Abstract
Background and Purpose In patients already suffering from cancer, the additional occurrence of stroke can aggravate the burden of the disease. The purpose of this study was to compare risk factors for haemorrhagic and ischemic strokes in cancer and non-cancer patients. Methods A retrospective analysis, including 1,274 stroke patients admitted to a stroke unit, was conducted from 2004 to 2007. Classical risk factors for stroke and clinical outcome measures were compared between cancer and non-cancer patients. Results Twelve percent of stroke patients had an additional diagnosis of cancer. In the non-cancer population, 84% had ischemic and 16% had haemorrhagic strokes. In cancer patients, 86% had ischemic and 14% had haemorrhagic strokes. Vascular risk factors in cancer patients, including hypertension, atrial fibrillation, coronary vessel disease, smoking, hypercholesterolemia and diabetes mellitus, showed no difference compared to the non-cancer population. Only thrombotic events occurred more often in the cancer cohort. The most frequent cancer types were urogenital, breast and gastrointestinal. Regarding clinical outcome, cancer patients had an inferior neurological condition at discharge and a trend towards a longer stay in the stroke unit. Conclusions The frequency of ischemic and haemorrhagic stroke in tumour patients is similar to that in the non-cancer population. Cerebrovascular risk factors do not significantly vary between cancer and non-cancer patients. The higher frequency of thrombotic events in cancer patients may reflect a coagulation disorder, commonly found in patients with malignancy. Clinical outcome in cancer patients may be worsened by the pre-existent co-morbidity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebrovascular disorders are the most frequent neurological disease and cancer is the second most frequent cause of death in the industrial world. From the neurologist’s point of view, however, stroke is a less frequent neurological complication in cancer patients, as compared to metastases or neurotoxicity of anticancer treatment [1].
However, according to an autopsy study [2], cerebrovascular ischemic infarcts occur in a large number of cancer patients. The clinical significance of these findings is not clear, as the range includes silent infarcts and diffuse vascular encephalopathies. In the literature, the incidence of stroke in cancer patients is quoted as being a common neurological complication [2–4].
Cerebral haemorrhages have been reported more frequently, especially in haematological malignancies. In patients with leukaemia and lymphoma, 72% and 36% of strokes, respectively, were haemorrhagic [5].
Evaluations based on stroke criteria [6] and common risk factors, such as hypertension, diabetes mellitus, hyperlipidemia, coronary vessel disease and smoking, suggest a more even distribution between cancer- and non-cancer-related strokes [7–10].
Beside the classical risk factors for stroke, several cancer-specific types and causes of stroke, such as direct tumour effects, coagulation disorders, intravascular coagulation, infection, septic thrombi and therapeutic and diagnostic procedures, have to be considered. These additional factors have not been analysed in the present study.
The purpose of this study was to investigate the occurrence of ischemic and haemorrhagic stroke, and to compare classical risk factors and clinical outcome measures in patients with cancer and stroke versus non-cancer patients with stroke.
Methods
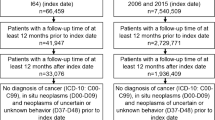
Patients admitted between 2004 and 2007 to the stroke unit of the KFJ-Hospital in Vienna, a teaching hospital of the Medical University of Vienna, were included in the study, using data from the facility’s computerised database. Analysis was performed according to an anonymous protocol. Patients had to sign a general informed consent on admission, which includes medical data processing.
Our stroke unit takes the form of an intermediate care setting. After acute admission and acute diagnosis and treatment, patients are transferred to normal care and rehabilitation units. Patients were identified according to the ICD 10 classification for stroke and cancer. The study followed stringent criteria for stroke diagnosis, including only patients with computer tomography of the brain (CCT) or magnetic resonance imaging (MRI) of the brain showing a new vascular lesion according to neurological signs and symptoms. Patients with possible stroke, negative CCT or MRI of the brain or TIA-like (transient ischemic attack) syndromes were excluded. Each patient record was reviewed separately in order to obtain detailed information. The analysis protocol included age, gender, history of cancer and risk factors for stroke, such as hypertension, atrial fibrillation, diabetes mellitus, coronary vessel disease, smoking, hypercholesterolemia and history of thrombosis (deep vein thrombosis, pulmonary embolism). Etiological evaluations for stroke were based on the TOAST (Trial of Org 10172 in Acute Stroke Treatment) criteria [6].
Routine examinations in all stroke patients included electrocardiogram, CCT, MRI—in most cases including T1-, T2-weighted images, echo planar imaging, and the apparent diffusion coefficient, laboratory tests (routine haematology and biochemistry including cardial enzymes, and coagulation parameters), neurological and physical examination, and patients’ medical history and medication.
We also considered length of stay in the stroke unit, and NIHSS (National Institute of Health Stroke Scale) score at admission and discharge from the stroke unit. The cancer cohort included patients with known cancer and with newly diagnosed cancer at the time of stroke. Cancer-related data, such as prior anti-cancer treatment and time of cancer diagnosis, were taken from patient files. Patients with cerebral metastases initially considered as stroke were excluded from the study, as were strokes in cancer patients where the cause of stroke was directly related to a primary brain tumour or associated treatment (neurosurgical procedure, radionecrosis, gamma knife treatment, etc.). Patients admitted to the stroke unit with diagnoses other than stroke were excluded.
Data analysis
The standard version of the SPSS statistical package for Windows 12.0G was used for data evaluation. Analysis of differences in the frequency of categorical variables was performed using the chi-square test. The Mann–Whitney U test was used to compare ordinal data between cancer and non-cancer patients. The reported P values are the results of two-sided tests. A P value <0.05 was considered statistically significant.
Results
In total, 1,274 consecutive patients with stroke, admitted to our stroke unit, were assessed for type of stroke, common risk factors for stroke, and clinical outcome measures. During the investigation period, 191 patients were admitted with diseases other than stroke, and were excluded from the analysis.
The median age in cancer patients with stroke was 68.1 years (range: 28–96 years) and 66.9 years (range: 31–93 years) in non-cancer patients. Fifty-eight percent of cancer patients with stroke were males compared to 53% males in the non-cancer group.
Of all the stroke patients, 153 (12%) had an additional diagnosis of cancer. In cancer patients, 86% had ischemic and 14% had haemorrhagic strokes. In the non-cancer population, 84% had ischemic and 16% had haemorrhagic strokes. According to the TOAST criteria, there was no statistically significant difference between cancer and non-cancer patients with respect to the subtypes of ischemic strokes (Table 1).
Vascular risk factors in cancer patients, including hypertension, atrial fibrillation, coronary vessel disease, smoking, diabetes mellitus and hypercholesterolemia, showed no statistically significant difference compared to the non-cancer population. Only thrombotic events [deep vein thrombosis (DVT) and pulmonary embolism (PE)] yielded a statistically significant difference (Table 2).
Echocardiography was performed in 57% of patients with stroke and cancer and in 61% of non-cancer stroke patients. Valvular vegetations without clinical and laboratory signs of infection were detected in only ten patients (three cancer and seven non-cancer patients), and retrospectively classified as non-thrombotic endocarditis (NBTE). Only four non-cancer patients had transoesophageal echocardiography; all other patients received transthoracic echocardiography.
The most frequent cancer types associated with stroke were urogenital, breast, gastrointestinal, haematological and lung. Haematological malignancies, lung cancer and melanoma had the highest proportion of haemorrhagic strokes (Table 3). In four patients (two lung cancer, one ovarian cancer and one patient with CLL) the cancer was diagnosed at the time of the stroke. In cancer patients with haemorrhagic strokes, thrombocytopenia was present in nine patients (41%). According to the NCI-CTC criteria, six patients had grade I thrombocytopenia and three grade II thrombocytopenia. Whereas in non-cancer patients with haemorrhagic strokes, only seven patients (4%) with thrombocytopenia (NCI-CTC grade I) could be detected. One patient (NHL) had a multilocular occipital and mid brain bleeding, and eight patients had basal ganglia and thalamus haemorrhages in a rather classic distribution normally seen in hypertensive haemorrhagic strokes. In 18 patients (77%), the haemorrhage occurred during progressive cancer disease or during anticancer treatment.
The median NIHSS on admission in stroke patients with cancer was seven, compared to six in the non-cancer cohort, but the difference did not reach statistical significance. Conversely, at discharge, patients with cancer and stroke had a significantly worse NIHSS than the non-cancer patients (eight vs five) (Table 4). Analysing the NIHSS according to different cancer entities, lung cancer, urogenital cancers and breast cancer patients exhibited the most pronounced neurological deterioration at discharge (Table 5).
Out of 942 patients with ischemic stroke, 89 underwent thrombolysis (9%). From 131 cancer patients, 7 received thrombolysis (5%).
The median length of stay at the stroke unit was 3.6 days for the non-cancer patients and 3.9 days for the cancer patients. The difference did not reach statistical significance. Four cancer patients (3%) and 19 (2%) non-cancer patients died during their stay at the stroke unit.
Discussion
This study highlights the relationship between two common diseases of stroke and cancer. Analysis of classical risk factors concerning cerebrovascular disease showed a similar distribution in cancer patients with stroke as compared to non-cancer patients with stroke. Only thrombotic events occurred more often in cancer patients with stroke than in non-cancer patients with stroke.
Some papers have stated that classical risk factors are not as important as factors attributed to the cancer, such as direct tumour effects, coagulation disorders, infection, and therapeutic and diagnostic procedures [2]. Two large clinical studies by Cestari [10], and Zhang [11] found no significant differences in classical vascular risk profile between cancer patients and a series of stroke patients. In our study, only thrombotic events occurred statistically more often in cancer patients than in the non-cancer cohort. There were also fewer patients with atrial fibrillation in the cancer population, although statistical significance was not reached. Similar results were found by Cestari et al. [10].
Some contradictory results are reported in the literature regarding epidemiological data on stroke in cancer patients. Some authors quote stroke as a common neurological complication in cancer patients [2–4], while others, including review articles, tend to describe a lack of significant difference regarding the frequency of stroke for both groups [10–12]. As compared to most of the previous studies, the present investigation is strengthened by inclusion of modern imaging techniques, clinical and neurological stroke criteria adopted by a specialised stroke unit, and by the distinction between ischemic and haemorrhagic strokes.
In our study, the overall frequency of ischemic and haemorrhagic stroke was similar in both groups. However, there was a high proportion of ischemic strokes (96% ischemic vs 4% haemorrhagic strokes) in patients with gastrointestinal cancers (Table 3). At least for gastric cancer and colorectal cancer, no increased risk for strokes was reported by Lindvig et al. [4] and Kune et al. [13]. These studies did not, however, differentiate between ischemic and haemorrhagic.
Besides chemotherapy-related increased risks for ischemic stroke, such as cisplatin-based chemotherapy, cyclophosphamide, 5 FU, taxol, paclitaxel l-asparaginase and tamoxifen, no specific malignancies have been reported to cause ischemic strokes more often than others [14–19]. Generally, the risk of chemotherapy-induced stroke seems low and not highly influenced by the histological type of cancer [20]. Therefore, the high proportion of ischemic stroke in gastrointestinal tumours in our series remains unclear and may be due to the small sample size. In addition, the distribution of primary malignancies, most commonly urogenital, gastrointestinal and breast, does not reflect the incidence of these tumours and may be attributed to a referral bias [21].
It is postulated that distinct mechanisms initiated by the cancer cause coagulopathy, by activation of the coagulation system through inflammation and/or procoagulants. The acquired prothrombotic state is argued to be associated with an increased risk for ischemic stroke [22, 23]. This assumption is in line with our findings of significantly more thrombotic events in cancer patients with ischemic strokes, which may be interpreted as a clinical sign for a coagulation disorder. Nonetheless, this was not reflected by a higher frequency of strokes in our cancer population.
It is assumed that the most common single cause of ischemic stroke in cancer patients is NBTE [2, 24] yet only 59% of patients with NBTE in a large autopsy series of 171 cases suffered from malignancy [25]. It can be associated with any type of cancer, but seems to be more frequent in adenocarcinoma, particularly pancreatic carcinoma, mucin-producing carcinomas of the lung or gastrointestinal tract, and lymphoma [26–29]. The low proportion of patients with NBTE (1%) in our study seems under-represented, but similar infrequent findings of NBTE were also reported in the paper by Cesatri, with 3% [10]. In our survey, this finding might be due to the relatively low proportion of echocardiography performed in the study population, or to the strict criteria regarding additional signs of infection, or to imaging results showing multiple infarcts [29–33].
In our series, no major differences were detected between cancer and non-cancer patients with respect to subtypes of stroke, based on the TOAST classification. Cestari [10] and Zhang [11], who also analysed stroke etiologies by means of TOAST criteria, reported fewer patients with large vessel atherosclerosis (21% in Zhang’s series vs 10% in Cestari’s) than the 41% observed in our study. Results were more similar to our findings for cardio-embolism and small vessel disease (see also Table 1). The reason for the discrepancy in the frequency of large vessel disease may be the ambiguous classification of stroke types according to clinical and radiological parameters. The standardised workup performed in our specialised cerebrovascular unit may explain the more comparable frequencies of different stroke etiologies in our patient groups, as seen in a large series of stroke patients [34].
Cerebral haemorrhages seem to occur more often in patients with haematological malignancies and in lung cancer [3, 35, 36]. These reports may be confirmed in our study, as the highest frequencies for haemorrhagic strokes were found for haematological malignancies and lung cancer. In the paper by Zhang [11], there was an increased risk for haemorrhagic strokes in the cancer population, which was attributed to several factors, such as chemotherapy-induced thrombocytopenia, disseminated intravascular coagulopathy (DIC) and other coagulation disorders. In our study, thrombocytopenia occurred more often in the cancer population. However, the pathophysiological mechanism of intracerebral haemorrhages in cancer patients, which is generally attributed to a coagulopathy, is a matter of discussion and cannot be attributed to thrombocytopenia alone [2, 37]. At least for leukaemia and lymphoma, the coagulopathy is typically acute DIC or thrombocytopenia or hyperviscosity that can lead to systemic and brain haemorrhage [3, 12, 36, 37].
Outcome measures exhibited significant higher neurological impairment in cancer patients with stroke at time of discharge. Lung and urogenital cancers showed the most pronounced neurological deterioration at discharge, but these two groups also showed the highest median age. A clear clustering for any cancer entity with a worse outcome could not be detected. However, the sample size concerning each tumour was small.
Further, patients with stroke and cancer had a tendency to stay longer at the stroke unit than non-cancer patients. These results may be explained by the generally impaired general health of cancer patients and by the concurrence of two severe diseases, although there is currently a lack of evidence to support this point [10, 11, 18, 24, 28].
The lower proportion of thrombolysis in the cancer cohort may be attributed to the physicians’ concerns regarding possible haemorrhagic complications in cancer patients. However, related data are missing. Further investigations are warranted to evaluate the impact of thrombolysis in stroke patients with cancer.
The results of this study demonstrate that the overall frequency of ischemic and haemorrhagic stroke in cancer patients is similar to that of non-cancer patients. In addition, classical risk factors, except for thrombotic events, do not differ significantly between the two groups.
Based on these results, management of stroke in cancer patients should probably be based on general recommendations for stroke treatment and prevention. However, co-morbidity in cancer patients, such as thrombocytopenia, recent surgery and treatment with drugs that may increase the risk for intracerebral heemorrhage (heparin, anticancer drugs), have to be considered, especially in the case of thrombolysis. To date, no specific approach to patients with both stroke and cancer is known. This demands future research.
References
Clouston PD, DeAngelis LM, Posner JB (2006) The spectrum of neurological disease in patients with systemic cancer. Ann Neurol 31:268–273. doi:10.1002/ana.410310307
Graus F, Rogers LR, Posner JB (1985) Cerebrovascular complications in patients with cancer. Medicine (Baltimore) 64:16–35. doi:10.1097/00005792-198501000-00002
Posner JB (1995) Vascular disorders. In: Posner JB (ed) Neurologic complications of cancer. Davies, Philadelphia, pp 199–299
Lindvig K, Moller H, Mosbech J, Jensen OM (1990) The pattern of cancer in a large cohort of stroke patients. Int J Epidemiol 19:498–504. doi:10.1093/ije/19.3.498
Rogers LR (1994) Cerebrovascular complications in cancer patients. Oncology 8:23–30; Williston Park
The Publications Committee for the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) Investigators (1998) Low molecular weight heparinoid, ORG 10172 (danaparoid), and outcome after acute ischemic stroke: a randomized controlled trial. JAMA 279:1265–1272
Chaturvedi S, Ansell J, Recht L (1994) Should cerebral ischemic events in cancer patients be considered a manifestation of hypercoagulability? Stroke 25:1215–1218
Zhang YY, Cordato D, Shen Q, Sheng AZ, Hung WT, Chan DK (2006) Risk factor, pattern, etiology and outcome in ischemic stroke patients with cancer: a nested case-control study. Cerebrovasc Dis 23:181–187. doi:10.1159/000097639
Yashin AI, Ukraintseva SV, Akushevich IV, Arbeev KG, Kulminski A, Akushevich L (2008) Trade-off between cancer and aging: what role do other diseases play? Evidence from experimental and human population studies. Mech Ageing Dev :25. (Epub ahead of print)
Cestari DM, Weine DM, Panageas KS, Segal AZ, De Angelis LM (2004) Stroke in patients with cancer: incidence and aetiology. Neurology 64:2025–2030
Zhang YY, Chan DKY, Cordato D, Sheng AZ (2006) Stroke risk factor, pattern and outcome in patients with cancer. Acta Neurol Scand 114:378–383. doi:10.1111/j.1600-0404.2006.00709.x
Grisold W, Oberndorfer S, Struhal W (2009) Stroke and cancer: a review. Acta Neurol Scand 119:1–16. doi:10.1111/j.1600-0404.2008.01059.x
Kune GA, Kune S, Watson LF (2007) Colorectal cancer risk, chronic illnesses, operations and medications: case control results from the Melbourne Colorectal Cancer Study 1988. Int J Epidemiol 6:951–957. doi:10.1093/ije/dym193
Li SH, Chen WH, Tang Y, Rau KM, Chen YY, Huang TL et al (2006) Incidence of ischemic stroke post-chemotherapy: a retrospective review of 10,963 patients. Clin Neurol Neurosurg 108:150–156. doi:10.1016/j.clineuro.2005.03.008
Chan AT, Leung WT, Johnson PJ (1994) Cerebrovascular event following taxol infusion. Clin Oncol (R Coll Radiol) 6:202–203. doi:10.1016/S0936-6555(94)80062-6
Ohashi S, Yazumi S, Nishio A et al (2006) Acute cerebral infarction during combination chemotherapy with s-1 and cisplatin for a young patient with a mucin-producing adenocarcinoma of the stomach. Intern Med 45:1049–1053. doi:10.2169/internalmedicine.45.1720
Rollins N, Winick N, Bash R et al (2004) Acute methotrexate neurotoxicity: findings on diffusion-weighted imaging and correlation with clinical outcome. AJNR Am J Neuroradiol 25:1688–1695
Braithwaite RS, Chlebowski RT, Lau J, George S, Hess R, Col NF (2003) Meta-analysis of vascular and neoplastic events associated with tamoxifen. J Gen Intern Med 18:937–947. doi:10.1046/j.1525-1497.2003.20724.x
Bushnell CD, Goldstein LB (2004) Risk of ischemic stroke with tamoxifen treatment for breast cancer: a meta-analysis. Neurology 63:1230–1233
Rogers LR (2004) Cerebrovascular complications in patients with cancer. Semin Neurol 24:453–460. doi:10.1055/s-2004-861539
Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ (2007) Cancer statistics 2007. CA Cancer J Clin 57:43–66. doi:10.3322/canjclin.57.1.43
Hiatt BK, Lentz SR (2002) Prothrombotic states that predispose to stroke. Curr Treat Options Neurol 4:417–425. doi:10.1007/s11940-002-0009-1
Lee AY (2002) Cancer and thromboembolic disease: pathogenic mechanisms. Cancer Treat Rev 28:137–140. doi:10.1016/S0305-7372(02)00044-0
Rogers LR (2003) Cerebrovascular complications in cancer patients. Neurol Clin 21:167–192. doi:10.1016/S0733-8619(02)00066-X
Steiner I (1993) Nonbacterial thrombotic endocarditis-a study of 171 case reports. Cesk Patol 29:58–60
Gonzalez Quintela A, Candela MJ, Vidal C et al (1991) Non-bacterial thrombotic endocarditis in cancer patients. Acta Cardiol 46:1–9
Herrera dP, Esteban EE, Gimenez SJV, Pareja MA, Moscoso dP (2004) Nonbacterial thrombotic endocarditis as initial event of lung cancer. An Med Interna 21:495–497
Ojeda VJ, Frost F, Mastaglia FL (1985) Non-bacterial thrombotic endocarditis associated with malignant disease: a clinicopathological study of 16 cases. Med J Aust 42:629–631
Reisner SA, Brenner B, Haim N, Edoute Y, Markiewicz W (2000) Echocardiography in nonbacterial thrombotic endocarditis: from autopsy to clinical entity. J Am Soc Echocardiogr 13:876–881. doi:10.1067/mje.2000.106070
Singhal AB, Topcuoglu MA, Buonanno FS (2002) Acute ischemic stroke patterns in infective and nonbacterial thrombotic endocarditis: a diffusion-weighted magnetic resonance imaging study. Stroke 33:1267–1273. doi:10.1161/01.STR.0000015029.91577.36
Edoute Y, Haim N, Rinkevich D, Brenner B, Reisner SA (1997) Cardiac valvular vegetations in cancer patients: a prospective echocardiographic study of 200 patients. Am J Med 102:252–258. doi:10.1016/S0002-9343(96)00457-3
Daniels SK, Brailey K, Priestly DH, Herrington LR, Weisberg LA, Foundas AL (1998) Aspiration in patients with acute stroke. Arch Phys Med Rehabil 79:14–19. doi:10.1016/S0003-9993(98)90200-3
Ding R, Logemann JA (2000) Pneumonia in stroke patients: a retrospective study. Dysphagia 15:51–57
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EEIII (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41
Quinones-Hinojosa A, Gulati M, Singh V et al (2003) Spontaneous intracerebral haemorrhage due to coagulation disorders. Neurosurg Focus 14:11. doi:10.3171/foc.2003.14.6.11
Glass J (2006) Neurologic complications of lymphoma and leukaemia. Semin Oncol 33:342–347. doi:10.1053/j.seminoncol.2006.03.004
Nguyen T, DeAngelis LM (2006) Stroke in cancer patients. Curr Neurol Neurosci Rep 6:187–191. doi:10.1007/s11910-006-0004-0
Acknowledgment
This work was supported by funding from the European Community’s Sixth Framework Programme (Contract LSSM-CT-2005-518174). It reflects only the authors’ views and the Community is not liable for any use that may be made of the information contained herein.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s11060-009-9903-7
Rights and permissions
About this article
Cite this article
Stefan, O., Vera, N., Otto, B. et al. Stroke in cancer patients: a risk factor analysis. J Neurooncol 94, 221–226 (2009). https://doi.org/10.1007/s11060-009-9818-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-009-9818-3