ABSTRACT
Purpose
Release profiles of two ciprofloxacin hydrochloride formulations for the treatment of respiratory infection were evaluated using different in vitro methodologies and characterised for aerosol performance and toxicity.
Methods
Spray-dried ciprofloxacin and ciprofloxacin spray-dried with polyvinyl alcohol as a controlled release (CR) agent at a 50:50 w/w ratio were formulated and physico-chemically characterised. Aerosol performances were assessed in vitro using a liquid impinger. Drug release was performed using a modified Franz cell and a validated air interface Calu-3-modified twin stage impinger (TSI). Ciprofloxacin toxicity was also established in vitro.
Results
Both formulations had a similar size distribution, while CR ciprofloxacin had superior aerosol performance and stability. The release profiles showed the CR formulation to have a higher transport rate compared to ciprofloxacin alone in the cell model. Contrary results were observed using the diffusion cell. Results suggest that the air interface cell model provides a more physiologically relevant model than the modified Franz cell. Toxicity analysis showed that the lung epithelial cells could tolerate a wide range of ciprofloxacin concentrations.
Conclusions
This study establishes that the in vitro modified TSI air interface Calu-3 model is capable of evaluating the fate of inhaled powder formulations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Therapies targeting respiratory tract infections represent the largest proportion of the antibacterial market (1). In some diseases where mucociliary clearance is reduced, such as in cystic fibrosis and chronic obstructive pulmonary disease, patients are at increased risks of infection, resulting in a significant morbidity and mortality associated with these pathologies (2). Subsequently, these patients are prescribed long-term systemic and/or inhaled antibiotic regimens. Maintenance treatment for these chronic conditions via the inhaled route is preferred over oral drug administration as it directly targets the site of infection, requires lower doses, minimises systemic toxicity and reduces the emergence of drug resistance. Dry powder inhalers (DPI) demonstrate many benefits in respiratory drug delivery including cost effectiveness, convenience, providing improved drug stability and higher dosing potential.
One of the major challenges faced by localised treatment of respiratory tract infections is the rapid absorption and clearance of antibiotics from the lungs. Considering drug-resistance prevention and antimicrobial effect, a sustained high concentration over an extended period of time at the site of infection should benefit treatment for chronic infection. Hence, controlled release antibiotic formulations are a logical approach, as it increases the residence time of antibiotics through the gradual and predictable release of active drug and potentially reduces treatment burden.
Although the release profiles of dry powder controlled release (CR) formulations have previously been studied (3, 4), there is no standard pharmacopoeia methodology to date for the evaluation of in vitro release rates for CR respiratory drugs. This could be attributed to the lack of predictability and correlation between available in vitro models and the in vivo state for pulmonary drugs. In addition, the respiratory system displays great complexity with regards to accessibility, anatomy, dose delivery and consistency; hence, developing a physiological relevant model remains a challenge.
Depositions of pulmonary drugs from current aerosol devices occur mainly in the airways where the epithelium is the principal barrier to drug absorption. The normal human airways are lined with a ~10 μm film of liquid consisting predominantly of endogenous phospholipids and mucus with a volume of approximately ~1 μL per cm2 (5). Hence, the release profiles of CR formulations assessed in large volume models are not anatomically consistent with the lung in vivo. It has been previously suggested that a modified Franz diffusion cell model is most useful for the analysis of CR formulation’s release rates, since it is capable of differentiating the release profiles of various CR pulmonary formulations. (4). Furthermore, this model is likely to be more similar to the lung physiology, since this apparatus is based on a particle wetting and diffusion mechanism rather than large volume ‘sink’ dissolution. While this model has been shown to differentiate CR formulations, a recent in vivo ovine model, using similar formulations, showed prolonged blood plasma concentrations far outside the range expected from the in vitro models (6).
Subsequently, a model of the airway epithelium is proposed which could potentially be used to reflect the transport characteristics in vivo and to effectively predict the pharmacokinetics of CR dry powder pulmonary drugs in preclinical drug development. Calu-3, a sub-bronchial epithelial cell line cultured at the air interface is a well-established and characterized model for the study of drug delivery and toxicology in the airways (7–11). Compared to the in vivo state, this model has similar morphology, electrical resistance and mucus production. Furthermore, the confluent mucous layer formed after 11 days in culture on the surface of the Calu-3 model also contains acidic glycoproteins and surfactants, typically found in mucus in vivo (7,8,12–14). However, the model is yet to be evaluated for its release profiling ability for dry powder CR formulations. In addition, most of the studies assessing CR dry powder formulations have been performed using drug solutions or suspensions, which are significantly different to in vivo processes, as aerosol particles are impacted onto the mucosal surfaces of epithelial cells. This is based on the assumption that deposition and the release of drug from solid microparticulates follow a series of processes which include impaction, wetting, and dissolution, followed by transport across the epithelium unless cleared by macrophages or the mucociliary system. Subsequently, this approach has been investigated by Grainger et al. to evaluate permeability of large molecular weight dextrans across the epithelium using a twin stage impinger (TSI) for solute deposition onto the air-interfaced Calu-3 model (15). In this study, dry powder CR formulations of respirable size were applied onto the Calu-3 cellular model to evaluate drug transport kinetics.
The aim of this study is to investigate and compare the release profiles of two dry powder ciprofloxacin formulations, spray-dried ciprofloxacin and CR ciprofloxacin using different in vitro methodologies. Ciprofloxacin hydrochloride was selected as the model drug for its broad spectrum activity against most gram-positive and gram-negative bacteria (16). Additionally, ciprofloxacin hydrochloride has a low molecular weight, is water-soluble, and is not affected by the spray-drying process (17). The CR component used in this formulation was polyvinyl alcohol (PVA), as it has been shown that a viscous solution containing only 1% w/w PVA has successfully altered the release of 5(6)-carboxyfluorescein in an in vivo rat model (18). In addition, PVA was recently reported to be non-toxic when applied to the human alveolar basal epithelium cell line A549 (19). The formulations were evaluated with respect to their physico-chemical properties, aerosol performance, cell toxicity and release profiles using the modified Franz diffusion model and air-interface Calu-3 cell model.
MATERIALS AND METHODS
Materials
Ciprofloxacin hydrochloride was used as supplied (MP; Biomedical Australasia Pty Limited, NSW, Australia). Polyvinyl alcohol (PVA) with a molecular weight of 22,000 and a reported degree of hydrolysis of 98% was supplied from BDH Limited (Poole, England). Non-essential amino acids solution, trypan blue solution (0.4% w/v), mucin from porcine stomach Type III, CelLytic™ M Cell Lysis, protease inhibitor cocktail to dimethyl sulfoxide (DMSO) were purchased from Sigma-Aldrich (Sydney, Australia). Other cell culture reagents including trypsin-EDTA solution (2.5 g/L trypsin, 0.5 g/L EDTA), Dulbecco’s Modified Eagle’s Medium (DMEM, without phenol red and L-glutamine, including sodium bicarbonate and 15 mM HEPES), phosphate-buffered saline (PBS), L-glutamine solution (200 mM), fetal bovine serum (FBS), Hank’s balanced salt solution (HBSS) were obtained from Invitrogen (Australia). Transwell cell culture inserts (0.33 cm2 polyester, 0.4 μm pore size) were purchased from Corning Costar (Lowell, USA); all other sterile culture plastic wares were from Sarstedt (Adelaide, Australia). The CellTiter 96® AQueous One Solution Cell Proliferation Assay was obtained from Promega (USA). All solvents used were of analytical grade and were supplied by Biolab (Victoria, Australia).
Cell Culture
Calu-3 cell line (HTB-55) was purchased from the American Type Cell Culture Collection (ATCC, Rockville, USA). Cells between passages 33 and 41 were cultured in 75 cm2 flasks in pre-warmed Dulbecco’s Modified Eagle’s medium supplemented with 10% (v/v) fetal bovine serum, 1% (v/v) non-essential amino acid solution and 1% (v/v) L-glutamine solution and were maintained at 37°C in 5% CO2 and 95% humidity until confluency was reached. Medium was exchanged every 2 to 3 days and the cells passaged weekly according to ATCC recommended guidelines.
Calu-3 cells were grown at the air-interface to allow monolayer differentiation, and experiments were performed between day 11 and 14. Briefly, cells were seeded at a density of 5 × 105 cells/cm2 on 24 Transwell cell culture inserts. The cells were introduced onto the apical surface of the Transwell in 100 μL medium with 500 μL medium added to the basolateral chamber. The medium in the apical chamber was removed after 24 h, and medium was only replaced in the basolateral chambers every 2–3 days. These conditions have previously been established by Haghi et al. (7).
Transepithelial Electrical Resistance
Transepithelial electrical resistance (TEER) measurements were performed after experiments on the Calu-3 monolayer and were compared to untreated cells. Measurements were performed using an epithelial voltohmmeter (EVOM, World Precision Instruments, USA) attached to STX-2 chopstick electrodes. Prior to resistance measurements, pre-warmed medium was added to the apical chamber and allowed to equilibrate for 30 min in a humidified condition with 5% CO2 and 95% humidity at 37°C. Ten measurements were taken per well, and the TEER was calculated by subtracting the resistance of cell-free inserts and correcting for the surface area of the Transwell polyester cell culture support as previously described (6).
Spray-Dried Microparticulate System Preparation
Single ciprofloxacin and controlled release ciprofloxacin formulations containing 50% PVA (w/w) were prepared by spray drying (Buchi B-191 Spray Dryer, Buchi, Switzerland) to allow comparison of their release profiles.
Briefly, the single ciprofloxacin formulation was prepared by dissolving ciprofloxacin HCl in water, and the feed solution was spray dried at the following conditions: feed concentration of 50 mg/mL, feed rate of 4 mL/min, aspiration rate of 47.6 m3h−1, atomizing pressure of 800 kPa, inlet of 110°C and a measured outlet temperature of 80°C.
The controlled release (CR) formulation of ciprofloxacin was prepared by co-spray drying aqueous solutions of ciprofloxacin hydrochloride and PVA. The pre-calculated amount of PVA was dissolved in water to obtain a concentration of 1.5% (w/v) at 90°C with constant agitation until a clear solution was obtained. Following the cooling of PVA solution to room temperature, ciprofloxacin solution was added. Similar spray-drying conditions were applied with the exception of the inlet and temperature of 120°C and 66°C, respectively.
Ciprofloxacin Analysis
Quantification of both formulations, with and without PVA, was performed using high-performance liquid chromatography (HPLC). Analysis of ciprofloxacin hydrocholoride was achieved using a Shimadzu Prominence UFLC system equipped with the SPD-20A UV–vis detector, LC-20AT liquid chromatography, RID 10A refractive index detector and SIL-20A HT Autosampler (Prominence UFLC, Shimadzu Corporation, Japan) and Optimal ODS-H column (3 μm, 150 × 4.6 mm, Capital HPLC Limited, Scotland). The mobile phase comprised a mixture of methanol and 0.1 M sodium dihydrogen phosphate (30:70, v/v) with pH adjusted to 3.35 with phosphoric acid to allow ciprofloxacin separation. Standards were prepared in MilliQ water. HPLC was set according to the following conditions: detection wavelength 275 nm, flow rate of 0.8 mL/min, and an injection volume of 100 μL. Linearity was obtained between 0.5 and 100 μg/mL (R2 = 0.99) with a retention time of 26.57 min.
Particle Size Distribution
Particle size distribution of spray-dried ciprofloxacin only and controlled release ciprofloxacin samples were measured by laser diffraction (Mastersizer 2000, Malvern Instruments, UK) using dry powder feeder (Scirocco 2000, Malvern Instruments, UK). Approximately 3 mg of sample was dispersed in air using 4-bar pressure and was measured with a refractive index of 1.52. Samples were analysed in triplicates.
Scanning Electron Microscopy
Microparticles morphologies were visualised using scanning electron microscopy (Intellection Quemscan, Zeiss, Australia) at 10 kV. Samples were mounted onto carbon sticky taps, which were attached to aluminium stubs and gold coated (Sputter coater S150B, Edwards High Vacuum, UK) at 40 nm thickness prior to imaging.
Differential Scanning Calorimetry
Differential scanning calorimetery (DSC—DSC823e, Mettler-Tolledo, Switzerland) was used to analyse the thermal responses of each formulation. Approximately 5 mg of powders were measured and crimp-sealed in DSC sample pans with the lid pierced. Thermal properties were analysed at 10°C/min temperature ramp over 40 and 400°C range. Data were normalised for initial mass. Temperatures of each exothermic and endothermic peak and onset were determined using STARe V9.0x software (Mettler-Tolledo).
Dynamic Vapour Sorption
The moisture sorption characteristics of the spray-dried microparticles were assessed using dynamic vapour sorption (DVS). Samples (15 mg) were added onto the sample pan and were dried at 0% relative humidity (RH) before exposure to two sorption cycles of 0 to 90% RH at a 10% increment. Equilibrium of moisture sorption was determined by a change in mass-to-time ratio (dm/dt) of 0.0005% min−1. An automated water sorption analyser (DVS-1, Surface measurement systems Ltd., UK) was used to determine the moisture sorption profiles of samples.
In Vitro Aerosol Performance Studies
Both spray-dried single and controlled release ciprofloxacin were analysed for aerosolisation efficiency using a multi stage liquid impinger (MSLI) (Apparatus A, European Pharmacopoeia, Chapter 2.9.18, Copley Scientific, UK) and an Aerolizer® (Norvartis Surrey, UK). The flow rate through the MSLI was controlled by a GAST rotary vein pump and solenoid valve timer (Copley Scientific). Prior to the experiment, the flow rate was tested and set to 60 mL/min using a calibrated flow meter (TSI, Shoreview, USA). At this flow rate, the cut-off aerodynamic diameters of each stage of the MSLI are 13, 6.8, 3.1, and 1.7 μm for stages 1, 2, 3 and 4, respectively. Stage 5 contained a filter housing to capture particles less that 1.7 μm. Twenty mL of MilliQ water was accurately added to each collection stage of the MSLI. Samples were pre-weighed (5 ± 0.05 mg) and filled into a size 3 hard gelatine capsule (Capsugel, Australia) and carefully placed into the dosage chamber of an Aerolizer®. The Aerolizer® was fitted into a mouthpiece adapter which was connected to the MSLI using a United State Pharmacopoeia (USP) throat. The samples were tested at 60 mL/min for 4 s. After actuation, the device, capsule, throat, all stages and filter were washed separately using water and analysed using HPLC. Each sample was tested in triplicate.
In Vitro Drug Release Studies
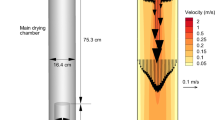
Calu-3 TSI-Modified Cell Model
A glass twin stage impinger (TSI; British Pharmacopoeia Apparatus A, Copley Scientific, UK) was adapted to fit the cell culture transwell inserts at the lower second chamber where particles with aerodynamic diameter of <6.4 μm (respirable particles) are deposited. The assembly of the apparatus was based on a modified TSI which was previously described (15). In general, the TSI was assembled based on the British Pharmacopeia with the absence of solution in the lower chamber and a custom-made mouthpiece adapter connected to an Aerolizer® at the entrance of the TSI. A Transwell insert was then fixed firmly upon the connecting tube of the second lower chamber, which was pre-wrapped with parafilm, allowing particles to be impacted and deposited on the Calu-3 air-interface cell layer. An appropriate amount of powder was weighed into size 3 hard gelatine capsules and placed into the dosage chamber of the Aerolizer® to obtain a powder amount of <35 μg deposited onto the cells after actuation. The powder was aerosolised at 60 mL/min for 4 s.
After deposition of the powder, the Transwell insert was removed and placed into a well of a 24-well plate containing 600 μL of pre-warmed HBSS (receiver fluid). At pre-determined time intervals (up to 4 h) the Transwell insert was transferred into a new well with fresh HBSS in order to maintain sink conditions. At the final time point, the transwell insert was transferred to an empty well, and the top of the cells were gently washed with HBSS buffer to collect any remaining drug on the cell monolayer. Finally, the cells were removed from the filter insert by trypsinisation and subsequently lysed in CelLytic™ M Cell Lysis reagent in the presence of 1% (v/v) protease inhibitor cocktail, on ice according to the manufacturer’s recommendation, to quantify intracellular drug. The lysates were centrifuged at 10,000 × g for 10 min at 4°C, and supernatant was collected and diluted to an appropriate volume. These samples were collected for HPLC analysis. The estimated quantity of powder deposited on the cells is the sum of the drug that has been transported and the drug recovered from the cell surface and within the cells at the final time point.
Franz Cell Diffusion Apparatus
The diffusion apparatus was based on a modified Franz diffusion cell, which has been previously described (3,20,21). The apparatus was set up with each cell of the multi-station Franz cell station (VB6, PermeGear Inc., USA) contained within a heated water jacket that was maintained at 37 ± 0.05°C via a circulating water bath. Fifty mL of HBSS solution was equilibrated (37 ± 0.05°C) in a water bath and was pumped into the inlet port of the Franz cell at 5 mL/min via a multichannel peristaltic pump (Minipuls 3, Gilson, USA). The sampling port of the cell was connected to a second pump channel, which in turn returned the sample flow to the 50 mL sink. A 0.45 μm filter membrane (MF™ Membrane Filters, Millipore, USA) was clamped to the Franz cell with an internal diameter of 2.5 cm available for diffusion. The set-up ensured constant volume within the Franz cell and the filter uniformly wetted. The continual renewal of dissolution medium combined with constant agitation of the magnetic stirrer at the bottom of the Franz cell ensured sinks conditions. Once the system was equilibrated and stable, pre-weighed samples (1 ± 0.05 mg) were evenly spread over the pre-wetted membrane filter. Samples of 0.6 mL were taken from the 50 mL reservoir at predetermined time interval (up to 4 h) and analysed in triplicate by HPLC.
Cell Viability Assay
The cytotoxicity profiles of ciprofloxacin and PVA were assessed using CellTiter 96® AQueous One Solution Cell proliferation Assay (Promega, USA). Calu-3 cells were seeded into sterile 96-well microtitre plates at a density of 5 × 104 cells/well and were left overnight to allow for cell attachment. Cells were treated with increasing concentrations of ciprofloxacin hydrochloride in complete DMEM medium in a final volume of 200 μL. Control wells contained cells and medium without the addition of drugs. Plates were incubated at 37°C in 5% CO2 and 95% humidity for 72 h. The cells were analysed for viability following the addition of 20 μL of AQueous One Solution to each well and incubation for 4 h at 37°C in 5% CO2 and 95% humidity. Absorbance of the wells was measured at 490 nm using a fluorescence plate reader (POLARstar Optima, BMG Labtech, Germany). The cell viability (%) was calculated based on the formula: \( \left( {\left( {{\text{average}}\;{\text{absorbance}}\;{\text{of}}\;{\text{treated}}\;{\text{cells}}/{\text{average}}\;{\text{absorbance}}\;{\text{of}}\;{\text{control}}\;{\text{cells}}} \right) \times 100} \right) \). The concentration that produced a 50% decrease in cell viability after 72 h, also known as the IC50 value, was calculated following the 72 h treatment period.
Confocal Microscopy Live-Cell Imaging
Ciprofloxacin formulations were deposited onto the air interface Calu-3 cells using the modified TSI apparatus as described above. Image acquisition was performed on the Transwell inserts in a 24-well plate immediately after deposition of ciprofloxacin using a confocal microscope (LSM 510 Microscope Meta, Carl Zeiss, Australia) at 10x objective at pre-determined time points. The confocal aperture was set to 1.0 Airy unit, and the UV laser (405 nm) was used for excitation of ciprofloxacin. Settings (aperture, gain and laser power) were determined prior to imaging and were maintained throughout. For three-dimensional image projections of the ciprofloxacin transport through the epithelial cells, Z-scans in 2.2 μm increments were taken above the Transwell filter and projected using Image J software.
Particle Visualisation
Particle visualisation was performed to analyse the microparticle solid state changes upon contact with mucin. Microscope slides were first wetted in Mucin Type III at a concentration of 0.5 mg/mL. Dry powder formulations were then applied onto the slides and were viewed using light microscope (CX41, Olympus, Japan) at 10x magnification.
Statistical Analysis
All results are expressed as mean ± standard deviation of at least three replicate experiments. Unpaired 2-tailed t-tests were performed to determine significance (which was quoted at the level of P < 0.05) between treatment groups. IC50 value was established by fitting the data to the inhibitory Sigmoid Emax model onto the % cell viability versus drug concentration plot using GraphPad Prism (version 5). The release rates of ciprofloxacin formulations were statistically analysed to evaluate the formulation performances using Fit Factors described by Moore and Flanner (22).
RESULTS AND DISCUSSION
In this study, ciprofloxacin formulations were assessed in terms of their physico-chemical properties, cell toxicity, aerosol performance and release profiles using the modified TSI-cell model and the Franz diffusion cell. For a clearer and better understanding of the formulation’s properties, the study was divided into two main sections: (1) physical characteristics and (2) in vitro characteristics of formulations.
Physical Characteristics
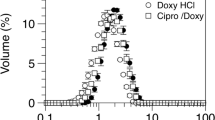
The particle size distributions of the spray-dried only and CR ciprofloxacin are shown in Fig. 1. In general, the particles display a similar size distribution with small variations. This could be attributed to the systems being subjected to similar spray-drying conditions and concentrations. Median volume diameters of 1.89 ± 0.28 μm and 2.49 ± 0.03 μm were observed for spray-dried and CR ciprofloxacin, respectively (n = 3). These sizes fall within the range for respiratory delivery.
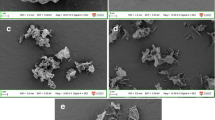
Scanning electron micrographs of single spray-dried ciprofloxacin and CR ciprofloxacin are shown in Fig. 2a and b, respectively. Overall, the microparticles display a spherical geometrical appearance and have similar diameters, in good agreement with the particle size data. The morphology of spray-dried ciprofloxacin alone had a corrugated surface in contrast to the co-spray dried system with PVA, which presented a smoother surface with occasional cavity formation. These observations were in good agreement with previous studies (3,17,19). Such morphologies were consistent with particle collapse following the rapid drying process during manufacturing.
The thermal properties of ciprofloxacin formulations were investigated to analyse the influence of heat flow on the microparticulate system. The response of each sample to the temperature ramp is displayed in Fig. 3. Spray-dried ciprofloxacin alone showed water loss from 30°C to 170°C, which was indicated by the broad diffuse endothermic peak. Following that, a series of exothermic peaks at 175°C and 194°C were observed, suggestive of a phase transition from amorphous to crystalline of ciprofloxacin. The sharp endothermic peak at 323°C was attributed to melting and subsequent decomposition of ciprofloxacin at 348°C. The thermal response of CR ciprofloxacin formulation showed a comparable profile with broad diffuse peak, succeeded by a single phase transition exothermic peak and a sharp melting peak at similar temperatures. Interestingly, an additional two endothermic peaks were observed at 224°C and 273°C for the CR formulation. This is indicative of the melting point for PVA and ciprofloxacin, respectively, as previously reported (3,17). The lower melting points for both the constituents as compared to their pure counterparts were presumably due to an increase in entropy in this co-processed system.
The effect of humidity on moisture sorption was analysed to further understand the relative stability of the formulations’ solid-state. The moisture sorption profiles (first sorption cycle) for spray-dried ciprofloxacin and CR ciprofloxacin are shown in Fig. 4. Analysis of the spray-dried ciprofloxacin isotherm showed a rapid increase in the moisture uptake between 0 and 50% RH (~8%). However, any further increase in the partial water vapour pressure above 50% RH resulted in a dramatic decrease in mass, indicative of the characteristic water loss during crystallisation due to the removal of plasticising water. In comparison, the moisture sorption for CR ciprofloxacin showed a different profile. Although a mass loss was also observed after the exposure of the formulation to 50% RH, the characteristic recrystallisation mass loss was found to occur over a much longer period. Such observations suggest that PVA stabilises the amorphous ciprofloxacin where a greater amount of adsorbed moisture is required to induce sufficient mobility for molecules to align and crystallise.
In Vitro Characteristics
The in vitro aerosolisation efficiency of ciprofloxacin formulations is shown in Fig. 5. Data are represented as the percentage of the total drug deposited in device/capsule and at each stage of the MSLI over the total mass recovered. The fine particle fraction was calculated as the cumulative percentage of drug deposited from stage 3 to the filter of the MSLI (particles with aerodynamic diameter of less than 6.8 μm). In general, the CR ciprofloxacin formulation (FPF = 28.72 ± 1.99%) had a statistically higher aerosol performance in comparison to the single spray-dried ciprofloxacin (FPF = 19.01 ± 2.41%) (p < 0.05). This is indicative that ciprofloxacin on its own is more cohesive. Subsequently, the powders remained in the capsules or as agglomerates after aerosolisation and hence deposited at higher stages. On the other hand, the CR ciprofloxacin formulation had a higher FPF, which, interestingly, is counterintuitive to what is understood about the relationship between surface morphology and particle size on aerosolisation efficiency. It is expected that spray-dried ciprofloxacin alone, which has a corrugated surface, would have lower aerosolisation efficiency, as the contact area between contiguous particle faces would be reduced, hence resulting in a reduction in adhesion force (23,24). However a recent study by Salama et al. demonstrated similar findings using di-sodium chromoglycate co-spray dried with varying amounts of PVA where an increase in PVA concentration resulted in an increase in aerosolisation efficiency due to its surface chemistry and reduced capillary formation (20). Hence, the increase in aerosol performance of CR ciprofloxacin was presumably due to the addition of PVA where its chemical nature had a major influence on the aerosolisation efficiency.
Release profiles over time of spray-dried ciprofloxacin and CR ciprofloxacin dry powder formulations using two different in vitro methodologies, the modified Franz diffusion cell and the air-interface Calu-3 cell model, are shown in Fig. 6. Drug concentrations were measured and expressed in terms of percent total recovery throughout the experiments, and data were plotted as mean cumulative percentage (± standard deviation) of drug released over 4 h. With the Franz diffusion cell, dry powder formulations deposited on the filter membrane were rapidly wetted followed by diffusion into the surrounding media. Analysis of the ciprofloxacin-only release from the diffusion cell demonstrated a rapid release rate with ≥95% of drug released within the first hour, in contrast to CR ciprofloxacin, where approximately 88% of the drug was released over a 4-hour period. This was in good agreement with previous studies (3,4). Interestingly, the release profile of the same ciprofloxacin formulations was found to be the opposite in the Calu-3 cell model, where CR ciprofloxacin showed a higher percentage of drug transported across the cell epithelia compared to spray-dried ciprofloxacin alone.
Similar transport kinetics to that observed using the Calu-3 model were observed in an in vivo ovine model where the area under the curve for CR formulation of disodium chromoglycate (DSCG) was higher in comparison to DSCG alone (6). The different transport rates of the ciprofloxacin formulations observed could possibly be attributed to the different mucosa-particle interactions, which were made possible by the modified TSI air-interfaced Calu-3 cell system. It is hypothesised that the PVA component within the microparticulate system could have enhanced the drug transport across the lung epithelium through a combination of several mechanisms.
The two ciprofloxacin formulations have different physicochemical properties. The deposition of the spray-dried ciprofloxacin only formulation onto the Calu-3 cells promotes rapid crystallisation of ciprofloxacin. This is demonstrated in Fig. 7a, where microscopic analysis of the formulations, showed crystal formation upon contact with mucin. In contrast, the CR ciprofloxacin formulation remained in its amorphous state as shown in Fig. 7b. Thus, there is increasing evidence to suggest that the PVA component within the CR microparticulate system stabilises the amorphous form of ciprofloxacin, allowing a rapid dissolution of drug into the surrounding epithelial lining fluid. Although the mucin solution used in this investigation was not ‘ideal’ in comparison to native mucus, other researchers have used ‘simulated mucus’ for the study of pulmonary formulations (25,26) with optimal results.
This is further supported by confocal images taken at various time points after the deposition of dry powder ciprofloxacin formulations from the surface of Calu-3 cells (Table I). For the first time, the dry powder drug deposition and transport on cells were visualised using live cell confocal imaging, made possible by the inherent fluorescent properties of ciprofloxacin, allowing better analysis of the drug-mucosa interactions. It was observed that ciprofloxacin was present on the mucus and within the cell, indicating that the drug is transported through transcellular route, although the two formulations have different dissolution and diffusion behaviours upon deposition. The spray-dried ciprofloxacin alone showed slow diffusional spreading of ciprofloxacin from concentrated areas to the surrounding epithelial lining fluid after 2 h, presumably due to its slower dissolution from stable crystal formation. In comparison, the CR ciprofloxacin formulation showed a rapid diffusion into the cell lining fluid within 15 min, as seen with the widespread distribution of ciprofloxacin on the Calu-3 cells. Additionally, PVA forms a ‘gel’-like material enabling a larger coverage of the cell surface area, which is illustrated in Fig. 7. Subsequently, this could have facilitated the transport of ciprofloxacin across the epithelial cells by exposing more cells to the drug.
Another possible explanation for the enhanced drug transport of ciprofloxacin from CR formulations is the reduction of ciprofloxacin hydrochloride charges by PVA. At physiological pH 7.4, ciprofloxacin exists as zwitterions (pka1 = 6.5, pka2 = 8.5 and pI = 7.4), with a negatively charged carboxyl group and a positively charged nitrogen of the piperazine ring (10). However, with the presence of PVA (a weak acid; pka = 10.67), a complex interaction may exist between the long chain hydroxy groups and the ionised moieties on the ciprofloxacin molecule. This is currently being investigated further.
The release kinetics for the different formulations and different methodology were statistically analysed and compared using Moore and Flanner’s Fit Factors (22), adopted by the Food and Drug Administration guidance for dissolution testing in the industry (27). Simply, the Fit Factor is a model that has independent approaches to compare release profiles for a test and reference formulation using a difference factor (f 1 ) and a similarity factor (f 2 ). For curves to be considered different, arbitrary limits with f 1 ≥ 10 and f 2 ≤ 50 were chosen for analysis. Analysis of these factors (Table II) for the release profiles of ciprofloxacin formulations using the Franz diffusion cell apparatus confirmed that CR ciprofloxacin has different release profile compared to the control spray-dried ciprofloxacin alone. However, the release profiles curves for the ciprofloxacin formulations on the Calu-3 cell model were not as explicit, as it has f 1 and ‘borderline’ f 2 values of 23.68 and 53.02, respectively, although a clear difference in the percentage released at any time point could be distinguished. It should be noted that a study by Polli et al. showed limiting f 2 values at 50 to be conservative (28). In that study, two metoprolol tartarate formulations were compared and were found to be different based on this scale, although it has been proven to be bioequivalent. Nevertheless, it can be concluded that the modified TSI air-interfaced Calu-3 cell model is also capable in differentiating the release profiles of different formulations.
Transepithelial electrical resistance (TEER) was measured after the experiment and was compared to the untreated cells to assess the integrity of the epithelial cells. This was performed to determine if the high local concentration of ciprofloxacin at deposition point might have detrimental effect to the cells. It was found that there was no significant difference between the control cells and cells treated with either spray-dried ciprofloxacin alone (p = 0.056) or CR ciprofloxacin (p = 0.084) (Fig. 8). Hence, it was evident that the deposition of different dry powder formulations had no effect on epithelial cell integrity under the conditions or timescale studied.
The dose response cytotoxicity profile of ciprofloxacin hydrochloride on Calu-3 cells was established and is shown in Fig. 9. Calu-3 cells were exposed to increasing concentrations of ciprofloxacin over a 72 h treatment period. The viability of cells was calculated with reference to the untreated cells where average absorbance was normalised to 100% viability. The IC50 value was found to be 363.92 ± 1.15 μM. This value is significantly lower compared to the amount of dry powder deposited onto the Calu-3 cell surface considering that the cell lining fluid is of much lower quantity, which was estimated to be 3.44 μL (15). However, it should be noted that the cell viability assay is not representative of the air-interface Calu-3 model used in the transport experiments, as the cells are grown in liquid and hence do not produce a mucus layer nor allow the cells to differentiate the same way. The presence of the mucus layer in the differentiated model may serve as a protective barrier in limiting the dissolution of ciprofloxacin and hence maintaining low concentrations of drug being directly exposed to the cells. Nonetheless, the viability assay demonstrates the wide range of ciprofloxacin concentration that these cells can tolerate in the absence of the protective mucosal barrier. A previous study by Salama et al., showed that PVA was not toxic to lung epithelial cells over the same range of concentration (19). However, further toxicity studies in vivo are required to assess the long-term effects of both ciprofloxacin and PVA.
CONCLUSION
The deposition of respirable dry powder aerosol formulations onto the air-interface Calu-3 cells using a modified TSI provides a more representative in vitro model of the in vivo state in terms of mucosa particle interaction. This model could potentially simulate the deposition of drugs to the tracheo-bronchiolar region of the lungs after inhalation. It allows particles to dissolve and diffuse into the thin aqueous layer of mucus and/or surfactant lining of the airway epithelial cells, which has been demonstrated to play an important role in determining the respiratory absorption rate. Hence, due to its physiological relevance, this system has the potential to evaluate the release profiles of novel inhaled CR dry powder formulation with enhanced correlation to in vivo measurements. However, further work with an alveolar cell model is required to investigate the fate of such respiratory formulations deposited into the peripheral lung, where pulmonary surfactant is the dominant lining fluid in the alveolar region. Future studies will focus on correlating this in vitro model with in vivo release rates and investigating the role of transporters in ciprofloxacin absorption in the lung.
REFERENCES
Traini D, Young PM. Delivery of antibiotics to the respiratory tract: an update. Expert Opin Drug Deliv. 2009;6(9):897–905.
Murray TS, Egan M, Kazmierczak BI. Pseudomonas aeruginosa chronic colonization in cystic fibrosis patients. Curr Opin Pediatr. 2007;19(1):83–8.
Adi H, Young PM, Chan H-K, Salama R, Traini D. Controlled release antibiotics for dry powder lung delivery. Drug Dev Ind Pharm. 2010;36(1):119–26.
Salama RO, Traini D, Chan H-K, Young PM. Preparation and characterisation of controlled release co-spray dried drug-polymer microparticles for inhalation 2: evaluation of in vitro release profiling methodologies for controlled release respiratory aerosols. Eur J Pharm Biopharm. 2008;70(1):145–52.
Widdicombe JH. Regulation of the depth and composition of airway surface liquid. J Anat. 2002;201(4):313–8.
Salama R, Ladd L, Chan H-K, Traini D, Young P. Development of an ovine dry powder inhalation model for the evaluation of conventional and controlled release microparticles. AAPS J. 2009;11(3):465–8.
Haghi M, Young PM, Traini D, Jaiswal R, Gong J, Bebawy M. Time- and passage-dependent characteristics of a Calu-3 respiratory epithelial cell model. Drug Dev Ind Pharm. 2010;36:1207–14.
Grainger CI, Greenwell LL, Lockley DJ, Martin GP, Forbes B, Grainger CI, et al. Culture of Calu-3 cells at the air interface provides a representative model of the airway epithelial barrier. Pharm Res. 2006;23(7):1482–90. Comparative Study Research Support, Non-U.S. Gov’t.
Bur M, Lehr CM, Bur M, Lehr C-M. Pulmonary cell culture models to study the safety and efficacy of innovative aerosol medicines. Expert Opin Drug Deliv. 2008;5(6):641–52. Research Support, Non-U.S. Gov’t Review.
Cavet M, West M, Simmons N. Transepithelial transport of the fluoroquinolone ciprofloxacin by human airway epithelial Calu-3 cells. Antimicrob Agents Chemother. 1997;41(12):2693–8.
Ehrhardt C, Kneuer C, Bies C, Lehr C-M, Kim K-J, Bakowsky U. Salbutamol is actively absorbed across human bronchial epithelial cell layers. Pulm Pharmacol Ther. 2005;18(3):165–70. Research Support, Non-U.S. Gov’t, Research Support, U.S. Gov’t, P.H.S.
Fiegel J, Ehrhardt C, Schaefer UF, Lehr C-M, Hanes J. Large porous particle impingement on lung epithelial cell monolayers—toward improved particle characterization in the lung. Pharm Res. 2003;20(5):788–96.
Mathias NR, Timoszyk J, Stetsko PI, Megill JR, Smith RL, Wall DA. Permeability characteristics of Calu-3 human bronchial epithelial cells: in vitro—in vivo correlation to predict lung absorption in rats. J Drug Target. 2002;10(1):31–40.
Yan Z, Aaron C, Thomas H. Cultured human airway epithelial cells (Calu-3): a model of human respiratory function, structure, and inflammatory responses. Crit Care Res Pract. 2010;2010
Grainger CI, Greenwell LL, Martin GP, Forbes B. The permeability of large molecular weight solutes following particle delivery to air-interfaced cells that model the respiratory mucosa. Eur J Pharm Sci. 2009;71(2):318–24.
Moazeni E, Gilani K, Sotoudegan F, Pardakhty A, Najafabadi AR, Ghalandari R, et al. Formulation and in vitro evaluation of ciprofloxacin containing niosomes for pulmonary delivery. J Microencapsul. 2010;27(7):618–27.
Adi H, Young PM, Chan H, Stewart P, Agus H, Traini D. Cospray dried antibiotics for dry powder lung delivery. J Pharm Sci. 2007
Yamamoto A, Yamada K, Muramatsu H, Nishinaka A, Okumura S, Okada N, et al. Control of pulmonary absorption of water-soluble compounds by various viscous vehicles. Int J Pharm. 2004;282(1–2):141–9.
Salama RO, Traini D, Chan HK, Sung A, Ammit AJ, Young PM. Preparation and evaluation of controlled release microparticles for respiratory protein therapy. J Pharm Sci. 2009;98(8):2709–17.
Salama R, Hoe S, Chan H-K, Traini D, Young PM. Preparation and characterisation of controlled release co-spray dried drug-polymer microparticles for inhalation 1: influence of polymer concentration on physical and in vitro characteristics. Eur J Pharm Biopharm. 2008;69(2):486–95.
Franz TJ. Percutaneous absorption on the relevance of in vitro data. J Investig Dermatol. 1975;64(3):190–5.
Moore JW, Flanner HH. Mathematical comparison of dissolution profiles. Pharm Technol. 1996;20(6):64–74.
Adi S, Adi H, Tang P, Traini D, Chan H-K, Young PM. Micro-particle corrugation, adhesion and inhalation aerosol efficiency. Eur J Pharm Sci. 2008;35(1–2):12–8.
Chew NYK, Tang P, Chan H-K, Raper JA. How much particle surface corrugation is sufficient to improve aerosol performance of powders? Pharm Res. 2005;22(1):148–52.
Yang Y, Tsifansky MD, Wu CJ, Yang HI, Schmidt G, Yeo Y. Inhalable antibiotic delivery using a dry powder co-delivering recombinant deoxyribonuclease and ciprofloxacin for treatment of cystic fibrosis. Pharm Res. 2010;27(1):151–60.
Sweeney LG, Wang Z, Loebenberg R, Wong JP, Lange CF, Finlay WH. Spray-freeze-dried liposomal ciprofloxacin powder for inhaled aerosol drug delivery. Int J Pharm. 2005;305(1–2):180–5.
Administration FaD. Guidance for industry; dissolution testing of immediate release solid oral dosage forms. August 1997
Polli JE, Rekhi GS, Augsburger LL, Shah VP. Methods to compare dissolution profiles and a rationale for wide dissolution specifications for metoprolol tartrate tablets. J Pharm Sci. 1997;86(6):690–700.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ong, H.X., Traini, D., Bebawy, M. et al. Epithelial Profiling of Antibiotic Controlled Release Respiratory Formulations. Pharm Res 28, 2327–2338 (2011). https://doi.org/10.1007/s11095-011-0462-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-011-0462-1