 24 h exposure to free drug (Fig. 5). In contrast, all other treatments with PSL loaded with gemcitabine or curcumin or both drugs led to great decrease in cell viability (30–70%) in a dose dependent manner.
Comparative cytotoxic effects (MTT cell viability)of various gemcitabine and curcumin formulations alone or in combinations to MIA PaCa-2 after exposure for different time: (A) 24 h, (B) 48 h and (C) 72 h. Results are mean ± SD, n = 6, from two independent experiments. The DL (w/w) of gemcitabine and curcumin in the PSL was 0.5% and 0.9%, respectively, as such the molar ratio of gemcitabine to curcumin was 1:1. *p < 0.01, ** p < 0.0001(unless specified, p values denote difference between PSL gemcitabine and free gemcitabine solution.
In contrast, treatment with gemcitabine PSL (2.5–25 μM) caused significant cytotoxicity (p < 0.01) after 48 h exposure, resulting in an IC50 2.3 ± 0.1 μM. The gemcitabine-curcumin PSL demonstrated significant enhanced cytotoxicity at concentrations >5 μM (p < 0.01–0.0001) compared to the single drug-loaded PSLs. At 72 h, less than 1% of the MIA PaCa-2 cells were viable after treatment with dual-drug loaded PSL at 25 μM. The single drug loaded PSLs also showed high cytotoxicity as exposure time increased.
In addition, all the liposomal formulations demonstrated a concentration-dependent cytotoxicity at each time period (p < 0.01). Blank liposomes with equivalent lipid concentrations did not show significant cytotoxicity following 72 h exposure with cell viabilities of 93 ± 3%.
PSL Stability
Table II shows the physicochemical properties of gemcitabine-curcumin PSL prepared by the SVI method and stored as liposomal pellets over a 3-month period with no significant changes over this time frame at 4°C (p > 0.05).
Pharmacokinetics
Following drug administration none of the animals showed any signs of stress.
The gradient HPLC method was validated following extraction from plasma samples spiked with both gemcitabine and curcumin. No interference was observed at the retention time for both gemcitabine and curcumin. The extraction recoveries following a two-step protein precipitation using acetonitrile were in the range of 97% to 103 ± 0.6% for both drugs. The assays for both drugs had satisfactory intra-day and inter-day precision and accuracy at concentrations of 0.5, 5 and 10 μM with relative standard deviations varying 0.2–1.72% and recoveries ranging from 95.6 ± 1.5% to 103 ± 0.6% (n = 3). The calculated LOQ and LOD for both gemcitabine and curcumin were 0.03 μM and 0.01 μM, respectively.
The plasma drug concentration-time profiles after i.v. administration of their free solutions and PSL formulation are shown in Fig. 6.
The gemcitabine-curcumin PSL resulted in a significantly reduced Clearance (CL) of gemcitabine (p < 0.05), leading to an approximately 2.5-fold increase in the AUC0-∞ compared to gemcitabine solution (Table III). The elimination phase half-life (T1/2) and mean retention time (MRT) were increased by approximately 5-fold and 3-fold, respectively.
The presence of curcumin appeared to increase the gemcitabine concentrations in plasma although did not significantly change the pharmacokinetic parameters of the gemcitabine solution (p > 0.05 for all the cases).
Remarkedly, the Vd and CL of curcumin in the PSL were reduced by 4 to 4.6-fold (p < 0.05). which lead to significantly higher curcumin concentrations at the earlier time points (e.g., 7.5-fold at 15 min). Not surprisingly, the Vd and CL values of free curcumin (lipophilic) were much higher than those of gemcitabine (hydrophilic).
Discussion
MRP5 has been reported to be over-expressed in several PDAC cell lines (e.g. MIA PaCa-2) and confers resistance to gemcitabine (22). Therefore, co-treatment with curcumin may potentially enhance gemcitabine activity in PC by inhibition of MRP5. In addition, curcumin possesses many anticancer properties making it an attractive agent as a combination therapy to treat drug-resistant cancer (32).
PSL was constructed with DOPE/CHEMS/DSPE-mPEG2000. At neutral pH, CHEMS is ionized, stabilizing the bilayer. Once the carboxyl group of CHEMS (pKa 5.8) is protonated at low pH, the bilayer of DOPE is converted to an invert hexagonal (HII) structure, releasing the drug content (45, 46). As previously reported (23), increasing PEGylation degree (DSPE-mPEG2000 (0–5%) significantly reduced the pH-sensitivity of PSL (Fig. 2). This is due to the shielding of the pH-sensitive membrane to the proton (H+) by the PEG layer. Additionally, reduction in the liposomal zeta potential from −37 mV (non-PEGylation) to −8 mV as a result of PEGylation may decrease the attraction to H+ around the liposomal surface (23).
Compared to PEGylation, the effect of incorporation of curcumin on the pH-sensitivity of PSL was insignificant (Fig. 2). Curcumin in the liposome bilayers may inhibit the transformation of the DOPE when contacting H+. However, curcumin had no significant effect on the zeta potential of the resulting PSL which may be the most important reason for the insignificant effect on pH-sensitivity.
In this study the formulation effects on pH-sensitivity was tested using a rapid in vitro calcein leakage assay. Our previous study (39) demonstrated that this calcein leakage assay results closely reflect the endosome escape property of PSL in MIA PaCa-2 cells that was observed with confocal microscopy: a rapid calcein leakage in vitro in 10 min corresponded to a strong intracellularly well-distributed calcein fluorescence at 2 h. In contrary, if calcein leakage is slow the intracellular fluorescence remains as ‘dots’ or invisible.
In MIA PaCa-2 cells, the intracellular accumulation of gemcitabine was increased by co-incubation with curcumin solution or its liposomal formulations in a concentration-dependent manner from 5 to 100 μM (Fig. 3). Previous studies by Paxton et al. showed functional expression of MRP5 in MIA PaCa-2 cells and identified curcumin as an MRP5 inhibitor (22). It worth noting that the same group also found that curcumin (free drug solution at 2–20 μM) inhibited human equilibrative nucleoside transporter 1 (the influx transporter for gemcitabine) in MIA Paca-2 cells following 1-h co-incubation (47). It is plausible that curcumin increased gemcitabine accumulation by inhibiting MRP5. As a lipophilic compound (log P 2.5), curcumin may more readily interact with MRP5 on the cell membrane than liposomal bilayers (22). Curcumin in PSL significantly increased gemcitabine accumulation in the cells (p < 0.01), more effective than curcumin in NPSL at >50 μM. However, it remains unclear why NPSL was more effective than PSL curcumin at 1–10 μM. Interestingly, co-treatment with blank PSL at high concentrations also enhanced gemcitabine accumulation by the cells. This may be caused by the passive diffusion of extracellular gemcitabine into PSL followed by internalization to MIA PaCa-2 cells. To maintain cell viability and reduce interference of gemcitabine metabolites, intracellular drug concentrations were measured after 3 h. The MRP5 inhibition effect of curcumin might be more clearly manifested as time is extended or intracellular gemcitabine concentration is increased.
Previous data indicated that the NPSL did enhance cytotoxicity compared to free gemcitabine when the DL was below 0.5% (31). In contrast, the PSL with the same DL in the present study significantly increased the potency of gemcitabine (Fig. 5). The PSL is considered to be taken up via energy-mediated endocytosis, followed by ‘endosomal escape’, allowing an efficient drug exposure to nucleus (48, 49). Significantly, the PSL further increased the gemcitabine cytotoxicity to MIA PaCa-2 by addition of curcumin. Three possible contributing factors from curcumin may be involved: i) inhibition of MRP5 mediated efflux of gemcitabine (Fig. 3); ii) sensitizing the cells to gemcitabine by modulation of miR-200 and miR-21 (9); and iii) exerting anticancer effect by various pathways.
Following i.v. administration to rats, the dual-drug loaded PSL resulted in a 2.5-fold increase in AUC, and a 4.5-fold longer T1/2, compared to the gemcitabine solution (Fig. 6; Table III). Since the extravasation efficiency of liposomes from blood vessels to tumours relies on both local blood flow and their microvascular permeability (50). Therefore a prolonged circulation time is essential (51, 52) with a minimal 6 h half-life required in tumour-targeted drug delivery (53). Interestingly, the co-administration of curcumin solution reduced both Vd and CL of gemcitabine, resulting in the AUC of gemcitabine, although not statistically different (p values 0.06–0.07).. This is likely due to the inhibiting effect of curcumin on the MRP5, which are found in the basolateral membrane of many organs particularly liver (5, 20, 21). In a previous report, the CL of doxorubicin (P-gp substrate), was reduced by co-administration with curcumin via P-gp inhibition (54).
The plasma curcumin concentration in rats at the dose of 1.2 mg/kg was similar to the reported clinical trial data with a peak range of 0.06–0.1 μM (29 to 412 ng/ml) after orally taking 8 g/day (7). Compared to free curcumin solution, PSL provided a curcumin concentration in plasma >1 μM during the first 1 h after injection. Similar concentrations were reported for a 5 mg/kg dose of a liposomal formulation (55) and 30 mg/kg for curcumin loaded in a lipid-based nanoparticulate system after i.v. injection in mice (56). Furthermore, the PSL favourably reduced the CL and Vd of curcumin with an approximately 4-fold increase in AUC in rats. Therefore, further studies are warranted to investigate the in vivo anti-tumour effects of gemcitabine-curcumin dual loaded PSL. However, the dose of gemcitabine 1 mg/kg used in the pharmacokinetic study following bolus injection to rats is equivalent to 10 mg in an adult patient of 60 kg (~5 mg/m2 by body surface) (57) while the clinical dose by intravenous infusion over 30 min for free gemcitabine is 1000 mg/m2. Therefore, a significant increase in DL (the drug to lipid ratio) in the PSL is required to allow clinical dosing. On the other hand, an effective intracellular delivery approach with liposomal protection from drug inactivation and combination with curcumin may both reduce the gemcitabine dose required in the clinical translation.
Conclusions
In the present study, curcumin-gemcitabine PSL demonstrated better gemcitabine intracellular accumulation and greater cytotoxicity towards pancreatic cancer cells, compared to gemcitabine only PSL. Co-encapsulation within the same PSL system resulted in superior in vivo exposure for both gemcitabine and curcumin and significantly improved pharmacokinetic profiles. The research highlighted that curcumin could enhance the efficacy of gemcitabine via inhibition of MRP5 efflux transporter which mediated gemcitabine resistance in PC cells. The in vivo anti-tumour effect of the gemcitabine-curcumin PSL deserves further investigation.
References
McGuigan A, Kelly P, Turkington RC, Jones C, Coleman HG, McCain RS. Pancreatic cancer: a review of clinicaldiagnosis, epidemiology, treatment and outcomes. World J Gastroenterol. 2018;24:4846–61.
Ercan G, Karlitepe A, Ozpolat B. Pancreatic cancer stem cells and therapeutic approaches. Anticancer Res. 2017;37:2761–75.
Manuel Hidalgo MD. Pancreatic cancer. N Engl J Med. 2010;362:1605–17.
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58:71–96.
König J, Hartel M, Nies AT, Martignoni ME, Guo J, Büchler MW, et al. Expression and localization of human multidrug resistance protein (ABCC) family members in pancreatic carcinoma. Int J Cancer. 2005;115:359–67.
Fletcher JI, Haber M, Henderson MJ, Norris MD. ABC transporters in cancer: more than just drug efflux pumps. Nat Rev Cancer. 2010;10:147–56.
Kanai M, Yoshimura K, Asada M, Imaizumi A, Suzuki C, Matsumoto S, et al. A phase I/II study of gemcitabine-based chemotherapy plus curcumin for patients with gemcitabine-resistant pancreatic cancer. Cancer Chemother Pharmacol. 2011;68:157–64.
Hilbig A, Oettle H. Gemcitabine in the treatment of metastatic pancreatic cancer. Expert Rev Anticancer Ther. 2008;8:511–23.
Ali S, Ahmad A, Banerjee S, Padhye S, Dominiak K, Schaffert JM, et al. Gemcitabine sensitivity can be induced in pancreatic Cancer cells through modulation of miR-200 and miR-21 expression by curcumin or its analogue CDF. Cancer Res. 2010;70:3606–17.
Szakács G, Paterson JK, Ludwig JA, Booth-Genthe C, Gottesman MM. Targeting multidrug resistance in cancer, Nat Rev Drug Discov. 2006;5:219–234.
Shukla S, Zaher H, Hartz A, Bauer B, Ware JA, Ambudkar SV. Curcumin inhibits the activity of ABCG2/BCRP1, a multidrug resistance-linked ABC drug transporter in mice. Pharm Res. 2008;26:480–7.
Mach CM, Mathew L, Mosley SA, Kurzrock R, Smith JA. Determination of minimum effective dose and optimal dosing schedule for liposomal curcumin in a xenograft human pancreatic cancer model. Anticancer Res. 2009;29:1895–900.
Hamano N, Bottger R, Lee S, Yang Y, Kulkarni J, Ip S, et al. Robust microfluidic technology and new lipid composition for fabrication of curcumin-loaded liposomes: effect on the anticancer activity and safety of cisplatin. Mol Pharm. 2019;16:3957–67.
Tang X, Bi H, Feng J, Cao J. Effect of curcumin on multidrug resistance in resistant human gastric carcinoma cell line SGC7901/VCR. Acta Pharmacol Sin. 2005;26:1009–16.
Tuordey MJ. Curcumin a potent cancer preventive agent: mechanisms of cancer cell killing. Interv Med Appl Sci. 2014;6:139–46.
Limtrakul P, Anuchapreeda S, Buddhasukh D. Modulation of human multidrug-resistance MDR-1 gene by natural curcuminoids. BMC Cancer. 2004;4:1–6.
Pastorelli D, Fabricio ASC, Giovanis P, D'Ippolito S, Fiduccia P, Soldà C, et al. Phytosome complex of curcumin as complementary therapy of advanced pancreatic cancer improves safety and efficacy of gemcitabine: results of a prospective phase II trial. Pharmacol Res. 2018;132:72–9.
Bar-Sela G, Epelbaum R, Schaffer M. Curcumin as an anti-cancer agent: review of the gap between basic and clinical applications. Curr Med Chem. 2010;17:190–7.
Batra H, Pawar S, Bahl D. Curcumin in combination with anti-cancer drugs: a nanomedicine review. Pharmacol Res. 2019;139:91–105.
Oguri T, Achiwa H, Sato S, Bessho Y, Takano Y, Miyazaki M, et al. The determinants of sensitivity and acquired resistance to gemcitabine differ in non -small cell lung cancer: a role of ABCC5 in gemcitabine sensitivity. Mol Cancer Ther. 2006;5:1800–6.
Hagmann W, Jesnowski R, Löhr JM. Interdependence of gemcitabine treatment, transporter expression, and resistance in human pancreatic carcinoma cells. Neoplasia. 2010;12:740–7.
Li Y, Revalde JL, Reid G, Paxton JW. Modulatory effects of curcumin on multi-drug resistance-associated protein 5 in pancreatic cancer cells. Cancer Chemother Pharmacol. 2011;68:603–10.
Fanciullino R, Ciccolini J. Liposome-encapsulated anticancer drugs: still waiting for the magic bullet? Curr Med Chem. 2009;16:4361–73.
Hyodo K, Yamamoto E, Suzuki T, Kikuchi H, Asano M, Ishihara H. Development of liposomal anticancer drugs. Biol Pharm Bull. 2013;36:703–7.
Hofheinz RD, Gnad-Vogt SU, Beyer U, Hochhaus A. Liposomal encapsulated anti-cancer drugs, Anticancer Drugs. 2005;16:691–707.
Laouini A, Jaafar-Maalej C, Limayem-Blouza I, Sfar S, Charcosset C, Fessi H. Preparation, characterization and applications of liposomes: state of the art. J Colloid Sci Biotechnol. 2012;1:147–68.
Jantscheff P, Esser N, Graeser R, Ziroli V, Kluth J, Unger C, et al. Liposomal gemcitabine (GemLip) efficient drug against hormone-refractory Du145 and PC-3 prostate cancer xenografts. Prostate. 2009;69:1151–63.
Graeser R, Bornmann C, Esser N, Ziroli V, Jantscheff P, Unger C, et al. Antimetastatic effects of liposomal gemcitabine and empty liposomes in an orthotopic mouse model of pancreatic cancer. Pancreas. 2009;38:330–7.
Kim IY, Kang YS, Lee DS, Park HJ, Choi EK, Oh YK, et al. Antitumor activity of EGFR targeted pH-sensitive immunoliposomes encapsulating gemcitabine in A549 xenograft nude mice. J Control Release. 2009;140:55–60.
Perche F, Torchilin VP. Recent trends in multifunctional liposomal nanocarriers for enhanced tumor targeting. J Drug Delivery. 2013;2013:1–32.
Xu H, Paxton J, Lim J, Li Y, Zhang W, Duxfield L, et al. Development of high-content gemcitabine PEGylated liposomes and their cytotoxicity on drug-resistant pancreatic tumour cells. Pharm Res. 2014;31:2583–92.
Gao Y, Tang M, Leung E, Svirskis D, Shelling A, Wu Z. Dual or multiple drug loaded nanoparticles to target breast cancer stem cells. RSC Adv. 2020;10:19089–105.
Fattal E, Couvreur P, Dubernet C. “Smart” delivery of antisense oligonucleotides by anionic pH-sensitive liposomes. Adv Drug Del Rev. 2004;56:931–46.
Karanth H, Murthy RSR. pH-sensitive liposomes—principle and application in cancer therapy. J Pharm Pharmacol. 2007;59:469–83.
Geisow MJ, Evans WH. pH in the endosome measurements during pinocytosis and receptor-mediated endocytosis. Exp Cell Res. 1984;150:36–46.
Murphy RF, Powers S, Cantor CR. Endosome pH measured in single cells by dual fluorescence flow cytometry : rapid acidification of insulin to pH 6. J Cell Biol. 1984;98:1757–62.
III DEO, Peppas NA. Opsonization, biodistribution, and pharmacokinetics of polymeric nanoparticles. Int J Pharm. 2006;307:93–102.
Gabizon A, Shmeeda H, Barenholz Y. Pharmacokinetics of pegylated liposomal doxorubicin: review of animal and human studies. Clin Pharmacokinet. 2003;42:419–36.
Xu H, Paxton JW, Wu Z. Enhanced pH-responsiveness, cellular traff icking, cytotoxicity and long-circulation of pegylated liposomes with post-insertion technique using gemcitabine as a model drug. Pharm Res. 2015;32:2428–38.
Xu H, Paxton J, Lim J, Li Y, Wu Z. Development of a gradient high performance liquid chromatography assay for simultaneous analysis of hydrophilic gemcitabine andlipophilic curcumin using a central composite design and its application in liposome development. J Pharm Biomed Anal. 2014;98:371–8.
Slepushkin VA, Simões S, Dazini P, Newman MS, Guo LS, de Lima MCP, et al. Sterically Stabilized pH-sensitive Liposomes. J Biol Chem. 1997;272:2382–8.
Kang W, Svirskis D, Sarojini V, McGregor AL, Bevitt J, Wu Z. Cyclic-RGDyC functionalized liposomes for dual-targeting of tumor vasculature and cancer cells in glioblastoma: An in vitro boron neutron capture therapy study. Oncotarget. 2017;8.
Vali AM, Toliyat T, Shafaghi B, Dadashzadeh S. Preparation, optimization, and characterization of topotecan loaded PEGylated liposomes using factorial design. Drug Dev Ind Pharm. 2008;34:10–23.
El-Gibaly I, Abdel-Ghaffar SK. Effect of hexacosanol on the characteristics of novel sustained-release allopurinol solid lipospheres (SLS): factorial design application and product evaluation. Int J Pharm. 2005;294:33–51.
Simoes S, Slepushkin V, Duzgunes N, Lima MCPd. On the mechanisms of internalization and intracellular delivery mediated by pH-sensitive liposomes. Biochim. Biophys. Acta. 2001;1515:23–37.
Paliwal SR, Paliwal R, Vyas SP. A review of mechanistic insight and application of pH-sensitive liposomes in drug delivery. Drug Deliv. 2014;22:231–42.
Revalde JL, Li Y, Wijeratne TS, Bugde P, Hawkins BC, Rosengren RJ, et al. Curcumin and its cyclohexanone analogue inhibited human equilibrative nucleoside transporter 1 (ENT1) in pancreatic cancer cells. Eur Aust J Pharm. 2017;803:167–73.
Kirkham M, Parton RG. Clathrin-independent endocytosis: new insights into caveolae and non-caveolar lipid raft carriers. Biochim Biophys Acta. 2005;1745:273–86.
Huang RB, Mocherla S, Heslinga MJ, Charoenphol P, Eniola-Adefeso O. Dynamic and cellular interactions of nanoparticles in vascular-targeted drug delivery. Mol Membr Biol. 2010;27:190–205.
Matsumura Y, Maeda H. A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agent Smancs. Cancer Res. 1986;46:6387–92.
Maruyama K. Intracellular targeting delivery of liposomal drugs to solid tumors based on EPR effects. Adv Drug Deliv Rev. 2011;63:161–9.
Yin H, Liao L, Fang J. Enhanced permeability and retention (EPR) effect based tumor targeting: the concept, application and Prospect. JSM Clin Oncol Res. 2014;2:1010.
Fenske DB, Cullis PR. Liposomal nanomedicines. Expert Opin Drug Deliv. 2008;5:25–44.
Ma W, Wang J, Guo Q, Tu P. Simultaneous determination of doxorubicin and curcumin in rat plasma by LC-MS/MS and its application to pharmacokinetic study. J Pharm Biomed Anal. 2015;111:215–21.
Li J, Jiang Y, Wen J, Fan G, Wu Y, Zhang C. A rapid and simple HPLC method for the determination of curcumin in rat plasma: assay development, validation and application to a pharmacokinetic study of curcumin liposome. Biomed Chromatogr. 2009;23:1201–7.
Mohanty C, Sahoo SK. The in vitro stability and in vivo pharmacokinetics of curcumin prepared as an aqueous nanoparticulate formulation. Biomaterials. 2010;31:6597–611.
Nair A, Jacob S. A simple practice guide for dose conversion between animals and human. J Basic Clin Pharm. 2016;7:27–31.
ACKNOWLEDGMENTS AND DISCLOSURES
The financial support from a Marsden Fund (UOA1201) provided by the Royal Society of New Zealand and an Auckland Medical Research Fund (1113026).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xu, H., Li, Y., Paxton, J.W. et al. Co-Delivery Using pH-Sensitive Liposomes to Pancreatic Cancer Cells: the Effects of Curcumin on Cellular Concentration and Pharmacokinetics of Gemcitabine. Pharm Res 38, 1209–1219 (2021). https://doi.org/10.1007/s11095-021-03072-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-021-03072-2