Abstract
Patients with glioma frequently suffer from deficits of neurocognitive functioning (NCF), though few studies have assessed NCF in localized glioma patients prior to surgery. One hundred and three patients (M age = 52.0; M education = 14.6 years) with histologically confirmed glioma in the right (RTL: n = 30; 57 % glioblastoma) or left temporal lobe (LTL: n = 73; 49 % glioblastoma) completed presurgical neuropsychological assessment. Impairment of NCF was identified in 75 % of all patients. Notably, patients with RTL glioma were most frequently impaired on measures of verbal memory and executive functioning, and at similar rates as the LTL group. Nonetheless, χ2 tests revealed that impairment rates were significantly higher in the LTL group on attention and object naming tests (p ≤ .05). Independent-samples t-tests revealed that mean performances of patients with LTL glioma were also significantly below RTL patients on measures of attention (p = .01), verbal learning and memory (p = .05), and language (p < .03). A trend was observed in which anterior LTL tumors were associated with reduced verbal learning and medial LTL lesions with delayed recall problems, though patients with lesions involving multiple LTL regions exhibited the greatest difficulty across all verbal memory measures. Significant group differences in NCF performances remained so after controlling for FLAIR volume and tumor histology. These findings indicate that temporal lobe glioma frequently present with impaired NCF, though impairments are often milder in RTL compared to LTL patients. Nonetheless, the relatively frequent verbal memory impairment in the RTL group underscores the bilaterality of verbal memory processes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Monitoring neurocognitive functioning (NCF) is increasingly recognized as essential for optimal clinical care and as important endpoints in clinical trials for patients with glioma [1, 2]. Despite increasing research devoted to understanding relationships between glioma and NCF, the existing literature tends to involve small sample sizes, poor regional specificity of tumor site, and evaluation of NCF is usually performed only after surgery or initiation of adjuvant therapies [3–5]. In light of these limitations, clinicians and researchers often look to studies of other focal neurological populations for insights into the potential relationships between tumor location and NCF at time of initial presentation.
Some of the most widely studied brain-behavior relationships across neurologic populations pertain to material-specific lateralization. Studies examining the lateralization of temporal lobe functions frequently utilize temporal lobe stroke [6–8] and epilepsy [9–12] populations, given the relatively localized pathology in these patient groups. A convergence of research with these groups points to some generalities relating structure, pathology, and NCF. Broadly, the left temporal lobe (LTL) is associated with verbal memory and other language functions, while the right temporal lobe (RTL) is primarily linked to visuospatial memory and nonverbal abilities, assuming left hemisphere language dominance [8].
While it is true that verbal and visual functions are differentially impacted by LTL versus RTL pathology, considerable evidence suggests that the temporal lobes do not process material in a dichotomous, material-specific manner [13–15]. Functional neuroimaging data indicate that bilateral temporal lobe structures are activated during verbal memory tasks, though exact processes differ between hemispheres [16]. Similarly, a recent study suggests that problems with allocentric navigation may occur in patients with right or left temporal lobe epilepsy [13], further questioning the notion of strict lateralization of temporal lobe functions.
Despite the prima facie similarities between populations, inferences regarding NCF drawn from studies of epilepsy and stroke patients may be inaccurate when extended to brain tumor populations. Brain tumor patients tend to exhibit a more subtle and diffuse pattern of neurocognitive dysfunction compared to stroke populations, even in cases with similar regional involvement [6]. This is likely attributable, at least in part, to the differing pathophysiological processes involved with the lesions. That is, the dysfunction caused by stroke depends largely on the direct destruction of neurons, while most tumors begin by displacing neuronal tissues without actually causing immediate damage. Further, in addition to lesion size and location, relationships between NCF and glioma can be impacted by various treatment effects. The present study aims to minimize any such confounding factors and clarify the relationships between NCF and lateralized temporal lobe glioma prior to initiation of treatment.
Methods
Participants
Treatment-naïve adults with glioma restricted to the LTL or RTL were identified in The University of Texas MD Anderson Cancer Center (MDACC) neuropsychology and neurosurgery databases. One hundred and three clinically-referred patients completed detailed neuropsychological evaluation before treatment between 2001 and 2010 and were subsequently included in the study. These patients were referred by their neurosurgeon for clinical purposes. Of those included, 73 had glioma restricted to the LTL while 30 had glioma limited to the RTL. The MDACC Institutional Review Board approved the study.
Data collection and coding
Temporal lobe segmentation
Three distinct temporal lobe areas were defined to describe tumor location, including the lateral anterior, lateral posterior, and medial regions. The anterior region comprised the temporal pole, in addition to the area lateral to the temporal horn of the ventricle extending approximately 30–35 mm posteriorly from the pole. The posterior region consisted of the lateral region extending posteriorly from that point, not to exceed 99 mm from the temporal pole. The medial region was designated as the area medial to the temporal horn of the lateral ventricle, including the hippocampal formation and parahippocampal gyrus. The tumor boundary was defined as the entire occupied space on T1-weighted MRI or the enhancing area on T1-weighted with contrast MRI. A fourth group, multi-region, included tumors with extension into two or more regions. More fine-grained segmentation was attempted but was not useful due to sample size limitations.
Lesion size
Volumetric analysis was performed on MRI scans with MedVision 1.41 software, as previously described [17]. T1-weighted volume was defined as the greater of the hypointense region on T1-weighted MRI, or the hyperintense area on gadolinium-enhanced T1-weighted MRI. FLAIR volume was defined as the area of hyperintensity identified on the FLAIR MRI sequence.
Neurocognitive testing
NCF testing was conducted by a neuropsychologist or a trained neuropsychology staff member supervised by a neuropsychologist. The NCF tests routinely administered are listed by domain with abbreviations defined in the tables accompanying the results. The number of patients administered a given NCF test differed by instrument, as the patient evaluations utilized a flexible battery and were performed for clinical purposes. Approximately half of the total sample did not have data for the HVLT-R DR and HVLT-R Recog variables, as clinic practices initially utilized an earlier version of the HVLT that did not include the delayed memory trials. Nonetheless, HVLT TR trials are identical between versions and HVLT-R normative data were used for all HVLT variables.
NCF test scores were standardized using published normative data [18–24], all of which were stratified by patient age, as well as gender and level of education when appropriate, and converted into z-scores (M = 0, SD = 1). Performance on an individual NCF test at or below a z-score of −1.5 was considered impaired. Grip Strength Difference and Grooved Pegboard Difference scores were calculated as the difference between the standardized scores of the hands contralateral and ipsilateral to the tumor. Motor performances were considered impaired if the hand contralateral to the tumor was at least 1.5 standard deviations less than the hand ipsilateral to the tumor. A derived composite was calculated, referred to as the Clinical Trial Battery Composite (CTB Comp). The CTB Comp variable is the mean of the z-scores for COWA, TMTA, TMTB, HVLT-R TR, HVLT-R DR, and HVLT-R Recog and has been routinely used in brain tumor clinical trials. [25–27] Impairment on the CTB Comp was defined as a score that fell at or below −.7, consistent with prior demonstration of optimal classification accuracy when compared to a full neuropsychological evaluation (unpublished data).
Statistical analysis
Independent-samples t-tests and Pearson χ2 tests were used to compare differences across LTL and RTL glioma patient groups for all clinical, demographic, and NCF variables. For mean NCF scores that significantly differed across temporal lobe groups, follow-up one-way analysis of covariance (ANCOVA) tests controlling for tumor grade (high vs. low) were performed, given known associations between tumor histology and NCF. [28] Mean NCF performances were further analyzed by temporal lobe region of lesion with one-way analysis of variance (ANOVA) for both LTL and RTL groups. Tukey’s honestly significant difference (HSD) test was used for post hoc comparisons. Associations between lesion volume (T1-weighted and FLAIR MRI) and NCF measures were determined with Pearson product-moment correlations (r). Volume indices that were significantly associated with NCF performances were included in follow-up analyses of significant LTL/RTL differences controlling for volume with one-way ANCOVA. Sensitivity analyses were conducted with independent-samples t-tests to determine relationships between NCF, handedness, seizure status, and medication use. All statistical analyses were performed with SPSS 21.0 (IBM Corp). Given the exploratory nature of the analyses, two-sided tests were used with an uncorrected significance level of p ≤ .05.
Results
Demographic and clinical characteristics
Sample characteristics are presented by LTL (n = 73) and RTL (n = 30) group in Table 1. Demographic and clinical characteristics did not significantly differ between groups.
Neurocognitive performances
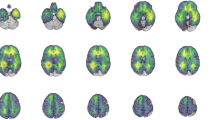
For the combined sample, 75 % of patients fell within the impaired range on at least 1 test, with similar rates of impairment on at least 1 test across LTL (74 %) and RTL (77 %) groups. Rates of NCF impairment on individual tests are shown in Fig. 1. LTL patients exhibited significantly greater rates of impairment than RTL patients on tests of attention [Digit Span: χ2(1, N = 103) = 3.90, p = .05] and expressive language [Naming: χ2(1, N = 101) = 3.78, p = .05]. Mean NCF performances are described in Table 2. LTL patients exhibited significantly worse performances than RTL patients on tests of attention [Digit Span: t(101) = −3.24, p = .01], verbal learning [HVLT-R TR: t(101) = −2.00, p = .05], and expressive [Naming: t(99) = −2.78, p = .01] and receptive language [Token: t(95) = −2.29, p = .03]. Follow-up ANCOVAs demonstrated that mean NCF group differences remained significant when controlling for tumor grade, including Digit Span [F(1, 100) = 11.21, p = .001, partial ω2 = .10], HVLT-R TR [F(1, 100) = 4.95, p = .03, partial ω2 = .05], Naming [F(1, 98) = 7.87, p = .006, partial ω2 = .07], and Token [F(1, 99) = 6.36, p = .01, partial ω2 = .06].
Neurocognitive impairment by LTL and RTL glioma group. Impairment defined as a z-score ≤ −1.5. Asterisks indicate significant differences between LTL and RTL groups, p ≤ .05. Sample sizes: Digit Span (LTL = 73; RTL = 30), HVLT-R TR (LTL = 73; RTL = 30), HVLT-R DR (LTL = 39; RTL = 12), HVLT-R Recog (LTL = 38; RTL = 13), Digit Symbol (LTL = 72; RTL = 30), TMTA (LTL = 72; RTL = 29), TMTB (LTL = 69; RTL = 28), Similarities (LTL = 70; RTL = 28), COWA (LTL = 73; RTL = 29), Token (LTL = 69; RTL = 28), Naming (LTL = 72; RTL = 29), Block Design (LTL = 72; RTL = 29), Grip (LTL = 70; RTL = 26), Peg (LTL = 72; RTL = 27), CTB Comp (LTL = 38; RTL = 11)
Neurocognitive performances by tumor location
NCF performances by tumor location within the temporal lobe are displayed in Table 3. For the LTL, auditory attention performances on Digit Span differed significantly across the 4 regions [F(3, 69) = 2.88, p = .04], though pair-wise post hoc comparisons did not remain significant. A trend was observed in which patients with multi-region LTL tumors tended to exhibit lower scores than those with tumors restricted to a single LTL region. Verbal memory performances showed a trend in which learning (HVLT-R TR) was lower for the lateral anterior LTL group while delayed memory (HVLT-R DR and Recog) was lower for the medial LTL group, though again, patients with LTL glioma with extension into multiple regions were lowest. Figure 2 displays verbal learning and memory performances by LTL region.
For the RTL, analyses of performances by regional involvement were limited by small group sizes. Nonetheless, processing speed on TMTA significantly differed across the four RTL regions [F(3, 28) = 5.86, p = .004]. Pair-wise post hoc comparisons indicated that patients with multi-region tumors performed significantly below those with tumors restricted to any individual region.
Clinical characteristics and NCF
With the exception of upper extremity strength, performances did not differ by handedness for either the LTL or RTL group. For patients with LTL glioma, Grip was significantly lower in right handed compared to left handed patients [t(68) = −5.19, p < .001]. Similarly, in the RTL group Grip was significantly lower for left handed versus right handed patients [t(24) = 2.54, p = .018].
Increased T1-weighted tumor volume was not associated with lower performance on any NCF measures for the LTL or RTL group. Increased FLAIR lesion volume of LTL patients was significantly associated with reduced auditory attention on Digit Span (r = −.26, df = 70), verbal learning on HVLT-R TR (r = −.27, df = 70), and manual dexterity on Peg (r = −.41, df = 69). For RTL patients, increased FLAIR volume was not associated with lower NCF test scores. Differences between LTL and RTL NCF performances remained significant after controlling for FLAIR volume for both Digit Span [F(1, 100) = 5.70, p = .01, partial ω2 = .10] and HVLT-R TR [F(1, 100) = 3.11, p = .05, partial ω2 = .04].
Patients with history of seizure did not perform significantly lower than those without on any measures. However, patients with history of seizure performed significantly better than those without on measures of receptive language [Token: (M = .22, SD = .87) vs. (M = −.38, SD = 1.25), t(100) = 2.86, p = .005] and executive function [TMTB: (M = −.61, SD = 1.97) vs. (M = −1.75, SD = 2.72), t(95) = 2.30, p = .024]. Of those patients with seizure, 91 % were on anticonvulsant medication. Patients on anticonvulsants also performed significantly better than those not on antiepileptic drugs on a measure of executive function [TMTB: (M = −.68, SD = 1.52) vs. (M = −2.47, SD = 3.48), t(81) = 3.26, p = .014]. Patients who were on steroids did not perform significantly differently than those not on the medication.
Discussion
To our knowledge, this represents the first comprehensive characterization of NCF in newly diagnosed, treatment-naïve patients with glioma restricted to the LTL or RTL. NCF impairment was common, as 75 % of the overall sample fell within the impaired range on at least 1 measure with similar rates between temporal lobe groups. This is slightly below impairment rates reported by Talacchi et al. [29] who assessed the pre-operative cognitive functioning of 29 patients with high or low grade glioma within frontal, temporal, or parieto-occipital regions. They identified NCF impairment on at least 1 measure in 79 % of preoperative glioma patients while utilizing a more conservative cut-off of 2.0 SDs below normative means. The observed impairment rates in our study also fell below those reported by Tucha et al. [30], who found impairment on 1 or more measures in over 90 % of patients with frontal or temporal glioma at the time of diagnosis, using a more liberal cut-off of approximately 1.3 SDs below normative means (10th percentile). These differences may be attributable, in part, to variability in sample sizes, NCF tests, normative standards, and impairment criteria. Additionally, the slightly higher impairment rates of other studies may reflect their inclusion of tumors within varying cerebral lobes, creating a sample with potentially more diffuse neuronal damage and associated NCF deficits. Nonetheless, the present findings establish that NCF impairment is frequent in temporal lobe glioma patients prior to initiation of treatment, regardless of cerebral hemisphere involved.
Neurocognitive profiles of patients with LTL and RTL glioma
The NCF profiles of LTL patients were characterized by relatively frequent impairment in verbal learning and memory, executive functioning, language, and attention. Difficulties within these domains tended to worsen with involvement of multiple temporal lobe regions, and attention and verbal learning were significantly associated with FLAIR (but not T1-weighted) volume, indicating that difficulties with these functions may be exacerbated by the presence of more infiltrative tumor and edema. Conversely, LTL patients generally performed within normal limits on measures of processing speed, visuospatial abilities, and motor function. However, it should be noted that manual dexterity was associated with FLAIR volume, suggesting that contralateral motor function may become impacted as edema surrounding LTL glioma increases. This is likely related to the influence of edema or mass effect impinging upon extratemporal motor pathways (e.g., the corticospinal tract).
Similar to their LTL counterparts, RTL glioma patients also exhibited prominent executive and verbal learning and memory impairment, with additional difficulties noted on measures of processing speed and fine motor control. Reduced motor control contralateral to the RTL tumor site may reflect greater vulnerability of nondominant versus dominant hand motor functions, as the population was largely right hand dominant. RTL group performances were generally within normal limits on measures of attention and most language functions. The NCF of RTL patients did not differ by region involved or T1-weighted and FLAIR volume.
While rates of memory and executive impairment were similar across LTL and RTL groups, impairment rates were significantly higher in the LTL group on indices of auditory attention and expressive language. Additionally, mean demographically-adjusted z-scores were significantly lower for the LTL group across measures of auditory attention, verbal learning, and receptive and expressive language indicating greater severity of impairment. Differences remained significant even when controlling for lesion volume and tumor grade. This lateralized pattern is generally consistent with the literature regarding the effects of focal temporal lobe epilepsy [10–13] and stroke [6–8]. These findings are also generally consistent with a recent report indicating that radiotherapy to LTL tumors results in worse memory and executive functioning outcomes, and radiation doses to the RTL causes deficits in visuospatial function. [31] Similarly, left hemisphere tumors have been previously associated with slower processing speed and attention deficits. [32] However, these studies were unable to identify effects specifically attributable to tumor location itself, as NCF testing occurred months to years after diagnosis and treatment, and lesion locations were distributed throughout various lobes of the brain. Accordingly, our results indicate more definitively that tumor itself can have a profound impact upon NCF prior to treatment, with temporal lobe glioma showing similar lateralizing patterns to that of other focal neurologic diseases.
Verbal memory performances, tumor location, and laterality
A trend was observed for LTL glioma patients, suggesting some regional differences within the LTL in verbal learning and memory processes. Specifically, new learning appeared most impacted by tumors restricted to anterior aspects of the LTL, while delayed recall and recognition were lowest when the tumors involved medial structures. This is consistent with findings implicating anterior LTL structures with encoding and the hippocampus with memory consolidation [5, 33, 37]. Although LTL glioma patients exhibited more severe verbal memory impairment, it is notable that RTL patients also showed frequent verbal memory deficits as discussed above. As such, hemispheric differences in temporal lobe memory functions may be more reflective of processing asymmetry rather than homogeneous lateralization of verbal and nonverbal abilities, consistent with mounting evidence from cognitive and clinical neuroscience [9, 33–37].
Potential limitations and strengths
While the present study advances the literature regarding temporal lobe glioma and NCF, and more generally, lateralization of temporal lobe functions, several limitations exist. Perhaps most limiting are the relatively small sample sizes, which restricted the ability to perform more fine-grained segmentation of tumor location, reducing the power to detect differences in NCF by temporal region involved. Additionally, the number of patients administered a given NCF measure differed by instrument, as the patient evaluations were performed for clinical purposes. Despite these considerations, the sample size was of similar if not favorable size compared to existing studies, and the battery of tests was fairly comprehensive. Another strength is regional specificity, as all patients had tumors restricted to the temporal lobes with similar distribution of tumors within the temporal lobe across LTL and RTL groups.
Consistent with existing literature, a large proportion of the sample had comorbid seizures [38], likely originating from tissue near the tumor within the temporal lobe. It is well-known that temporal lobe epilepsy often results in significant NCF impairment, with memory representing one of the most commonly affected domains [9]. However, glioma patients with seizure disorder did not perform worse than those without. Interestingly, patients with a history of seizures actually performed better than those without on measures of receptive language and executive function. Similarly, those on antiepileptic medications exhibited better executive function performances than those not taking antiepileptic medication. Rather than suggesting a positive effect of seizures or anticonvulsant medication upon NCF, this likely reflects the fact that fewer high grade glioma patients have seizures compared to lower grade patients [38], and those with high grade glioma tend to exhibit greater NCF problems than low grade patients [28].
Conclusions
Patients with glioma involving the temporal lobes frequently present with significant NCF impairment. Similar to findings with other focal neurological populations, the pattern of deficits for LTL patients revealed greatest weaknesses with verbal learning, memory, and language, though additional problems with executive functioning and attention were observed. While NCF deficits were somewhat more severe and widespread for the LTL group, impairment was frequent in both RTL and LTL groups, even on measures of verbal memory. This suggests that verbal memory processes may recruit distributed bilateral brain regions, questioning the strict lateralization of verbal learning and recall. While consistent with emerging cognitive neuroscience regarding distributed neural networks, these findings may also reflect a more diffuse pathophysiological lesion for brain tumors than other focal neurological diseases. Incorporation of structural and functional neuroimaging techniques with traditional neuropsychological methods may improve our understanding of the underlying brain dysfunction responsible for the development of NCF impairment in patients with lateralized glioma. Nonetheless, the data presented can help clinicians better understand expected NCF difficulties for temporal lobe glioma at time of initial presentation, which may be further useful in the prediction of longitudinal outcome, though further work is needed.
References
Benedict RHB, Schretlen D, Groninger L, Brandt J (1998) Hopkins verbal learning test revised: normative data and analysis of inter-form and test-retest reliability. Clin Neuropsychol 12:43–55
Wefel JS, Cloughesy T, Zazzali JL et al (2011) Neurocognitive function in patients with recurrent glioblastoma treated with bevacizumab. Neuro Oncol 13:660–668
Hilverda K, Bosma I, Heimans JJ et al (2010) Cognitive functioning in glioblastoma patients during radiotherapy and temozolomide treatment: initial findings. J Neurooncol 97:89–94
Scheibel RS, Meyers CA, Levin VA (1996) Cognitive dysfunction following surgery for intracerebral glioma: influence of histopathology, lesion location, and treatment. Neuro Oncol 30:61–69
Weitzner MA, Meyers CA (1997) Cognitive functioning and quality of life in malignant glioma patients: a review of the literature. Psychooncology 6:169–177
Anderson SW, Damasio H, Tranel D (1990) Neuropsychological impairments associated with lesions caused by tumor or stroke. Arch Neurol 47:397–405
Cumming TB, Marshall RS, Lazar RM (2013) Stroke, cognitive deficits, and rehabilitation: still an incomplete picture. Int J Stroke 8:38–45
Edwards JD, Jacova C, Sepehry AA, Pratt B, Benavente OR (2013) A quantitative systematic review of domain-specific cognitive impairment in lacunar stroke. Neurology 80:315–322
Bell B, Lin JJ, Seidenberg M, Herman B (2011) The neurobiology of cognitive disorders in temporal lobe epilepsy. Nat Rev Neruol 7:154–164
Bigras C, Shear PK, Vannest J, Allendorfer JB, Szaflarski JP (2013) The effects of temporal lobe epilepsy on scene encoding. Epilepsy Behav 26:11–21
Lillywhite LM, Saling MM, Briellmann RS, Weintrob DL, Pell GS, Jackson GD (2007) Differential contributions of the hippocampus and rhinal cortices to verbal memory in epilepsy. Epilepsy Behav 10:553–559
Longo CA, Kerr EN, Smith ML (2013) Executive functioning in children with intractable frontal lobe or temporal lobe epilepsy. Epilepsy Behav 26:102–108
Amlerova J, Laczo J, Vlcek K, Javurkova A, Andel R, Marusic P (2013) Risk factors for spatial memory impairment in patients with temporal lobe epilepsy. Epilepsy Behav 26:57–60
Jones-Gotman M, Zatorre RJ, Olivier A et al (1997) Learning and retention of words and designs following excision from medial or lateral temporal-lobe structures. Neuropsychologia 35:963–973
Kennepohl S, Sziklas V, Garver KE, Wagner DD, Jones-Gotman M (2007) Memory and the medial temporal lobe: hemispheric specialization reconsidered. Neuroimage 36:969–978
Johnson SC, Saykin AJ, Flashman LA, McAllister TW, Sparling MB (2001) Brain activation on fMRI and verbal memory ability: functional neuroanatomic correlates of CVLT performance. J Int Neuropsychol Soc 7:55–62
Shi WM, Wildrick DM, Sawaya R (1998) Volumetric measurement of brain tumors from MR imaging. J Neurooncol 37(1):87–93
Benton A, Hamsher K, Sivan A (2000) Multilingual aphasia examination manual. AJA Associates Inc., Iowa City
Heaton RK, MillerSW Taylor MJ, Grant I (2004) Revised comprehensive norms for an expanded Halstead-Reitan battery: demographically adjusted neuropsychological norms for African American and Caucasian adults. Psychological Assessment Resources Inc, Lutz
Ruff RM, Light RH, Parker SB, Levin HS (1996) Benton controlled oral word association test: reliability and updated norms. Arch Clin Neuropsychol 11:329–338
Tombaugh TN (2004) Trail making test A and B: normative data stratified by age and education. Arch Clin Neuropsychol 19:203–214
Trites Ronald L (1977) Neuropsychological test manual. Royal Ottawa Hospital, Ottawa
Wechsler D (1981) Wechsler adult intelligence scale–revised. The Psychological Corporation, San Antonio
Wechsler D (1997) Wechsler adult intelligence scale–III. The Psychological Corporation, San Antonio
Armstrong TR, Wefel JS, Wang M et al (2013) Net clinical benefit analysis of Radiation Therapy Oncology Group 0525: a phase III trial comparing conventional adjuvant temozolomide with dose-intensive temozolomide in patients with newly diagnosed glioblastoma. J Clin Oncol 31:4076–4084
Brown PD, Pugh S, Laack NN et al (2013) Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: a randomized, double-blind, placebo-controlled trial. J Neuroncol 15:1429–1437
Gilbert MR, Dignam JJ, Armstrong TS et al (2014) A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 370:699–708
Noll KR, Sullaway C, Ziu M, Weinberg JS, Wefel JS (2015) Relationships between tumor grade and neurocognitive functioning in patients with glioma of the left temporal lobe prior to surgical resection. Neuro Oncol 17(4):580–587
Talacchi A, Santini B, Savazzi S, Gerosa M (2011) Cognitive effects of tumour and surgical treatment in glioma patients. J Neurooncol 103:541–549
Tucha O, Smely C, Preier M, Lange KW (2000) Cognitive deficits before treatment among patients with brain tumors. Neurosurgery 47:324–333
Peiffer AM, Leyrer CM, Greene-Schloesser DM et al (2013) Neuroanatomical target theory as a predictive model for radiation-induced cognitive decline. Neurology 80:747–753
Klein M, Heimans JJ, Aaronson NK et al (2002) Effect of radiotherapy and other treatment-related factors on mid-term to long-term cognitive sequelae in low-grade gliomas: a comparative study. Lancet 360:1361–1368
Golby AJ, Poldrack RA, Brewer JB et al (2001) Material-specific lateralization in the medial temporal lobe and prefrontral cortex during memory encoding. Brain 124:1841–1854
Lee TM, Yip JT, Jones-Gotman M (2002) Memory deficits after resection from left or right anterior temporal lobe in humans: a meta-analytic review. Epilepsia 43:283–291
Martins IP, Caeiro L, Ferro JM (2013) Cognitive and behavioral disorders according to stroke site and side. In: Godefroy O (ed) The behavioral and cognitive neurology of stroke, 2nd edn. Cambridge, New York
Ralph MA, Ehsan S, Baker GA, Rogers TT (2012) Semantic memory is impaired in patients with unilateral anterior temporal lobe resection for temporal lobe epilepsy. Brain 135:242–258
Saling MM (2009) Verbal memory in mesial temporal lobe epilepsy: beyond material specificity. Brain 132:570–582
Shaller B, Ruegg SJ (2003) Brain tumor and seizures: pathophysiology and its implications for treatment revisited. Epiliepsia 44:1223–1232
Acknowledgments
Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number R01NR014195 (J.S.Wefel). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Rights and permissions
About this article
Cite this article
Noll, K.R., Ziu, M., Weinberg, J.S. et al. Neurocognitive functioning in patients with glioma of the left and right temporal lobes. J Neurooncol 128, 323–331 (2016). https://doi.org/10.1007/s11060-016-2114-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-016-2114-0