Hemorheological and antiaggregant properties of new o-isobornylphenol derivatives were investigated in ex vivo experiments. 4-Methyl-2,6-diisobornylphenol and 2-(dibutylamino)methyl-4-methyl-6-isobornylphenol hydrochloride demonstrated the maximum hemorheological activity. After intragastric administration, these compounds decreased the blood viscosity at low shear rates, suppressed the development of blood “hyperviscosity” before incubation (20.0 ± 0.4°C, 1 h), and reduced ADP-induced (4 × 10–6 M) aggregation of platelets. The hemorheological and antiaggregant effects of the investigated compounds were comparable to those of pentoxifylline.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Blood rheology disorders such as an increase of blood viscosity, an elevated aggregation of erythrocytes, and their detrimental deformation are characteristic of many cardiovascular diseases (hypertension, atherosclerosis, ischemic heart disease) [1, 2]. An escalation of free-radical processes can contribute to the disruption of the micro-and macrorheological properties of blood [3, 4]. Thus, it was shown [5] that activation in erythrocytes of free-radical processes decreases the viscosity and deformation of erythrocyte membranes and alters the erythrocyte morphology, thereby changing the ability of these cells to aggregate and deform. Furthermore, active oxygen species formed during free-radical processes stimulate thrombocyte aggregation, which in turn aggravates the course of the aforementioned diseases [6].
Research during the last decades has shown that hemorheological disorders can be corrected and the threat of thrombus formation can be reduced by using non-specific antioxidant therapy [7–14].
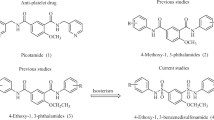
The goal of the present work was to investigate the hemorheological and antiaggregant activity of new semi-synthetic derivatives of o-isobornylphenol (I – III) that exhibit high antioxidant activity and low toxicity [15–17].

Experimental chemical part
Melting points were determined on a Kofler block and are uncorrected. The course of reactions and purity of products were monitored by TLC on Sorbfil plates using petroleum ether:Et2O (5:1). Compounds on plates were detected by treatment with aqueous KMnO4 solution (5%) containing conc. H2SO4 (0.15 mL). IR spectra were recorded in KBr pellets on a Specord M-80 instrument. PMR and 13C NMR spectra were recorded in CDCl3 on a Bruker DRX-400 spectrometer (400 MHz for 1H; 125, 13C). Benzene was dried over CaCl2 and distilled over metallic Na. The petroleum ether fraction with bp 65 – 70°C was collected. Column chromatography used silica gel (Alfa Aesar 70/230 μm) and was packed wet.
The studied terpenophenols 2-methyl-6-isobornylphenol (I), 4-methyl-2,6-diisobornylphenol (II), and 4-methyl-2-isobornylphenol, which was starting material for the synthesis of the aminomethylphenol hydrochloride (III), were prepared by the literature method [18].
1,7,7-Trimethyl-2-exo-(2-hydroxy-3-methylphenyl)bicycle[2.2.1]heptane (I), light-yellow crystals, mp 85°C. IR spectrum (νmax , cm–1, KBr): 3620 (O—H), 2960 and 1464 (CH3, CH2), 1188 (=C—O), 824 and 760 (C—H).
PMR spectrum (δ, ppm, J/Hz, CDCl3): 0.78 sec, 0.84 sec, 0.89 sec (9H, C10H3, C9H3, C8H3), 2.24 (s, 3H, C17H3), 1.33 – 1.38 (m, 1H5, CH2), 1.41 – 1.45 (ddd, 1H6, J = 9, 3, 3, CH2), 1.55 – 1.65 (m, 2H3,6, CH2), 1.84 – 1.87 (m, 2H4,5,CH2), 2.18 – 2.23 (m, 1H3, CH2), 3.07 (t, 1H2, J = 8.8), 4.65 (s, OH), 6.8 (t, 1H15, J = 7.6), 6.94 (d, 1H14, J = 7.3), 7.15 (d, 1H16, J = 7.8).
Mass spectrum (m/z): 244 [M]+, 134 (100), 109 (14), 121 (41), 229 (20).
4-Methyl-2,6-bis-exo-(1,7,7-trimethylbicyclo[2.2.1]heptan-2-yl)phenol (II), colorless crystals, mp 206 – 208°C. IR spectrum (νmax, cm–1, KBr): 3600 – 3000 (O—H), 1170 (=C—O), 880 and 770 (C—H).
PMR spectrum (δ, ppm, J/Hz, CDCl3): 0.81 sec, 0.85 sec, 0.91 sec (18H, C10,10′H3, C9,9′H3, C8,8′H3), 2.29 (s, 3H, C17H3), 1.31 – 1.47 (m, 4H, H5,5′, H6,6′, CH2), 1.54 – 1.71 (m, 4H, H3,3′,6,6′, CH2), 1.83 – 1.92 (m, 4H, H4,4′,5,5′, CH2), 2.22 – 2.31 (m, 2H, H3,3′, CH2), 2.99 (t, 2H2,2′, J = 8.8), 4.66 (s, OH), 6.96 (s, 2H, H14, H16).
13C NMR spectrum (δ, ppm, 100 MHz, CDCl3): 151.84 (C-12), 128.49 (C-11), 125.77 (C-14, C-16), 127.69 (C-15), 49.92 (C-1), 48.18 (C-7), 46.09 (C-4), 45.48 (C-2), 40.03 (C-6), 33.93 (C-3), 27.57 (C-5), 21.44 (C-8), 20.24 (C-9), 12.50 (C-10). C27H40O.
2-[(Dibutylamino)methyl]-4-methyl-6-{exo-(1,7,7-trimethylbicyclo[2.2.1]hept-2-yl)}phenol hydrochloride (III), colorless powder, mp 70 – 72°C (Et2O). 4-Methyl-2-isobornylphenol (4.0 mmol) and paraformaldehyde (4.8 mmol) were dissolved in anhydrous benzene (20 mL) at 20°C, treated with di-n-butylamine (4.8 mmol), and refluxed for 6 h. When the reaction was finished, the excess of solvent was removed at reduced pressure. The reaction mixture was separated over a column (Silicagel 70/230 μm, eluent petroleum ether:Et2O with increasing fraction of the latter). The resulting amine was dissolved in Et2O and treated dropwise at room temperature with alcoholic HCl (2N) until the pH was 6. The precipitate of the hydrochloride was filtered off, washed with Et2O, and dried in vacuo. Elemental analysis of III agreed with that calculated.
Experimental biological part
Hemorheological activity of the o-isobornylphenol derivatives was studied using 25 Wistar male rats (250 – 300 g). Derivatives I, II, and III were injected intragastrically at a dose of 100 mg/kg as suspensions in starch paste (1 mL). The reference drug was pentoxifylline, which was injected intragastrically to rats at a dose of 400 mg/kg. Control animals received starch paste (1 mL). The intragastric injection was made 1 h before collecting blood.
Blood was collected for the study from a common carotid artery under ether anesthesia. Sodium citrate solution (3.8%) was added to the blood as a stabilizer (1:9 ratio).
Blood viscosity was measured in an AKR-2 rotation viscosimeter in the shear rate range 5 – 300 sec–1. Spontaneous aggregation of erythrocytes was studied using the sillectometry method [19] as modified by us [20]. The criterion of erythrocyte aggregation activity was the half-life of aggregation T 1/2. Rheological indices were studied before and after incubation of blood at 20.0 ±0.4°C for 60 min, which reproduced the in vitro blood hyperviscosity model.
Thrombocyte aggregation in thrombocyte-rich plasma (TRP) was determined by the nephelometry method of Born [21]. Thrombocyte aggregation was estimated in standardized plasma [13] on an AT-02 instrument. Aggregatograms were recorded using a Recorder 2210. The aggregation inductor was ADP at a final concentration of 4 × 10–6 M.
Animals were housed according to rules adopted by the European Convention on the Protection of Vertebrate Animals Used for Experimental and Other Scientific Purposes (Strasbourg, 1986). Animals were euthanized after the completion of the experiments by an ether overdose.
Statistical processing was carried out using the Statistica 6.0 software. The average and standard deviation were calculated. The Student t-criterion was used in order to find inter-group differences.
The initial blood viscosity values at shear rates 5 – 300 sec–1 for control animals fell in the range from 8.5 ± 0.2 to 4.4 ± 0.1 mPa·s. Incubation of these blood samples for 60 min at 20.0 ± 0.4°C produced a significant (by 14 – 31%) increase in the blood viscosity (Table 1). The increase of blood viscosity after incubation can be explained by the development of lactacidosis under normoxic conditions that was caused by catabolic changes in the cytoskeleton and plasmalemma of erythrocytes. These led to a degradation of the blood rheological properties [22–24].
Pentoxifylline caused a reduction of blood viscosity at low shear rates by 6 – 14% that was statistically significant compared with the controls. The blood viscosity increased after incubation over the whole range of shear rates. However, the values of this parameter were reliably lower by 8 – 24% compared with the controls (Table 1). Thus, intragastric injection of pentoxifylline to rats improved the initial hemorheological value at low shear rates and inhibited the development of blood hyperviscosity under in vitro conditions.
Compounds II and III of the studied o-isobornylphenol derivatives had significant effects on blood viscosity. Rats that received these compounds showed a reliable viscosity reduction at low shear rates by 6 – 14% and 2 – 15%, respectively. The blood viscosity values after incubation at shear rates from 5 to 100 sec-1 were lower in both groups compared with the controls (by 6 – 25%).
The initial erythrocyte aggregation values were not statistically different among the groups (Table 2). Incubating blood of the control group of rats increased erythrocyte aggregation by 35% (p < 0.05). Injecting pentoxifylline, II, and III suppressed erythrocyte aggregation upon incubation. This was seen in the reliable increase of erythrocyte aggregation half-life compared with the controls by 34, 25, and 24%, respectively (Table 2).
The amplitude of ADP-induced thrombocyte aggregation in the control was 28 ± 1%. Intragastric injection of pentoxifylline reduced this parameter to 19%. The o-isobornylphenol derivatives studied by us exhibited a pronounced antithrombocyte activity. The amplitude of ADP-induced aggregation was 17 – 18%, which was 32 – 39% less than the control value and comparable with the effect of pentoxifylline (Fig. 1).
Effect of Single Intragastric Injection of Pentoxifylline (400 mg/kg), 2-Methyl-6-isobornylphenol (100 mg/kg, I), 4-Methyl-2,6-diisobornylphenol (100 mg/kg, II), and 2-(Dibutylamino)methyl-4-methyl-6-isobornylphenol hydrochloride (100 mg/kg, III) on Amplitude of ADP-Induced Thrombocyte Aggregation. Note: + p < 0.05 compared to control.
Thus, the results suggest that the o-isobornylphenol derivatives exhibited a pronounced hemorheological and antiaggregant activity. Keeping in mind the lipophilic nature of the compounds, it can be assumed that these derivatives inhibit the development of blood hyperviscosity by interacting with the membrane lipid layer and stabilizing the erythrocyte cytoskeleton. Use of the studied compounds reduced the aggregation capability of thrombocytes, which is also a favorable component of the mechanism of action of the compounds on hemostasis. The combination of high activity and low toxicity may lead to the discovery of new highly effective drugs.
References
E. V. Roitman, Tromboz, Gemostaz, Reologiya, No.3, 13–27 (2003).
G. Crepaldi, A. Calabro, M. Belloni, et al., Ric. Clin. Lab., 13(3), 89–104 (1983).
E. V. Roitman, I. I. Dement?eva, O. A. Azizova, et al., Tromboz, Gemostaz, Reologiya, No. 1, 15–17 (2000).
J. Mo, J. Fan, Z. Guo, et al., Med. Hypotheses, 41(6), 516–520 (1993).
H. Watanabe, A. Kobayashi, T. Yamamoto, et al., Free Radical Biol. Med., 8(6), 507–514 (1990).
L. Iuliano, A. R. Colavita, R. Leo, et al., Free Radical Biol. Med., 22, 999–1006 (1997).
A. C. Cox, G. H. Rao, J. M. Gerrard, and J. G. White, Blood, 55, 907–914 (1980).
E. Agradi, A. Petroni, A. Socini, and C. Galli, Prostaglandins, 22, 255–266 (1981).
C. Cordova, A. Musca, F. Violi, et al., Atherosclerosis, 41, 15–19 (1982).
A. N. Zakirova, L. N. Minzhazetdinova, F. Kh. Kamilov, et al., Ter. Arkh., 66(9), 24–28 (1994).
G. Mojzisova and M. Kuchta, Physiol. Rev., 50, 529–535 (2001).
U. K. Senturk, O. Yalcin, F. Gunduz, et al., Appl. Physiol., 98, 1272–1279 (2005).
M. B. Plotnikov, G. A. Chernysheva, V. I. Smol?yakova, et al., Eksp. Klin. Farmakol., No. 1, 67–69 (2007).
H.-C. Cheng, C.-M. Chan, H.-S. Tsay, et al., Circ. J., 71, 597–603 (2007).
A. V. Kuchin, in: Abstracts of Papers of the VIth All-Russian Scientific Seminar “Chemistry and Medicine” [in Russian], Ufa (2007), p. 24.
E. V. Buravlev, I. Yu. Chukicheva, M. B. Plotnikov, and A. V. Kuchin, in: Abstracts of Papers of the VIth All-Russian Scientific Seminar “Chemistry and Medicine” [in Russian], Ufa (2007), p. 138.
M. B. Plotnikov, I. S. Ivanov, V. I. Smol?yakova, et al., in: Abstracts of Papers of the VIth All-Russian Scientific Seminar “Chemistry and Medicine” [in Russian], Ufa (2007), pp. 80 – 81.
I. Yu. Chukicheva and A. V. Kuchin, Ross. Khim. Zh., 48(3), 21–38 (2004).
E. S. Gabrielyan and S. E. Akopov, Blood Cells and Circulation [in Russian], Aiastan, Erevan (1985).
M. B. Plotnikov, O. I. Aliev, and F. V. Popel?, Klin. Lab. Diagn., No. 3, 457–458 (1995).
G. V. R. Born, Nature, 194(4832), 927–929 (1962).
B. D. Kavanagh, B. E. Coffey, D. Needham, et al., Br. J. Cancer, 67(4), 734–741 (1993).
V. I. Sorokovoi, N. N. Mochenova, and G. M. Nikitina, Byull. Eksp. Biol. Med., No. 5, 555–558 (1994).
A. G. Kriebardis, M. H. Antonelou, K. E. Stamoulis, et al., J. Cell. Mol. Med., 11(1), 148–155 (2007).
Author information
Authors and Affiliations
Additional information
Translated from Khimiko-Farmatsevticheskii Zhurnal, Vol. 44, No. 10, pp. 9 – 12, October, 2010.
Rights and permissions
About this article
Cite this article
Plotnikov, M.B., Smol’yakova, V.I., Ivanov, I.S. et al. Synthesis and biological activity of o-isobornylphenol derivatives. Pharm Chem J 44, 530–533 (2011). https://doi.org/10.1007/s11094-011-0511-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11094-011-0511-4