Abstract
The antimicrobial effects of the cold plasma for the dental pathogenic microorganism propose a promising approach to the Denture Stomatitis (DS) treatment. However, it is crucial to understand that the complexity of the biofilm microenvironment may compromise the efficiency of the therapy. As one of the major issue for DS, Candida albicans biofilms (ATCC10231) formed on denture base resins were treated by cold Ar/O2 (2 %) plasma jet. Spatial viability of the biofilms was investigated with confocal scanning laser microscopy through evaluating their inside cross-section properties. Results showed Candida albicans biofilms with thickness of ~100 µm was completely inactivated by 8 min plasma treatment. Morphology change of the fungi was also observed by the scanning electron microscopy. Drug susceptibilities, the sessile minimum inhibitory concentration (SMIC50) of the biofilm for amphotericin B and fluconazole were decreased from >32 and >256 µg/mL to 8 and 64 µg/mL after 1 min’s plasma treatment, respectively. The reactive species produced from plasma were monitored by optical emission spectroscopy. The successfully inactivation of Candida albicans biofilms and the significant enhancement of its drug susceptibilities induced by the plasma released reactive species propose a promising strategy for the treatment of DS caused by drug-resistant Candida albicans biofilms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Denture stomatitis (DS), an inflammatory process that may cause severe health damage, happens to 60 % of the denture wearers [1]. DS is highly associated with Candida in saliva and deficient denture hygiene. Accumulation of Candida albicans biofilms on dentures, mucous surface and acrylic resins may cause serious inflammation [2]. Although method has been proposed for DS such as physical cleaning, it is suffering from low efficiency and high failure rate. Pharmacotherapy including chlorhexidine, amphotericin B and fluconazole has also been introduced for DS treatment [3]. However, antifungal drug resistance is observed for the treatment of denture stomatitis in the denture wearers [4]. Thus, the urgent requirement for effective treatment of the Candida albicans biofilms is more than obvious.
During the last few years, cold plasma has attracted a great deal of attentions to the medical fields, attributing to its merits including room temperature, containing rich reactive oxygen species (ROS) and reactive nitrogen species (RNS) [5, 6]. Its dental applications, including oral microorganism inactivation [7–14], tooth whitening [15–19], dental material modification [20–22] and oral cancer treatment [23] have been reported. Its efficacy in inactivating microorganisms reminds us of its potential application in dealing with oral inflammatory process.
As polymethyl methacrylate (PMMA) is the most important raw material for denture base production, formation of the oral Candida albicans biofilms on the PMMA denture base resins is a critical issue for the patients especially those suffering from HIV, diabetes and cancers after chemotherapy and radiation [24]. Studies explore the surface modification effect of cold plasma on PMMA. Liebermann et al. [21] found the surface energy of PMMA had been improved after plasma treatment. Meanwhile, few reports have attempted to inactive Candida albicans related oral pathogen by cold plasma [25–27]. Hiromitsu Yamazaki et al. [26] foud the pH dependent inactivation effect of cold plasma on planktonic Candida albicans. Tim Maisch et al. [27] found that plasma at room temperature can lead to an 3 ~ 5 log10 reduction on 24-h Candida albicans biofilms formed on 6-well plates, which is comparable to 70 % ethanol treatment. Successful treatment of Candida albicans by cold He/O2 plasma has been demonstrated both in petri dish and liquid environment [25, 28]. However, it is crucial to understand the complexity of the biofilm microenvironment on PMMA may compromise the efficiency of the therapy [29]. The complexes of microenvironments provide a perfect shelter for the surviving of the biofilm. Until now, few studies focus on the oral Candida albicans biofilms formed on PMMA denture base resin and their drug susceptibility, which is believed analogous to the pathological condition of the DS.
In this study, we reported the treatment of the Candida albicans biofilms formed on the PMMA denture base resin and their drug susceptibility influenced by Ar/O2 cold plasma. Fungus viability, morphology changes as well as the drug susceptibility of the biofilm were investigated. Optical emission spectroscopy (OES) was employed to probe the reactive species produced by plasma. Possible mechanisms in terms of the biofilms inactivation and enhancement of the drug susceptibility were proposed.
Experimental Set Up and Methods
PMMA Denture Base Resin Preparation
PMMA denture base resin samples with diameter of 1.2 cm and thickness of 2 mm cylinder shape were prepared according to the manufacturer’s instructions (Vertex Rapid Simplified, Vertex-Dental BV, Zeist, Netherlands). The samples were randomly distributed into the following groups: control group without plasma treatment and treatment groups. The treatment groups were composed of 1, 2, 4, 6 and 8 min plasma treatment. Each of the treatment has three replicates. All samples were prepared with the sequence of sterile water, ultrasound, and warm water (60 °C) for three times, then dipped into a citrate buffer for 10 min and washed with deionized water for 5 times. Finally saliva coating for 90 min was applied [30].
Biofilms Formation
Single colony of Candida albicans strains (ATCC 10231) grown on SDA (1 % yeast extract, 2 % peptone, 2 % glucose, 2 % agar) plate was selected to 30 mL YPD (1 % yeast extract, 2 % peptone, and 2 % glucose) [31] overnight at 37 °C. Candida albicans cells which were most viable (in logarithmic growth phase) were collected and centrifuged at 3000g for 10 min, then the collection was diluted with phosphate buffer solution (PBS, pH = 7.4) to 1 × 107 colony formation unit (CFU)/mL. Suspension with volume of 1.5 mL was added to a pre-prepared PMMA denture base resin, which was placed in a sterile 24 well plate. The plate was then incubated at 37 °C for 90 min at 100 rpm agitation for initial adhesion of cells, and the un-adhered cells were removed through 2 mL of PBS washing. Finally the denture base resins were loaded to a new 24-well plate with 1.5 mL fresh YPD medium and incubated at 37 °C for 48 h at 100-rpm agitation in order to form a robust biofilms.
Plasma Treatment of Candida albicans Biofilms
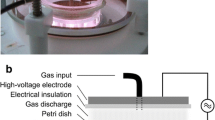
Geometry structure of the cold plasma device and treatment set up are presented in Fig. 1. The plasma was produced in a Teflon tube (Daxiang Inc, Beijing, China) with inner and outer diameters of 7 and 10 mm respectively. An outer copper foil with a thickness of 2 mm attached to the Teflon tube was served as the high potential electrode and placed at 5 cm above the end of the Teflon. The plasma was driven by a 10-kHz sinusoidal alternative voltage source with 18 kV (peak-to-peak). Argon (Ar) and oxygen (O2) mixture (Ar 98 %, O2 2 %) was used as working gas. Plume length was measured ~5 cm from end of the nozzle and injected into the atmospheric pressure air. The distance from the end of the nozzle to the sample was fixed at 1 cm, while the sample temperature was measured as 28 ± 3 °C during the treatment period. We have determined the optimum parameters with the treatment time fixed at 2 min (supplementary Fig. 1). Results showed that when the input current was fixed at 2.5 A, the 5 slm flow rate achieved the best inactivation rate. After that, we fixed the flow rate at 5 slm and found that the input current of 2.5 and 3 A achieved the best inactivation rate. Taking the stability of plasma into consideration, the input current of 2.5 A and flow rate of 5 slm was chosen for formal experiment. The PMMA denture base resin samples with 48 h biofilms were exposed to plasma at the durations of 1, 2, 4, 6 and 8 min. Emission spectrum from 200 to 850 nm was obtained by multi-channel fiber optic spectrometer (AvaSpec-2048-8-USB2, Avantes, Eerbeek, Netherlands) with a fiber optics cable placed along the nozzle axis with an end-on view. The spectral resolution was 0.1 nm. The system was controlled by Avaspec-USB2.0. After pre-test, the integral time is fixed to 600 ms to avoid saturation. The three repeated data was averaged and transferred to origin software before it was plotted. Representative species were assigned according to the database from National Institute of Standards and Technology. Detailed device geometry and operating parameters are illustrated in the work [8].
Analysis Procedure
CFU Analysis
The PMMA denture base resin samples with 48 h biofilms were exposed to plasma under different treatment times. After the treatment, fungal biofilms were collected according to the protocol described in the previous study [32]. 100 μL of the total 1 ml fungal solution was spread on agar plate before it was cultivated at 37 °C for 16 h and counted. The detection limit is 10 CFU/mL. Three samples from each treatment condition were repeated for statistical analysis.
Confocal Scanning Laser Microscopy (CSLM) Analysis
In order to evaluate the viability of the biofilms before and after plasma treatment, specimens were prepared for CSLM analysis. The biofilms after treatment were incubated with the reagents of the LIVE/DEAD Viability Kit (Invitrogen, Carlsbad, CA) for 15 min to stain according to manufacture instructions. The viability of the fungi can be distinguished by the stains. Live cells are stained green, while dead cells are stained red. An argon ion laser (λ = 488 and 543 nm) excitation source equipped with laser-scanning microscope (with an LSM 5 Exciter laser module; Zeiss, Oberkochen, Germany) was employed to analyze the results under a dry objective lens (×20). Images for CSLM were generated by software ZenLightEdition.
Scanning Electron Microscopic (SEM) Analysis
The sample from each treatment condition was chosen and fixed with 2.5 % glutaraldehyde for 24 h, and dehydrated with alcohol in the concentration orders of 10, 30, 50, 70, 90 and 100 %. Subsequently, the samples were cleaned with double distilled water and dried for 24 h before imaging. Finally, all the samples were mounted on aluminum stubs, sputtered with gold–palladium (30 mA, 60 s) and analyzed under SEM (Hitachi S-4800, Japan). Images were captured at different magnification (×2000, ×5000, and ×10,000).
Drug Susceptibility Test
Drug susceptibility test was adapted the protocol [33]. Biofilms from control group and plasma-treated group were collected and adjusted to the same starting cells concentration (107 cells/mL) before the drug susceptibility test. Fluconazole (FLU) (F4682, LKT, USA) and amphotericin B (AMB) (A2942, Sigma, USA) at the double-diluted concentrations (from 1024 to 1 μg/mL and to 0.125 μg/mL, respectively) were added to the biofilm samples and incubated for 24 h at 37 °C. Negative controls were set as empty wells and positive controls were set as wells without antifungals. The metabolic activities of the biofilms were analyzed by XTT assay: add 100 μl of the XTT/menadione solution to each well containing biofilm as well as to negative control wells (for the measurement of background XTT-colorimetric levels). Then the plates were incubated in the dark for 2–3 h at 37 °C. The results of optical density (OD) were measured from a SPECTROstar Omega absorbance plate reader with a Rapid UV/Vis spectrometer (BMG, Germany) at 490 nm. The sessile minimum inhibitory concentration (SMIC50), which is the lowest concentration of drug that reduces the OD of the biofilm by 50 %, was calculated. Each treatment was repeated for three times.
PMMA Surface Properties Evaluations
Surface morphology and peak-to-valley surface roughness of PMMA denture base resin was measured and tested by a 3D laser scanning confocal microscope (LSCM) (VK-X200; KEYENCE, Osaka, Japan). First, typical location was selected and pictures of surface were taken before and after treatment. Then the surface roughness average (Ra) of the specimen was determined in transverse length (0.8 mm). The travelling speed of probe is 0.5 mm/s. Ra is calculated by Eq. (1):
where Ra = the arithmetic average deviation from the mean line, L = the sampling length and y = the ordinate of the profile curve. Five sites of each sample were randomly selected, and the mean Ra values (μm) were calculated. There were three samples in each condition.
Statistical Analysis
Statistically significant differences were determined by analysis of two-tailed t test. Differences were considered statistically significant at P < 0.05. The values were expressed as mean ± standard error (s.e.).
Results
Plasma Components Analysis
As shown in Fig. 2a, plasma optical emissions were recorded between 250 and 850 nm. The spectrum is dominated by the Ar emission at 750 nm, O emissions at 777 and 844 nm, N2 emission at 337 nm, and OH radical. The OH radical (oxidation potential of 2.08 eV), atomic oxygen and reactive nitrogen species observed in the emission spectrum are believed to play an important role for the biofilms inactivation. Normalized intensity of four emissions from optical emission spectrum recorded between 250 and 800 nm was illustrated in Fig. 2b. Atomic oxygen (777 nm), OH radical, and reactive nitrogen species have been detected and the relative intensity of atom oxygen and reactive nitrogen species consist with the inactivation result in supplementary Fig. 1. So these species are believed to play an important role in the plasma sterilization process [34].
a Optical emission spectrum of Ar/O2 (2 %) plasma at gas flow rate of 5 standard liter per minute and input current of 2.5 A. Results were recorded from 200 to 850 nm, with dominant emissions Ar (750 nm), N2 (337 nm), O (777, 844 nm) and OH (A–X); b Normalized intensity of reactive species with current and gas flow rate change. Results were recorded from optical emission spectrum from 300 to 800 nm, including Ar (750 nm), N2 (337 nm), O (777 nm) and OH (308 nm) (Color figure online)
Plasma Inactivation Effect
The inactivation of Candida albicans biofilm by cold plasma was investigated through the CFU counting. Figure 3 illustrated a clear reduction of the biofilms by increasing the plasma treatment time. 2−log10 reduction was observed right after 1-min plasma treatment, and a significant difference was established compared with the gas control group. A steady increase of the reduction was also noticed as the time increased from 2 to 6 min. When the plasma exposure time increased to 8 min, the 6−log10 inactivation reduction was recorded. No detectable CFUs residual in the samples can be measured after 8 min treatment.
The inactivation effect of Ar/O2 plasma towards the Candida albicans biofilms formed on PMMA denture base resin. Candida albicans biofilms were treated with Ar/O2 plasma at 1, 2, 4, 6, and 8 min. Error bars indicate the mean standard errors between samples in same group. (asterisk means there is a significant difference compared with the Ar/O2(2 %) gas group (P < 0.01). The detection limit of CFU analysis in this study is 10 CFU/mL)
Spatial Viability of the Biofilms
Figure 4 3D illustrated the perspective view image of the thickness and 3D morphology of the biofilms formed on the denture tablet acquired under CSLM. After 48 h of incubation, the thickness of the biofilms formed on PMMA denture base resin reached ~100 μm (Fig. 4 3D). Most of the fungi in biofilms were inactivated after 8 min Ar/O2 plasma treatment, which was shown by the pronounced red area in Fig. 4 (3D-c, f). The biofilms in control group were shown in Fig. 4 (3D-a, d) while those treated by Ar/O2 gas were shown in Fig. 4 3D-b, e.
3D Morphology of the biofilms CSLM images on denture tablet with 3D images. a and d control, 0 min treatment; b and e treatment of Ar/O2 gas flow without plasma for 8 min; c and f treatment of Ar/O2 plasma for 8 min. 2D Single (the first and second images) and merged (the third image) CSLM images of 2D cross-section scan of the biofilms treated by plasma at a 0 (the control), b 1, c 2, d 4, e 6, and f 8 min. The white dash lines of merged images indicate the position where the cross-section scan is conducted. The cross-section layout has been presented by the right side (vertical scan) and bottom (horizontal scan) of each image with direction indicated by the white arrow as shown in (a). The alive biofilms are stained as green color while the dead are stained as red. (The scale bar is 100 μm) (Color figure online)
Due to the nature of the three dimensional structure of the biofilms, it is important to investigate the fungal viability inside the biofilms. Figure 4 2D illustrated the images of cross-section scans (single images as well as the merged image) of the Candida albicans biofilms before and after plasma (Ar/O2) treatment. Images acquired from the cross-section scans, at both vertical and horizontal directions indicated by the white dash line, were presented in the separated right and bottom side of each frame. As shown in Fig. 4 2D-a, biofilms in control group was stained in green, which suggests the fungi were alive. The progressive red areas became obvious when the treatment time increased from 1 to 8 min as shown in Fig. 4 2D-b–2D-f, which indicates fungi were dead. These results were well synchronized with the observation from the scans along the vertical and horizontal direction.
Morphology Observation
Figure 5 illustrated series of SEM photographs of the biofilms formed on PMMA denture base resin before and after plasma treatment under magnifications of ×2000, ×5000 and ×10,000. As shown in Fig. 5a–c, the control samples cell appeared as integral and round shape. The biofilm matrix and internal connections of the biofilms on denture base resin are observed (images not shown here). Meanwhile, ruptures of the cell membrane were observed after plasma treatment, indicated by the red arrows and red circles as shown in Fig. 5d–f. Cell shape was deformed after 8 min plasma treatment.
SEM photographs of the biofilms in the control groups (a)–(c), and plasma treatment group (d)–(f) under magnifications ×2000, ×5000 and ×10,000. Red arrows and circle indicate cell membrane damage. The integral cell and round shape were observed in the control group, while the ruptured and deformed cells were observed in the plasma treatment group (Color figure online)
Drug Susceptibility
Drugs susceptibility of the biofilms was investigated to study the plasma effect on the drug resistance of the biofilms. SMIC50 of Candida albicans biofilms for both AMB and FLU were illustrated in Table 1. The AMB and FLU SMIC50 of the biofilms decreased from >32 and >256 μg/mL to 8 and 64 μg/mL after 1 min plasma treatment. A smooth decrease was observed when the treatment time increased from 2 to 6 min, while the SMIC50 dropped to 1 and 16 μg/mL for AMB and FLU respectively after 8 min plasma exposure. The significant decrease of the SMIC50 suggested that the sensitivity of the biofilms to the antifungal drugs is dramatically increased after plasma treatment.
PMMA Surface Properties Evaluations
The surface properties are of great importance for denture base resin and studies have found that rough surfaces on denture-base materials promote the adhesion of Candida albicans in vitro [35] Thence, the plasma influence on denture base resin needs to be addressed before the further consideration of its possible applications. Ra, which is known as the arithmetic mean roughness value, is universally recognized parameter for evaluating the surface roughness. As shown in Fig. 6c, statistical analysis illustrated that no significant changes of surface roughness of PMMA denture base resin were observed after plasma treatment (P > 0.05), which consist with the study of Anja Liebermann [21]. Because a direct comparison of different profilometric techniques are hard to accomplish, to offer a better understanding of the surface change of denture base resin before and after treatment images of the denture surface acquired from 3D laser scanning confocal microscope were shown in Fig. 6a, b. No significant difference was observed. In order to perform the clinical applications, further investigation will be conducted in terms of detailed surface property changes with biofilms under different thickness.
Discussions
The antimicrobial effects of the cold plasma for the dental pathogenic microorganism propose a promising approach to the clinical DS treatment. Although a few studies have reported the successful treatment of dental microorganism in root canal cavity [8, 12], the fungi biofilms are still a big challenge in clinical therapy. In our previous study, successful treatment 10 strains of Candida biofilms (4 strains of Candida albicans, 3 strains of Candida glabrata, and 3 strains of Candida krusei) in vitro were demonstrated within 1 min’s treatment [25, 28]. However, it is important to realize the complex of the environment can compromise the efficiency of the therapy [29]. For here, Candida albicans (ATCC 10231) biofilm cultivated on denture base resin was employed to study the plasma inactivation effect as one step forward when complex environment is involved to mimic the clinical realistic. Bearing this idea in mind, the 48-h Candida albicans biofilms developed on PMMA denture base resin was employed to analogue the Candida albicans related DS. The inactivation of Candida albicans by cold plasma was investigated through the CFU counting. Figure 3 illustrated a clear reduction of the Candida albicans by increasing the plasma treatment time. When the plasma exposure time increased to 8 min, no detectable CFUs residual in the samples can be measured. And the log10 reduction value for 8 min was above six, which satisfies the requirement of the US Food and Drug Administration for sterility assurance level of implantable medical devices [36].
CSLM results illustrated the perspective view image of the thickness and 3D morphology of the biofilm formed on the denture tablet. When observing the color, we found that inactivation of the ~100 μm biofilm was achieved after 8 min plasma treatment, while only 1 min was required when the biofilm was grown in the 96-well plate [25]. The differences between the inactivation efficiency indicate the compromise of the therapy because the denture base resin provides a shelter for the biofilm against the environment pressure [37, 38].
When investigating the fungal viability inside the biofilms, we deduce that the 2-log reduction after 1 min plasma treatment is believed due to the inactivation of several spots of biofilms [39]. Because the CSLM images present the results scanned through 2 μm thickness of the biofilm. The dead cells (red spot) in Fig. 4 2D-b present the cell viability only on the top layer, which can be convinced through observing the cross-section scans shown on the images at right and bottom sides. It can be observed the bottom layer of the biofilm is mostly stained green before 6 min. Meanwhile, a dominated red color was observed in Fig. 4 2D-f, which indicates the biofilms were nearly inactivated. The corresponding cross-section scans also confirmed these results, indicating that cold plasma could achieve the inactivation of biofilms from points to entire surface. Compared with previous report, a significant improvement is noticed while only 15 µm inactivation were observed [40].
SEM results showed that ruptures of the cell membrane were observed after plasma treatment, indicated by the red arrows and red circles as shown in Fig. 5d–f. Cell shape was deformed after 8 min plasma treatment, which may cause lethal damage to cell survival.
Drugs susceptibility of the biofilm was investigated to study the plasma effect on the drug resistance of the biofilm. SMIC50 of Candida albicans biofilm for both AMB and FLU were illustrated in Table 1. The significant decrease of the SMIC50 suggested that the sensitivity of the biofilm to the antifungal drugs is dramatically increased after plasma treatment. Drug resistance is another main issue for the failure treatment of DS [4, 41]. The drug susceptibility of Candida albicans biofilms prepared on PMMA denture base resin to both AMB and FLU increased 90 % after only 8 min plasma treatment, while increment of 10 % of the susceptibility to antifungal drugs has been recognized as a breakthrough [42], which prompts the superiority of cold plasma treatment for the Candida albicans biofilms formed on denture base resin. According to the widely accepted pharmacological reports, AMB and FLU are interfering ergosterol on cell membrane and cytochrome P450 in cells [43], respectively. Kobayashi et al. [44] found that the reactive oxygen species production is important to the antifungal activity of miconazole, which shares the same pharmacophore with FLU. Wink et al. [45] also verified the inhibition of cytochromes P450 by nitric oxide and a nitric-oxide-releasing agent. Atomic oxygen, OH radical, and strong excited nitrogen emissions detected in the plasma (Fig. 2a) are believed to play an important role to the inactivation process [46, 47], which is attributed to activate oxidative stress pathway and change of the cell cycle pathway [34]. The reaction can be simulated by Fig. 7, where ROS and RNS were generated by plasma and penetrate the membrane of Candida albicans biofilms. After that, ROS and RNS can destruct ergosterol on cell membrane and cytochrome P450 in cells. As a result, the drug susceptibility was increased. However, the in vivo study is required to support its identity as a promising strategy for biofilms caused DS treatment.
Conclusions
In summary, Candida albicans biofilms formed on PMMA denture base resin with thickness of 100 µm are investigated by CSLM. Excellent inactivation is confirmed with both CFU counting and fluorescence viability test after 8 min cold Ar/O2 (2 %) plasma treatment, while no significant influences on PMMA surface roughness is observed. The oxidative stress induced by plasma is believed to play an important role for the cell rupture. Moreover, biofilms susceptibility of AMB and FLU has been increased an order of magnitude after plasma treatment, which reveals a promising strategy for the treatment of DS caused by drug-resistant Candida albicans biofilms. However, further study will be carried out to investigate the biofilms in vivo experiment before clinical applications.
References
Bc W, Cj T, Md W, Dw H, Kw K (1998) Aust Dent J 43:160
Emami E, Kabawat M, Rompre PH, Feine JS (2014) J Dent 42:99
Duyck J, Vandamme K, Muller P, Teughels W (2013) J Dent 41:1281
Bueno M, Urban V, Barbério G, Silva WD, Porto V, Pinto L, Neppelenbroek K (2013) Oral Dis 21:57
von Woedtke T, Reuter S, Masur K, Weltmann KD (2013) Phys Rep 530:291
Graves DB (2012) J Phys D Appl Phys 45:263001
Duarte S, Kuo SP, Murata RM, Chen CY, Saxena D, Huang KJ, Popovic S (2011) Phys Plasmas 18:073503
Pan J, Sun K, Liang YD, Sun P, Yang XH, Wang J, Zhang J, Zhu WD, Fang J, Becker KH (2013) J Endodont 39:105
Wang R, Zhou H, Sun P, Wu H, Pan J, Zhu W, Zhang J, Fang J (2011) Plasma Med 1:143
Yang B, Chen JR, Yu QS, Li H, Lin MS, Mustapha A, Hong LA, Wang Y (2011) J Dent 39:48
Du T, Shi Q, Shen Y, Cao Y, Ma J, Lu X, Xiong Z, Haapasalo M (2013) J Endodont 39:1438
Jiang C, Chen MT, Gorur A, Schaudinn C, Jaramillo DE, Costerton JW, Sedghizadeh PP, Vernier PT, Gundersen MA (2009) Plasma Process Polym 6:479
Koban I, Holtfreter B, Hübner NO, Matthes R, Sietmann R, Kindel E, Weltmann KD, Welk A, Kramer A, Kocher T (2011) J Clin Periodontol 38:956
Koban I, Matthes R, Hübner N-O, Welk A, Meisel P, Holtfreter B, Sietmann R, Kindel E, Weltmann K-D, Kramer A (2010) New J Phys 12:073039
Sun P, Pan J, Tian Y, Bai N, Wu H, Wang L, Yu C, Zhang J, Zhu W, Becker KH (2010) IEEE T Plasma Sci 38:1892
Pan J, Sun P, Tian Y, Zhou H, Wu H, Bai N, Liu F, Zhu W, Zhang J, Becker KH (2010) IEEE T Plasma Sci 38:3143
Pan J, Yang XH, Sun K, Wang J, Sun P, Wu HY, Becker KH, Zhu WD, Zhang J, Fang J (2013) IEEE T Plasma Sci 41:325
Wang J, Yang XH, Sun K, Sun P, Pan J, Zhu WD, Becker KH, Zhang J, Fang J (2012) IEEE T Plasma Sci 40:2157
Lee HW, Nam SH, Mohamed AAH, Kim GC, Lee JK (2010) Plasma Process Polym 7:274
Valverde GB, Coelho PG, Janal MN, Lorenzoni FC, Carvalho RM, Thompson VP, Weltemann KD, Silva NRFA (2013) J Dent 41:51
Liebermann A, Keul C, Bahr N, Edelhoff D, Eichberger M, Roos M, Stawarczyk B (2013) Dent Mater 29:935
Dong XQ, Ritts AC, Staller C, Yu QS, Chen M, Wang Y (2013) Eur J Oral Sci 121:355
Kim G, Park S, Kim G, Lee JKJ (2011) Plasma Med 1:45
Bulacio L, Paz M, Ramadan S, Ramos L, Pairoba C, Sortino M, Escovich L, Lopez C (2012) J Mycol Med 22:348
Sun Y, Yu S, Sun P, Wu H, Zhu W, Liu W, Zhang J, Fang J, Li R (2012) PLoS ONE 7:40629
Yamazaki H, Ohshima T, Tsubota Y, Yamaguchi H, Jayawardena JA, Nishimura Y (2011) Dent Mater J 30:384
Maisch T, Shimizu T, Isbary G, Heinlin J, Karrer S, Klämpfl TG, Li Y-F, Morfill G, Zimmermann JL (2012) Appl Environ Microbiol 78:4242
Sun P, Sun Y, Wu HY, Zhu WD, Lopez JL, Liu W, Zhang J, Li RY, Fang J (2011) Appl Phys Lett 98:021501
Rautemaa R, Ramage G (2011) Crit Rev Microbiol 37:328
Lazarin AA, Machado AL, Zamperini CA, Wady AF, Spolidorio DMP, Vergani CE (2013) Arch Oral Biol 58:1
Ramage G, Vandewalle K, Wickes BL, Lopez-Ribot JL (2001) Rev Iberoam Micol 18:163
Jin Y, Samaranayake LP, Samaranayake Y, Yip HK (2004) Arch Oral Biol 49:789
Pierce CG, Uppuluri P, Tristan AR, Wormley FL, Jr Mowat E, Ramage G, Lopez-Ribot JL (2008) Nat Protoc 3:1494
Feng H, Wang R, Sun P, Wu H, Liu Q, Fang J, Zhu W, Li F, Zhang J (2010) Appl Phys Lett 97:131501
Radford D, Sweet S, Challacombe S, Walter J (1998) J Dent 26:577
Reich MS, Akkus O (2013) Cell Tissue Bank 14:381
Chandra J, Kuhn DM, Mukherjee PK, Hoyer LL, McCormick T, Ghannoum MA (2001) J Bacteriol 183:5385
Al-Fattani MA, Douglas LJ (2006) J Med Microbiol 55:999
Bayliss DL, Walsh JL, Iza F, Shama G, Holah J, Kong MG (2012) Plasma Process Polym 9:597
Xiong Z, Du T, Lu X, Cao Y, Pan Y (2011) Appl Phys Lett 98:221503
Sanglard D, Odds FC (2002) Lancet Infect Dis 2:507
Fothergill AW, Sutton DA, McCarthy DI, Wiederhold NP (2014) J Clin Microbiol 52:994
Kunze KL, Wienkers LC, Thummel KE, Trager WF (1996) Drug Metab Dispos 24:414
Kobayashi D, Kondo K, Uehara N, Otokozawa S, Tsuji N, Yagihashi A, Watanabe N (2002) Antimicrob Agents Ch 46:3113
Wink DA, Osawa Y, Darbyshire JF, Jones CR, Eshenaur SC, Nims RW (1993) Arch Biochem Biophys 300:115
Duday D, Clement F, Lecoq E, Penny C, Audinot JN, Belmonte T, Kutasi K, Cauchie HM, Choquet P (2013) Plasma Process Polym 10:864
Wu HY, Sun P, Feng HQ, Zhou HX, Wang RX, Liang YD, Lu JF, Zhu WD, Zhang J, Fang J (2012) Plasma Process Polym 9:417
Acknowledgments
This research was supported by Natural Science Foundation No. 81200821 (China) and Bioelectrics. Inc (USA).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, G.M., Sun, P.P., Pan, H. et al. Inactivation of Candida albicans Biofilms on Polymethyl Methacrylate and Enhancement of the Drug Susceptibility by Cold Ar/O2 Plasma Jet. Plasma Chem Plasma Process 36, 383–396 (2016). https://doi.org/10.1007/s11090-015-9656-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11090-015-9656-3