Abstract
To investigate late toxicity among patients with newly-diagnosed brain metastases undergoing stereotactic radiosurgery (SRS) with concurrent systemic therapies with or without whole-brain radiation therapy (WBRT). Patients with newly-diagnosed brain metastasis who underwent SRS at a single tertiary-care institution from 1997 to 2015 were eligible for inclusion. The class and timing of all systemic therapies were collected for each patient. The primary outcome was the cumulative incidence of radiographic radiation necrosis (RN). Multivariable competing risks regression was used to adjust for confounding. During the study period, 1650 patients presented with 2843 intracranial metastases. Among these, 445 patients (27%) were treated with SRS and concurrent systemic therapy. Radiographic RN developed following treatment of 222 (8%) lesions, 120 (54%) of which were symptomatic. The 12-month cumulative incidences of RN among lesions treated with and without concurrent therapies were 6.6 and 5.3%, respectively (p = 0.14). Concurrent systemic therapy was associated with a significantly increased rate of RN among lesions treated with upfront SRS and WBRT (8.7 vs. 3.7%, p = 0.04). In particular, concurrent targeted therapies significantly increased the 12-month cumulative incidence of RN (8.8 vs. 5.3%, p < 0.01). Among these therapies, significantly increased rates of RN were observed with VEGFR tyrosine kinase inhibitors (TKIs) (14.3 vs. 6.6%, p = 0.04) and EGFR TKIs (15.6 vs. 6.0%, p = 0.04). Most classes of systemic therapies may be safely delivered concurrently with SRS in the management of newly-diagnosed brain metastases. However, the rate of radiographic RN is significantly increased with the addition of concurrent systemic therapies to SRS and WBRT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Brain metastases are the leading cause of cancer-related neurological morbidity in the United States, affecting 15–30% of cancer patients [1, 2]. Local therapies include resection, stereotactic radiosurgery (SRS), whole-brain radiation therapy (WBRT), or a combination of these modalities. However, the potential for increased toxicity when combining local and systemic therapies remains poorly understood.
SRS is a treatment option that offers high rates of local control [3]. However, radiation necrosis (RN) is the primary dose-limiting toxicity following SRS, occurring following 5–10% of treatments [4,5,6]. RN is symptomatic in 50% of cases, and may worsen neurologic deficits and necessitate prolonged treatment with steroids or anti-angiogenic agents. Recently reported data have suggested that systemic therapies may be safely delivered with SRS, but given the rarity of RN, these studies have been underpowered to detect which specific agents may increase the rate of RN [7]. To our knowledge, no studies have investigated whether the addition of upfront WBRT to SRS with modern concurrent systemic therapies increases the risk of RN.
In the present study, we sought to define the relationship between RN and the timing of SRS in relation to cytotoxic chemotherapy, hormone therapy, targeted therapies, and immunotherapy. We hypothesized the following: (1) the rate of radiographic RN is not significantly increased with the addition of concurrent systemic therapies to SRS alone; (2) the rate of RN is significantly increased with the addition of concurrent systemic therapies to SRS + WBRT; (3) the rates of RN are increased only with the use of specific targeted agents.
Methods and materials
Patient selection and data collection
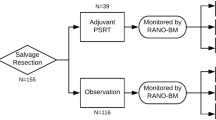
We conducted an IRB-approved retrospective cohort study including all patients with newly-diagnosed brain metastasis between 1997 and 2015 who underwent SRS with or without WBRT or resection at a single tertiary-care institution. Patients treated with surgery and/or WBRT alone were excluded, as were patients without radiographic follow-up.
The following data were collected in an IRB-approved registry: age, gender, primary pathology, Karnofsky performance status (KPS), survival, number of brain metastases, presence of extracranial metastases, graded prognostic assessment (GPA) [8], overall survival, lesion laterality, location, maximum diameter, volume, prescription dose, maximum dose, conformality index, heterogeneity index, gradient index [9], and timing of systemic therapies, SRS, WBRT, and surgical resection.
Systemic therapies
All cytotoxic, hormone, cytokine (interleukins, interferons), and targeted systemic therapies were collected for each patient. Cytotoxic agents were divided into the following classes: alkylating agents, nucleoside analogs, folate analogs, intercalating agents, platinum-containing agents, taxanes, topoisomerase inhibitors, and vinca alkaloids. Targeted therapies were divided into the following classes: VEGF antibodies, VEGFR tyrosine kinase inhibitors (TKIs), HER2 antibodies (trastuzumab and pertuzumab), EGFR TKIs (including lapatinib, a dual HER2/EGFR TKI), ALK TKIs, BRAF inhibitors, mTOR inhibitors, and PD-1/CTLA-4 inhibitors. Concurrent systemic therapy was defined as an agent administered on the same day as SRS, or within five biological half-lives of the date of SRS (corresponding to ~97% metabolism or elimination). Each agent’s biological half-life was recorded from the adult Lexi-Drug® database [10]. Systemic therapies that were stopped more than five biological half-lives before SRS, or initiated more than five biological half-lives after SRS were not considered concurrent therapies.
Stereotactic radiosurgery delivery and clinical follow-up
SRS was delivered with a 201- or 192-source Gamma Knife system (models B, C, 4C, and Perfexion, Elekta Instruments AB, Stockholm, Sweden). For planning, the dose prescribed to the peripheral margin was typically chosen based on lesion size according to RTOG 90-05 [11]. Patients were seen in clinic with repeat MRIs 4–6 weeks after SRS, and were subsequently followed every 3 months.
Outcome measures
The primary outcome was the cumulative incidence of radiographic RN, calculated from the date of SRS. RN was defined on the basis of pathologic and/or radiographic evidence. In general, ring-enhancing lesions demonstrating enlargement with surrounding edema were suspicious for RN [12, 13]. Short-interval follow-up imaging was performed to distinguish progressive disease from RN using an institutional algorithm [12]. For equivocal cases, a multidisciplinary brain tumor board met to achieve a clinical consensus. If a consensus was not reached, patients typically underwent positron emission tomography (PET), MRI with cerebral blood volume, short interval imaging follow-up, or biopsy/resection to differentiate tumor recurrence from RN. The secondary outcome was overall survival, calculated from the date of first brain metastasis.
Statistical analysis
For baseline characteristics, continuous data were compared across cohorts with Student’s t-tests or Wilcoxon rank-sum tests, while categorical data were compared with Fisher’s exact or Chi-squared tests. The Kaplan–Meier method was used to estimate overall survival. Differences in survival were compared using log-rank tests. Cumulative incidences were used to estimate the time-dependent risk of RN for each lesion [14]. Non-informative censoring was performed only at loss to radiographic follow-up. Death was a second competing cause. To test for differences in cumulative incidences across cohorts, Gray’s tests were utilized [14, 15].
Multivariable analysis for overall survival was conducted on a per-patient basis using Cox proportional hazards modeling. Multivariable analysis for RN was conducted on a per-lesion basis using the competing risk model described by Fine and Gray [16]. Models were adjusted for the following covariates, with death as a competing risk: use of concurrent systemic therapy, age, gender, presence of extracranial metastases, number of brain metastases, KPS, primary pathology, prior/concurrent WBRT, prior surgery, lesion location, maximum diameter, prescription dose, conformality index, heterogeneity index, and gradient index. Covariates were chosen based upon previously-identified risk factors for RN, variables prognostic for survival, and systemic therapies to test the research hypothesis. Covariates demonstrating association (p ≤ 0.10) with survival or RN on univariate analysis were evaluated in a multivariable model including all two-way interactions. Analyses were conducted using R and the cmprsk statistical software package [17, 18]. Two-sided tests with p < 0.05 were considered statistically significant.
Results
Patient characteristics
In this study, 1650 patients presented with 2843 intracranial metastases and met inclusion criteria. Excluded patients from the registry were 2246 patients with brain metastasis who did not undergo SRS within the study period, 289 patients who underwent SRS only in the salvage setting, and 182 patients who did not undergo follow-up imaging after upfront SRS. Among the 1650 included patients, 445 (27%) were treated with a concurrent systemic therapy at the time of upfront SRS (Table 1).
Systemic therapies
Among these 445 patients, 218 (49%) received concurrent targeted therapies, 179 (40%) received concurrent hormone therapies, 126 (28%) received concurrent cytotoxic therapies, and 7 (2%) received concurrent cytokine therapies. The most commonly utilized targeted and cytotoxic agents were HER2 antibodies (69 patients, 16%), VEGFR TKIs (60 patients, 13%), nucleoside analogs (46 patients, 10%), and taxanes (36 patients, 8%).
Overall survival
Unadjusted median survival was significantly greater among patients receiving concurrent therapy (12.4 vs. 10.5 months, p = 0.01, Table 2). However, this did not remain significant after multivariable analysis (Table 3, HR 0.90, 95% CI 0.78–1.03, p = 0.11).
In the subsets of patients treated with upfront WBRT (12.4 vs. 10.3 months, p = 0.07) and without upfront WBRT (12.4 vs. 10.7, p = 0.13), median survival was not significantly greater with the use of concurrent therapy. However, among patients with breast cancers, median survival was extended with concurrent therapy (18.2 vs. 13.8 months, p < 0.01). Concurrent therapy was not associated with extended median survival in other pathologies, including molecular subtypes of NSCLC and melanoma.
Lesion characteristics and radiation necrosis
Among the 2843 metastases treated with SRS, 854 (30%) were treated with concurrent systemic therapies (Table 4). On a per-lesion basis, the most commonly utilized cytotoxic and targeted therapies were VEGFR TKIs (119 lesions, 14%), HER2 antibodies (111 lesions, 13%), VEGF antibodies (89 lesions, 10%), and nucleoside analogs (88 lesions, 10%).
Radiographic RN developed following treatment of 222 (8%) lesions. Among these 222 lesions, 120 (54%) were symptomatic. Confirmatory diagnosis was most commonly established with serial MRI and tumor board review (45%), cerebral blood volume MRI (35%), positron emission tomography (14%), and pathology (6%). The 12-month cumulative incidences of RN among lesions treated with and without concurrent therapies were 6.6 and 5.3%, respectively (Table 2, p = 0.14). Concurrent therapy was associated with a significantly increased rate of RN among lesions treated with upfront WBRT (8.7 vs. 3.7%, p = 0.04, Fig. 1a). The hazard rate for RN among patients receiving concurrent systemic therapies was greatest in the 4.5–9 months after SRS; thereafter, few events were observed. In contrast, among lesions treated with primary SRS (without upfront WBRT), concurrent systemic therapy was not associated with an increased rate of RN (5.7 vs. 6.3%, p = 0.61, Fig. 1b).
Concurrent cytokine therapies (0.0 vs. 5.3%, p = 0.41), cytotoxic therapies (2.7 vs. 5.3%, p = 0.07), and hormone therapy (6.5 vs. 5.3%, p = 0.20) were not associated with significantly greater 12-month cumulative incidences of RN. Moreover, no individual classes of cytotoxic therapies were associated with elevated rates of RN (Fig. 2). In contrast, concurrent targeted therapies significantly increased the 12-month cumulative incidence of RN (8.8 vs. 5.3%, p < 0.01). Among these therapies, statistically significantly increased rates of RN were observed with the use of VEGFR TKIs (13.0 vs. 5.3%, p = 0.04), HER2 antibodies (9.0 vs. 5.3%, p = 0.01), and EGFR TKIs (14.0 vs. 5.3%, p = 0.01).
Forest plot of unadjusted hazard ratios for radiation necrosis with 95% confidence intervals. *Denotes number of lesions treated with each class of concurrent therapy. Circle size is proportional to number of lesions. Bolded text indicates 95% confidence intervals that do not cross 1.00. TKI tyrosine kinase inhibitor
To control for confounding by pathology, subset analyses were performed in the renal, HER2-amplified breast, and lung adenocarcinoma populations. Among renal metastases, concurrent VEGFR TKIs were associated with a significantly increased 12-month cumulative incidence of RN (14.3 vs. 6.6%, p = 0.04) (Fig. 3a). This effect appeared consistent both with (21.4 vs. 0.0%, p = 0.03) and without (13.1 vs. 8.3%, p = 0.11) concurrent WBRT. Among HER2-amplified metastases, concurrent HER2 antibodies (9.0 vs. 7.7%, p = 0.83) and lapatinib (12.5 vs. 7.7%, p = 0.24) were not associated with significantly increased 12-month cumulative incidences of RN. Finally, among lung adenocarcinoma metastases, concurrent EGFR TKIs were associated with an increased 12-month cumulative incidence of RN (15.6 vs. 6.0%, p = 0.04, Fig. 3b). This effect was most apparent among patients undergoing concurrent WBRT (20.0 vs. 3.3%, p = 0.02) compared to patients undergoing SRS alone (10.3 vs. 7.9%, p = 0.45).
Following multivariable competing risks regression, concurrent systemic therapies trended toward association with RN (HR 1.49, 95% CI 0.91–2.02, p = 0.08, Table 3). To confirm the unadjusted results, identical multivariable models were constructed among lesions treated with or without upfront WBRT. In the subset of lesions treated with upfront WBRT, concurrent systemic therapies significantly increased the rate of RN (HR 2.01, 95% CI 1.19–3.38, p < 0.01). In contrast, the rate of RN was not significantly increased with the use of concurrent systemic therapies among the subset of lesions treated without upfront WBRT (HR 1.29, 95% CI 0.88–1.89, p = 0.20). Prognosticators such as KPS and extracranial disease were highly associated with RN.
Discussion
To our knowledge, we report the largest and most comprehensive evaluation of late toxicity following SRS with or without WBRT among patients receiving concurrent systemic therapies. In support of our hypotheses, we observed that concurrent systemic therapies significantly increase the rate of radiographic RN when delivered with SRS and WBRT, but concurrent systemic therapies did not significantly increase the rate of RN among patients receiving SRS alone.
The present study builds upon a single-institution retrospective cohort study of toxicity following SRS with or without concurrent (week of SRS treatment) systemic therapies [7]. Among 291 SRS treatments, 174 received SRS alone, while 108 received SRS with concurrent systemic therapy. No significant differences in RN between the two cohorts were observed (6 vs. 4%, p = 0.55). However, this report was limited by small sample size (only 14 RN events), exclusion of patients undergoing SRS with WBRT, and lack of time-dependent, competing risk, or per-lesion analyses.
Cytotoxic chemotherapy
Among the 2843 metastases treated in this study, we observed no significant difference in the 12-month cumulative incidence of RN between lesions treated with or without concurrent systemic therapy (6.6 vs. 5.3%, p = 0.14). We performed subset analyses for each class of systemic therapy and observed no evidence of increased toxicity with concurrent cytotoxic therapies. Our findings are supported by Colaco et al., who reported the incidence of RN among 180 patients undergoing SRS with systemic therapies; in this report, the crude odds of RN was lower among patients receiving chemotherapy (OR 0.38, p = 0.06). However, the authors utilized logistic rather than time-dependent competing risks regression [19]. A separate investigation comprising 118 RN events reported that capecitabine delivered within 1 month of SRS was associated with an increased risk of symptomatic RN [5], though this finding was not replicated in our series. A possible explanation for this is that the authors did not perform subset analyses among individual pathologies (specifically breast cancers). However, the present investigation included only 88 lesions treated with concurrent nucleoside analogs. As more patients receive capecitabine, its safety profile when delivered around the time of SRS will require further study.
Targeted therapies
We observed a significantly increased rate of RN among patients treated with concurrent targeted therapies, driven primarily by VEGFR and EGFR TKIs. In a recently-published series of nearly 2000 patients undergoing SRS, renal histology, lung adenocarcinoma histology, HER2 amplification, and ALK/BRAF mutational status were associated with RN [4]. The mechanism for this effect may relate to the increased efficacy of radiation therapy when delivered with VEGFR and EGFR TKIs [20]. VEGFR TKIs alter both tumor angiogenesis and cell proliferation, simultaneously reducing vascularization of metastases while inducing cell apoptosis. These agents are associated with a variety of adverse effects, as VEGFR TKIs also act upon a variety of receptor tyrosine kinases expressed on normal tissue. It is possible that tyrosine kinase inhibition on either normal or metastatic tissue is responsible for the increase rate of RN. Preclinical data have suggested that VEGFR TKIs create a vascular normalization window, thereby increasing radiosensitivity [21]. This hypothesis has been supported by clinical data showing significantly greater rates of serious bowel injury in a series of 76 patients treated with stereotactic body radiation therapy with or without VEGFR TKIs, perhaps secondary to interruption of sublethal damage repair [22]. In contrast, overexpression of EGFR in metastatic tissue results in uncontrolled cell division; EGFR-directed TKIs induce cell apoptosis by blocking the EGFR signaling cascade. It is plausible that repair of radiation-induced sublethal damage is possible in the presence of normal EGFR signaling, but the combination of SRS and EGFR inhibition lead to tissue necrosis. Supporting this, Chiang et al. reported significantly increased rates of radiation-recall pneumonitis among patients with NSCLC who received EGFR TKIs within 90 days of thoracic radiotherapy [23]. Given that the half-lives of most VEGFR/EGFR TKIs are less than 2 days, it would not be unreasonable to hold these agents for 2–3 half lives before and after SRS.
Several previous reports have suggested increased rates of RN with select targeted therapies. Patel et al. reported that BRAF inhibitors increase the rate of RN following SRS [24]. Multiple separate studies have failed to replicate these results, and current consensus guidelines recommend holding BRAF inhibitor therapy for 1 day before and after SRS [4, 25].
Whole-brain radiation therapy
We observed that concurrent systemic therapies more than doubled the cumulative incidence of RN among patients receiving SRS and WBRT (8.7 vs. 3.7%). Moreover, we also noted that peak period for radiation necrosis in this population occurred in the 5–9 month interval from treatment. SRS therefore provides a unique advantage over WBRT, as most patients with brain metastasis die from extracranial disease. Moreover, recovery from SRS is remarkably shorter—patients do not typically experience the acute side effects associated with WBRT. Finally, although patients treated with SRS may require salvage treatments for intracranial relapse, previous studies have demonstrated that retreatments have a modest treatment-related toxicity, do not negatively affect a patient’s performance status, and may maintain a patient’s quality of life [26, 27].
Randomized data have demonstrated that the addition of systemic therapy to WBRT increases both extracranial and CNS toxicity [28,29,30]. In a phase III trial, patients with NSCLC brain metastases were randomized to SRS + WBRT with or without temozolomide or erlotinib [31]. The results suggest that the addition of systemic therapy to radiation therapy increases CNS toxicity and mortality. The frequency of grade ≥3 toxicity was significantly greater for patients treated with concurrent systemic therapies (45 vs. 11%, p < 0.01). These findings are supported by the present investigation, in which a significantly increased rate of RN was observed only with the addition of upfront WBRT to SRS with concurrent systemic therapies. Moreover, in the present study, EGFR TKIs in the lung adenocarcinoma population were implicated as agents responsible for this effect.
Strengths and limitations
As a single institutional retrospective study, several limitations must be considered when interpreting these results. To minimize the possibility of misdiagnosis of RN, our institution utilizes a comprehensive semiweekly tumor board, serial MR imaging, and advanced imaging modalities when surgical intervention is not warranted to establish a diagnosis. Although prospective data would offer greater internal validity, the rarity of RN necessitates large retrospective investigations to detect risk factors that could be prospectively validated. Dose to normal tissue, a previously-identified risk factor for RN, was not collected in this investigation; however, the conformality index served as a dimensionless index for normal tissue dose, and was included in all models. Moreover, it is possible that the dose to normal tissue is higher among clustered lesions, which was not quantified in this study.
To address selection bias and confounding, a consecutive patient sample treated in the upfront setting was studied, and several candidate predictors were included in competing risks models. Critically, our results demonstrate that the addition of upfront WBRT to SRS with concurrent systemic therapies increases CNS toxicity. These results are therefore potentially practice-changing, supporting assertions that WBRT should be omitted in the upfront setting among patients initiating systemic therapy. Future investigations might seek to compare the rate of RN in a cohort of patients undergoing WBRT alone, as well as a cohort of patients previously-treated with targeted therapies.
Conclusions
We observed low rates of radiographic RN among patients treated with SRS and concurrent cytotoxic chemotherapy, hormone therapy, and cytokine therapy. In support of our hypothesis, the rate of RN was only significantly increased with the addition of concurrent systemic therapies to SRS and WBRT. No corresponding increase in RN was observed among patients treated with concurrent therapies and SRS alone. These data support a growing body of evidence favoring the omission of upfront WBRT to spare neurocognition and late neurotoxicity.
References
Chang EL, Wefel JS, Hess KR et al (2009) Neurocognition in patients with brain metastases treated with radiosurgery or radiosurgery plus whole-brain irradiation: a randomised controlled trial. Lancet Oncol 10(11):1037–1044
Nayak L, Lee EQ, Wen PY (2011) Epidemiology of brain metastases. Curr Oncol Rep 14(1):48–54
Suh JH (2010) Stereotactic radiosurgery for the management of brain metastases. N Engl J Med 362(12):1119–1127
Miller JA, Bennett EE, Xiao R et al (2016) Association between radiation necrosis and tumor biology following stereotactic radiosurgery for brain metastasis. Int J Radiat Oncol Biol Phys 96(5):1060–1069
Sneed PK, Mendez J, Vemer-van den Hoek JGM et al (2015) Adverse radiation effect after stereotactic radiosurgery for brain metastases: incidence, time course, and risk factors. J Neurosurg 123(2):373–386
Mohammadi AM, Schroeder JL, Angelov L et al (2016) Impact of radiosurgery prescription dose on the local control of small (≤2 cm) brain metastases. J Neurosurg 27:1–9
Shen CJ, Kummerlowe MN, Redmond KJ et al (2016) Stereotactic radiosurgery: treatment of brain metastasis without interruption of systemic therapy. Int J Radiat Oncol Biol Phys 95(2):735–742
Sperduto PW, Berkey B, Gaspar LE et al (2008) A new prognostic index and comparison to three other indices for patients with brain metastases: an analysis of 1,960 patients in the RTOG database. Int J Radiat Oncol Biol Phys 70(2):510–514
Balagamwala EH, Suh JH, Barnett GH et al (2012) The importance of the conformality, heterogeneity, and gradient indices in evaluating Gamma Knife radiosurgery treatment plans for intracranial meningiomas. Int J Radiat Oncol Biol Phys 83(5):1406–1413
Lexicomp Online®, Adult Lexi-Drugs®, Hudson, Ohio: Lexi-Comp, Inc.; January 29, 2015
Shaw E, Scott C, Souhami L et al (2000) Single dose radiosurgical treatment of recurrent previously irradiated primary brain tumors and brain metastases: final report of RTOG protocol 90-05. Int J Radiat Oncol Biol Phys 47(2):291–298
Chao ST, Ahluwalia MS, Barnett GH et al (2013) Challenges with the diagnosis and treatment of cerebral radiation necrosis. Int J Radiat Oncol Biol Phys 87(3):449–457
Stockham AL, Tievsky AL, Koyfman SA et al (2012) Conventional MRI does not reliably distinguish radiation necrosis from tumor recurrence after stereotactic radiosurgery. J Neurooncol 109(1):149–158
Gray RJ (1988) A class of K-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 16(3):1141–1154
Dignam JJ, Kocherginsky MN (2008) Choice and interpretation of statistical tests used when competing risks are present. J Clin Oncol 26(24):4027–4034
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94(446):496–509
R Core Team (2015) R statistical software package
Gray B (2014) R cmprsk package: subdistribution analysis of competing risks. R package version 2.2-7
Colaco RJ, Martin P, Kluger HM, Yu JB, Chiang VL (2016) Does immunotherapy increase the rate of radiation necrosis after radiosurgical treatment of brain metastases? J Neurosurg 125(1):17–23
Miller JA, Balagamwala EH, Angelov L et al (2016) Spine stereotactic radiosurgery with concurrent tyrosine kinase inhibitors for metastatic renal cell carcinoma. J Neurosurg Spine 25:766–774
Hsu H-W, Wall NR, Hsueh C-T et al (2014) Combination antiangiogenic therapy and radiation in head and neck cancers. Oral Oncol 50(1):19–26
Barney BM, Markovic SN, Laack NN et al (2013) Increased bowel toxicity in patients treated with a vascular endothelial growth factor inhibitor (VEGFI) after stereotactic body radiation therapy (SBRT). Int J Radiat Oncol Biol Phys 87(1):73–80
Chiang C-L, Chen Y-W, Wu M-H, Huang H-C, Tsai C-M, Chiu C-H (2016) Radiation recall pneumonitis induced by epidermal growth factor receptor-tyrosine kinase inhibitor in patients with advanced nonsmall-cell lung cancer. J Chin Med Assoc 79(5):248–255
Patel KR, Chowdhary M, Switchenko JM et al (2016) BRAF inhibitor and stereotactic radiosurgery is associated with an increased risk of radiation necrosis. Melanoma Res 26(4):387–394
Gaudy-Marqueste C, Carron R, Delsanti C et al (2014) On demand Gamma-Knife strategy can be safely combined with BRAF inhibitors for the treatment of melanoma brain metastases. Ann Oncol 25(10):2086–2091
Kotecha R, Damico N, Miller JA et al (2016) Three or more courses of stereotactic radiosurgery for patients with multiply recurrent brain metastases. Neurosurgery. doi:10.1093/neuros/nyw147
Miller JA, Kotecha R, Barnett GH et al (2016) Quality of life following stereotactic radiosurgery for single and multiple brain metastases. Neurosurgery. doi:10.1093/neuros/nyw166
Kleinberg L, Grossman SA, Piantadosi S et al (1999) The effects of sequential versus concurrent chemotherapy and radiotherapy on survival and toxicity in patients with newly diagnosed high-grade astrocytoma. Int J Radiat Oncol Biol Phys 44(3):535–543
Cao KI, Lebas N, Gerber S et al (2015) Phase II randomized study of whole-brain radiation therapy with or without concurrent temozolomide for brain metastases from breast cancer. Ann Oncol 26(1):89–94
Soussain C, Ricard D, Fike JR et al (2009) CNS complications of radiotherapy and chemotherapy. Lancet 374(9701):1639–1651
Sperduto PW, Wang M, Robins HI et al (2013) A phase 3 trial of whole brain radiation therapy and stereotactic radiosurgery alone versus WBRT and SRS with temozolomide or erlotinib for non-small cell lung cancer and 1 to 3 brain metastases: Radiation Therapy Oncology Group 0320. Int J Radiat Oncol Biol Phys 85(5):1312–1318
Author contributions
JMK: Conceptualization, formal analysis, methodology, visualization, writing—original draft, writing—review and editing. JAM: Conceptualization, formal analysis, methodology, visualization, writing—review and editing. RK and STC: Conceptualization, writing—review and editing. RX, AJ, MCW, MSA, AMM, DMP, ESM, JHS, GHB, MAV, LA and GHS: Investigation, writing—review and editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J.M. Kim, J.A. Miller, R. Xiao, A. Juloori, M.C. Ward, A.M. Mohammadi, D.M. Peereboom, E.S. Murphy, L. Angelov and G.H. Stevens have declare that they have no conflict of interest. R. Kotecha: Honorarium and research support from Varian Medical Systems. M.S. Ahluwalia: Consulting and grant from Elekta; Grant support from Boehringer Ingelheim, Bristol-Myers Squibb, Novartis, Spectrum Pharmaceuticals, Tracon Pharmaceuticals, Novocure; Consultant for Merck, Genentech/ Roche, Incyte, Caris Lifesciences, Monteris Medical, MRI interventions Inc. J.H. Suh: Travel, Elekta; Honorarium and Research Support, Varian Medical Systems. G.H. Barnett: Consultant for Monteris Medical, Inc.; Royalty interests for Mako Surgical Corp, Roche. M.A. Vogelbaum: Equity and royalty interests, company founder and officer for Infuseon Therapeutics, Inc; Honorarium for scientific advisory meeting from Pharmicokinesis, Inc.; Honorarium for DSMB membership from Neuralstem, Inc. S.T. Chao: Honorarium, Varian Medical Systems.
Rights and permissions
About this article
Cite this article
Kim, J.M., Miller, J.A., Kotecha, R. et al. The risk of radiation necrosis following stereotactic radiosurgery with concurrent systemic therapies. J Neurooncol 133, 357–368 (2017). https://doi.org/10.1007/s11060-017-2442-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-017-2442-8