Abstract
Invasion into surrounding normal brain and resistance to genotoxic therapies are the main devastating aspects of glioblastoma (GBM). These biological features may be associated with the stem cell phenotype, which can be induced through a dedifferentiation process known as epithelial-mesenchymal transition (EMT). We show here that tumor cells around pseudopalisading necrotic areas in human GBM tissues highly express the most important EMT inducer, transforming growth factor (TGF-β), concurrently with the EMT-related transcriptional factor, TWIST. In addition, the stem cell markers CD133 and alkaline phosphatase (ALPL) were also highly expressed around necrotic foci in GBM tissues. The high expression of TGF-β around necrotic regions was significantly correlated with shorter progression-free survival and overall survival in patients with GBM. High expression of stem cell markers, ALPL, CD133, and CD44 was also correlated with poor outcomes. These results collectively support the hypothesis that tissue hypoxia induces the stem cell phenotype through TGF-β-related EMT and contributes to the poor outcome of GBM patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gliomas are classified according to histopathological features that distinguish three cellular lineages, astrocytic, oligodendrocytic, and ependymal, and four malignancy grades, grades I to IV according to the criteria established by the World Health Organization (WHO) [1]. The most malignant form of gliomas, grade IV glioblastoma (GBM), is supposed to originate from oligodendrocyte precursor cells [2]. The most devastating and refractory aspects of GBM are the highly invasive nature that prevents curative tumor resection and the resistance to apoptosis-inducing therapies. Individual tumors with the same morphology likely have different refractory features that are responsible for the markedly heterogeneous survival periods [3]. According to The Cancer Genome Atlas sub-classification of GBM, the mesenchymal subtype frequently expresses neural stem cell markers and is associated with an aggressive phenotype [4–6]. Non-mesenchymal subtypes usually acquire the gene expression pattern of the mesenchymal subtype at recurrence after chemotherapy and radiotherapy [6], indicating that phenotypic transition may depend on environmental signals.
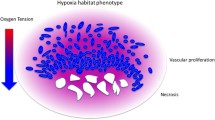
A prominent characteristic of the GBM microenvironment is hypoxia, which is caused by abnormal structure, function, and distribution of neo-angiogenesis and aberrant induction of the intravascular coagulation cascade [7, 8]. A hypoxic microenvironment is generally regarded as a potent inducer of epithelial-mesenchymal transition (EMT) which induces polarized epithelial cells to undergo multiple epigenetic changes that result in dedifferentiation of cells and acquisition of stem cell features [11–15]. The EMT is mainly mediated by transforming growth factor-β (TGF-β) among many other signaling pathways [9, 10]. TGF-β family members also play an important role in the maintenance of pluripotent stem cells and cancer stem cells [16]. In addition, a hypoxic microenvironment in tumor tissues leads to recruitment of circulating or residential myeloid cells, such as macrophages or microglia, into the tumor stroma [16, 17]. These cells release high levels of TGF-β, which triggers upregulation of transcription factors necessary for EMT such as TWIST or Snail and further progression of EMT [16–21]. Indeed, the phenotypic transition to the mesenchymal subtype of GBM may be directly induced by TGF-β [22].
We hypothesize that hypoxia induces stem cell properties in GBM cells through TGF-β-mediated EMT, which contributes to treatment resistance and poor outcomes. Such a correlation has not been demonstrated in human GBM tissues. To address this issue, we performed an integrated histological and molecular analysis of EMT-related factors such as TGF-β and TWIST, and we analyzed the expression of stem cell markers in relation to necrotic areas in GBM tissues.
Materials and methods
Patients and tissue specimens
We performed a retrospective study of 80 patients with GBM. All tissue samples were obtained from patients treated at the Chiba University Hospital at the time of the patient’s first surgery. Two independent neuropathologists confirmed the histopathological diagnoses of all specimens according to the criteria established by WHO in 2007. All patients with GBM were treated with 60 Gy local-field irradiation and concurrent temozolomide. The chemotherapy protocol was administered according to Stupp’s regimen, and the maintenance chemotherapy was continued for a median of 1.5 years. Written informed consent was obtained from each patient. Brain magnetic resonance images of all patients were obtained with and without gadolinium enhancement to assess the infiltrative or disseminated areas during the survival period.
Immunohistochemical analysis
For immunohistochemical analyses of gliomas, paraffin-embedded samples were sectioned at a thickness of 6 μm and mounted on microscopic slides. The primary antibodies used in this study were: anti-TGF-β1 antibody (1:200, R&D Systems, Minneapolis, MN), anti-alkaline phosphatase (ALPL) antibody (1:100, Abcam, Inc. Cambridge, UK), anti-CD133 antibody (1:20, Miltenyi Biotec, Germany), anti-CD44 antibody (1:100, Novocastra Laboratories, Ltd., Newcastle, UK), anti-TWIST antibody (1:100, Abcam), anti-IDH1-R132H antibody (1:100, MBL Co., Ltd, Nagoya, Japan), and anti-O6-methylguanine-DNA methyltransferase (MGMT) monoclonal antibody MT3.1 (1:200, Chemicon, Inc., Temecula, CA, USA). Heat-induced epitope retrieval was performed by microwaving the sections in 10 mM EDTA buffer, pH of 7.2. The samples were incubated overnight with the antibodies in the same buffer, followed by incubation with biotinylated secondary antibody (1:500, DAKO, Tokyo, Japan). The bound antibodies were visualized with the avidin–biotin-peroxidase complex method and diaminobenzidine tetrachloride (Santa Cruz Biotechnology, Santa Cruz, CA). Sections were counterstained with hematoxylin. A positive staining result was considered a tumor in which >10 % of cells had cytoplasmic, membranous or nuclear staining.
Histological analysis related to pseudopalisading necrosis
The pseudopalisading necrosis is shown to represent a hypoxic areas [23]. For immunohistochemical analysis, the positive rates were calculated as the percent of cells positive for the marker. We selected two representative areas both in the pseudopalisading necrotic areas and non-necrotic areas, and calculated the positive rate separately. When the positive rate in the necrotic area was 10 % or more, the case was judged as “necrotic positive” irrespective of the positive rate of non-necrotic areas. When the positive rate in the necrotic area was below 10 % and that in the non-necrotic area was 10 % or more, the case was judged as “non-necrotic positive”. Therefore, some necrotic positive cases may have a higher positive rate of the non-necrotic area than that of the necrotic area.
Statistical analysis
The survival periods of patients with GBM were calculated. Progression-free survival (PFS) was calculated from the date of initial surgery until the first sign of radiological progression, death, or last follow-up. Overall survival (OS) was also calculated from the date of initial surgery until the date of death or last follow-up. The Kaplan–Meier method was used to estimate the survival rates, and the Cox-Mantel log-rank test was applied to compare the survival differences among the patients. Analyses were performed using StatView software (SAS Institute Inc., Cary, NC). Multivariate analysis was performed with the commercially available software using the Cox proportional hazards regression model (SPSS, Inc., Chicago, IL).
Results
Clinical course of the GBM patients
Eighty patients with histologically confirmed, newly diagnosed GBM from 2007 to 2014 were included in this study. Characteristics of the patients are summarized in Table 1, and are similar to those of previous reports. Patients were equally distributed between older and younger than 60 years of age and by sex. Karnofsky performance status (KPS) score below 70 was observed in 45 patients (56 %). Total resection was accomplished in 34 patients (43 %). MGMT protein expression that was judged to be 10 % or more was observed in 34 of the 75 cases with tissue available (45 %). IDH1 status was also determined with immunohistochemical analysis using anti-IDH1R132H antibody, which showed that five cases (6 %) were positive for the IDH1-mutant protein. The median PFS was 16 months, and the median OS was 22 months. Marked heterogeneity in OS was observed among the patients, with an OS of over 5 years in nine patients and less than 1 year in 18 patients.
TGF-β
Necrotic areas, which are considered to be hypoxic, were observed in all cases. Only pseudopalisading necrosis was considered for evaluation of the cellular response to hypoxia in this study. All the results of immunohistochemical analyses are summarized in Table 2. The result showed positive TGF-β expression in 71 % of the patients (53 among 75 patients examined). The necrotic-positive frequency was 27 % (20 of 75 cases) and the frequency of non-necrotic positive was 44 % (33 of 75 cases) (Fig. 1a). The mean positive rate for TGF-β in the necrotic-positive cases was 34.3 ± 19.2 %, whereas that of the non-necrotic regions was 18.6 ± 8.3 % (p = 0.0027, unpaired t test) (Fig. 1b). This result indicates that TGF-β expression is higher in hypoxic areas than in non-hypoxic areas in some GBM patients.
Transforming growth factor-β (TGF-β) immunohistochemistry. a Representative results of a necrotic positive case in which positive cells are clustered around a necrotic area (a), and a non-necrotic positive case in which positive cells are mainly located in an area distant from necrosis (b). b Bar graph comparing the positive rates of TGF-β expression between necrotic and non-necrotic areas (p = 0.040)
TWIST
TWIST is a strong inducer of EMT, which is directly correlated with stem cell properties. Immunohistochemical analysis showed that 47 % of the patients had tumors that were positive for TWIST (35 of 75 patients examined). Similar to TGF-β, the positive rate of TWIST tended to be higher in necrotic areas than in non-necrotic areas (24.1 ± 5.5 % vs. 10.6 ± 5.5 %) without statistical significance (p = 0.1234, unpaired t-test). This is likely in part because the number of positive cases was small compared with the number of cases that expressed TGF-β. Expression of TWIST was a significant factor for short PFS (p = 0.0273) but not for OS.
Relationship between stem cell markers and necrosis
Because necrotic areas in GBM tissues were enriched with TGF-β and TWIST, we also analyzed the expression of stem cell markers. The stem cell markers CD133, CD44, and the pluripotent stem cell marker ALPL were examined. ALPL is highly expressed in the embryonic inner cellular mass and is traditionally used as a pluripotent stem cell marker [15–18]. Immunohistochemical analysis showed that CD133 was positive in 52 % of the patients (33 of 64 patients examined) (Fig. 2a). The positive rate of CD133 was significantly higher in necrotic areas than in non-necrotic areas (36.9 ± 16.3 % vs. 22.0 ± 11.4 %) (p = 0.0047, unpaired t-test) (Fig. 2b). ALPL was positive in 55 % of the patients (35 of 64 patients examined). The positive rate was also significantly higher in necrotic areas than in non-necrotic areas (34.1 ± 15.1 % vs. 21.3 ± 9.5 %) (p = 0.0106, unpaired t-test) (Fig. 2b). In contrast, CD44 was expressed in all GBM tissues examined, and the immunostaining pattern was categorized as moderate (n = 36, 51 %) or intense (n = 34, 49 %). However, the staining pattern was not correlated with necrotic areas.
Patient survival according to TGF-β expression in necrotic areas
Patients with high TGF-β expression tended to have shorter survival than those without TGF-β expression, but the difference was not statistically significant (p = 0.1211). TWIST expression was also not significantly associated with patient survival (data not shown). We next compared the patient survival among three classes of TGF-β expression related to necrotic areas: negative (both necrotic and non-necrotic areas showed staining of 10 % or less), non-necrotic positive (only non-necrotic areas were positive), or necrotic positive (necrotic areas were positive). Twenty-two cases were negative, 33 cases were non-necrotic positive, and 20 cases were necrotic positive. The patients who were necrotic positive showed significantly shorter survival than those who were non-necrotic positive or with negative TGF-β expression (p = 0.0028 for PFS and p = 0.0134 for OS, necrotic positive vs others, log-rank test) (Fig. 3). Expressions of ALPL, CD133, and CD44 each was a poor prognostic factor for survival irrespective of expression patterns related to necrosis. ALPL was significant both for OS and PFS (p = 0.0102 and p = 0.0447, respectively) and CD133 was significant only for OS (p = 0.0207). The intense CD44 immunostaining was a significant factor both for a shorter PFS and a shorter OS (p = 0.0089 and p = 0.0119, respectively).
Multivariate analysis of survival
To confirm the prognostic value of expression levels of stem cell markers, we performed multivariate analysis of survival of 64 patients who had full immunohistochemical data among 80 GBM patients included in this study (Table 3). Known prognostic factors such as age (≥60 years), KPS (<70), extent of surgical resection (non-total resection), and MGMT protein expression were also included in the analysis. The stem cell markers ALPL and CD133 were also included. An age of ≥60 years and KPS of <70 did not significantly affect the survival period. Non-total resection was an independent factor for poor prognosis both in PFS and OS (HR 3.376, p = 0.0290 and HR 3.276, p = 0.0275, respectively). Among the molecular factors, only ALPL was a significant factor for OS but not for PFS (HR 2.967, p = 0.0384 and HR 2.734, p = 0.0725, respectively). No other molecular factors were significant in the multivariate analyses including high TGF-β expression around necrosis.
Discussion
We show in this report that high expression of TGF-β, TWIST, and stem cell markers is more frequently observed around necrotic areas than non-necrotic areas in human GBM tissues. Patients with positive immunostaining of TGF-β tended to have shorter survival than those without positive TGF-β staining without a statistical significance [24]. This tendency has been confirmed in the patients with necrotic positive of TGF-β who survived significantly shorter than those without the TGF-β expression pattern. TGF-β is frequently positive in GBM (71 % in this study) as a result of various signal transduction pathways [24]. Only high expression of TGF-β around hypoxic areas may be correlated with poor survival, which is mainly caused by the acquisition of stem cell properties through EMT. The negative result in multivariate analysis would be due to a low statistical power of the small patient cohort. These results collectively suggest that a hypoxic microenvironment is correlated with EMT induction through TGF-β expression and that the resulting stem cell phenotype in GBM tissues may be a main cause of treatment resistance and poor outcomes.
Hypoxia is observed not only during the natural course of glioma progression but also in response to treatment of the glioma including radiation therapy and a targeted therapy such as bevacizumab. These therapeutic modalities are toxic to the vascular endothelial cells and shrink the vascular system, leading to further hypoxia in the tumor tissues. Glioma cells that have survived irradiation possess gene expression patterns that are enriched in EMT-inducing molecules, which endows a radioresistance to the tumor cells [25, 26]. DNA damage responses in GBM cells promote migration and invasion of the tumor cells through EMT with enhanced expression of TGF-β, hypoxia-inducible factor-1α, vascular endothelial growth factor (VEGF), epidermal growth factor, or hepatocyte growth factor [27–32]. Recently, Mahabir et al. showed that the radiation-related induction of EMT in malignant gliomas is accelerated by TGF-β derived from mesenchymal cells in the tumor microenvironment [32]. Although hypoxia is a main inducer of the TGF-β-related EMT, a direct correlation of hypoxia and TGF-β has been scarcely evidenced in human GBM. The present data support the hypothesis that TGF-β induced by hypoxia plays a crucial role in the possible acquisition of invasive phenotype following radiation therapy.
Treatment with bevacizumab, which targets VEGF, initially restores abnormal distribution and high permeability of vasculature via a process called the normalization phase [33]. With prolonged treatment with bevacizumab beyond the vascular normalization phase, the tumor develops progressive hypoxia [33]. Hypoxia is an important environmental stimulus that directly or indirectly promotes the stem cell phenotype [34–37]. First, hypoxia induces DNA hypomethylation, which is the epigenetic background of stem cells [38, 39]. Second, hypoxia induces glioma cells to release hypoxia inducible factor-1α and VEGF, which attract myeloid cells from bone marrow into glioma tissues [16, 17]. The recruited myeloid cells release multiple growth factors such as interleukin-6, interleukin-10, and matrix metalloproteinases, as well as TGF-β [16, 17, 40]. TGF-β also recruits mesenchymal stem cells into the glioma tissues, which contributes to further malignant progression of GBM [9, 21, 41]. This vicious hypoxia-related cycle may be a reason that bevacizumab is not effective in prolonging OS in newly diagnosed GBM patients.
The clinical picture of glioma is quite heterogeneous, even in the same histological category and grade. Such a phenotypic diversity in glioma tissues is partly due to various microenvironmental factors as well as intrinsic genetic alterations. We found that the essential EMT-inducing factors TGF-β and TWIST are highly expressed around necrotic areas in relation to high expressions of stem cell markers. Anti-VEGF therapy such as bevacizumab may be candidates for modulating the glioma hypoxic microenvironment to enhance the efficacy of radiotherapy and to obtain a better outcome for GBM patients.
References
Aldape K, Zadeh G, von Deimling A et al (2015) Glioblastoma: pathology, molecular mechanisms and markers. Acta Neuropathol 129:829–848
Liu C, Sage JC, Miller MR et al (2011) Mosaic analysis with double markers reveals tumor cell of origin in glioma. Cell 146:209–221
Iwadate Y, Sakaida T, Hiwasa T et al (2004) Molecular classification and survival prediction in human gliomas based on proteome analysis. Cancer Res 64:2496–2501
Phillips HS, Kharbanda S, Chen R et al (2006) Molecular subclasses of high-grade glioma predict prognosis, delineate a pattern of disease progression, and resemble stages in neurogenesis. Cancer Cell 9:157–173
Verhaak RGW, Hoadley KA, Purdom E, Wang V, Qi Y et al (2010) Integrated genomic analysis identifies clinically relevant subtypes of glioblastoma characterized by abnormalities in PDGFRA, IDH1, EGFR, and NF1. Cancer Cell 17:98–110
Zarkoob H, Taube JH, Singh SK, Mani SA, Kohandel M (2013) Investigating the link between molecular subtype of glioblastoma, epithelial- mesenchymal transition, and CD133 cell surface protein. PLoS One 8:e64169
Heddleston JM, Li Z, McLendon RE, Hjelmeland AB, Rich JN (2009) The hypoxic microenvironment maintains glioblastoma stem cells and promotes reprogramming towards a cancer stem cell phenotype. Cell Cycle 8:3274–3284
Cooper LAD, Gutman DA, Chisolm C et al (2012) The tumor microenvironment strongly impacts master transcriptional regulators and gene expression class of glioblastoma. Am J Path. 180:2108–2118
Charles NA, Holland EC, Gilbertson R et al (2011) The brain tumor microenvironment. Glia. 59:1169–1180
Jensen RL (2009) Brain tumor hypoxia: tumorigenesis, angiogenesis, imaging, pseudoprogression, and as a therapeutic target. J Neurooncol 92:317–335
Mani SA, Guo W, Liao M-J et al (2008) The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell 133:704–715
Bao S, Wu Q, McLendon RE et al (2006) Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature 444:756–760
Bhat KPL, Balasubramaniyan V, Vaillant B, Ezhilarasan R, Hummelink K et al (2013) Mesenchymal differentiation mediated by NF-kB promotes radiation resistance in glioblastoma. Cancer Cell 24:331–346
Zhang X, Zhang W, Mao XG, Zhen HN, Cao WD, Hu SJ (2013) Targeting role of glioma stem cells for glioblastoma multiforme. Curr Med Chem 20:1974–1984
Murat A, Migliavacca E, Gorlia T, Lambiv WL, Shay T et al (2008) Stem cell-related “self-renewal” signature and high epidermal growth factor receptor expression associated with resistance to concomitant chemoradiotherapy in glioblastoma. J Clin Oncol 26:3015–3024
Ye X-Z, Xu S-L, Xin Y-H et al (2012) Tumor-associated microglia/macrophages enhance the invasion of glioma stem-like cells via TGF-β1 signaling pathway. J Immunol 189:444–453
Piao Y, Liang J, Holmes L et al (2012) Glioblastoma resistance to anti-VEGF therapy is associated with myeloid cell infiltration, stem cell accumulation, and a mesenchymal phenotype. Neuro-Oncology 14:1379–1392
Kalluri R, Weinberg RA (2009) The basics of epithelial-mesenchymal transition. J Clin Invest 119:1420–1428
Zeisberg M, Neilson EG (2009) Biomarkers for epithelial-mesenchymal transitions. J Clin Invest 119:1429–1437
Mikheeva SA, Mikheev AM, Petit A et al (2010) Twist1 promotes invasion through mesenchymal change in human glioblastoma. Mol Cancer. 9:194
Shinojima N, Hossain A, Takezaki T et al (2012) TGF-β mediated homing of bone marrow-derived human mesenchymal stem cells to glioma stem cells. Cancer Res 73:2333–2344
Kahlert UD, Nikkhah G, Maciaczyk J (2013) Epithelial-to-mesenchymal (-like) transition as a relevant molecular event in malignant gliomas. Cancer Let. 33:131–138
Rong Y, Durden DL, Van Meir EG et al (2006) ‘Pseudopalisading’ necrosis in glioblastoma: a familiar morphologic feature that links vascular pathology, hypoxia, and angiogenesis. J Neuropath Exp Neurol 65:529–539
Bruna A, Darken RS, Rojo F et al (2007) High TGFβ-Smad activity confers poor prognosis in glioma patients and promotes cell proliferation depending on the methylation of the PDGF-B gene. Cnacer Cell 11:147–160
Theys J, Jutten B, Habets R et al (2011) E-cadherin loss associated with EMT promotes radioresistance in human tumor cells. Radioth Oncol 99:392–397
Meng J, Li P, Zhang Q et al (2014) A radiosensitivity gene signature in predicting glioma prognostic via EMT pathway. Oncotarget 5:4683–4693
Hardee ME, Marciscano AE, Medina-Ramirez CM et al (2012) Resistance of glioblastoma-initiating cells to radiation mediated by the tumor microenvironment can be abolished by inhibiting transforming growth factor-β. Cancer Res 72:4119–4129
Kim Y-H, Yoo K-C, Cui Y-H et al (2014) Radiation promotes malignant progression of glioma cells through HIF-1alpha stabilization. Cancer Lett 354:132–141
Zhou YC, Liu JY, Li J et al (2011) Ionizing radiation promotes migration and invasion of cancer cells through transforming growth factor-beta-mediated epithelial- mesenchymal transition. Int J Radiat Oncol Biol Phys 81:1530–1537
Zhang M, Kleber S, Rohrich M et al (2011) Blockade of TGF-beta signaling by the TGFbetaR-1 kinase inhibitor LY2109761 enhances radiation response and prolongs survival in glioblastoma. Cancer Res 71:7155–7167
Timke C, Zieher H, Roth A et al (2008) Combination of vascular endothelial growth factor receptor/platelet-derived growth factor receptor inhibition markedly improve radiation tumor therapy. Clin Cancer Res 14:2210–2219
Mahabir R, Tanino M, Elmansuri A et al (2014) Sustained elevation of Snail promotes glial-mesenchymal transition after irradiation in malignant glioma. Neuro-Oncology 16:671–685
Jain RK (2005) Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science 307:58–62
Bar EE, Lin A, Mahairaki V, Matsui W, Eberhart CG (2010) Hypoxia increases the expression of stem-cell markers and promotes clonogenicity in glioblastoma neurospheres. Am J Pathol 177:1491–1502
Evans SM, Judy KD, Dunphy I et al (2004) Hypoxia is important in the biology and aggression of human glial brain tumors. Clin Cancer Res 10:8177–8184
Li Z, Bao S, Wu Q et al (2009) Hypoxia-inducible factors regulate tumorigenic capacity of glioma stem cells. Cancer Cell 15:501–513
Kaur B, Khwaja FW, Severson EA et al (2005) Hypoxia and hypoxia-inducible-factor pathway in glioma growth and angiogenesis. Neuro Oncol 7:134–153
Shahrzad S, Bertrand K, Minhas K, Coomber BL (2007) Induction of DNA hypomethylation by tumor hypoxia. Epigenetics 2:119–129
Skowronki K, Andrews J, Rodenhiser DI, Coomber BL (2014) Genome-wide analysis in human colorectal cancer cells reveals ischemia-mediated expression of motility genes via DNA hypomethylation. PlosOne 9: e103243
Schonberg DL, Lubelski D, Miller TE, Rich JN (2014) Brain tumor stem cells: molecular characteristics and their impact on therapy. Mol Aspects Med 39:82–101
Bechnan J, Isakson P, Joel M et al (2014) Recruited brain tumor-derived mesenchymal stem cells contribute to brain tumor progression. Stem Cells 32:1110–1123
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iwadate, Y., Matsutani, T., Hirono, S. et al. Transforming growth factor-β and stem cell markers are highly expressed around necrotic areas in glioblastoma. J Neurooncol 129, 101–107 (2016). https://doi.org/10.1007/s11060-016-2145-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-016-2145-6