Abstract
Purpose
To propose and test a new accelerated aging protocol for solid-state, small molecule pharmaceuticals which provides faster predictions for drug substance and drug product shelf-life.
Materials and Methods
The concept of an isoconversion paradigm, where times in different temperature and humidity-controlled stability chambers are set to provide a critical degradant level, is introduced for solid-state pharmaceuticals. Reliable estimates for temperature and relative humidity effects are handled using a humidity-corrected Arrhenius equation, where temperature and relative humidity are assumed to be orthogonal. Imprecision is incorporated into a Monte-Carlo simulation to propagate the variations inherent in the experiment. In early development phases, greater imprecision in predictions is tolerated to allow faster screening with reduced sampling. Early development data are then used to design appropriate test conditions for more reliable later stability estimations.
Results
Examples are reported showing that predicted shelf-life values for lower temperatures and different relative humidities are consistent with the measured shelf-life values at those conditions.
Conclusions
The new protocols and analyses provide accurate and precise shelf-life estimations in a reduced time from current state of the art.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
We recently reviewed the available literature on methods and current knowledge in the field of accelerated aging of pharmaceutical dosage forms (1). While the methods discussed in that review reveal a number of techniques in the field appropriate for a range of pharmaceutical dosage forms, the current paper focuses on the largest single category of pharmaceutical products: small-molecule solid dosage forms. Currently, accelerated aging processes for such dosage forms involve a range of conditions including such stress conditions as elevated temperatures and humidities; however, generally each organization uses a very limited range of conditions for such testing (often only a single condition). Samples are often aged in packaging with no corrections made for the role of the packaging in the accelerated aging process. In many stability studies, only a narrow range of conditions are used, typically 40°C/75% RH for 6–24 weeks. With single-condition stability studies, general guideline are often employed (e.g., 40°C/75% RH for 6 months corresponds to 2 years of shelf-life at 25°C/60%.RH). When multiple conditions are used, it has been difficult to connect the data obtained to meaningfully extrapolate to other conditions. Attempts at using Arrhenius fitting have often been unsuccessful.
The shelf-life at a given condition is set by the time it takes to form a specific degradation product or the total of all degradation products. In most cases, the shelf-life is limited by the rate of formation of the most prevalent degradation product; however, in some cases, a different degradant may have a lower qualified level and in fact become the limiting factor in setting shelf-life. In the current paper an improved accelerated aging protocol and statistical analysis for determining the chemical stability of both solid drug substances and formulated solid dosage forms are described. As with current methodologies, this improved protocol provides an indication of the rate of formation of each degradation product separately, which can in turn be used to set shelf-life. While theoretically the shelf-life of such products involves both their chemical and physical stabilities, for the majority of drugs in solid dosage forms, physical instabilities (i.e., gradual changes in dissolution rates rather than rapid adjustment to environmental humidity conditions) are extremely rare provided the most stable drug polymorphic form is used. Consequently, chemical instability (i.e., time to form a critical level of a limiting degradant) largely determines a solid dosage form’s shelf-life, with reduced time to determine the shelf-life potentially speeding the drug development process. Any accelerated aging process can result in erroneous predictions since there are intrinsic assumptions necessary when accelerating the processes. Although the occasional system will not follow the assumptions used in the predictions, the proposed approaches allow accurate estimates in most cases, and in dramatically reduced time-frames compared to traditional protocols. In addition, unlike previous protocols, the proposed protocols and analyses provide an explicit accounting for relative humidity’s effects on drug stability, which in turn, can help in packaging selection.
MATERIALS AND METHODS
The compounds used in this study and their primary degradation products are shown in Fig. 1.
Aspirin tablets (Brooks brand; 325 mg; containing dicalcium phosphate dihydrate, glyceryl triacetate, hydroxypropylmethyl cellulose, starch and talc) and Vitamin C tablets (Brooks brand; 500 mg USP; containing microcrystalline cellulose, cellulose, crospovidone, magnesium stearate, stearic acid, silica dioxide and sodium dodecylsulfate) were purchased commercially. Tablets were studied using bottles containing salt slurries (specifically sodium chloride or magnesium chloride) or desiccants (1 g Sorb-It™ canisters) to control the relative humidity. After storage in 20, 30, 40, 50 and 70°C chambers for 3 and 6 weeks, tablets were removed and stored at 5°C.
Tablets of CP-456,773 were prepared by blending 12.81 g of CP-456,773 (2), 186.69 g of Avicel PH200 and 99.00 g of mannitol 2080 in a bottle for 20 min using a Turbula™ blender. To this was added 1.50 g of magnesium stearate followed by an additional 3-min of blending. The blend was tableted (7/16″ SRC tooling, 500 mg per tablet) using an F-press. Tablets were stored at 5°C prior to placement in stability chambers.
Tablets of CP-481,715 were prepared by blending 6.02 g of CP-481,715 (3), 193.48 g of Avicel PH200 and 99.00 g of mannitol 2080 in a bottle for 20 min using a Turbula™ blender. To this was added 1.50 g of magnesium stearate followed by an additional 3-min of blending. The blend was tableted (7/16″SRC tooling, 500 mg per tablet) using an F-press. Tablets were stored at 5°C prior to placement in stability chambers.
Controlled release tablets of CP-481,715 were prepared by blending 6.02 g of CP-456,773-2, 193.48 g of Polyox WSR-N80 (PEO) and 99.00 g of mannitol 2080 in a bottle for 20 min using a Turbula™ blender. To this was added 1.50 g of magnesium stearate followed by an additional 3-min of blending. The blend was tableted (7/16″ SRC tooling, 500 mg per tablet) using an F-press. Tablets were stored at 5°C prior to placement in stability chambers.
Spray-dried CP-481,715 (4) was prepared by spray-drying a mixture of 0.375 wt.% HPMC (E3 Prem) and 0.125 wt.% of the drug from methanol. Tablets were prepared by blending 40 g of the spray-dried material, 164.29 g of Avicel PH200 and 80.00 g of mannitol 2080 in a bottle for 20 min using a Turbula™ blender. To this was added 1.43 g of magnesium stearate followed by an additional 5-min of blending. The blend was tableted (7/16″ SRC tooling, 500 mg per tablet) using an F-press. Tablets were stored at 5°C prior to placement in stability chambers.
Tablets of CP-865,569 were prepared by combining 69.6 g of the drug (5–7) with 297 g of lactose monohydrate (FastFlo™), 594 g of microcrystalline cellulose (Avicel PH102) and 30 g of sodium starch glycolate (Explotab™) in a V-blender. The blend was mixed for 15 min then milled through a Comill (speed 4, impeller 1609). The milled blend was mixed an additional 10 min, then 5 g of magnesium stearate was added, followed by an additional 5 min of blending. The blend was roller compacted through a Vector TF mini to a solid fraction of 0.62 (pressure, 375 psi; roller speed, 4 rpm; auger speed, 23 rpm). The ribbons were milled through a Comill, then blended for 10 min. Magnesium stearate was added (5 g) followed by 5 min blending. The blend was tableted using a Kilian T100 press with 1/4″ SRC tooling, to give 100 mg per tablet.
Instrumentation and Analytical Conditions
For the aspirin analysis, one tablet was added to a 100-mL volumetric flask, and about 50 mL of water added to facilitate the disintegration of the tablet. The solutions were sonicated for about 2 h then adjusted to volume with mobile phase. The solution was filtered through a 0.45 μm nylon filter (Gelman filter) fitted with a 10 mL syringe and further diluted 1–10 mL prior to analysis. The chromatographic system consisted of an Agilent 1100 HPLC chromatograph (Agilent Technologies) equipped with a binary solvent delivery system, thermostated column compartment, an autosampler and a photodiode array detector. Separation was performed using a YMC Pro C18 column (150 × 4.6 mm × 5 μm, 10-μL injection volume) maintained at 30°C. The mobile phase consisted of 25% acetonitrile and 75% of aqueous buffer (20 mM potassium phosphate monobasic, pH 2.25). Separation was done under isocratic conditions at a flow rate of 1.5 mL/min, and the analytes were monitored at a wavelength of 235 nm. Quantification was achieved by comparing chromatographic peak areas from a salicylic acid (Sigma-Aldrich) reference material as a standard.
For the ascorbic acid samples, a color analyzer model Labscan XE (Hunter Associates laboratory Inc., Reston, Virginia) was used. A calibration standard of dehydroascorbic acid was prepared by dissolving 200 mg of the material in 50 mL of water in a 100 mL volumetric flask, sonicating for about 15 min, then diluting to volume with acetonitrile. Samples were made from the stock solution by dilution to make 0.005, 0.025, 0.05, 0.5, 2.5 mg/mL. These dilute solutions were equivalent to 0.1, 0.5, 1.0, 10.0, and 50.0% concentration relative to the nominal sample preparation concentration (ascorbic acid at 5 mg/mL). Ascorbic acid sample solutions were prepared by combining one tablet and about 50 mL of water to a 100-mL volumetric flask. The solutions were sonicated for about 2 h then adjusted to volume with acetonitrile. The sample solutions were filtered through a 0.45-μm nylon filter and analyzed colorimetrically. The system was calibrated prior to sampling using the light and dark standards provided with the instrument. The calibrated color analysis used ΔE* as defined in Eq. 1
where ΔL* is the difference in lightness (L*) between the sample and the control, Δa* being the difference in red/green color (a*), and Δb* being the difference in yellow/blue color (b*). A calibration curve of ΔE* values versus the concentration of dehydroascorbic acid (Sigma-Aldrich) was used to quantify the amount of degradant in the ascorbic acid tablets.
For the CP-456,773 tablets, analysis of the degradation was analogous to earlier reported methods (8). A dissolving solvent was prepared by combining 750 mL of 50 mM Na2HPO4 with 250 mL of acetonitrile. One tablet and 50 mL of the dissolving solvent were combined and sonicated for 5 min, then placed on a shaker for 10 min. Samples were filtered through a 0.45 μm PTFE syringe filter before injection onto an HPLC column (YMC basic, 3 pm, 150 × 4.6 mm, column temperature 30°C, detection at 215 nm, flow rate of 1.5 mL/min, injection volume of 10 μL). The HPLC assay was a gradient consisting of part A being 50 mM KH2PO4 pH 5.2/acetonitrile (80/20), and part B being pure acetonitrile. The samples were eluted initially with 93 parts A, 7 parts B, then changing to 50:50 after 20 min. Degradant quantification was calculated based on the area percent of the degradant peak compared to the drug peak.
For the CP-481,715, one tablet and 70 mL of 10 mM NaH2PO4 were combined and sonicated for 30 min, and then the volume was adjusted with the dissolving solvent to 100.0 mL. Samples were filtered through a 0.45-μm Gelman Acrodisc PTFE filter before injection onto an HPLC column (YMC basic, 3 pm, 150X4.6 mm, column temperature 30°C, detection at 215 nm, flow rate of 1.5 mL/min, injection volume of 5 μL). The HPLC assay was a gradient consisting of part A being 50 mM NaClO4 in 0.2% H3PO4, part B being pure acetonitrile and part C being pure methanol. The sample was eluted initially with 88:7:5, (A:B:C) adjusting to 40:55:5 over 50 min. Degradant quantification was calculated based on the area percent of the degradant peak compared to the drug peak.
For CP-865,569, one 125 mgA tablet was accurately weighed and quantitatively transferred into a 100 mL flask. About 70 mL of dissolving solvent (2.76 g NaH2PO4 in 2.0 L water) was added, and the sample was sonicated for at least 30 min or until the tablet had fully disintegrated. Dissolving solvent was added to volume, then the solution was filtered using a Gelman Acrodisc 0.45 μm PTFE or 0.45 μm Nylon 25-mm syringe filter (discarding first 2 mL of filtrate) before injection onto an HPLC column (YMC basic, 3 pm, 150 × 4.6 mm, column temperature 30°C, detection at 210 nm, flow rate of 1.5 mL/min, injection volume of 5 μL). The HPLC assay was a gradient consisting of part A being 50 mM NaClO4 in 0.2% H3PO4, part B being pure acetonitrile and part C being pure methanol. The sample was eluted initially with 88:7:5, (A:B:C) adjusting to 40:55:5 over 50 min. Degradant quantification was calculated based on the area percent of the degradant peak compared to the drug peak.
Statistical Software
The propagation of errors for the extrapolated shelf-life estimations was carried out using a custom software program developed on the SAS statitical software package (available from SAS Institute, Gmbh, Heidelberg, Germany). In this program, an error in the concentration of degradation product at a given time was assigned a value based on either multiple sample measurements at that condition or based on overall quantification of error for the entire data set (assuming poolability). From this error, a T-distribution of 5,000 points around the average value was generated based on the Monte-Carlo approach incorporated in SAS. These points were used to determine a distribution of rate constants assuming a zero-order function (linear) by least squares fit to the data, including the zero-time point. The error was propagated through the logarithm function for each temperature and relative humidity condition. These data were fit with a multiple regression package on SAS to determine three parameters, with each set of data. The fits were extrapolated to the shelf-life conditions with the overall error determined based on the distribution of the points generated.
RESULTS AND DISCUSSION
To achieve rapid shelf-life estimations for solid drug substances and products, three concepts are used together. These concepts include performing stability studies taking into account an isoconversion paradigm (to compensate for heterogeneous kinetics) and a moisture-corrected Arrhenius equation (to compensate for the effect of relative humidity on reaction rates). The data from these experiments are then analyzed using statistics to explicitly account for imprecision in the data and extrapolations. These concepts are described in detail in the following sections.
Isoconversion Paradigm
An organic compound in solution can undergo chemical reactions to give one or more products, with each product produced according to a rate equation. In a simple case, a compound reacts to give a single product, with the rate depending on the concentration of the initial compound still present (i.e., first order). For drug substances and drugs in solid dosage forms, this simple case will involve the same kinetic processes, albeit generally at a much slower rate. However, if the drug is present in a mixture of forms (e.g., crystalline, defect site, amorphous, solid solutions), this simple process can become more complicated. Typically, the rate of reaction for amorphous drugs is orders of magnitude greater than that for crystalline material. In some cases, reaction from crystalline drug may involve a reactive-form intermediate. Assuming either that a particular solid-state reaction proceeds from each form directly or through a reactive-form intermediate, there will be an initial rapid rate of reaction due to any reactive-form material present (due to processing steps, especially in the presence of excipients) followed by a slower rate (steady state) as this material is consumed as represented kinetically below (where Dcrystalline is the crystalline drug, Dreactive is the more reactive drug form and P is the reaction product):

The difference in the rates reflected in Eqs. 3 and 4 can be quite significant since k2 is often much greater than k1 or k3.
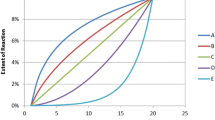
As an illustration, a calculated example of this heterogeneous behavior is shown in Fig. 2, where a small amount of reactive-form drug and a large amount of crystalline drug progress to a product with k2 assumed to be much greater than keff. As can be seen in this figure, the first part of the product formation curve is dominated by the small amount of rapidly reacting material, while the latter part of the reaction is dominated by the slower, but more prevalent crystalline phase. Deconvoluting the two component factors in the kinetics from the product formation curve can require a number of points taken throughout the course of reaction: a process that is labor and time-consuming.
As one increases the temperature (or humidity), the two component rate expressions of the model heterogeneous system from Fig. 2 can change their relative contributions based on their respective activation energies (and moisture sensitivities). Determining an Arrhenius expression for this system would not only requires sufficient data at each temperature to deconvolute the relative contributions from the individual rates, but also requires sufficient temperature measurements to deconvolute the potentially different activation energies. As becomes clear, even with a simple case (one drug to one product, constant relative humidity), an experimental design becomes difficult to implement in a timely and efficient process.
The opposite issue arises when an inhibitor (e.g., an antioxidant) is present: initial reaction is suppressed then proceeds as the inhibitor is consumed. Since the activation energetics for inhibitor degradation may be different than that for the drug degradation, deconvolution can be complex.
In practice, however, the expiration date for a drug product is generally limited by the rate of formation of the first 0.2–0.5% of a product (with respect to the starting drug level). The low degradation percentage that is relevant for expiry setting often means that only the faster of the degradation processes actually contributes significantly to the rate up to that level of degradation. This allows a simplification of the heterogeneous rate expression to reduce to a homogeneous expression (e.g., Eq. 3), albeit with validity only to conversions where the one rate dominates. Whether this rate is first order or zero order, the process can be approximated as zero order; i.e., the rate constant can be estimated from the initial slope. This approximation is best suited for conversion percentages that are lower than the amount of drug initially in the reactive form.
As one increases the temperature (and relative humidity), the approximation that the product formation is only a function of the rate for reactive-drug form will remain valid only if the percentage of drug product produced remains low. Maintaining the amount of degradant at a constant low value can be considered an isoconversion paradigm: the conversion is maintained within the same drug-form kinetics even as the conditions provide greater rates of reaction. Isoconversion principles have been applied previously to thermal analyses of drug stability when activation parameters vary with conversion percentage (9,10). To use the proposed isoconversion paradigm for each degradation product, a critical degradation product level (corresponding to the conversion percentage which limits expiry) is assigned which determines the appropriate time a sample should remain in a stability chamber. The isoconversion paradigm can be contrasted with using fixed stability times at each accelerated stability condition in the following illustrative examples:
-
Example 1
Homogeneous kinetics: product forms from a single drug form or with the same rate for different forms
In this example, whether the rate constant for the amorphous and crystalline drug forms are the same throughout the temperature range, or the rate of conversion between crystalline drug and amorphous drug is fast, the result is a single rate of conversion to product. Whether one uses the isoconversion paradigm or maintains a constant time, the extrapolated Arrhenius fit will be equivalent, as shown in Fig. 3. When the kinetics are homogeneous, in fact, greater conversions generally allow more precise determinations of the rate constants. The result is that the reliability of the extrapolated product formation rate, and corresponding shelf life, is greater with greater amounts of degradant formation. It is still advisable to maintain relatively low conversion to be consistent with the zero-order approximation.
-
Example 2
Reactive-form drug reacts faster than crystalline drug
This example involves the common situation where a degradant forms faster from a small amount of amorphous drug present in a solid dosage form. In this case, a constant time stability sampling will shift to a greater percentage contribution from the slower kinetic process as the temperature increases (greater extent of reaction). The result, as shown in Fig. 4, is that the Arrhenius plot extrapolates to indicate a greater instability than actually found. In contrast, the isoconversion paradigm maintains kinetics based on the less stable (amorphous) drug throughout the temperature range. The result (Fig. 4) is that the projected stability is consistent with the actual stability based on the model conditions.
As an experimental illustration of this behavior, the drug candidate CP-456,773, which hydrolyzes to CP-470,465, was examined in tablet formulation. In Fig. 5, this process is followed as a function of time, showing non-linear kinetics, even with relatively low amounts of degradation. As can be seen, there is a faster initial rate of degradant formation followed by a slower rate. As temperature increases, the behavior follows that illustrated in Fig. 4: extrapolation based on the isoconversion paradigm provides a better low temperature estimate than that based on a constant time (Fig. 6).
-
Example 3
Inhibitor consumed before any product formed
In a number of solid pharmaceutical formulations, the presence of an inhibitor (e.g., antioxidant) prevents a degradation pathway until the inhibitor is substantially consumed, at which time the drug degradation can proceed rapidly. The reaction therefore has a lag time before proceeding (Fig. 7). While using the zero-order approximation is clearly in error, the isoconversion concept still allows for a reasonable prediction (and better than a process using a set time at each point) of the shelf-life at lower temperatures as shown in Fig. 8. With a matched time for each temperature, the effect of the lag time decreases as the temperature increases. This serves to make the drug appear relatively less stable at higher temperatures (faster rate), which results in a prediction of greater extrapolated lower temperature stability than will actually be observed.
Obviously, there are many other scenarios which will each have different consequences to the rate and accuracy of any extrapolation. Ultimately, however, the isoconversion concept will provide a reduced likelihood of erroneous predictions for complex kinetic systems compared to fixed exposure time conditions, and dramatically less risk than using a single temperature condition.
Arrhenius plot for calculated system where rate of product formation for both amorphous and crystalline are equal (4.2 × 10−6) with equal activation energies (22 kcal/mol) with first material at a lower level (0.5%) than second (98%). The isoconversion (to 0.20%) model (squares) and matched exposure time (42 days) model (triangles) both extrapolate to the actual 30°C value (diamond) of the model.
Calculated Arrhenius plot based on Fig. 2 assuming k2 >> keff (k2 = 4.2 × 10−4; keff = 4.2 × 10−7) with first material at a lower level (0.5%) than second (98%); Ea2 = Ea eff = 22 kcal/mol. The isoconversion (to 0.20%) model (squares) and matched exposure time (42 days) model (triangles) extrapolate to shelf-lives (at 30°C) of 2.54 and 1.14 years, respectively, compared to the actual 30°C value (diamond) of the model of 2.55 years.
Arrhenius plots of rate of intramolecular cyclization from tablets of CP-456,773 stored at 60%RH using an isoconversion paradigm (i.e., adjusting pull-times to give similar conversions at each temperature) vs. using constant exposure-times independent of temperature showing closer agreement of the former predictive modeling method to observed (experimental) 30°C rate (note that the 30°C value was not used in either line fitting).
Calculated Arrhenius plot based on Fig. 7 assuming the activation energies for both the inhibitor loss and product formation are 22 kcal/mol. The isoconversion paradigm uses a constant 0.2% conversion, while the matched time curve uses 20 days for each temperature. The extrapolated shelf-life to 30°C and 0.2% product is 639 and 308 days for the matched time and isoconversion methods, respectively. The actual value based on the model is 300 days.
Decoupling Relative Humidity
The effect of relative humidity on reaction rates for solid pharmaceuticals can be expressed by the following equation:
where k is the rate constant, A, Ea and B are fit constants with the variables temperature, T, and percent relative humidity (%RH) (11). There are two important aspects of this equation: the form of the relative humidity sensitivity and the independence of the temperature and relative humidity terms. The humidity sensitivity from Eq. 5 predicts a linear response of ln k versus the percent relative humidity in isothermal experiments. This is shown, for example, with the drug CP-481,715 in Fig. 9. Further examples are shown in Table I where in each case, a linear relationship was found between ln k and the percent relative humidity at a constant temperature. Table I tabulates the slopes (B values) for a range of drugs/formulations from the literature and present study. As can be seen, these values vary considerably with different systems with no clear trend. In particular, hydrolytic reactions are no more moisture sensitive than non-hydrolytic reactions, suggesting that the humidity sensitivity is dominated by physical effects (plasticization) rather than any direct reaction with water. The average and median for the B-values of Table I are both 0.04. This means that an increase in relative humidity of 50% (e.g., from 20 to 70%) will lead to a seven-fold increase in degradation rate for the average system.
Another aspect of Eq. 5 is that the temperature and humidity effects are independent; that is, there are no cross-terms in the equation. This was examined with a number of model tablets by determining the B-values at different temperature conditions (see Table II). As can be seen, the B-values are generally independent of temperature consistent with the model.
Using Eq. 5, systems that might be considered non-Arrhenius in the solid state, in fact behave in a predictable manner. Obviously, if relative humidity is not controlled at any elevated temperature, the results could very well not appear Arrhenius. This is shown, for example, in Fig. 10 where a drug degradation process appears non-Arrhenius when relative humidity is not kept constant; however, when it is maintained at a constant value, the behavior fits the Arrhenius equation. It should be noted that this equation applies to samples stored under conditions where the material is exposed to the indicated relative humidity, i.e., in open bottles. In closed bottles, blisters, or bottles with desiccants, the relative humidity inside the package as a function of time affects the overall drug stability (B. MacDonald, M. Roy, S. Shamblin, K.C. Waterman, manuscript in preparation).
Proposed Protocol: Early Development
In the early phases of formulation development, the challenge in establishing an isoconversion stability protocol is that one does not know, a priori, what time, at each temperature and humidity condition, will generate the critical degradant concentration. If the extent of reaction is too great, there is a risk that the corresponding kinetics represent a significant contribution from a less releactive drug form. If too little degradation occurs, there can be insufficient data to extrapolate a meaningful shelf-life from. Acknowledging this issue, a stability protocol can be used based on average behaviors; however, significant deviations from the average can lead to greater error bars in the predictions. In virtually all cases, however, the direction of deviation from the assumed activation parameters is apparent. For example, if greater degradation than the isoconversion paradigm occurs at higher temperatures, the activation energy is too high (and vice versa). In practice, the significantly reduced times involved in making these shelf-life predictions often enables a second round (based on the preliminary data) to be conducted in less time than a standard lower temperature protocol. In any formulation development beyond the initial stability investigation, the time that a sample is stored at a condition can be based on the activation energy (and relative humidity sensitivity as discussed below). Building upon preliminary activation parameters, as stability screens are performed during the drug development process, allows for more rapid and accurate projections.
With the isoconversion paradigm and the moisture-corrected Arrhenius equation, it is now possible to effectively use higher temperatures than previously considered useful. While it is possible that multiple pathways to the same product, each with different activation energetics, can lead to behavior that does not fit this model, this is not a common occurrence. What is more often seen is that the relative distribution of products changes with temperature, yet does not affect the predictions for each product. Determining the overall shelf-life may require determining the limits set by multiple products to find which product is limiting at a given condition.
To take advantage of the isoconversion paradigm and the humidity-decoupled Arrhenius equation (Eq. 5), an optimal experimental design with a reasonable number of experiments (and limited number of storage chambers) can be proposed which maintains the kinetics under each condition to be in a similar manifold (i.e., kinetics for the amorphous drug) assuming, at least in initial studies, an average behavior for the drug. Since temperature and humidity are independent variables in the solution to Eq. 5, a minimal set of three experiments with varying temperature and humidity is required, with no degree of freedom remaining in the solution. Additional conditions provide improved precision in the overall estimation. It is also possible to assume some contribution from a temperature and humidity cross-term and allow this coefficient to be determined as part of any fitting program. The independence of temperature and percent relative humidity seen from Table II, however, suggest that this is generally not necessary. Adding the cross-term necessitates a greater data set to get a comparable precision of fitting (four vs. three fitted parameters).
One can set a maximum temperature (up to about 80°C) used in a stability study up to the melting temperatures of the drug or excipients. The higher the temperature and humidity conditions used, the faster a stability study can be completed; however, the greater the distance for extrapolation to shelf-life conditions, the greater the loss in precision, as will be discussed below. In early formulation development, screening studies (e.g., excipient compatibility screening) can be somewhat imprecise since one is generally looking for the best excipients to use, rather than providing an exact shelf-life determination. In such screening processes, simple protocols can be proposed using an average activation energy (about 22 kcal/mol, see Table I) and an average humidity sensitivity (B-value of 0.04, see Table II). These average values may eventually be able to be refined based on information about a specific drug, such as degradation mechanism; however, in the absence of other information, they represent reasonable starting points. The times at each condition can be estimated using Eq. 6:
where t T,RH is the time at an oven temperature T and humidity RH, t prediction is the time at the shelf-life predicting condition, R is the gas constant and Ea is the activation energy. As an example, to predict a one-year degradation level at 25°C and 60%RH, the calculation for 50°C and 70%RH is as follows:
A generic protocol is proposed in Table III that varies temperature and humidity. This design decouples humidity and temperature, and provides a rapid estimation of the parameters of Eq. 5. An extra sample is allowed to age in the oven at 70°C and 75% RH to provide some stability information for very stable formulations. If the amount of degradation under that condition is significantly above the critical degradant concentration, only the earlier time point should be used in the data analysis.
Proposed Protocol: Late Development
The high degree of imprecision in the shelf-life estimate from the two-week protocol of Table III is appropriate in early phases of product development, but may be unacceptable at later phases. Traditional shelf-life programs involve lengthy stability studies which do not provide adequate decoupling of the humidity and temperature effects on stability to make accurate predictions beyond the actual test conditions themselves. If, on the other hand, the data from the preliminary investigations are available, it is possible to carefully select the residence times of the samples in chambers for the isoconversion paradigm (based on Eq. 6), providing a reduced overall time for the study and adequate decoupling of temperature and humidity. These methods also allow adaptation of the conditions based on any lot-to-lot variability in initial drug substance purity. In the end, the proposed system-specific protocol will have a quantifiable error bar on any predicted shelf-life (as discussed below) which can be refined over time by adding measurements from long-term (low temperature, humidity) samples. In practice, relatively unstable systems can be quickly identified since there is adequate data at short times to make precise predictions. For more stable systems, predictions may have large error bars yet allow for confident minimal shelf-life determinations, as will be discussed below.
Propagation of Errors Using Monte Carlo Method
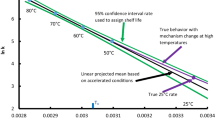
Once stability data are obtained from the protocol as described above, it is desirable to not only provide a reasonable estimate of the shelf-life at a given temperature and humidity condition, but also to assess the precision of the prediction. The errors in quantification of the degradant level at each temperature, relative humidity, and time condition (“cell”) propagate through to the rates at those temperature-RH conditions, and ultimately to the final fit based on Eq. 5. In order to provide a convenient method for calculating this error, we have employed a Monte-Carlo simulation approach. In this approach, the data in each cell are assumed to come from a Normal distribution, with the mean equal to the average degradant value for that cell, and with the standard deviation being representative of the within-cell variability. The Monte-Carlo computer program uses the Normal distribution to generate 5,000 simulated experiments, and applies Eq. 5 to the data from each simulated experiment, in order to construct confidence limits on degradation rates at any temperature-RH condition. As one would expect, the simulation shows that the greater the extrapolation with respect to temperature, the greater the corresponding error bars are around the predicted values. This can be seen in Fig. 11 (where the relative humidity has been kept constant). Similarly, the error bars with respect to the relative humidity depend on the distance from the average relative humidity.
The error associated with each degradant at a given time, temperature and relative humidity contributes to the eventual error in the extrapolated predicted stability. To determine the error at each condition, the most thorough, and most resource consumptive, method would be to assay multiple samples at each condition. Another approach assumes that the errors at all the conditions are poolable statistically. Under this scenario, the error for each condition is assumed to be a constant standard deviation. The error can be determined using repeat measurements at any one condition or sets of conditions. In the latter case, the assumption of poolability can be tested statistically, and adjusted if needed.
Statistical extrapolation of data with decoupled humidity and temperature (according to Eq. 5) has been applied to a number of test drugs formulated in tablets (see Table IV). As can be seen in the table, there is generally good agreement between the extrapolated predictions and the actual experimental data. This is true even though the types of degradation processes, types of solid dosage forms (crystalline drug in immediate release or controlled release dosage forms, amorphous dispersions) and range of stabilities vary widely.
It should be noted that the shelf-life estimations, with error bars, as described above provide an analysis only of the given system studied. To determine the variability of a particular dosage form with respect to batch to batch differences, this study would need to be carried out (at least in part) for each batch independently, as is generally common practice presently. One advantage of the proposed protocol is that it should be possible to determine such batch sensitivity more efficiently, i.e., in less time.
Handling Very Stable Systems
If no degradation above the noise level is observed under a particular condition, it is still possible to use that fact to provide a prediction of stability. One can use the Monte-Carlo approach to simulate degradation at a level below quantification by assuming the “true” amount of degradant under a particular condition is somewhere between zero and the limit of quantification (or limit of detection). The rate at that condition will then be represented as a distribution of the simulated concentrations divided by the appropriate storage time. This approach can allow an improved estimation of shelf-life, at least in terms of error bars. As an extreme case, a shelf-life can be quantitatively estimated even in the situation where there are no detectable degradant levels at any condition examined. For example, a recent drug candidate was studied in a three-week protocol with the following conditions: 50°C/20%RH/21 days, 50°C/60%RH/21 days, 60°C/5%RH/15 days; 60°C/75%RH/10 days; 70°C/5%RH/4 days and 80°C/40%RH/2 days. Under all conditions, the level of the degradants was found to be below the limit of quantification (0.005%). The above Monte-Carlo simulation was applied to the data using a normal distribution of points based on a degradant concentration in the range of 0.000–0.005% in each cell. From this, a shelf-life at 30°C/60%RH (to 0.2%) was determined to be 59 years with a 90% confidence interval of 2.5–1,390 years. Even though the data indicate a very large error bar, there is high confidence that a two-year shelf life can be set. This approach allows even very stable systems to be examined in rapid protocols. Once these initial data were obtained, the subsequent protocols provided greater times at higher stress conditions and thereby reduced the error bars (on the low end) for shelf-life estimations.
CONCLUSIONS
Reliable estimates for ambient shelf-life values for small molecule drugs in solid dosage forms can be achieved in relatively short times by combining an experimental design that decouples temperature and relative humidity effects with an isoconversion paradigm. Effectively, the times in each stability chamber are set to provide approximately the same amount of drug degradation product as the predicted conditions. The degradation kinetics can be analyzed using a humidity-corrected Arrhenius equation. Imprecision in the data can be effectively incorporated using a Monte-Carlo simulation to propagate the variation inherent in the experiment and provide error bars at extrapolated conditions. In early development phases, greater imprecision in predictions is tolerated to allow faster screening with reduced sampling. A two-week protocol is proposed that provides a quick screen for excipient compatibility. As drug development progresses, these early development data can be used to provide case-specific accelerated stability test conditions, optimized for the isoconversion principle, i.e., to provide similar degradant levels at each test condition. The reported examples show that predicted shelf-life values at lower temperatures and different relative humidities are consistent with the measured shelf-life values at those conditions.
References
K. C. Waterman, and R. C. Adami. Accelerated aging: prediction of chemical stability of pharmaceuticals. Int. J. Pharm. 293:101–125 (2005).
F. J. Urban, V. J. Jasys, J. W. Raggon, R. A. Buzon, P. D. Hill, J. F. Eggler, and J. D. Weaver. Novel synthesis of 1-(1,2,3,5,6,7-hexahydro-s-indacen-4-yl)-3-[4-(1-hydroxy-1-methylethyl)furan-2-sulfonyl]urea, an antiinflammatory agent. Synth. Comm. 33(12):2029–2043 (2003).
B. Li, B. Andresen, M. F. Brown, R. A. Buzon, C. K.-F. Chiu, M. Couturier, E. Dias, F. J. Urban, V. J. Jasys, J. C. Kath, W. Kissel, T. Le, Z. J. Li, J. Negri, C. S. Poss, J. Tucker, D. Whritenour, and K. Zandi. Process development of CP-481715, a novel CCR1 antagonist. Org. Proc. Res. Dev. 9(4):466–471 (2005).
D. T. Friesen, M. J. Gumkowski, R. J. Ketner, D. A. Lorenz, J. A. S. Nightingale, R. M. Shanker, and J. B. West. Pharmaceutical compositions of dispersions of drugs and neutral polymers. Int. Patent Appl. WO 2003000235A1 (2003) p. 210.
M. M Hayward. Preparation of [(2-piperazinyl-2-oxoethoxy)phenyl]alkanesulfonic acids and analogs as CCR1 receptor antagonists for treatment of inflammation and immune disorders. Int. Patent Appl. WO2002102787A2, p. 44 (2002).
M. F. Brown, A. S. Gaweco, R. P. Gladue, and M. M. Hayward. Preparation of piperazine sulfonic acid derivatives as chemokine receptors CCR1 antagonists for the treatment of fibrosis, Alzheimer disease and other disorders Int. Patent Appl. WO2004039377A1, p. 56 (2004).
U. Kaufmann. Preparation of piperazine derivatives as CCR1 antagonists for the treatment of endometriosis. Int. Patent Appl. WO2005079769A2 pp. 291 (2005).
K. M. Alsante, P. Boutros, M. A. Couturier, R. C. Friedmann, J. W. Harwood, G. J. Horan, A. J. Jensen, Q. Liu, L. L. Lohr, R. Morris, J. W. Raggon, G. L. Reid, D. P. Santafianos, T. R. Sharp, J. L. Tucker, and G. E. Wilcox. Pharmaceutical impurity identification: A case study using a multidisciplinary approach. J. Pharm.Sci. 93(9):2296–2309 (2004).
T. Vlase, G. Vlase, and N. Doca. Thermal stability of food additives of glutamate and benzoate type. J. Therm. Anal. Calor. 80(2):425–428 (2005).
G. T. Long, S. Vyazovkin, N. Gamble, and C. A. Wight. Hard to swallow dry: kinetics and mechanism of the anhydrous thermal decomposition of acetylsalicylic acid. J. Pharm. Sci. 91(3):800–809 (2002).
S. Yoshioka and V. J. Stella. Stability of Drugs and Dosage Forms, Plenum, New York, 2000, pp. 108–113.
T. Hladon, B. Cwiertnia. The effect of humidity on the stability of diclofenac sodium in inclusion complex with ß-cyclodextrin in the solid state. Pharmazie 54(12):943–944 (1999).
D. Genton and U. W. Kesselring. Effect of temperature and relative humidity on nitrazepam stability in solid state. J. Pharm. Sci. 66:676–680 (1977).
M. Zajac. Stability of crystalline mecilliname sodium salt in the solid phase. Acta Pol. Pharm. 41:659–664 (1984).
M. C. Lai, M. J. Hageman, R. L. Schowen, R. T. Borchardt, and E. M. Topp. Chemical stability of peptides in polymers. 1. Effect of water on peptide deamidation in poly(vinyl alcohol) and poly(vinyl pyrrolidone) matrixes. J. Pharm. Sci. 88(10):1073–1080 (1999).
L. N. Bell and M. J. Hageman. Differentiating between the effects of water activity and glass transition dependent mobility on a solid state chemical reaction: aspartame degradation. J. Agric. Food Chem. 42:2398–2401 (1994).
Z. Plotkowiak. The effect of chemical character of certain penicillins on the stability of the ß-lactam group in their molecules. Pharmazie 44:837–839 (1989).
E. Pawelczyk, Z. Plotkowiak, and M. Helska. Kinetics of thermal decomposition of talampicillin hydrochloride in the solid state. Pharmazie 55(5):390–391 (2000).
F.Y. Tripet and U.W. Kesselring. Etude de stabilité de l-acide folique à l’état solide en function de la température et de l’humidité. Pharm Acta Helv. 50(10):318–322 (1975).
R. G. Strickley and B. D. Anderson. Solid-state stability of human insulin II. Effect of water on reactive intermediate partitioning in lyophiles from pH 2–5 solutions: stabilization against covalent dimmer formation. J. Pharm. Sci. 86(6):645–653 (1997).
Acknowledgments
The authors would like to acknowledge the assistance of Dr. Julie Lorenz for her helpful discussions and suggestions. The authors would also like to acknowledge the assistance of Yan Liu, Shilpa Naik and Yukun Ren, each of whom contributed to the programming of the Monte-Carlo simulation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Waterman, K.C., Carella, A.J., Gumkowski, M.J. et al. Improved Protocol and Data Analysis for Accelerated Shelf-Life Estimation of Solid Dosage Forms. Pharm Res 24, 780–790 (2007). https://doi.org/10.1007/s11095-006-9201-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-006-9201-4