Abstract
Primary central nervous system lymphoma (PCNSL) is a rare non-Hodgkin’s lymphoma that occurs in immunocompetent and human immunodeficiency virus (HIV) patients. Despite treatment advances, previous reports have produced conflicting information about survival trends over time. Using the Surveillance, Epidemiology, and End Results (SEER) data, 2,557 patients diagnosed with PCNSL between 1973 and 2004 were identified and classified by HIV status. Potential predictors of survival were evaluated using log-rank tests. Hazard ratios and 95% confidence intervals (CIs) were computed using a Cox proportional hazards regression model. The cohort included 1,732 (67.7%) HIV-negative patients and 825 (32.3%) HIV-positive patients. Median overall survival was 12 months (95% CI 10, 13) among HIV-negative patients. In this group, median survival increased over time, from 7.5 months (95% CI 6, 14) for patients diagnosed in the 1970s, to 14 months (95% CI 11, 20) for patients diagnosed in the 2000s. Independent predictors of mortality included older age (hazard ratio [HR] 1.03 [95% CI 1.02, 1.03]), earlier year of diagnosis (HR 0.98 [95% CI 0.98, 0.99]), male sex (HR 1.20 [95% CI 1.08, 1.34), married status (HR 0.70 [95% CI 0.63, 0.78]), and receipt of radiation therapy (HR 0.69 [95% CI 0.61, 0.77]). HIV positivity was a powerful adverse prognostic factor in the overall cohort (HR 4.55 [95% CI 4.01, 5.16]). Despite treatment advances, survival among PCNSL patients in the United States remains poor. However, in the subset of PCNSL patients who are HIV-negative, survival has improved over time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary central nervous system lymphoma (PCNSL) is a rare extra-nodal non-Hodgkin’s lymphoma (NHL) that involves the brain, spinal cord, meninges, and eyes. Approximately 2,000 cases are diagnosed annually in the United States [1]. Although the incidence is declining in patients with human immunodeficiency virus (HIV) [2], most data demonstrate an increasing incidence among immunocompetent adults. Reasons for the rising incidence are unclear but may include improved diagnosis with ascertainment bias [3].
PCNSL is sensitive to both radiation and chemotherapy. Unfortunately, this treatment sensitivity has not translated into high rates of disease control or cure [3]. This is unexpected since the cure rate of localized extranodal systemic NHL is approximately 70%. Untreated, PCNSL is a rapidly fatal neoplasm. Traditionally, whole brain radiation therapy (WBRT) has been the treatment of choice, with median survival of approximately 1 year [4]. The combination of WBRT with chemotherapy is limited by high rates of neurotoxicity, particularly in patients over 60 years of age [5]. This is an important obstacle because the median age of diagnosis is 60 years old [1]. Clinical trials during the 1990s demonstrated that high-dose methotrexate (MTX)-based chemotherapy regimens are active against PCNSL with high response rates and prolongation of survival. Median survival is reported in the range of 14 months to 5 years, depending on the specific population studied and the regimen used [6]. There is no standard-of-care for PCNSL, but there is a consensus that optimal therapy includes MTX with or without additional chemotherapy agents, possibly followed by WBRT [6]. There is similarly no standard approach to the treatment of HIV-associated PCNSL. Effective approaches may include MTX-based chemotherapy, radiation therapy, and highly-active anti-retroviral therapy in the absence of specific anti-tumor treatment [6].
Few studies have evaluated the use of MTX-based treatment regimens in the community. In a study of 579 patients older than 65 years of age with PCNSL diagnosed between 1994 and 2002 and identified from Surveillance, Epidemiology, and End Results (SEER) cancer registry data linked with Medicare claims, 20% of patents received no treatment. Of those who received treatment, radiation therapy alone was the most common approach (46%), followed by combination therapy (33%) and chemotherapy alone (22%) [7]. These data suggest that failure of patients in the community to receive optimal therapy may explain why population-based data have not consistently identified an improvement in survival over time [8]. Among 1,565 diagnosed in the United States from 1975 to 1999, there was no survival trend over time [9]. Similar findings were reported in 122 Canadian patients from 1990 to 2003 [10] and 98 Norwegian patients from 1989 to 2003 [11]. However, 739 Japanese patients diagnosed between 1985 and 2004 did demonstrate improved survival over time [12]. Patients diagnosed in the intervals from 1985 to 1994, 1995 to 1999, and 2000 to 2004 had median survival of 18, 29, and 24 months, respectively. Independent comparisons of the two more recent intervals to the oldest interval yielded statistically significant survival differences. Additionally, among HIV-positive patients with PCNSL, those diagnosed between 1997 and 2002 had prolonged survival compared to those diagnosed between 1994 and 1996 [13]. Given increasing awareness of the value of MTX-based chemotherapy in treating PCNSL patients in the United States, we hypothesized that PCNSL patients diagnosed more recently have a survival advantage over patients diagnosed further in the past.
Materials and methods
Cases were identified from the SEER database of the National Cancer Institute from 1973 to 2006 who had NHL subtypes (ICD-O-3 histology codes 9590, 9591, 9670-9699, 9701-9705, 9714, 9719, 9727-9729) confined to the CNS (ICD-O-3 topography codes C70.0-C72.9). To examine a homogenous study population and to reduce the probability of including individuals with metastatic lesions, subjects were excluded if PCNSL was not the first primary cancer. Subjects were also excluded if the case was identified from autopsy or death certificate data.
In addition to topography and histology, information on sex, race, age, marital status, radiation therapy, and year of diagnosis was available. In order to protect patient confidentiality, the SEER registry does not make information about chemotherapy available to researchers. Surgery information was not reviewed because its role in PCNSL therapy is limited to biopsy for tissue diagnosis. Because there is a major prognostic difference between HIV-associated PCNSL and the same disease in immunocompetent patients, we attempted to identify subjects with HIV-associated PCNSL and exclude them from the primary analysis. The SEER database does not report HIV status but provides cause-of-death data. Patients who died of HIV or “other infectious and parasitic diseases” are classified under SEER cause-of-death code 50040. For this analysis, patients with cause-of-death code 50040 were assumed to have HIV and are referred to as HIV-positive. This is similar to the approach taken by others in a recent SEER analysis [9]. We also classified patients with Kaposi’s sarcoma, a common AIDS-associated malignancy, as HIV-positive. All other patients were assumed to be immunocompetent and are referred to as HIV-negative. Because our approach was less robust in identifying patients living with HIV, as compared with patients who had died with HIV, we excluded cases diagnosed in 2005 and 2006. This decision ensured that fewer than 10% of subjects were alive at the time of analysis.
Race was defined according to categories of White and non-White, because of small sample sizes in subdivisions of the non-White category. Marital status was dichotomized as currently married or not currently married. Age and year of diagnosis were used as continuous variables in the proportional hazards model. For stratified log-rank tests, age was categorized as 0–39, 40–59, and ≥60 years old, and year of diagnosis was categorized by decade. Radiation therapy was dichotomized as received or not received. The primary outcome variable was time to death as measured in months.
Differences between the HIV-positive and HIV-negative cohorts were evaluated using Wilcoxon tests for continuous data and Chi square or Fisher’s exact tests for categorical data. Kaplan–Meier product limit curves were constructed and stratified by potentially relevant predictors of survival. This approach was not used in the HIV-positive cohort because of the marked homogeneity of the cohort with respect to predictors of survival. Differences in survival were evaluated with log-rank tests. Hazard ratios were computed using a Cox proportional hazards regression model [14]. All analyses were completed using the SAS statistical software package (version 9.1.3). Statistical tests were two-tailed with type one error of 0.05.
Results
Patient characteristics
There were 3,057 cases of primary CNS NHL diagnosed between 1973 and 2004 in the SEER database. Of these, 104 were excluded from the analysis because they were identified at death. Of the remaining 2,953 cases, 396 were excluded because NHL was not the first primary cancer. The remaining 2,557 cases were included in the analysis. Subject characteristics are summarized in Table 1. Of the total, 1,732 (67.7%) patients were classified as HIV-negative and 825 (32.3%) as HIV-positive. Median age was 52 years (interquartile range 38–68 years). The HIV-negative cohort was substantially older than the HIV-positive cohort (median ages 63 and 37 years, respectively; P < 0.0001). The large majority of subjects were diagnosed in 1980 or later.
In the HIV-negative cohort, 55.3% of subjects were male, whereas 91.8% of subjects in the HIV-positive cohort were male (P < 0.0001). The race distribution also differed between the cohorts. In the HIV-negative cohort, only 12.7% of subjects were classified as non-White, as compared to 30.7% of subjects in the HIV-positive cohort (P < 0.0001). While most of the HIV-negative subjects were married at the time of diagnosis (61.2%), most of the HIV-positive subjects were unmarried (89.4%; P < 0.0001). The large majority of cases occurred in the brain. Relatively few occurred in the meninges, cranial nerves, or spine. More HIV cases were reported to the San Francisco-Oakland registry (40.1%) than to any other registry. The next largest number of cases was reported to the Atlanta registry (14.4%). Among HIV-negative subjects, the largest numbers of cases were reported to registries in Detroit (18.5%), San Francisco-Oakland (18.0%), Connecticut (15.7%), Seattle (13.6%), and Iowa (13.5%). The largest proportion of cases was identified in the 1990s; this decade accounted for 82.6% of HIV-associated cases compared to 47.2% of HIV-negative cases, likely due to an increase in the geographic areas covered by SEER during this time. Causes of death in the full cohort were coded as HIV (32.3%), non-Hodgkin’s lymphoma (39.0%), brain tumor (5.3%), other neoplasms (2.5%), cardiac or cerebrovascular disease (3.2%), and other (2.8%). At the time of reporting to SEER, 239 patients were alive (9.4%).
Radiation trends
The likelihood of receiving radiation therapy was approximately one-third in both HIV-positive and HIV-negative cohorts. There was a decrease in the proportion of subjects who received radiation therapy over time (Table 2; P < 0.0001). In the 1970s and 1980s, approximately three-quarters of subjects received radiation, whereas approximately half of subjects received radiation between 2000 and 2004. This trend was apparent in both HIV-negative (P < 0.0001) and HIV-positive (P = 0.008) cohorts.
Survival
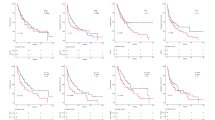
For the HIV-negative cohort, median survival was 12 months (95% CI 10, 13), and for the HIV-positive cohort, 2 months (95% CI undetermined; Fig. 1). The remaining survival analyses were performed in the HIV-negative cohort only (Table 3). Median survival increased over time (P = 0.0001) from 7.5 months (95% CI 6, 14) for patients diagnosed in the 1970s, to 14 months (95% CI 11, 20) for patients diagnosed in the 2000s (Fig. 2). Significant predictors of mortality in unadjusted analyses included White race (11 months [95% CI 9, 13] compared to 17 months [95% CI 12, 15]), older age (7 months [95% CI 6, 9] in the ≥60 years category compared to 15 months [95% CI 10, 22] in the 0–39 years category and 27 months [95% CI 23, 26] in the 40–59 years category), married status (14 months [95% CI 12, 16] compared to 8 months [95% CI 6, 10]), and receipt of radiation therapy (14 months [95% CI 13, 17] compared to 3 months [95% CI 3, 4]). Results of multivariable modeling are presented in Table 4. Independent predictors of mortality included older age (hazard ratio (HR) 1.03 [95% CI 1.02, 1.03]), earlier year of diagnosis (HR 0.98 [95% CI 0.98, 0.99]), male sex (HR 1.20 [95% CI 1.08, 1.34]), married status (HR 0.70 [95% CI 0.63, 0.78]), and receipt of radiation therapy (HR 0.69 [95% CI 0.61, 0.77]). HIV positivity was a powerful adverse prognostic factor in the overall cohort (HR 4.55 [95% CI 4.01, 5.16]). Results were unchanged when age and year of diagnosis were entered into the multivariable model in categorical fashion.
Discussion
These are the first population-based data collected in the United States to demonstrate an improvement in survival over time for HIV-negative patients with PCNSL. This study also confirms the value of well-known predictors of survival including age, receipt of radiation therapy, and HIV status. Additionally, the data indicate that male sex is a relatively weak but significant predictor of reduced overall survival in PCNSL. As has been observed for systemic cancers [15] and other brain tumors [16], we found that patients who are married at diagnosis have favorable survival compared to their unmarried counterparts.
A possible explanation for improving survival over time is increasing use of methotrexate-based chemotherapy regimens, although we cannot specifically examine that hypothesis as the data do not include information on chemotherapy. Alternatively, increases in survival with time could be attributed to improved supportive care or increasing rates of aggressive treatment. These data do not permit us to specifically investigate these possibilities.
As others have reported [9], we found that the proportion of patients receiving radiation therapy has declined over time. This trend was apparent in both HIV-positive and HIV-negative cohorts. Presumably this reflects increasing awareness of the fact that the combination of radiation therapy with chemotherapy is neurotoxic, particularly among patients over the age of 60 years, who represent approximately half of the PCNSL population. As anticipated, our data showed survival prolongation for radiation therapy in HIV-positive and HIV-negative patients over the age of 60 years (data not shown).
These data confirm the generally recognized fact that PCNSL is associated with poor survival. Even in the most recent decade, median survival for immunocompetent patients is only 14 months in the SEER cohort. Patients with HIV-associated PCNSL have dismal median survival of 2 months. Although clinical trial data and retrospective studies from academic medical centers have reported much higher median survival numbers [17–20], these population-based data may accurately reflect PCNSL-associated outcomes in the community.
These conclusions must be interpreted in the context of the known limitations of the study. Among the most important of these is the failure of SEER data to capture potentially important prognostic information related to chemotherapy, comorbidities, performance status, and socioeconomic status. Our effort to identify patients with HIV used approaches that were previously reported [9, 21]. Although there are no better methods, these have inherent flaws. Because the SEER cause-of-death classification has combined HIV with “other infectious and parasitic diseases,” some of the subjects classified here as HIV-positive were likely misclassified. In addition, this classification scheme relies primarily on causes of death. As a result, most of the patients who were alive at the time of SEER registry reporting (n = 239; 9.4%) are classified here as HIV-negative. In order to limit the number of patients for whom HIV status misclassification was possible, we restricted the analysis to patients in the SEER database diagnosed in or before 2004.
The inability to accurately classify HIV patients in the SEER data has the potential to introduce bias. If the HIV-negative cohort includes a significant number of HIV-positive patients, improved survival over time could reflect advances in HIV treatment. The observation that survival in the HIV-negative cohort is slightly lower in the 1990s (when the prevalence of HIV was highest) than in the 1980s raises a concern about contamination of the HIV-negative cohort with HIV-positive patients. In addition to random misclassification, improvements over time in the accuracy with which the SEER database classifies HIV infection could also lead to an inaccurate conclusion of improved survival over time. There are no published data that specifically address this possibility. A recent report from the San Diego/Orange County cancer registry found that HIV patients were accurately classified in the large majority of cases [22], although this finding may not apply to the SEER data.
We considered repeating the analysis after excluding all patients who were alive but ultimately opted against this approach. Because our primary objective was to evaluate survival trends over time, and most of the living patients were diagnosed in the current decade, this would have substantially decreased the statistical power of the study. Furthermore, because HIV-positive patients with PCNSL have much shorter survival than HIV-negative patients, the misclassification of living HIV-positive patients as HIV-negative would tend to falsely reduce survival in the 2000–2004 cohort. Therefore, the finding that survival has increased over time seems likely to be accurate, and the magnitude of the difference may be an underestimate.
In summary, these data indicate that survival rates for HIV-negative patients diagnosed with PCNSL in the United States are improving over time. This result differs with a 2005 report that examined an earlier version of the SEER data ending in 1999 [9]. We suspect that increased use of methotrexate-based chemotherapy regimens accounts for increasing survival over time. Future studies using datasets that capture provision of chemotherapy are required to specifically test this hypothesis.
References
CBTRUS (2008) Statistical report: primary brain tumors in the United States, 2000–2004. Published by the Central Brain Tumor Registry of the United States
Hoffman S, Propp JM, McCarthy BJ (2006) Temporal trends in incidence of primary brain tumors in the United States, 1985–1999. Neuro Oncol 8:27–37
Abrey LE (2009) Primary central nervous system lymphoma. Curr Opin Neurol, 2009 [Epub ahead of print]
Nelson DF, Martz KL, Bonner H, Nelson JS, Newall J, Kerman HD, Thomson JW, Murray KJ (1992) Non-Hodgkin’s lymphoma of the brain: can high dose, large volume radiation therapy improve survival? Report on a prospective trial by the Radiation Therapy Oncology Group (RTOG): RTOG 8315. Int J Radiat Oncol Biol Phys 23:9–17
Abrey LE, Correa DD (2005) Treatment-related neurotoxicity. Hematol Oncol Clin North Am 19:729–738 viii
Morris PG, Abrey LE (2009) Therapeutic challenges in primary CNS lymphoma. Lancet Neurol 8:581–592
Panageas KS, Elkin EB, Ben-Porat L, Deangelis LM, Abrey LE (2007) Patterns of treatment in older adults with primary central nervous system lymphoma. Cancer 110:1338–1344
Abrey LE, Panageas KS (2006) Identifying and addressing barriers to the delivery of optimal therapy for primary central nervous system lymphoma in the broader community. Leuk Lymphoma 47:2449–2452
Panageas KS, Elkin EB, DeAngelis LM, Ben-Porat L, Abrey LE (2005) Trends in survival from primary central nervous system lymphoma, 1975–1999: a population-based analysis. Cancer 104:2466–2472
Shenkier TN, Voss N, Chhanabhai M, Fairey R, Gascoyne RD, Hoskins P, Klasa R, Morris J, O’Reilly SE, Pickles T, Sehn L, Connors JM (2005) The treatment of primary central nervous system lymphoma in 122 immunocompetent patients: a population-based study of successively treated cohorts from the British Colombia Cancer Agency. Cancer 103:1008–1017
Haldorsen IS, Krossnes BK, Aarseth JH, Scheie D, Johannesen TB, Mella O, Espeland A (2007) Increasing incidence and continued dismal outcome of primary central nervous system lymphoma in Norway 1989–2003 : time trends in a 15-year national survey. Cancer 110:1803–1814
Shibamoto Y, Ogino H, Suzuki G, Takemoto M, Araki N, Isobe K, Tsuchida E, Nakamura K, Kenjo M, Suzuki K, Hosono M, Tokumaru S, Ishihara S, Kato E, Ii N, Hayabuchi N (2008) Primary central nervous system lymphoma in Japan: changes in clinical features, treatment, and prognosis during 1985–2004. Neuro Oncol 10:560–568
Kreisl TN, Panageas KS, Elkin EB, Deangelis LM, Abrey LE (2008) Treatment patterns and prognosis in patients with human immunodeficiency virus and primary central system lymphoma. Leuk Lymphoma 49:1710–1716
Cox DR (1972) Regression models and life tables. J R Stat Soc[B] 34:187–202
Goodwin JS, Hunt WC, Key CR, Samet JM (1987) The effect of marital status on stage, treatment, and survival of cancer patients. JAMA 258:3125–3130
Chang SM, Barker FG II (2005) Marital status, treatment, and survival in patients with glioblastoma multiforme: a population based study. Cancer 104:1975–1984
Ferreri AJ, Dell’Oro S, Foppoli M, Bernardi M, Brandes AA, Tosoni A, Montanari M, Balzarotti M, Spina M, Ilariucci F, Zaja F, Stelitano C, Bobbio F, Corazzelli G, Baldini L, Ponzoni M, Picozzi P, Caligaris Cappio F, Reni M (2006) MATILDE regimen followed by radiotherapy is an active strategy against primary CNS lymphomas. Neurology 66:1435–1438
Hoang-Xuan K, Taillandier L, Chinot O, Soubeyran P, Bogdhan U, Hildebrand J, Frenay M, De Beule N, Delattre JY, Baron B (2003) Chemotherapy alone as initial treatment for primary CNS lymphoma in patients older than 60 years: a multicenter phase II study (26952) of the European Organization for Research and Treatment of Cancer Brain Tumor Group. J Clin Oncol 21:2726–2731
Zhu JJ, Gerstner ER, Engler DA, Mrugala MM, Nugent W, Nierenberg K, Hochberg FH, Betensky RA, Batchelor TT (2009) High-dose methotrexate for elderly patients with primary CNS lymphoma. Neuro Oncol 11:211–215
Shah GD, Yahalom J, Correa DD, Lai RK, Raizer JJ, Schiff D, LaRocca R, Grant B, DeAngelis LM, Abrey LE (2007) Combined immunochemotherapy with reduced whole-brain radiotherapy for newly diagnosed primary CNS lymphoma. J Clin Oncol 25:4730–4735
Pulido JS, Vierkant RA, Olson JE, Abrey L, Schiff D, O’Neill BP (2009) Racial differences in primary central nervous system lymphoma incidence and survival rates. Neuro Oncol 11:318–322
Diamond C, Taylor TH, Im T, Wallace M, Saven A, Anton-Culver H (2007) How valid is using cancer registries’ data to identify acquired immunodeficiency syndrome-related non-Hodgkin’s lymphoma? Cancer Causes Control 18:135–142
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Norden, A.D., Drappatz, J., Wen, P.Y. et al. Survival among patients with primary central nervous system lymphoma, 1973–2004. J Neurooncol 101, 487–493 (2011). https://doi.org/10.1007/s11060-010-0269-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-010-0269-7