Abstract
Aims
The goal of this study was to analyze cancer risk in stroke survivors followed for up to 10 years in general practices in Germany.
Methods
The current study sample included patients who received an initial stroke diagnosis in one of 1262 general practices in Germany between 2006 and 2015 (index date). Patients without stroke were matched (1:1) to patients with stroke by age, gender, index year, and 16 comorbidities diagnosed in the 12 months prior to the index date using a propensity score method. The main outcome of the study was the risk of cancer as a function of stroke within 10 years of the index date.
Results
The stroke and non-stroke groups included 9579 men and 9089 women. After 10 years of follow-up, 29.3% of men with stroke and 23.8% of those without stroke developed any of the included types of cancer (log-rank p value < 0.001). During the same time, the prevalence of cancer was 25.0% in women with stroke and 20.5% in women without stroke (log-rank p value < 0.001). There was a positive association between stroke and any cancer in men (hazard ratio [HR] = 1.18, 95% confidence interval [CI] 1.09–1.28) and in women (HR = 1.22, 95% CI 1.12–1.34). This association was significant for cancers of respiratory and intrathoracic organs in men and women and for cancers of digestive organs in men.
Conclusions
This study, including more than 37,000 patients from Germany, found that stroke was associated with an increased cancer risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In 2018, cancer was the second most common cause of death worldwide, and around 9.6 million people died because of cancer during this year (World Health Organization 2018). Cancer also has a major impact on patients’ quality of life (Medeiros et al. 2015), psychological well-being (Andrykowski et al. 2008), and physical comorbidities (Mao et al. 2007). In addition, this condition is associated with decreased ability to work (Munir et al. 2009) and substantial healthcare costs (Yabroff et al. 2011). Therefore, identifying additional risk factors for cancer is important, as it may be helpful in the development of new and effective preventive strategies.
Several studies have focused on the relationship between stroke and cancer in recent decades (Dearborn et al. 2014). For example, a nationwide follow-up study, including participants with and without cancer from Sweden, estimated that there was an increase in the risk of hemorrhagic and ischemic stroke within the first 6 months following a cancer diagnosis (Zöller et al. 2012). Interestingly, this risk decreased over time but remained significant even 10 years after the initial diagnosis of cancer. The association between cancer and stroke is likely mediated by hypercoagulability, venous-to-arterial embolism, nonbacterial thrombotic endocarditis, and direct tumor effects (Dearborn et al. 2014). By contrast, few authors have analyzed the rate of cancer in stroke survivors (Cocho et al. 2015; Qureshi et al. 2015; Selvik et al. 2015; Chen et al. 2017; Quintas et al. 2018). These previous works are subjected to several limitations [i.e., cross-sectional design (Cocho et al. 2015), non-inclusion of hemorrhagic stroke (Qureshi et al. 2015; Selvik et al. 2015), time-related bias (Chen et al. 2017), and insufficient follow-up (Qureshi et al. 2015; Quintas et al. 2018)], and it is unclear whether stroke is a long-term risk factor for cancer or only an early manifestation of the neoplastic disease.
Therefore, the goal of this study was to analyze cancer risk in stroke survivors followed for up to 10 years in general practices in Germany.
Methods
Database
This study is based on data from the Disease Analyzer database (IQVIA), which compiles drug prescriptions, diagnoses, basic medical and demographic data obtained directly and in anonymous format from computer systems used in the practices of general practitioners and specialists (Rathmann et al. 2018). Diagnoses (International Classification of Diseases, 10th revision [ICD-10]), prescriptions (Anatomical Therapeutic Chemical [ATC] Classification system), and the quality of reported data are being monitored by IQVIA based on a number of criteria (e.g., completeness of documentation, linkage between diagnoses and prescriptions).
In Germany, the sampling methods used for the selection of physicians’ practices were appropriate for obtaining a representative database of general and specialized practices (Rathmann et al. 2018). Prescription statistics for several drugs were very similar to the data available from pharmaceutical prescription reports. The age groups for given diagnoses in the Disease Analyzer database also corresponded to those in the relevant disease registries. Finally, this database has already been used in studies focusing on stroke (Jacob and Kostev 2017; Wiefarn et al. 2017) and cancer (Kostev et al. 2017, 2018).
Study population and variables
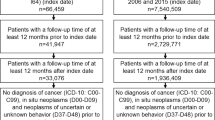
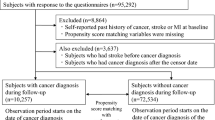
The current study sample included patients who received an initial stroke diagnosis (International Classification of Diseases, 10th edition [ICD-10]: I63, I64) at one of 1262 general practices in Germany between 2006 and 2015 (index date). Other types of nontraumatic hemorrhage in the brain (ICD-10: I60–I62), as hemorrhagic stroke is sometimes classified, were not included in this study. To guarantee the accuracy of the estimation of cancer incidence, the inclusion criteria were as follows: follow-up time of at least 12 months prior to the index date; follow-up time of at least 12 months after the index date; no diagnosis of cancer (C00–C99), in situ neoplasms (D00–D09), or neoplasms of uncertain or unknown behavior (D37–D48) prior to the index date; and age ≥ 18 years at the index date. After applying similar inclusion criteria, patients without stroke were matched (1:1) to patients with stroke, based on propensity scores using a greedy algorithm and derived from the logistic regression using age, gender, index year, and 16 comorbidities diagnosed in the 12 months prior to the index date. This regression did not include the identification number of general practices. The exact 16 comorbidities were certain infectious and parasitic diseases (A00–B99), benign neoplasms (D10–D36), diseases of the blood and blood-forming organs, and certain disorders involving the immune mechanism (D50–D89), endocrine, nutritional, and metabolic diseases (E00–E90), mental and behavioral disorders (F00–F99), diseases of the nervous system (G00–G99), diseases of the eye and adnexa (H00–H59), diseases of the ear and mastoid process (H60–H95), diseases of the circulatory system (I00–I99) excluding stroke (I63, I64), diseases of the respiratory system (J00–J99), diseases of the digestive system (K00–K93), diseases of the skin and subcutaneous tissue (L00–L99), diseases of the musculoskeletal system and connective tissue (M00–M99), diseases of the genitourinary system (N00–N99), congenital malformations, deformations, and chromosomal abnormalities (Q00–Q99), and injury, poisoning, and certain other consequences of external causes (S00–T98). The index date for participants without stroke was a randomly selected visit date between 2006 and 2015. A total of 18,668 patients with and 18,668 patients without stroke were included (Fig. 1).
Study outcome
The main outcome of the study was the risk of cancer (C00–C97) as a function of stroke within 10 years of the index date. The analyses included 13 cancers: cancer of lip, oral cavity, and pharynx (C00–C14), cancer of digestive organs (C15–C26), cancer of respiratory and intrathoracic organs (C30–C39), cancer of bone and articular cartilage (C40–C41), cancer of skin (C43–C44), cancer of mesothelial and soft tissue (C45–C49), cancer of breast (C50), cancer of female genital organs (C51–C58), cancer of male genital organs (C60–C63), cancer of urinary tract (C64–C68), cancer of eye, brain, and other parts of central nervous system (C69–C72), cancer of thyroid and other endocrine glands (C73–C75), and cancer of lymphoid, hematopoietic, and related tissue (C81–C96).
Statistical analyses
Descriptive analyses were obtained for all demographic and clinical variables, and mean ± SD were calculated for age. The cumulative incidence of any cancer in the stroke and non-stroke groups was calculated for up to 10 years after the index date using Kaplan–Meier curves in men and women separately. Patients were censored at the time of first cancer diagnosis or lost to follow-up, whichever occurred first. As there was no information on death, dead patients were considered as lost to follow-up in this study. Univariate Cox regression models were used to investigate the association between stroke and cancer in men and women. A p value of < 0.05 was considered statistically significant. The analyses were carried out using SAS 9.4.
Results
The stroke and non-stroke groups included 9579 men and 9089 women (Table 1). The mean age was 66.9 (SD = 11.9) years in men and 71.4 (SD = 13.0) years in women. After 10 years of follow-up, 29.3% of men with stroke and 23.8% of men without stroke developed any of the included types of cancer (log-rank p value < 0.001; Fig. 2). In women, the prevalence of cancer was 25.0% in women with stroke and 20.5% in women without stroke (log-rank p value < 0.001; Fig. 3). The difference in the prevalence of cancer in stroke survivors and controls was not significant after 1 year of follow-up in men (3.1% versus 2.6%; p value = 0.273) and in women (2.6% versus 2.1%; p value = 0.092). The results of the Cox regression models are displayed in Table 2. There was a positive association between stroke and any cancer in both men (hazard ratio [HR] = 1.18, 95% confidence interval [CI] 1.09–1.28) and women (HR = 1.22, 95% CI 1.12–1.34). This association was significant for two cancers in men (cancer of digestive organs: HR = 1.44, 95% CI 1.18–1.76; cancer of respiratory and intrathoracic organs: HR = 1.36, 95% CI 1.03–1.81) and for one cancer in women (cancer of respiratory and intrathoracic organs: HR = 2.95, 95% CI 1.75–4.95).
Discussion
This is one of the first observational studies investigating the long-term risk of cancer in stroke survivors. In this retrospective analysis including over 37,000 patients followed for up to 10 years in general practices in Germany, we observed that men and women with a history of stroke were at a higher risk for cancer compared to those without a history of stroke. This association was significant for cancers of the respiratory and intrathoracic organs in men and women, and for cancers of the digestive organs in men.
In recent years, several studies have focused on the prevalence of cancer in stroke survivors. Cocho et al. (2015) reported in 631 participants with acute ischemic stroke that 2.1% of the sample had occult malignancy. That same year, in an analysis of 3680 adults with non-disabling cerebral infarction, the age-adjusted annual rate of cancer was found to be higher in individuals with ischemic stroke than in the general population after one (standardized incidence ratio [SIR] = 1.2) and two years (SIR = 1.4) of follow-up (Qureshi et al. 2015). In 2018, Quintas and colleagues showed, in 381 ischemic stroke patients followed for 18 months, that approximately 7.6% of the sample developed cancer (Quintas et al. 2018). The authors further estimated that there was an average of 6 months between stroke onset and cancer diagnosis. The most frequent locations of the cancer were the colon (24.1%), lung (13.8%), and prostate (13.8%). Although the Qureshi and Quintas studies have shed some light on the stroke–cancer relationship, patients were followed for only a short period [i.e., 24 months (Qureshi et al. 2015) and 18 months (Quintas et al. 2018), respectively], and it is thus possible that cancer preceded the onset of stroke and that the stroke was favored by the hypercoagulable state of malignancy (Caine et al. 2002).
To the best of our knowledge, only two studies have analyzed the long-term risk of cancer in patients with a history of stroke. In 2015, researchers from Norway estimated, in 1282 ischemic stroke patients with no history of cancer, that neoplastic conditions were diagnosed in 4.3% of them after stroke (Selvik et al. 2015). Furthermore, the median time between the onset of stroke and the diagnosis of cancer was around 14 months, and almost 42% of patients were diagnosed with cancer in the year following stroke onset. The three most common cancer types were lung cancer (19.0%), prostate cancer (15.9%), and colorectal cancer (11.1%). Again, based on the short median time between stroke onset and cancer diagnosis, one cannot exclude the possibility that cancer was already present at the time of the stroke diagnosis. Another limitation of this study is that the analyses were restricted to ischemic stroke, and it is, therefore, difficult to extrapolate these findings to hemorrhagic stroke.
More recently, in 2017, Chen et al. (2017) observed, in more than 85,500 individuals who were followed for over 12 years in Taiwan, that the risk of cancer was lower in the stroke group than in the control group (HR = 0.79, 95% CI 0.74–0.84). It was hypothesized that patients are likely to modify their lifestyle (e.g., through diet, physical exercise, changes in sleep patterns) following a stroke. Nonetheless, when analyzing the different types of cancer separately, stroke was found to be a risk factor for brain cancer (HR = 3.09, 95% CI 1.80–5.30). Although this study is of particular interest, it has one important limitation that should be mentioned at this point. Based on the survival analysis, it is likely that the difference in the cumulative incidence rate of brain cancer between cases and controls was already significant after only a few months of follow-up and that there was no clear increase in this difference after the first year of follow-up (Chen et al. 2017). This severely undermines the findings and suggests that a substantial proportion of patients with stroke already had occult brain cancer at the index date. By contrast, the difference in the prevalence of cancer in stroke survivors and controls was not statistically significant after 1 year of follow-up in the present retrospective study conducted in Germany. Thus, it is unlikely that cancer preceded stroke and that there was a time-related bias in our analysis. Finally, there was a positive association between stroke and cancers of the respiratory and intrathoracic organs in men and women, and cancers of the digestive organs in men. Moreover, this study found no significant association between stroke and brain cancer. These findings may be explained by the power of the statistical analysis. Pulmonary and digestive cancers accounted for a substantial share of neoplastic disorders, whereas brain cancers were diagnosed in less than 0.5% of the population. Therefore, further studies are needed to gain a better understanding of the relationship between stroke and each type of cancer.
The large sample size and the long-term follow-up of patients are two major strengths of this study. Nonetheless, these findings should be interpreted in the light of several limitations. First, there was no data on the patients’ smoking and alcohol status, although these variables are known to be associated with both stroke (Reynolds et al. 2003; Shah and Cole 2010) and cancer (Boffetta and Hashibe 2006; Cornfield et al. 2009). It is possible that smoking and alcohol use were more common in stroke patients than in non-stroke patients and that this difference explained a substantial share of the stroke–cancer relationship. Second, there was a lack of information on inflammation markers (e.g., C-reactive protein, interleukins)—a factor that may at least partially predict the risk of cancer (Guo et al. 2015; Kakourou et al. 2015). Third, individuals followed in neurological practices were not included in the present study, which may have introduced a bias in the subsequent analyses. Fourth, a propensity score using a greedy algorithm and based on a large number of variables was used, and this resulted in the exclusion of approximately 30% of stroke patients. Fifth, since the regression used for propensity scores did not include the identification number of general practices, the distribution of these practices could be different between cases and controls. Finally, there was no information about patient deaths and, since both stroke and cancer have a significant impact on survival, this is an important limitation.
In conclusion, this study, including more than 37,000 patients from Germany, found an association between stroke and an increased cancer risk.
References
Andrykowski MA, Lykins E, Floyd A (2008) Psychological health in cancer survivors. Semin Oncol Nurs 24:193–201. https://doi.org/10.1016/j.soncn.2008.05.007
Boffetta P, Hashibe M (2006) Alcohol and cancer. Lancet Oncol 7:149–156. https://doi.org/10.1016/S1470-2045(06)70577-0
Caine GJ, Stonelake PS, Lip GYH, Kehoe ST (2002) The hypercoagulable state of malignancy: pathogenesis and current debate. Neoplasia N Y N 4:465–473. https://doi.org/10.1038/sj.neo.7900263
Chen C-W, Cheng T-J, Ho C-H, Wang J-J, Weng S-F, Hou Y-C, Cheng H-C, Chio C-C, Shan Y-S, Chang W-T (2017) Increased risk of brain cancer incidence in stroke patients: a clinical case series, population-based and longitudinal follow-up study. Oncotarget 8:108989–108999. https://doi.org/10.18632/oncotarget.22480
Cocho D, Gendre J, Boltes A, Espinosa J, Ricciardi AC, Pons J, Jimenez M, Otermin P (2015) Predictors of occult cancer in acute ischemic stroke patients. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc 24:1324–1328. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.02.006
Cornfield J, Haenszel W, Hammond EC, Lilienfeld AM, Shimkin MB, Wynder EL (2009) Smoking and lung cancer: recent evidence and a discussion of some questions. Int J Epidemiol 38:1175–1191. https://doi.org/10.1093/ije/dyp289
Dearborn JL, Urrutia VC, Zeiler SR (2014) Stroke and cancer—a complicated relationship. J Neurol Transl Neurosci 2:1039
Guo L, Liu S, Zhang S, Chen Q, Zhang M, Quan P, Lu J, Sun X (2015) C-reactive protein and risk of breast cancer: a systematic review and meta-analysis. Sci Rep 5:10508. https://doi.org/10.1038/srep10508
Jacob L, Kostev K (2017) Conflicts at work are associated with a higher risk of cardiovascular disease. Ger Med Sci GMS E J 15:Doc08. https://doi.org/10.3205/000249
Kakourou A, Koutsioumpa C, Lopez DS, Hoffman-Bolton J, Bradwin G, Rifai N, Helzlsouer KJ, Platz EA, Tsilidis KK (2015) Interleukin-6 and risk of colorectal cancer: results from the CLUE II cohort and a meta-analysis of prospective studies. Cancer Causes Control CCC 26:1449–1460. https://doi.org/10.1007/s10552-015-0641-1
Kostev K, Meister U, Kalder M, Jacob L (2017) Suspected cancer diagnoses made by general practitioners in a population with subsequently confirmed cancer diagnoses in Germany: a retrospective study of 31,628 patients. Oncotarget 8:84540–84545. https://doi.org/10.18632/oncotarget.20886
Kostev K, Lasrich M, Schüller L, Diogo I, Sesterhenn A, Jacob L (2018) Diagnoses of suspected cancer in otolaryngology practices in Germany. Mol Clin Oncol 9:459–463. https://doi.org/10.3892/mco.2018.1694
Mao JJ, Armstrong K, Bowman MA, Xie SX, Kadakia R, Farrar JT (2007) Symptom burden among cancer survivors: impact of age and comorbidity. J Am Board Fam Med 20:434–443. https://doi.org/10.3122/jabfm.2007.05.060225
Medeiros EA, Castañeda SF, Gonzalez P, Rodríguez B, Buelna C, West D, Talavera GA (2015) Health-related quality of life among cancer survivors attending support groups. J Cancer Educ Off J Am Assoc Cancer Educ 30:421–427. https://doi.org/10.1007/s13187-014-0697-8
Munir F, Yarker J, McDermott H (2009) Employment and the common cancers: correlates of work ability during or following cancer treatment. Occup Med 59:381–389. https://doi.org/10.1093/occmed/kqp088%5D
Quintas S, Rogado J, Gullón P, Pacheco-Barcia V, Dotor García-Soto J, Reig-Roselló G, Mondéjar R, Colomer R, Vivancos J (2018) Predictors of unknown cancer in patients with ischemic stroke. J Neurooncol 137:551–557. https://doi.org/10.1007/s11060-017-2741-0
Qureshi AI, Malik AA, Saeed O, Adil MM, Rodriguez GJ, Suri MFK (2015) Incident cancer in a cohort of 3,247 cancer diagnosis free ischemic stroke patients. Cerebrovasc Dis Basel Switz 39:262–268. https://doi.org/10.1159/000375154
Rathmann W, Bongaerts B, Carius H-J, Kruppert S, Kostev K (2018) Basic characteristics and representativeness of the German Disease Analyzer database. Int J Clin Pharmacol Ther 56:459–466. https://doi.org/10.5414/CP203320
Reynolds K, Lewis B, Nolen JDL, Kinney GL, Sathya B, He J (2003) Alcohol consumption and risk of stroke: a meta-analysis. JAMA 289:579–588. https://doi.org/10.1001/jama.289.5.579%5D
Selvik HA, Thomassen L, Bjerkreim AT, Næss H (2015) Cancer-associated stroke: the Bergen NORSTROKE study. Cerebrovasc Dis Extra 5:107–113. https://doi.org/10.1159/000440730
Shah RS, Cole JW (2010) Smoking and stroke: the more you smoke the more you stroke. Expert Rev Cardiovasc Ther 8:917–932. https://doi.org/10.1586/erc.10.56
Wiefarn S, Heumann C, Rettelbach A, Kostev K (2017) Risk of nonfatal stroke in type 2 diabetes mellitus patients: a retrospective comparison between disease management programs and standard care. J Diabetes Sci Technol 11:808–813. https://doi.org/10.1177/1932296817691304
World Health Organization (2018) Cancer—key facts. http://www.who.int/news-room/fact-sheets/detail/cancer. Accessed 14 Dec 2018
Yabroff KR, Lund J, Kepka D, Mariotto A (2011) Economic burden of cancer in the US: estimates, projections, and future research. Cancer Epidemiol Biomark Prev Publ Am Assoc Cancer Res Cosponsored Am Soc Prev Oncol 20:2006–2014. https://doi.org/10.1158/1055-9965.EPI-11-0650
Zöller B, Ji J, Sundquist J, Sundquist K (2012) Risk of haemorrhagic and ischaemic stroke in patients with cancer: a nationwide follow-up study from Sweden. Eur J Cancer 48:1875–1883. https://doi.org/10.1016/j.ejca.2012.01.005
Acknowledgements
Professional English language editing services were provided by Claudia Jones, MA, Radford, Virginia, United States.
Funding
The authors have received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Both authors declare that they have no conflicts of interest.
Ethical approval
German law allows the use of anonymous electronic medical records for research purposes under certain conditions. According to this legislation, it is not necessary to obtain informed consent from patients or approval from a medical ethics committee for this type of observational study that contains no directly identifiable data. Because patients were only queried as aggregates and no protected health information was available for queries, no IRB approval was required for the use of this database or the completion of this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jacob, L., Kostev, K. Cancer risk in stroke survivors followed for up to 10 years in general practices in Germany. J Cancer Res Clin Oncol 145, 1013–1020 (2019). https://doi.org/10.1007/s00432-019-02855-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-019-02855-w