Abstract
Pseudoprogression (psPD) is a radiation-induced toxicity that has substantial neurological consequence in glioblastoma (GBM) patients. MGMT promoter methylation has been shown to be an important prognostic factor of psPD, but the significance of extent of resection (EOR) remains unclear. We performed a retrospective analysis on newly diagnosed GBM patients with assessable MGMT promoter status who underwent the Stupp protocol. EOR was grouped into gross total resection (GTR), subtotal resection (STR), partial resection (PR) and stereotactic biopsy. Contrast enhancing lesion enlargement was classified as psPD or non-psPD. Among a total of 101 patients, GTR, STR, PR and stereotactic biopsy was performed in 57 (56.4 %), 34 (33.7 %), 9 (8.9 %) and 1 patient (1 %), respectively. Follow-up imaging at the end of Stupp protocol classified 45 patients (44.6 %) as psPD and 56 (55.4 %) as non-psPD. psPD was observed in 24 (61.5 %) of 39 patients with methylated MGMT promoter and 21 (33.9 %) of 62 patients with unmethylated MGMT promoter (p < 0.01). psPD was documented in 17 (29.8 %), 19 (55.9 %), 8 (88.9 %) and 1 (100 %) patient with GTR, STR, PR and stereotactic biopsy (p < 0.01), respectively. On multivariate analysis MGMT promoter status (OR 3.36, 95 % CI 1.36–8.34) and EOR (OR 4.12, 95 % CI 1.71–9.91) were independent predictors of psPD. A Cox proportional hazards model showed that MGMT status (HR 2.51, p < 0.01) and EOR (HR 2.99, p < 0.01) significantly influenced survival. MGMT status and EOR have a significant impact on psPD. GTR can reduce the side effects of psPD and prolong survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glioblastoma is the most common primary malignant brain tumor in adults and has a dismal prognosis [1, 2]. Median survival is only 14.6 months even with the standard care of, so-called Stupp protocol [3]. The occurrence of pseudoprogression (psPD), radiation-induced toxicity that has substantial neurological consequences, has been increasingly recognized since the European and Canadian randomized trial was published in 2005 [4–8]. Although psPD has been reported to be a favorable factor for survival it can have detrimental clinical consequence, increase the use of corticosteroids and downgrade the quality of life for glioblastoma patients. In addition, the difficulty in distinguishing psPD from a true progression can be misleading, and even fatal. psPD has been recognized as a manifestation of radiation therapy, but there are only a few publications on its actual incidence within a large series of glioblastoma patients undergoing the Stupp protocol. This can be attributed to the large number of factors that can create biases in the radiologic diagnosis of psPD. Moreover, despite technological advances in neuroimaging there is no imaging modality that can clearly differentiate psPD from a true progression. Known risk factors of psPD include total radiation dose, fraction size, addition of stereotactic radiosurgery (SRS) or chemotherapy to radiotherapy, and 06-methylguanine-DNA methyltransferase (MGMT) promoter methylation status, but the significance of extent of resection (EOR) remains unclear [6, 9–13]. The purpose of this study was to investigate the incidence and the prognostic importance of EOR for psPD in newly diagnosed glioblastoma patients with assessable MGMT promoter methylation status who were treated with the Stupp protocol.
Materials and methods
Eligibility criteria
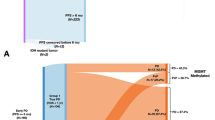
From July 2006 to November 2013, a total of 258 patients underwent surgery for newly diagnosed glioblastoma at Yonsei University Health System in Seoul, Republic of Korea. The data of 204 patients with assessable MGMT promoter methylation status were analyzed retrospectively after obtaining informed consent from every patient. The study was approved by the institutional review board and conducted in accordance with the ethical guidelines of the Declaration of Helsinki. In total, 175 patients underwent radiotherapy plus continuous daily temozolomide (TMZ) followed by 6 cycles of maintenance TMZ on an outpatient basis. Patients who only underwent surgery (n = 7), surgery followed by radiotherapy (n = 5), surgery followed by radiotherapy and chemotherapy (n = 3), and surgery followed by concurrent chemoradiotherapy only (n = 14) were excluded from the study. Of these, 101 patients were enrolled in the study excluding those who received total radiation dose exceeding 66 Gy (n = 31), fraction size exceeding 2.5 Gy (n = 5), and addition of SRS (n = 16) or immunotherapy (n = 22).
Patient evaluation
Patients’ neurologic status and blood tests for hematologic, renal, and liver panels were checked before the beginning of each chemotherapy cycle. Follow-up magnetic resonance imaging (MRI) was performed 4 weeks after the end of concurrent chemoradiotherapy, 23 days after the end of the 3rd and 6th TMZ cycles, every 6 months for the first 2 years after the end of Stupp protocol, and annually thereafter. DNA isolated from paraffin-embedded samples was used to determine MGMT promoter status by methylation-specific polymerase chain reaction (MSP) as previously described with some modifications [14–16]. Low-quality DNA yielding uncertain results on PCR results were discarded. Unmethylated control DNA and methylated control DNA with bisulfite treatment (Qiagen, Germany) were used as negative and positive controls, respectively. After the DNA was annealed at a temperature of 59 °C, PCR products were separated on 8 % polyacrylamide gels, stained with ethidium bromide and examined under ultraviolet illumination by a pathologist who was blinded to clinical information. MGMT promoter status was determined based on the molecular size of the PCR product compared to negative and positive controls [14–16].
Treatment (surgery, radiotherapy and chemotherapy)
Surgery was performed under neuro-navigation guidance (iNtellect Cranial Navigation®, Stryker, MI, USA) with diffuse tensor imaging (DTI) tractography (Stealthviz™, Medtronic, MN, USA) and 5-aminolevulinic acid (5-ALA) fluorescence. Patients took a standard preoperative oral dose of 1500 mg 5-ALA (Gliolan®, Medac, Germany) mixed with 50 mL of sterile water, 4 h prior to surgery. A blue-filter modified microscope (OPMI Pentero®, Carl Zeiss AG, Germany) was used for fluorescence guidance. Extent of resection (EOR) was classified by comparing contrast enhancing lesion between preoperative and postoperative gadolinium enhanced T1-weighted MRI performed within 48 h after surgery. All images were reviewed retrospectively by a single, experienced neuro-radiologist who was blinded to clinical information, taking into account postoperative blood products that appear hyperintense on non-contrast T1-weighted images. Patients were classified into four groups based on EOR: gross total resection (GTR), defined as more than 95 % resection; subtotal resection (STR), 90–95 % resection; partial resection (PR), less than 90 % resection; and stereotactic biopsy if the objective was histologic confirmation with no intention of cytoreduction. GTR included lobectomies, sparing eloquent areas in cases of non-dominant frontal or temporal lobe lesions. In cases of dominant hemisphere lesions, maximal lesionectomy with 5-ALA fluorescence was performed leaving eloquent areas with minimal 5-ALA staining. Areas of eloquence were defined according to the University of California, San Francisco (UCSF) classification and were as follows: sensorimotor areas (precentral and postcentral gyri), basal ganglia, internal capsule, thalamus, visual cortex around the calcarine sulcus and perisylvian language areas in the dominant hemisphere (superior temporal, inferior frontal, inferior parietal gyri) [17]. Tumor size was measured as the largest diameter of a contrast enhancing lesion on gadolinium enhanced T1-weighted MRI.
During the concomitant chemoradiotherapy phase, TMZ chemotherapy (75 mg/m2) was administered daily before each radiotherapy session. Radiotherapy began within 3 weeks after surgery in most of the patients. All patients received three-dimensional conformal radiotherapy (3D-CRT) or intensity-modulated radiotherapy (IMRT) with tomotherapy after computed tomography (CT) simulation. Gross tumor volume (GTV) was defined as the contrast enhancing residual tumor and operative cavity plus a 0.5–1 cm margin. Clinical target volume (CTV) was defined as the GTV plus peritumoral edema with a 1–2 cm margin. A smaller CTV (GTV plus a 1.5–2 cm margin, excluding the entire peritumoral edema) was applied for some patients (25/101, 24.8 %) in the earlier years of this study. CTV– GTV represented peritumoral edema with a 1–2 cm margin. Median GTV, CTV, and CTV–GTV were 115.0 cm3 (range, 10.6–307.2 cm3), 366.6 cm3 (range, 87.6–732.6 cm3), and 248.9 cm3 (range, 45.1–588.5 cm3), respectively. High and low GTV, CTV, and CTV–GTV were divided by their median values. Median doses of 60 Gy (range, 42–66 Gy) and 46 Gy (range, 24–54 Gy) were prescribed for the GTV and CTV, respectively. The most commonly used dose-fractionation schedule was 60 Gy with 2 Gy per fraction. Median duration of radiotherapy was 43 days (range, 30–74 days).
Maintenance TMZ chemotherapy (150 mg/m2/day for the first cycle and then 200 mg/m2/day for 5 days, every 28 days) was suspended after 6 cycles only if follow-up MRI showed no radiologic abnormalities according to the Response Assessment in Neuro-Oncology (RANO) criteria and the case was considered to be non-progressive disease (non-PD) [18]. A median 6 cycles (range, 1–24) of TMZ were administered. Chemotherapy was stopped at any time during the Stupp protocol under the following conditions: Karnofsky performance status (KPS) <50, absolute neutrophil count (ANC) <500/mm3, platelet count <10,000/mm3, or Common Terminology Criteria for Adverse Event (CTCAE) grade 3 or above (version 4.0, National Cancer Institute, published June 14, 2010).
Diagnosis of pseudoprogression
T2-weighted and gadolinium enhanced T1-weighted axial, coronal, sagittal images were acquired using 1.5-T (Intera, Philips Medical Systems, Best, Netherlands or Signa, General Electric Healthcare, Milwaukee, WI, USA) or 3.0-T (Achieva, Philips Medical Systems, Best, Netherlands) MRI systems. New enhancing lesions on gadolinium-enhanced T1-weighted MRI that appeared within the radiation field and regressed upon observation alone or with corticosteroids on serial MRI follow-ups were regarded as pseudoprogression (psPD) [18]. Lesions outside or within the radiation field that failed to disappear and continued to increase were considered progressive disease (PD) with consequent discontinuation of chemotherapy. PD and non-PD patients were defined as non-psPD patients. Diagnostic modalities other than conventional MRI such as magnetic resonance perfusion imaging (MRP), magnetic resonance spectroscopy (MRS), fluoro-deoxy glucose positron emission tomography (FDG-PET) and surgical tissue confirmation were used for equivocal diagnosis between psPD and PD.
MRP was performed to calculate the relative cerebral blood volume (rCBV) of the lesion of interest. Decreased rCBV indicated psPD resulting from ischemic changes caused by occlusive vasculopathy [19]. Multi voxel proton MRS was performed to compare the MR spectra of the lesion of interest and the adjacent normal brain tissue. Changes in choline (Cho)/creatinine (Cr) and N-acetylaspartate (NAA)/Cr ratios were also evaluated. Normal values for Cho/Cr and NAA/Cr were obtained from the normal appearing white matter on the contralateral hemisphere. Increased lactate/Cr and decreased Cho/Cr suggested psPD, which has previously been shown to dramatically increase lactate, and reduce NAA and Cr levels [20]. Patients undergoing 18F-FDG-PET were evaluated for metabolic activity using the radiotracer. No metabolic activity or radiotracer uptake implied psPD because of the low glucose metabolism in psPD [21].
psPD was diagnosed with conventional MRI (n = 16), surgery (n = 4), and by MRI combined with MRS (n = 11), MRP (n = 11), and FDG-PET (n = 3).
Statistical analysis
The interval to the development of psPD was defined as the time from completion of concomitant chemoradiotherapy to the time of diagnosis of psPD. Clinicopathologic factors affecting the incidence of psPD were evaluated using the two sample Student t test for continuous variables and the Fischer’s exact test for categorical variables. Multivariate analysis was performed using binary logistic regression analysis to determine predictors of psPD that had significance on univariate analysis. Results were presented as odds ratio (OR) with 95 % confidence interval (CI). Overall survival (OS) was measured from the day of surgery to the day of death or last outpatient visit. The Kaplan–Meier method was used to estimate OS. Univariate predictors of survival were assessed by the log-rank comparison method. Multivariate analysis was performed using the Cox proportional hazards model with factors that had significance on univariate analysis. Results were presented as hazards ratio (HR) with a 95 % CI. All statistical analyses were performed with SPSS software version 18.0 for Windows (SAS Institute, Inc., Chicago, IL, USA). Two-tailed p values of ≤0.05 were considered statistically significant.
Results
Patient characteristics
The study included 58 female (57.4 %) and 43 male patients with a median age of 57 years (range, 22–78 years) and a median KPS of 70 (range, 40–90). The median tumor size was 4.7 cm (range, 1–10 cm) and GTR, STR, PR, and stereotactic biopsy were performed in 57 (56.4 %), 34 (33.7 %), 9 (8.9 %), and 1 patient (1 %), respectively. MGMT promoter was methylated in 39 patients (38.6 %) and unmethylated in 62 patients (61.4 %). Median follow-up duration after surgery was 17.9 months (range, 4.0–76.1 months) (Table 1).
psPD was diagnosed in 45 patients (44.6 %), PD in 38 patients (37.6 %), and non-PD in 18 patients (17.8 %) at last MRI scan performed after the end of the Stupp protocol. Median interval to development of psPD was 3.9 months (range, 0–20 months). Patients who were diagnosed with psPD were symptomatic in 62.2 % of cases, with hemiparesis being the most common neurologic deficit (Table 2). There were no newly developed radiation-induced symptoms in non-psPD patients. Thiry-one patients (68.9 %) required corticosteroids, 4 patients (8.9 %) underwent cytoreductive surgery and psPD regressed in 10 patients (22.2 %) under observation alone. The majority of symptomatic patients improved after treatment, but 9 patients (32.1 %) remained unchanged.
Predictors of pseudoprogression
psPD was observed in 24 (61.5 %) of 39 patients with methylated MGMT promoter and 21 (33.9 %) of 62 patients with unmethylated MGMT promoter (p < 0.01). The incidence of psPD was different according to EOR: 29.8 % (17/57) for GTR, 55.9 % (19/34) for STR, 88.9 % (8/9) for PR, and 100 % (1/1) in the biopsy group (p < 0.01) (Table 3). There were no differences between the psPD and non-psPD group in preoperative KPS, tumor size, median GTV (105.7 cm3 for psPD, and 118.4 cm3 for non-psPD), median CTV (366.0 cm3 for psPD, and 367.1 cm3 for non-psPD), median CTV–GTV (198.9 cm3 for psPD, and 256.3 cm3 for non-psPD), and number of lobes involved by the lesion before surgery. On multivariate analysis MGMT promoter status (OR 3.36, 95 % CI 1.36–8.34) and EOR (OR 4.12, 95 % CI 1.71–9.91) were independent predictors of psPD (Table 4).
Significance of pseudoprogression on survival
A median OS of 28.8 months (95 % CI, 21.6–36.0 months) was achieved: 39.6 months (95 % CI, 27.8–51.3 months) in the psPD group and 24.7 months (95 % CI, 19.8–29.6 months) in the non-psPD group, with no statistical difference (p = 0.187). Median OS according to EOR divided into GTR and non-GTR groups was 39.6 months (95 % CI, 26.0–53.1 months) and 19.9 months (95 % CI, 15.5–24.5 months), respectively (p < 0.01). Median OS was also analyzed to determine the significance of pseudoprogression on survival within each EOR group. A significant difference in survival was noted between psPD and non-psPD patients who received GTR (p = 0.043) (Fig. 1a), but significance was lost in the STR (p = 0.792) (Fig. 1b) and PR groups (p = 0.395) (Fig. 1c). There was also no difference in survival between psPD and non-psPD patients who achieved more than 90 % tumor resection (STR and GTR groups) (p = 0.299). Age (p = 0.565), preoperative KPS (p = 0.718), and lesion eloquence (p = 0.187) were not predictive of survival. A Cox proportional hazards model showed that MGMT status (HR 2.51, p < 0.01) and EOR (HR 2.99, p < 0.01) significantly influenced survival.
Discussion
Distinguishing psPD from a PD in newly diagnosed glioblastoma patients undergoing the Stupp protocol has been a diagnostic dilemma for neuro-oncologists. psPD and PD share in common the underlying mechanism of blood–brain barrier (BBB) disruption, which causes nonspecific contrast enhancing lesion enlargement on MRI. Hence, misdiagnoses are frequent and can lead to inadequate, inappropriate or delayed treatment. psPD is a reversible change that generally occurs 3–12 months after the end of radiotherapy, but predominantly appears in the first 3 months [22]. The incidence of psPD in glioblastoma patients receiving the standard treatment has been reported to range from 6 to 46.7 %, but is suspected to occur more frequently [23]. For these reasons, many neuro-oncologists and the RANO criteria advocate caution when diagnosing PD until completion of the 3rd maintenance TMZ cycle, which falls within 3 months after the end of radiotherapy. This principle was followed carefully in this study, which no patient recurred before termination of the 3rd TMZ cycle. Correct diagnosis of psPD has been a controversial issue in studies involving this radiation-induced phenomenon. Even with the most advanced radiologic tool available today, serial imaging with conventional MRI may still remain the most reliable method to determine psPD or PD [4–6]. However, in equivocal diagnoses where follow-up imaging cannot yield a conclusion, imaging modalities with greater discrimination (higher specificity) can help avoid unnecessary surgeries. MRP, MRS, and FDG-PET are some of the tools with higher specificity that can compensate for the high false positive rate of a conventional MRI [24].
Apart from achieving a correct diagnosis, there are several other factors to consider in psPD studies. Radiation-related risk factors such as total radiation dose, fraction size, and the addition of SRS or chemotherapy to radiotherapy are potential biases that can affect psPD [9–13]. The occurrence of psPD shows a steep increase when total radiation doses exceed 65 Gy or fraction doses exceed 2.5 Gy per day [9–11]. Excluding these elements from the beginning of this analysis was important in order to examine the significance of EOR on psPD. To the authors’ knowledge, EOR has not previously been identified as a significant factor in psPD. The pathophysiology of psPD represents a combination of endothelial cell apoptosis, BBB breakdown, and radiation injury to residual tumor cells [25]. According to this notion, a greater number of residual tumor cells with increased apoptosis and disrupted BBB will lead to increased permeability and, as a consequence, radiographic enhancement. Brandes et al. [6] showed that MGMT methylated glioblastomas harbor higher incidence of psPD than unmethylated tumors. MGMT is an enzyme that inhibits apoptosis by preventing the accumulation of O6-methylguanine. Methylation of the MGMT promoter silences its expression, impeding the cell’s capability to repair radiation induced DNA damage and resulting in cell death [26, 27]. The results of this study showed that the greater the number of residual contrast enhancing tumor cells, the more susceptible the cells are to radiation injury. Larger CTV–GTV generally indicates that more normal brain tissue containing microscopically infiltrative tumor cells are being irradiated. Therefore, increased incidence of radiation-induced injury can be expected, regardless of EOR. However, a wider radiation field including the peritumoral edema did not increase the incidence of psPD in this study. This might be due to the fact that more tumor cells susceptible to radiation injury exist within the contrast enhancing region than the peritumoral edema [25].
It has previously been suggested that psPD has a favorable impact on survival in newly diagnosed glioblastoma patients undergoing the Stupp protocol [5, 6]. There is no doubt that epigenetic silencing of MGMT leads to improved survival [28]. Since MGMT methylated tumors tend to have higher levels of psPD and the biology of psPD enhances the effectiveness of chemotherapeutic agents, one might expect prolonged survival in patients with psPD. However, the results of this study showed that the occurrence of psPD was associated with increased survival only in the patients with GTR, and not in patients with gross residual tumors. We believe that the effect of EOR overpowers the effect of psPD associated with MGMT methylation. On multivariate analysis, only MGMT status and EOR significantly influenced survival.
The ultimate goal of decreasing psPD is to avoid any undesired neurologic deficits that can lower the patient’s compliance with the Stupp protocol. In this study, 62.2, 68.9 and 20 % of the patients with psPD exhibited neurologic deterioration, prolonged use of corticosteroids, and early termination of the Stupp protocol due to permanent deficits, respectively. EOR based on gadolinium enhancement proved to be sufficient for reducing psPD and its subsequent consequences as long as it included more than 95 % removal of the contrast enhancing lesions on MRI. psPD is a diagnosis of uncertainty. Only careful MRI follow-up according to the RANO criteria with the use of advanced radiologic techniques will help discern psPD from a PD in equivocal situations.
Conclusion
psPD is a radiation-induced phenomenon with subsequent brain edema that can lead to neurologic deterioration, prolonged use of corticosteroids and early termination of the Stupp protocol in newly diagnosed glioblastoma patients. It can be confusing with a true progression, leading to the risk of inappropriate, inadequate, or delayed treatment. MGMT status and EOR have a significant impact on psPD. GTR can concomitantly reduce the side effects of psPD and prolong survival.
References
Deorah S, Lynch CF, Sibenaller ZA, Ryken TC (2006) Trends in brain cancer incidence and survival in the United States: surveillance, epidemiology, and end results program, 1973 to 2001. Neurosurg Focus 20(4):E1
Surawicz TS, Davis F, Freels S, Laws ER Jr, Menck HR (1998) Brain tumor survival: results from the National Cancer Data Base. J Neurooncol 40:151–160
Stupp R, Mason WP, van den Bent MJ et al (2005) Radiotherapy plus concomitant and adjuvant temozolomide for glioblastoma. N Engl J Med 352:987–996
Chamberlain MC, Glantz MJ, Chalmers L, Van Horn A, Sloan AE (2007) Early necrosis following concurrent Temodar and radiotherapy in patients with glioblastoma. J Neurooncol 82:81–83
Taal W, Brandsma D, de Bruin HG et al (2007) The incidence of pseudo-progression in a cohort of malignant glioma patients treated with chemo-radiation with temozolomide. Cancer 113:405–410
Brandes AA, Franceschi E, Tosoni A et al (2008) MGMT promoter methylation status can predict the incidence and outcome of pseudoprogression after concomitant radiochemotherapy in newly diagnosed glioblastoma patients. J Clin Oncol 26:2192–2197
Peca C, Pacelli R, Elefante A et al (2009) Early clinical and neuroradiological worsening after radiotherapy and concomitant temozolomide in patients with glioblastoma: tumour progression or radionecrosis? Clin Neurol Neurosurg 111:331–334
Yaman E, Buyukberber S, Benekli M et al (2010) Radiation induced early necrosis in patients with malignant gliomas receiving temozolomide. Clin Neurol Neurosurg 112:662–667
Ruben JD, Dally M, Bailey M, Smith R, McLean CA, Fedele P (2006) Cerebral radiation necrosis: incidence, outcomes, and risk factors with emphasis on radiation parameters and chemotherapy. Int J Radiat Oncol Biol Phys 65:499–508
Brandsma D, Stalpers L, Taal W, Sminia P, van den Bent MJ (2008) Clinical features, mechanisms, and management of pseudoprogression in malignant gliomas. Lancet Oncol 9:453–461
Floyd NS, Woo SY, Teh BS et al (2004) Hypofractionated intensity-modulated radiotherapy for primary glioblastoma multiforme. Int J Radiat Oncol Biol Phys 58:721–726
Nieder C, Andratschke N, Wiedenmann N, Busch R, Grosu AL, Molls M (2004) Radiotherapy for high-grade gliomas. Does altered fractionation improve the outcome? Strahlenther Onkol 180:401–407
Hara W, Tran P, Li G et al (2009) Cyberknife for brain metastases of malignant melanoma and renal cell carcinoma. Neurosurgery 64:A26–A32
Esteller M, Hamilton SR, Burger PC, Baylin SB, Herman JG (1999) Inactivation of the DNA repair gene O6-methylguanine-DNA methyltransferase by promoter hypermethylation is a common event in primary human neoplasia. Cancer Res 59:793–797
Esteller M, Garcia-Foncillas J, Andion E et al (2000) Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med 343:1350–1354
Hegi ME, Diserens AC, Gorlia T et al (2005) MGMT gene silencing and benefit from temozolomide in glioblastoma. NEJM 352:997–1003
Chang EF, Smith JS, Chang SM et al (2008) Preoperative prognostic classification system for hemispheric low-grade gliomas in adults. J Neurosurg 109:817–824
Wen PY, Macdonald DR, Reardon DA et al (2010) Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol 28:1963–1972
Ellika SK, Jain R, Patel SC et al (2007) Role of perfusion CT in glioma grading and comparison with conventional MR imaging features. Am J Neuroradiol 28:1981–1987
Kamada K, Houkin K, Abe H, Sawamura Y, Kashiwaba T (1997) Differentiation of cerebral radiation necrosis from tumor recurrence by proton magnetic resonance spectroscopy. Neurol Med-Chir 37:250–256
Chao ST, Suh JH, Raja S, Lee SY, Barnett G (2001) The sensitivity and specificity of FDG PET in distinguishing recurrent brain tumor from radionecrosis in patients treated with stereotactic radiosurgery. Int J Cancer 96:191–197
de Wit MC, de Bruin HG, Eijkenboom W, Sillevis Smitt PA, van den Bent MJ (2004) Immediate post-radiotherapy changes in malignant glioma can mimic tumor progression. Neurology 63:535–537
Brandsma D, van den Bent MJAN (2009) Pseudoprogression and pseudoresponse in the treatment of gliomas. Curr Opin Neurol 22:633–638
Shah AH, Snelling B, Bregy A et al (2013) Discriminating radiation necrosis from tumor progression in gliomas: a systematic review what is the best imaging modality? J Neurooncol 112:141–152
Siu A, Wind JJ, Iorgulescu JB, Chan TA, Yamada Y, Sherman JH (2012) Radiation necrosis following treatment of high grade glioma—a review of the literature and current understanding. Acta Neurochir (Wien) 154:191–201
Liu L, Markowitz S, Gerson SL (1996) Mismatch repair mutations override alkyltransferase in conferring resistance to temozolomide, but not to 1,3-bis (2-chloroethyl) nitrosourea. Cancer Res 56:5375–5379
Ochs K, Kaina B (2000) Apoptosis induced by DNA damage O6-methylguanine is Bcl-2 and caspase-9/3 regulated and Fas/caspase-8 independent. Cancer Res 60:5815–5824
Olson RA, Brastianos PK, Palma DA (2011) Prognostic and predictive value of epigenetic silencing of MGMT in patients with high grade gliomas: a systematic review and meta-analysis. J Neurooncol 105:325–335
Acknowledgments
This study was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (NRF-2014R1A1A2058058).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Park, H.H., Roh, T.H., Kang, S.G. et al. Pseudoprogression in glioblastoma patients: the impact of extent of resection. J Neurooncol 126, 559–566 (2016). https://doi.org/10.1007/s11060-015-2001-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-015-2001-0